Abstract
Purpose
The purpose of this study was to examine the influence of diet family support on glucose outcome in Korean immigrants with type 2 diabetes taking into consideration patient gender.
Methods
A total of 143 Korean immigrants with type 2 diabetes were recruited from a West Coast Koreatown. Upon completing questionnaires (demographic, health history, and the Diabetes Family Behavior Checklist-II), a participant was given a finger stick blood test for glycosylated hemoglobin (A1C). Body mass index (BMI) and waist-to-hip ratio (WHR) were calculated after measurements were taken. Analyses assessed the independent associations of diet family support, gender, and diet family support by gender interactions with glucose outcome.
Results
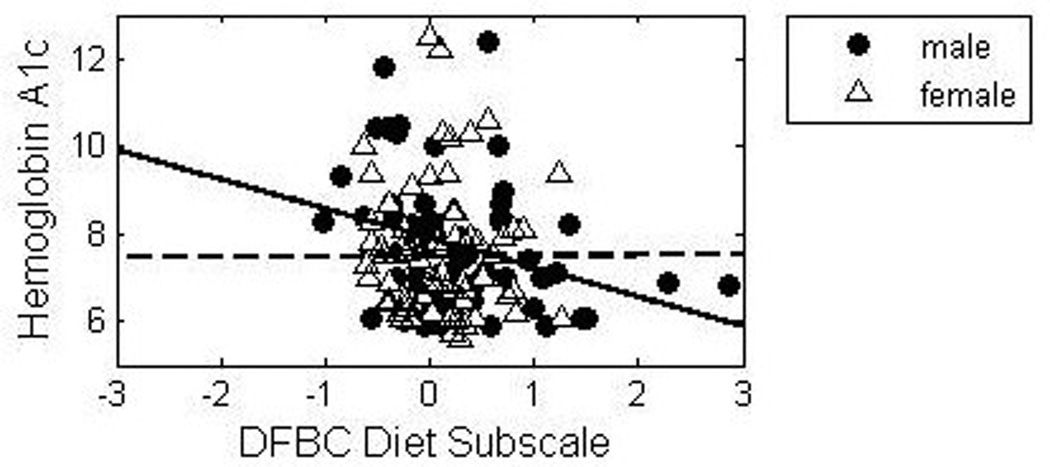
A higher level of diet family support was significantly associated with lower A1C, indicating the beneficial effect of diet family support on glucose control. Although the main effect of gender on A1C was not significant, the effect of the product term of family support and gender was, indicating that the significant beneficial impact of diet family support on A1C depends on gender. The impact is much more pronounced in men (B = −.516) than women (B = − .038).
Conclusions
Family support specific to diet is significantly associated with glucose outcomes in Korean immigrants with type 2 diabetes, that is, more perceived family support was associated with better glucose control. The positive impact of family support on glucose outcome was significantly stronger in men than women, even after other factors were taken into consideration.
Type 2 diabetes is rising at an alarming rate among Korean immigrants, the 5th largest Asian American subgroup in the United States. 1,2 In Southern California where over a quarter of the Korean population in the US live, the prevalence more than doubled (4.3% to 9.1 %) between 2003 and 2005, the highest rate of increase among Chinese, Vietnamese, Filipino, and Japanese Americans. 3 The prevalence rate in Korean immigrants is higher than Vietnamese (8.3%) and Chinese Americans (4.2%) in Southern California 3 and also higher than national survey data between 2004 and 2006 for Asian Americans (7.6%) and Caucasians (6.6%).4 Despite the high prevalence, little is known about diabetes management in Korean immigrants in the United States.
