Summary
Traumatic injury resulting in isolated dysfunction of the hypoglossal nerve is relatively rare and described in few case reports. We present a patient with isolated unilateral palsy of the twelfth cranial nerve (CN XII) resulting from recurrent airway intervention following extensive burn injuries. The differential diagnosis for paralysis of the CN XII is also discussed herein. This case illustrates the significance of comprehensive diagnostic evaluation and the need for refined airway manipulation in patients that require multiple endotracheal intubations
Keywords: hypoglossal nerve, endotracheal intubation, nerve injury, burn patients, intensive care
Abstract
Une blessure traumatique résultant en un dysfonctionnement isolé du nerf hypoglosse est relativement rare et décrit dans quelques rapports de cas. Nous présentons un patient atteint de paralysie hypoglossal unilatérale isolée à la suite de l’intervention des voies respiratoires récurrentes après de brûlures extensives. Le diagnostic différentiel de la paralysie du nerf crânien (NC XII) est également discuté ici. Ce cas illustre l’importance de l’évaluation diagnostique complète et la nécessité pour la manipulation délicate des voies respiratoires chez les patients qui nécessitent de multiples intubations trachéales.
Introduction
Injuries to the hypoglossal nerve following intubation have been reported in recent literature.1-14 However, hypoglossal nerve paralysis is still considered a rare complication of airway management. While a review of the literature reveals a few case reports describing this type of injury, no recent data is available on the prevalence of these incidents. Most reviewed cases described incidents of CN XII palsy following an elective general anesthesia, using an endotracheal tube with no difficulties during the intubation procedure.1,2,7-9,11,12 Some cases are related to the use of laryngeal mask airway.5,6,13,15-17 In a few of these cases, the injury is attributed to an unusual head or body positioning during intubation that is mostly due to surgical considerations.6,10 Most of these cases took place in the setting of scheduled elective surgeries, and all patients underwent a single endotracheal maneuver.
Herein we present a case of unilateral hypoglossal nerve injury in a patient with extensive burn injury, following multiple recurrent airway managements. Hypoglossal nerve paralysis has a wide differential diagnosis in a traumatic burn injury patient, which will be discussed.
Case report
A previously healthy 34 year-old man arrived at our hospital following a motor vehicle accident that included an explosion of volatile substances. He suffered 40% burns to his face and body, affecting his back, hands and calves as well as his arms bilaterally and circumferentially. Approximately 20% Total Body Surface Area (TBSA) suffered full thickness burns. Upon arrival at the emergency room, the patient was intubated due to the extent of his burn injuries and a concomitant suspected inhalation injury. The intubation procedure was performed without any difficulties; no force was used to place the endotracheal tube. Upon admission to our department a bronchoscopy was performed, resulting in findings that were compatible with severe inhalation injury. A 4cm long scalp laceration was cleaned and closed using a stapler. A total body Computerized Tomography (CT) scan was performed and ruled out any fractures, hemorrhages or injury to internal organs, including cervical spine and intracranial structures.
During his hospitalization period in the burn unit, the patient was extubated (three days after arrival). Two days later, he was re-intubated due to respiratory insufficiency derived from Acute Respiratory Distress Syndrome (ARDS). Again, intubation was successful and without complications. While still intubated and anaesthetized, the patient underwent repeated surgical debridement and skin grafting procedures. At each instance, there was no need for airway management since the patient was already intubated. Two weeks after his arrival the patient was again extubated successfully. At that time, the patient was given oxygen via mask and was administered with bronchodilator inhalations. Routine examination at this time demonstrated anisocoria with a dilated left pupil, possibly owing to a beta adrenergic effect of a bronchodilator inhalation. Both pupils were reactive to light. Further examination revealed no other neurological deficit; however, examination took place under light sedation and administration of analgesia. A second CT scan was performed and showed subdural fluid collection surrounding the frontal area that represented a subdural hygroma. No dural tear was diagnosed on examination of the spine and cranium, and there was no evidence of intracranial hemorrhage or herniation. The advice from neurosurgical consultation was that no surgical intervention was needed at the time.
A few weeks later, the patient underwent one more burn debridement surgery that required endotracheal intubation. He was extubated immediately after surgery without any complications. A day later, the patient’s wife reported that he had slurred speech and difficulty swallowing. Physical examination revealed pronounced deviation of the tongue to the left, without any associated unilateral tongue wasting or fasciculation. These findings may be explained by hypoglossal nerve paralysis. A CT angiography was performed, demonstrating normal vasculature and lingual asymmetry with fat atrophy on the left side. No pathological masses or lesions were found in the hypoglossal canal. There was also no residual evidence of the previously diagnosed subdural hygroma.
Finally, while left hypoglossal nerve dysfunction was diagnosed, examination of all other cranial nerves revealed nothing worthy of note. Therefore, we consider this case as an isolated peripheral nerve injury.
Upon routine follow-up sessions after discharge from the burn unit, the patient’s symptoms fully resolved spontaneously with no sequelae.
Discussion
The CN XII supplies the intrinsic and extrinsic muscles of the tongue, being a pure motor nerve. It has both bulbar and spinal origin; nerve fibers originate from the medulla oblongata, and C1 fibers join the nerve as it exits the skull. The cervical root fibers innervate the strap muscles of the neck. Supranuclear fibers originate from the contra-lateral cortical homunculus of the primary motor cortex. Both genioglossus muscles must be innervated and properly functioning to protrude the tongue in the midline. Tongue deviation is caused by unilateral disorder of the hypoglossal nerve. The tongue will protrude towards the weak muscle.
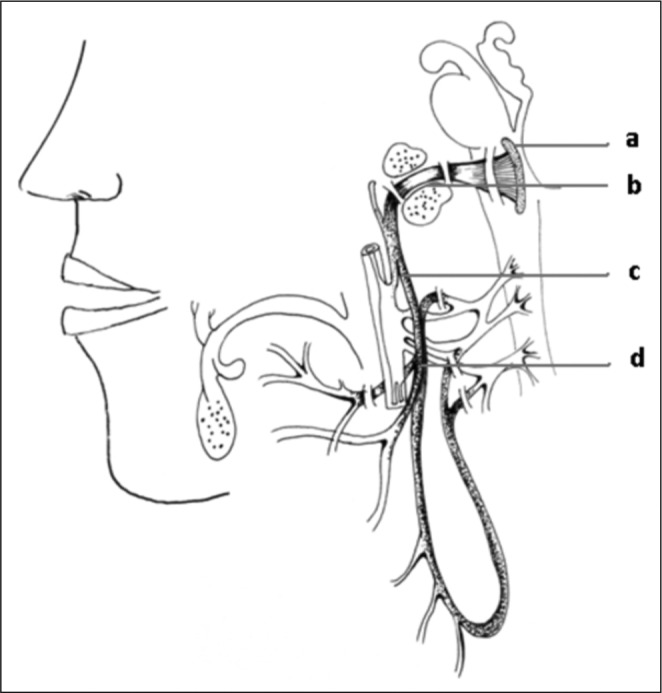
Thompson18 described an anatomic approach to the differential diagnosis of hypoglossal paralysis: supranuclear lesions will cause tongue deviation away from the lesion and, as an upper motor neuron injury, will not show atrophy or fasciculation; nuclear or infranuclear lesions will demonstrate lower motor neuron disorder which will be ipsilateral to the lesion. If the cervical strap muscles are involved, meaning the patient has difficulty swallowing, the lesion is suspected to be peripheral - distal to the point at which C1 fibers join the CN XII (Fig. 1 - d). In the setting of traumatic injury, fractures of the base of the skull may involve the hypoglossal canal (Fig. 1 - b). Vascular etiologies, like vertebral artery aneurism, carotid artery aneurism or jugular vein thrombosis are also possible causes (Fig. 1 - c). Infectious etiology should also be noted, as burn patients are often considered immuno-deficient. 19,20
Fig. 1. Lower motor neuron injury of CN XII (a) A pathology affecting the CN XII nucleus may cause ipsilateral paralysis. (b) The segment in the hypoglossal canal may be damaged following traumatic injury causing fractures of the base of the skull. (c) Following its course, the nerve may be injured by a vascular pathology. (d) Injury to the neck segment may involve the cervical strap muscles.