Diet plays an important role in the management of diabetes and inadequate diet is a commonly identified problem of diabetes management. 5–7 Following a recommended diabetes diet regimen may be particularly challenging for Korean immigrants with type 2 diabetes because staple foods in traditional Korean diet are high carbohydrate foods and most diabetes diet guidelines were developed for a Western diet. In studies with Chinese immigrants whose diet composition is similar to Korean, patients with type 2 diabetes identified diet as the major source of problem related to diabetes management. 6, 8 Patients also reported that having to restrict the amount of rice and not being able to share favorite foods with family members were unpleasant limitations and a struggle. 6, 9
Because lifestyle behaviors, such as diet and food preparation, are among the mainstays of diabetes management and these behaviors evolve through or take place within the family setting, the family has particular importance for patients with type 2 diabetes. 10–12 Diabetes management depends heavily on consistency, and activities such as diet often involve major lifestyle changes that affect daily routines and family relationships. 11 For this reason, an ecological or social systems perspective, which places the individual with chronic illness within his or her primary social context and observes how the individual and other members of the social context operate together to affect and be affected by disease outcomes seems the most appropriate framework.13 This framework suggests that the family is the social context with the most immediate and profound effects on diabetes management. 12 Family members’ responses to the disease and to disease management have been linked to a patient’s self-care behavior.14–15
In studies with European Americans, Latino, and Chinese American patients, family support has been shown to have a positive impact on glycemic control and self-care behaviors 16–17 or no impact. 18–19 Although the family’s role in successful diabetes management has been recognized 20–21 and this may be particularly true for Asian immigrants because of their family oriented culture, research in this area is extremely limited in Asian immigrant populations 22; very limited information is available for Korean immigrants.
Gender differences have been noted in giving and receiving social support. Women not only are disproportionately providers of social support but also are more likely to seek and use social support.23–24 The confluence of gender role and gender itself with social support has been mentioned in the literature although their effects on health outcomes have not been clearly delineated. This could be related to the fact that most studies measured self-management behaviors by self-report rather than using biological indices, 25 thus making it difficult to assess the direct impact of gender role and social support on disease outcomes. A few studies that examined gender differences in social support with respect to diabetes management reported that more diabetes specific support was related to better adherence to self-care among older men, but not among women, 26and dietary management was more difficult for women than men.27 Although less is known about the influence of social support and gender on diabetes management and outcomes among Asian populations, a few studies with Asian populations suggested that the influence of social support on subjective health and health outcomes may vary according to gender.28–30 Therefore, in the present study, we sought to examine the influence of dietary family support on glucose control in Korean immigrants with type 2 diabetes, taking into consideration patient gender.
Methods
Design and Sample
This cross-sectional descriptive study included a convenience sample of 143 immigrant Korean men and women with type 2 diabetes between 30 and 80 years of age. Subjects were recruited with flyers and posters from a variety of community sites in a West Coast Koreatown, including two health center clinic waiting areas, pharmacies, and shopping malls. The subjects were self-identified as Korean-born immigrants with a diagnosis of type 2 diabetes for at least a year and able to speak, read, and write in Korean or English. The study was approved by a university institutional review board, and all participants provided written informed consent.
Data Collection Procedures
After obtaining study consent, participants were asked to complete a questionnaire booklet which includes demographic information, health history, and the Diabetes Family Behavior Checklist – II in either English or Korean according to their preference. Upon completing the questionnaire, a participant was given a finger stick blood test to assess his or her level of glycosylated hemoglobin (A1C) and body mass index (BMI) and waist-to-hip ratio (WHR) were calculated after measurements were taken. A1C levels were obtained by the researcher or a staff nurse at one of the study sites using standardized procedures. When data collection was completed, participants were given the results of their A1C and anthropometric measures.
Measure of Dependent Variable: Glycosylated Hemoglobin (A1C)
The A1C level was measured from a finger stick sample of whole blood by the A1c Now Inview (Metrika, Sunnyvale, CA), an instrument certified by the National Glycohemoglobin Standardization Program. A1C was also obtained from those patients who were recruited at a health center and who offered their recorded A1C levels for the study. Because the clinic uses the same instrument (A1cNow Inview) as this study and these values were recorded by the clinic staff, participant-provided results were used if they were less than 3 months old instead of doing new finger stick tests.
Measures of Independent Variables
Family Support
Family support was measured by the Diabetes Family Behavior Checklist-II (DFBC). 5 The scale was developed to assess supportive and nonsupportive family behaviors specific to diabetes on a five-point Likert-type scale in the following areas: medication compliance, glucose testing, exercise, and diet. Scores can be calculated in several ways: a supportive summary score, a nonsupportive summary score, and regimen-specific composite scores. Previous studies indicate that subscales are stronger predictors of their respective areas of regimen adherence than either the overall supportive or nonsupportive summary score. 5 Regimen-specific subscales (diet, exercise) have been used in previous studies with Mexican Americans. 17 The present study used diet regimen-specific subscales, which is composed of 2 supportive and 2 non-supportive items: asking how often a particular family member will “praise you for following your diet” “eat at the same time that you do” “nag you about not following your diet” “eat foods that are not part of your diabetes diet” to assess diabetes family support specific to diet. Non-supportive items in this subscale were reverse coded, summed for total subscale scores, and then averaged to obtain mean scores. Higher scores indicate a stronger perception of supportive interaction. The internal consistency (Cronbach’s alpha) of this sample was .59. The DFBC II has not been validated in the Korean population. However, lower internal consistency would be expected in subscales given the few items contributing to the scores.5
Demographics and Health Variables
Information on age, gender, years with diabetes, and the number of diabetic medications was obtained from a patient’s self-report on the questionnaire. To determine BMI and WHR, height, weight, waist and hip circumferences were measured. Height was measured in centimeters - without shoes - using a non-stretching measuring tape secured to the wall. Weight was measured in kilograms by a professional body-weight scale; participants wore light clothing and no shoes or belongings (e.g., keys and cell phones). BMI was calculated using the formula BMI = kg/m2. Waist circumference was measured in centimeters by placing a nonstretching measuring tape in a horizontal plane around the bare abdomen at the top of the iliac crest or just above the hip bone. The reading was taken at the end of an expiration, making sure that the tape was secure but not too tight. The hip measurement was taken at the point yielding maximum circumference over the buttocks. WHR was calculated by dividing the waist measurement by the hip measurement.
Translation of Instruments
For this study, the DFBC was translated into Korean by the author and then back-translated into English by a bilingual graduate student nurse using techniques suggested by Brislin. 31Any discrepancies were resolved by the consensus of three bilingual Korean immigrants, two of whom were health care professionals and a volunteer translator at a medical center near the Korean community. The instrument was pilot tested with five diabetic patients in the same Korean community sites as the study population. A few problems were noted with the exact translation of some of words into Korean. Based on the feedback of the pilot-test participants, the three bilingual reviewers debated and decided to use the words whose meanings in Korean are closer to those in the scale’s original version and better understood by participants.
Statistical Analyses
Descriptive statistics provided information on the variables in this study. First, the differences of means were tested with independent group t-test and of the distribution of proportions with the chi-square test. Bivariate analyses were conducted to evaluate the relationship between the independent variables and A1C. Independent variables were examined for multicollinearity. To address this study’s first research question, does family support predict A1C, a multiple linear regression was done in which the level of glucose control, measured by A1C, was the dependent variable and family support, WHR, the number of years with diabetes, the number of diabetic medications, age, and gender were the independent variables. Body mass index (BMI) was not significantly correlated with A1C for the bivariate analysis and therefore not included in the model. First, the overall R2 of the main effect model was examined for significance. If the overall model was significant, the unique contribution of each separate independent variable in explaining the variance in A1C was tested. To answer the second research question, does gender influence the relationship between diet family support and glucose outcome (A1C), the product term (family support and gender) was entered in the second block (Model 2). The significance of the R2 change was examined for a significant interaction between family support and gender. Data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 12.0 (SPSS Inc., Chicago, IL).
Results
The respondents’ characteristics by gender are shown in Table 1. No significant differences in mean family size, duration with diabetes, number of diabetes medication, BMI, and A1C were observed between men and women. On average, women were older and lived in the US longer than men. Mean WHR was significantly higher in men than in women, which was an expected finding because men have a higher cut off for normal than women. Mean diet family support scores were significantly higher in men than women. The proportion of subjects who responded to ‘family member you have the most contact with’ was significant in men and women. Although the spouse was the family member with most contact for men and women, men were more likely to have the most contact with a spouse than women, whereas women were more likely to have the most contact with a child than did men.
Table 1.