For pathophysiology considerations, the review of the literature by Brimacombe et al.17 suggested potential predisposing factors: nitrous oxide use, rheumatoid arthritis, anticoagulation, lidocain lubricant. Nevertheless, it should be mentioned that some of these factors were described in a single case report. In addition, difficult insertion may predispose the disorder.14 Mechanisms of injury for isolated hypoglossal involvement include: compression injury caused by pressure of the laryngoscope Macintosh blade on the lateral border of the base of tongue while inserting an endotracheal tube,4 stretch neuropraxia caused by positional change of head or neck,17 and inflammation of surrounding tissue due to minimal trauma caused by the laryngeal mask, endotracheal tube or the Macintosh blade. Generally, complete recovery is made within 6 months – a progressive process that may correspond to compression injury.8
Conclusion
Our patient history and physical examination did not reveal a direct burn injury to the tongue tissue. Exclusion of possible causes is mandatory in a multi-trauma patient. In this case, head and neck CT angiography produced no pathological findings on examination of the intracranial circulation and great vessels of the neck. Radiology findings did not reveal fractures or skeletal pathology along the course of the CN XII. Complete blood count was taken on the day the symptom was presented and results were within normal limits. Vital signs follow-up did not show temperature variation (hyperthermia or hypothermia). In light of this, an infectious cause is less likely. In accordance with this patient’s clinical picture and physical examination, we suspected the nerve injury to be peripheral, distal to the point at which C1 fibers join CN XII. We conclude by exclusion, that nerve paralysis in the present case was probably due to direct nerve injury caused by recurrent endotracheal tube insertion.
Our case suggests the possibility that frequent airway manipulation over a short period of time might have contributed to hypoglossal nerve injury. A health care unit that treats patients who require recurrent intubations, such as burn patients, should avoid inappropriate airway manipulations that may lead to this injury.
The majority of hypoglossal paralysis cases associated with isolated intubation are transient, with an estimated recovery period of 1-6 months.8 In the case of our patient, one month after diagnosis, there were no pathological findings under neurological examination and he had normal hypoglossal nerve function at discharge. The patient required no further evaluation.
References
- 1.Drouet A, Straboni JP, Gunepin FX. Paralysis of the hypoglossal nerve after orotracheal intubation for general anesthesia. Ann Fr Anesth Reanim. 1999;18:811–2. doi: 10.1016/s0750-7658(00)88462-2. [DOI] [PubMed] [Google Scholar]
- 2.Venkatesh B, Walker D. Hypoglossal neuropraxia following endotracheal intubation. Anaesth Intensive Care. 1997;25:699–700. doi: 10.1177/0310057X9702500635. [DOI] [PubMed] [Google Scholar]
- 3.King C, Street MK. Twelfth cranial nerve paralysis following use of a laryngeal mask airway. Anaesthesia. 1994;49:786–7. doi: 10.1111/j.1365-2044.1994.tb04452.x. [DOI] [PubMed] [Google Scholar]
- 4.Bachmann G, Streppel M. Hypoglossal nerve paralysis after endonasal paranasal sinus operation in intubation narcosis. Laryngorhinootologie. 1996;75:623–4. doi: 10.1055/s-2007-997646. [DOI] [PubMed] [Google Scholar]