Characteristics of the Study Sample
| Variables | Total N=143 |
Men N=69 |
Women N=74 |
P values Men vs. Women |
|---|---|---|---|---|
| age | 62.4 (12.8) | 60.2 (13.3) | 64.5 (11.9) | .044* |
| Years in the United States | 21.7 ( 9.2) | 20.1 (9.5) | 23.2 (8.7) | .044* |
| Number of family living with the respondent | 1.64 (1.5) | 1.88 (1.4) | 1.41 (1.6) | .062 |
| Family member most contact with (%) | .004** | |||
| Spouse | 89 (62.2%) | 51 (73.9%) | 38 (51.4%) | |
| Child | 39 (27.3%) | 10 (14.5%) | 29 (39.2%) | |
| Other | 15 (10.5%) | 8 (11.6%) | 7 (9.5%) | |
| Years with diabetes | 6.78 (6.21) | 7.65 (7.07) | 5.96 (5.20) | .104 |
| Number of diabetic medications | 1.22 (0.80) | 1.12 (0.76) | 1.31 (0.83) | .145 |
| DFBC diet | 0.56 (1.06) | 0.77 (1.04) | 0.36 (1.05) | .023* |
| BMI | 25.8 (3.2) | 26.2 (3.2) | 25.4 (3.03) | .110 |
| WHR | 0.89 (0.05) | 0.92 (0.03) | 0.86 (0.04) | .000** |
| A1C | 7.59 (1.45) | 7.66 (1.45) | 7.53 (1.46) | .592 |
Mean (standard deviation)
A1C = glycosylated hemoglobin, DFBC = Diabetes Family Behavior Checklist, BMI = body mass index, WHR = waist-to-hip ratio
p < .05, 2-tailed.
p < .01, 2-tailed.
Table 2 shows the multivariate analyses of the effect of diet family support and gender on glucose control (A1C). As shown in model 1, age, gender, number of years with diabetes, the number of diabetes medications, WHR, and diet family support together explained approximately 19 percent of total variance in A1C (R2 =0.191, F(6, 136) = 5.34, p <.0001). The main effect of diet family support was significant. A higher level of family diet support was associated with lower A1C, therefore it had a beneficial effect on glucose control. A higher WHR, longer duration with diabetes, more diabetes medications were associated with higher A1C. The main effect of gender on A1C was not significant. However, in model 2, there was a significant R2 change, F (1,135) = 4.85, p < .029, with the addition of the product term of family support and gender, indicating that the significant beneficial impact of diet family support on A1C depends on gender.
Table 2.
Multiple regression analyses of the effect of diet family support and sex on glucose control (A1C)
| Source | R2 | Beta | sr2 | df | F | p | |
|---|---|---|---|---|---|---|---|
| Model 1 | Overall | .191 | 6, 136 | 5.34 | .000 | ||
| Age | −.023 | .037 | 1, 136 | 6.14 | .014* | ||
| Gender | .167 | .002 | 1, 136 | 0.33 | .566 | ||
| Years with diabetes | .041 | .026 | 1, 136 | 4.29 | .040* | ||
| Medication | .373 | .037 | 1, 136 | 6.16 | .014* | ||
| WHR | 5.325 | .020 | 1, 136 | 3.38 | .068 | ||
| DFBC Diet | −.264 | .035 | 1, 136 | 5.86 | .017* | ||
| Model 2 | Overall | .219 | 7, 135 | 4.85 | .029 | ||
| Age | −.020 | .027 | 1, 135 | 4.59 | .034* | ||
| Gender | .194 | .003 | 1, 135 | 0.46 | .500 | ||
| Years with diabetes | .041 | .025 | 1, 135 | 4.39 | .038* | ||
| Medication | .352 | .033 | 1, 135 | 5.63 | .019* | ||
| WHR | 6.097 | .026 | 1, 135 | 4.48 | .036* | ||
| DFBC Diet | −.516 | .063 | 1, 135 | 10.79 | .001* | ||
| Gender×DFBC | .478 | .028 | 1, 135 | 4.85 | .029* |
A1C = glycosylated hemoglobin, DFBC = Diabetes Family Behavior Checklist, BMI = body mass index, WHR = waist-to-hip ratio
p < .05, 2-tailed
In Figure 1., the impact of gender on the relationship between diet family support and gender was plotted. The graph shows that in men, as diet support increases, A1C goes down, indicating that family diet support benefits men (B = −.516). However, diet family support does not affect women at all or only at negligible levels (B = − .038).
Figure 1.
Discussion and Conclusions
The present study demonstrated that family support specific to diet is significantly associated with glucose outcomes in Korean immigrants with type 2 diabetes, that is, more perceived family support was associated with better glucose control. The association of family support with A1C was independent of age, duration of diabetes, number of diabetes medication, and waist-to-hip ratio. Further, the study found that the relationship between family support and glucose outcome is gender-dependent. The positive impact of family support on glucose outcome was significantly stronger in men than women, even after other factors were taken into consideration.
The study provided evidence that diet family support has direct influence on glucose control and the finding is consistent with previous studies that showed positive influence of family support on diabetes management in other ethnic minorities.17 The greater impact of diet family support on glucose control in men and virtually no effect on women was surprising. However, this finding was also consistent with two recent studies of social support and health in Japanese population. 29–30 In one study, low social support was associated with higher risk of stroke mortality in men, but not women, and in another study, significant positive association between the level of social support and good subjective health was observed among elderly men, but not among elderly women.
Social support literature shows that women are more involved than men in both giving and receiving social support. 24 Women also tend to seek and utilize support more than men. However, most social support studies were conducted with Caucasian populations and less is known about social support among Asian populations. In the current study, Korean men with type 2 diabetes received more support from family and seemed to utilize it better than women. This difference may be cultural and a possible explanation may be that Korean women, as with Japanese and Chinese women, are less expressive of their need to get support than Caucasian women. 32 Requesting support can be viewed as more of a burden in these cultures and Korean immigrant women may have been reluctant to impose on their family with their health problems. Alternatively, the men may not have been as helpful for the women as the women have been for the men. This is consistent with the general social support literature which suggests that men rely heavily on their female spouses for support but women do not rely on their male spouses as a primary source of support, turning more to their network of friends and other relations. Another possible explanation for gender differences might be that social support from a spouse may be more beneficial than from children given more men than women in this study identified their spouse as the person with whom they have most contact. If the spouse indeed is a better provider of support than children in diabetes diet management, women may be disadvantaged because they tend to live longer than men and are therefore less likely to have spouses available over time. Additional social support may need to be provided to women with no spouse. The third explanation is that traditional family role as well as gender may interact to influence perceptions of social support. For example, since wives are expected to be the primary family caregiver to their spouses, they are likely to comply with this expectation and revise dietary patterns for their male diabetic spouses. On the other hand, most male spouses do not assume the role of cook for their diabetic wives and thus do not offer much diet support. A qualitative study by Maclean 27 reported similar findings and suggested that men receive more direct support for their dietary needs from their spouses than do women.
Results of the present study point to two specific implications for both nursing practice and research. First, gender differences in receiving and utilizing family support for dietary self-management and its impact on glucose control should deserve attention and further investigation. Given that women are more prone to poor outcomes and complications from diabetes than men, 33 vigilance in maintaining optimal glucose control is essential for both genders. Second, gender difference should be considered when family support interventions are planned for diabetes management. Having more dietary support from family seems to be beneficial to men, but does not seem to be beneficial to women in Korean immigrants with type 2 diabetes. Therefore, diabetes educators and other health care providers working with this population may need to identify different sources of social support for Korean women with diabetes while encouraging support from family for men.
Certain limitations need to be considered when reviewing these findings. First, the study was cross-sectional and therefore causality cannot be assumed. We cannot conclude whether family support can predict glucose control with or without the influence of gender. Also, family support may change over time and longitudinal study may be needed to clarify gender and role differences in the relationship between changes in level of family support and glucose control. Second, although the scale used in this study was tested in previous studies, diet family support was assessed with a 4 item subscale. Therefore, other aspects of family support that may be important to diet management, such as helping selection of food, calculating calories and portions that deal with more instrumental domains of support, could not be assessed. Future studies should consider developing tools to better measure diet family support. Lastly, this study only examined family support in diet, therefore findings may not be generalized to other domains of diabetes management such as exercise or adherence to medications. Gender differences in other areas of diabetes self-management need further investigation.
In sum, the most important finding of this study is the gender differences in the relationship between family diet support and glucose outcome. Although gender by itself does not predict A1C, the relationship between diet support and glucose outcome are moderated by gender. Studies are needed to examine how best to utilize family support in men and women and its effect on glucose control. Future studies should also investigate which family member can be the best provider of support in diabetes management and whether the family member is different by gender, role, and culture. A deeper understanding of the roles gender and the family context play in day to day diabetes self-management would allow for the development of tailored interventions that maximize positive outcomes of diabetes care. In addition, identifying domains of family support that are specifically important to diabetes care in men and women will help both clinicians and researchers design effective family education programs and interventions targeting those areas.