- 5.Reier CE. Bleeding, dysphagia, dysphonia, dysarthria, severe sore throat, and possible recurrent laryngeal, hypoglossal, and lingual nerve injury associated with routine laryngeal mask airway management: Where is the vigilance? Anesthesiology. 2004;101:1241–2. doi: 10.1097/00000542-200411000-00034. author reply 1242-4. [DOI] [PubMed] [Google Scholar]
- 6.Sommer M, Schuldt M, Runge U, Gielen-Wijffels S, Marcus MA. Bilateral hypoglossal nerve injury following the use of the laryngeal mask without the use of nitrous oxide. Acta Anaesthesiol Scand. 2004;48:377–8. doi: 10.1111/j.0001-5172.2004.0332.x. [DOI] [PubMed] [Google Scholar]
- 7.Cinar SO, Seven H, Cinar U, Turgut S. Isolated bilateral paralysis of the hypoglossal and recurrent laryngeal nerves (bilateral tapia’s syndrome) after transoral intubation for general anesthesia. Acta Anaesthesiol Scand. 2005;49:98–9. doi: 10.1111/j.1399-6576.2004.00553.x. [DOI] [PubMed] [Google Scholar]
- 8.Tesei F, Poveda LM, Strali W, Tosi L, Magnani G, Farneti G. Unilateral laryngeal and hypoglossal paralysis (tapia’s syndrome) following rhinoplasty in general anaesthesia: Case report and review of the literature. Acta Otorhinolaryngol Ital. 2006;26:219–21. [PMC free article] [PubMed] [Google Scholar]
- 9.Yelken K, Guven M, Kablan Y, Sarikaya B. Isolated unilateral hypoglossal nerve paralysis following open septoplasty. Br J Oral Maxillofac Surg. 2008;46:308–9. doi: 10.1016/j.bjoms.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Rhee YG, Cho NS. Isolated unilateral hypoglossal nerve palsy after shoulder surgery in beach-chair position. J Shoulder Elbow Surg. 2008;17:28–30. doi: 10.1016/j.jse.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 11.Hung NK, Lee CH, Chan SM, Yeh CC, Cherng CH, Wong CS, et al. Transient unilateral hypoglossal nerve palsy after orotracheal intubation for general anesthesia. Acta Anaesthesiol Taiwan. 2009;47:48–50. doi: 10.1016/S1875-4597(09)60022-9. [DOI] [PubMed] [Google Scholar]
- 12.Lopes G, Denoel C, Desuter G, Docquier MA. Two cases of isolated unilateral paralysis of hypoglossal nerve after uncomplicated orotracheal intubation. Acta Anaesthesiol Belg. 2009;60:191–3. [PubMed] [Google Scholar]
- 13.Trujillo L, Anghelescu D, Bikhazi G. Unilateral hypoglossal nerve injury caused by a laryngeal mask airway in an infant. Paediatr Anaesth. 2011;21:708–9. doi: 10.1111/j.1460-9592.2011.03572.x. [DOI] [PubMed] [Google Scholar]
- 14.Umapathy N, Eliathamby TG, Timms MS. Paralysis of the hypoglossal and pharyngeal branches of the vagus nerve after use of a LMA and ETT. Br J Anaesth. 2001;87:322. [PubMed] [Google Scholar]
- 15.King C, Street MK. Twelfth cranial nerve paralysis following use of a laryngeal mask airway. Anaesthesia. 1999;49:786–7. doi: 10.1111/j.1365-2044.1994.tb04452.x. [DOI] [PubMed] [Google Scholar]
- 16.Hanumanthaiah D, Masud S, Ranganath A. Inferior alveolar nerve injury with laryngeal mask airway: A case report. J Med Case Reports. 2011;5:122. doi: 10.1186/1752-1947-5-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with the ProSeal laryngeal mask airway: A case report and review of the literature. Br J Anaesth. 2005;95:420–3. doi: 10.1093/bja/aei187. [DOI] [PubMed] [Google Scholar]
- 18.Thompson EO, Smoker WR. Hypoglossal nerve palsy: A segmental approach. Radiographics. 1994;14:939–58. doi: 10.1148/radiographics.14.5.7991825. [DOI] [PubMed] [Google Scholar]
- 19.Schwacha MG, Chaudry IH. The cellular basis of post-burn immunosuppression: Macrophages and mediators. Int J Mol Med. 2002;10:239–43. [PubMed] [Google Scholar]
- 20.Schwacha MG. Macrophages and post-burn immune dysfunction. Burns. 2003;29:1–14. doi: 10.1016/s0305-4179(02)00187-0. [DOI] [PubMed] [Google Scholar]