Acknowledgements
Support for this study was received from the National Institute of Nursing Research, National Institutes of Health (5 F31 NR009329). The author thanks Sally Rankin, PhD, RN for her thoughtful review of the manuscript and Steven Paul, PhD for his assistance with the statistical analyses.
Footnotes
Disclosure:
Author of this article has no conflict of interest to disclose.
References
- 1.Why is diabetes more common in Asian Pacific Islander? [Internet]. [updated 2004 Mar 2] Boston (MA): Joslin Diabetes Center, Asian American Diabetes Initiative; [cited 2008 Sep 1]. Available from: http://aadi.joslin.harvard.edu/intro/intro_why_asian.asp. [Google Scholar]
- 2.Current population reports, population characteristics: The Asian and Pacific Islander population in the United States. U. S. Census Bureau, Population Census. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 3.California Health Interview Survey (CHIS) [Internet]. [updated 2005 Jan 1] Los Angeles (CA): UCLA Center for Health Policy Research; [cited 2008 Jul 24]. Available from: http://www.his.ucla.edu/main/DQ2/output.asp. [Google Scholar]
- 4. [cited 2008 Dec 3];National Diabetes Statistics 2007 [Internet]. [updated 2008 Jun 1]. National Institute of Diabetes and Digestive and Kidney Diseases. Available from: http://diabetes.niddk.nih.gov/dm/pubs/statistics/
- 5.Glasgow RE, Toobert DJ. Social environment and regimen adherence among type II diabetic patients. Diabetes Care. 1988;11(5):377–386. doi: 10.2337/diacare.11.5.377. [DOI] [PubMed] [Google Scholar]
- 6.Rankin S, Galbraith M, Huang P. Quality of life and social environment as reported by Chinese immigrants with non-insulin-dependent diabetes mellitus. Diabetes Educ. 1997;23:171–177. doi: 10.1177/014572179702300208. [DOI] [PubMed] [Google Scholar]
- 7.Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes. Diabetes Care. 2002:1722–1728. doi: 10.2337/diacare.25.10.1722. [DOI] [PubMed] [Google Scholar]
- 8.Wang CY, Chan SM. Culturally tailored diabetes education program for Chinese Americans. A pilot study. Nurs Res. 2005;54:347–353. doi: 10.1097/00006199-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Lin CC, Anderson RM, Hagerty BM, Lee BO. Diabetes self-management experience: a focus group study of Taiwanese patients with type 2 diabetes. J Clin Nurs. 2008;17(5A):34–42. doi: 10.1111/j.1365-2702.2007.01962.x. [DOI] [PubMed] [Google Scholar]
- 10.Hauser ST. The study of families and chronic illness: Ways of coping and interacting. In: Brody G, Sigel I, editors. Methods of Family Research II. New York: Plenum; 1990. pp. 59–86. [Google Scholar]
- 11.Campbell TL. The effectiveness of family interventions for physical disorders. J Marital Fam Ther. 2003;29(2):263–281. doi: 10.1111/j.1752-0606.2003.tb01204.x. [DOI] [PubMed] [Google Scholar]
- 12.Fisher L, Weihs K. Can addressing family relationships improve outcomes in chronic disease? J Fam Pract. 2000;49:561–566. [PubMed] [Google Scholar]
- 13.Weihs K, Fisher L, Baird M. Families, health, and behavior. Fam Syst Health. 2002;20:7–46. [Google Scholar]
- 14.Fisher L, Chesla CA, Skaff MM, Gilliss C, Mullan JT, Bartz RJ, et al. The family and disease management in Hispanic and European-American patients with Type 2 diabetes. Diabetes Care. 2000;23(3):267–272. doi: 10.2337/diacare.23.3.267. [DOI] [PubMed] [Google Scholar]
- 15.Chesla CA, Fisher L, Skaff MM, Mullan JT, Gilliss CL, Kanter R. Family predictors of disease management over one year in Latino and European American patients with type 2 diabetes. Fam Process. 2003;42(3):375–390. doi: 10.1111/j.1545-5300.2003.00375.x. [DOI] [PubMed] [Google Scholar]
- 16.Fisher L, Chesla CA, Chun K, Skaff MM, Mullan JT, Kanter RA. Patient-appraised couple emotion management and disease management among Chinese American patients with Type 2 diabetes. J Fam Psychol. 2004;18(2):302–310. doi: 10.1037/0893-3200.18.2.302. [DOI] [PubMed] [Google Scholar]
- 17.Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with Type 2 diabetes. Diabetes Educ. 2004;30(6):980–993. doi: 10.1177/014572170403000619. [DOI] [PubMed] [Google Scholar]
- 18.Chyun D, Lacey KO, Katten DM, Talley S, Price WJ, Davey JA, et al. Glucose and cardiac risk factor control in individuals with Type 2 diabetes. Diabetes Educ. 2006;32(6):925–939. doi: 10.1177/0145721706295016. [DOI] [PubMed] [Google Scholar]
- 19.Gleeson-Kreig JA, Bernal H, Woolley S. The role of social support in the self management of diabetes mellitus among a Hispanic population. Public Health Nurs. 2002;19:215–222. doi: 10.1046/j.0737-1209.2002.19310.x. [DOI] [PubMed] [Google Scholar]
- 20.Glasgow RE, Wagner EH, Kaplan RM, Vincor F, Smith LN, Norman J. If diabetes is a health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;2:159–170. doi: 10.1007/BF02908297. [DOI] [PubMed] [Google Scholar]
- 21.El-Kebbi IM, Bacha GA, Ziemer DC, Musey VC, Gallina DL, Dunbar V, et al. Diabetes in urban African Americans: Use of discussion groups to identify barriers to dietary therapy among low-income individuals with non-insulin-dependent diabetes mellitus. Diabetes Educ. 1996;22:488–492. doi: 10.1177/014572179602200508. [DOI] [PubMed] [Google Scholar]
- 22.Esperat CM, Inouye J, Gonzalez EW, Owen DC, Feng D. Health disparities among Asian Americans and Pacific Islanders. Annu Rev of Nurs Res. 2004;22:135–159. [PubMed] [Google Scholar]
- 23.Taylor S. Social support. In: Friedman HS, Silver RC, editors. Foundations of Health Psychology. New York: Oxford University Press; 2007. pp. 145–171. [Google Scholar]
- 24.Tamres L, Janicki D, Helgeson VS. Sex differences in coping behavior: A meta-analytic review. Pers Soc Psychol Rev. 2002;6:2–30. [Google Scholar]
- 25.Gallant M. The influence of social support on chronic illness self-management: A review and directions for research. Health Educ Behav. 2003;30:170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- 26.Connell CM, Fisher EB, Houston CA. Relationships among social support, diabetes outcomes, and morale for older men and women. J Aging Health. 1992;4:77–100. [Google Scholar]
- 27.Maclean HM. Patterns of diet related self-care in diabetes. Soc Sci Med. 1991;32:689–696. doi: 10.1016/0277-9536(91)90148-6. [DOI] [PubMed] [Google Scholar]
- 28.Ho SC. Health and social predictors of mortality in an elderly Chinese cohort. Am J Epidemiol. 1991;133:907–921. doi: 10.1093/oxfordjournals.aje.a115970. [DOI] [PubMed] [Google Scholar]
- 29.Okamoto K, Tanaka Y. Gender difference in the relationship between social support and subjective health among elderly persons in Japan. Prev Med. 2004;38:318–322. doi: 10.1016/j.ypmed.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 30.Ikeda A, Iso H, Kawachi I, Yamagishi K, Inoue M, Tsugane S. Social support and stroke and coronary heart disease: The JPHC study cohort II. Stroke. 2008;39(3):768–775. doi: 10.1161/STROKEAHA.107.496695. [DOI] [PubMed] [Google Scholar]
- 31.Brislin RW, editor. The wording and translation of research instruments. Beverly Hills, CA: Sage; 1986. [Google Scholar]
- 32.Wellisch D, Kagawa-Singer M, Reid SL, Lin YJ, Nishikawa Lee S, Wellisch M. An exploratory study of social support: a cross-cultural comparison of Chinese-, Japanese-, and Anglo-American breast cancer patients. Psychooncology. 1999;8(3):207–219. doi: 10.1002/(SICI)1099-1611(199905/06)8:3<207::AID-PON357>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 33.Diabetes and Cardiovascular (Heart) Disease. [Internet]. [updated 2008 Mar 21] American Diabetes Association; [cited 2009 Jan 3]. Available from: http://www.diabetes.org/diabetes-statistics/heart-disease.jsp. [Google Scholar]