Summary
Deep and extensive burns of lower extremities present a difficult challenge to healthcare professionals. After debridement, bones, tendons or joints are frequently exposed and cannot be covered by simple autografts. Moreover, in the case of major burns, damage to the surrounding areas of skin and the severity of the patient’s overall condition, often count against using pedicled or microsurgical flaps. In dealing with such complex wounds, which are difficult to treat, several authors have recommended the combined use of Integra® and negative pressure wound therapy (NPWT). They emphasize that NPWT eliminates wound exudate, promotes neovascularisation and cell migration through the Integra® matrix while increasing its stability and adherence to the wound bed, as well as decreasing the time needed for its total integration. The case presented here is of a patient with major third-degree flame burns to the lower extremities. After debridement, the external and internal malleolus bilaterally became exposed as well as the partially debrided tendons (Achilles, extensor digitorum longus, long and short peroneus, anterior and posterior tibialis). After ruling out the use of local or microsurgical flaps due to the patient’s poor general condition and the presence of burns debrided to the fascia over both lower extremities, we elected to manage the patient with a combined treatment using Integra® and NPWT. After three weeks of treatment, the surface layer of the Integra® matrix was replaced with autografts. Due to partial loss of the skin grafts, a second autograft was needed. At present the patient is completely healed; he can walk with full flexion-extension of both ankles.
Keywords: burns, Integra®, negative pressure wound therapy
Abstract
Brûlures profondes et étendues des membres inférieurs du corp présentent un défi difficile pour les professionnels de la santé. Après débridement, les os, les tendons ou les articulations sont fréquemment exposés et ne peuvent pas être couverts par des simples autogreffes. En outre, dans le cas des grands brûlés, des dommages aux régions avoisinantes de la peau et de la gravité de l’état général du patient, contre-indiquent l’utilisation des lambeaux pédiculés ou de la microchirurgie. Dans le traitement de ces plaies complexes, qui sont difficiles à traiter, plusieurs auteurs ont recommandé l’utilisation combinée de l’Integra® et de la thérapie par pression négative (TPN). Ils soulignent que la TPN élimine les exsudats de la plaie, et favorise la néovascularisation et la migration des cellules à travers la matrice Integra®, tout en augmentant la stabilité et le collement du lit de la plaie et en réduisant le temps nécessaire à son intégration totale. Nous présentons le cas d’un patient avec des grandes brûlures au troisième degré causées par des flammes aux membres inférieurs. Après debridement, les malléoles externe et interne bilatérales sont devenues exposées ainsi que les tendons partiellement débridés (Achille, extenseur des orteils, long et court péronier latéral, muscles jambiers antérieurs et postérieurs). Après avoir exclu l’utilisation des lambeaux locaux ou de la microchirurgie en raison des brûlures débridées jusqu’à l’aponévrose sur les deux extrémités inférieures et le mauvais état général du patient, nous avons choisi de gérer le patient avec un traitement combiné de l’Integra® et de la TPN. Après trois semaines de traitement, la couche de surface de la matrice Integra® a été remplacée par des autogreffes. En raison de la perte partielle des greffes de peau, une deuxième autogreffe était nécessaire. Actuellement, le patient est complètement guéri; il peut marcher avec flexion et extension des deux chevilles.
Introduction
Deep and extensive wounds are very difficult to treat,1-3 particularly if the patient’s overall condition is severely negatively impacted. Such is the case in patients with multiple injuries and, more specifically, in patients with multiple injuries connected with major burns. Quite often, these burns result in exposure of tendons, bones, and joint structures that cannot be covered by simple autografts. In such cases, it is advisable to cover the exposed structures using both pedicled and microsurgical flaps. However, deep and widespread injury of an extremity may contraindicate the use of pedicled flaps. The poor overall condition of some major burn patients may also be incompatible with long surgeries or with surgical procedures requiring hemodynamic stability, such as microsurgical free tissue transfer.1,2,4 In these instances, the use of new techniques can save an extremity that would otherwise be doomed to amputation.3,5,6 Two examples of these new techniques are Integra® and NPWT.
Integra® (Johnson&Johnson, Hamburg, Germany) was first described in 1981 by Burke and Yanas, and was approved by the Food and Drug Administration in 1996. It is a completely noncellular artificial bilayer matrix. The outer silicone layer simulates the epidermis, serving to control moisture loss and prevent invasion by microorganisms. The inner layer is a three-dimensional porous matrix of cross-linked collagen and glycosaminoglycan of bovine origin that acts as a dermal regeneration template. Following migration of endothelial cells and fibroblasts, this results in the formation of a neodermis that, histologically and functionally, is very similar to normal dermis. This product has a very low antigenicity and degrades in a controlled period of time, being replaced by the host’s collagen, without any added scar tissue.4 Other benefits of Integra® include minimal pain and discomfort, optimal scarring and the ability to cover lesions without sacrificing the patient’s other tissues.6 However, as with most new interventions, it does have some drawbacks: it has a failure rate of approximately 25%,4,7 and a second surgical procedure is required after three to four weeks to replace the superficial silicone layer with thin autografts, thus lengthening hospital stay and increasing costs.1,2,4,7
Vacuum therapy, initially introduced by V.A.C., Kinetic Concepts, Inc., San Antonio, Texas, is the use of subatmospheric pressure as non-invasive adjuvant therapy to treat wounds. It is said to increase blood supply to the wound and to induce the formation of granulation tissue, thus stimulating the contraction phase of the wound and the proliferation of fibroblasts and endothelial cells. It also decreases bacterial load, eliminates exudate and slough, reduces oedema and swelling, and maintains an optimal moist environment for proper healing.4,7 However, its disadvantages include the need for prolonged treatment in order to obtain good results and the frequent friability and instability of the resulting granulation tissue.3
Combined Integra® and NPWT has resulted in reports of excellent dermal regeneration,1-3,5,6 with a 90% success rate compared to only 75% when Integra® is used alone,2,4,5,7 and probably in a shorter period of time. In vitro studies have shown that NPWT increases mitosis and the migration of endothelial cells in the Integra® matrix. This is an extremely important effect given that angiogenesis is key to the integration of dermal equivalents. Mechanical stress exerted on the Integra® also increases vacuolisation and cell proliferation, as well as tissue expansion, and allows for greater contact and stability of the Integra® with the wound bed. Finally, the negative pressure alone eliminates exudate and reduces bacterial colonization, thereby increasing the viability of the dermal equivalent that is extremely sensitive to infection.1
We present the case of a patient with major, third-degree burns to both lower extremities, as well as to the head and neck, requiring debridement of the leg fasciae, decortication of the four malleoli and partial debridement of the short and long peroneus tendons, anterior and posterior tibialis tendons, extensor digitorum longus, and the Achilles tendons. The depth and extension of the leg burns prevented the use of local grafts to cover both ankles and dorsal sides of the feet. The poor overall condition of the patient also contraindicated the use of microsurgical techniques. Given these factors and despite the acute phase of the wounds, we elected to use Integra® and NPWT.
Case report
A 60-year-old man with no pathological-medical history of interest was referred to us from his local hospital after suffering flame burns provoked by an ethylene gas explosion in his workplace. The patient had suffered third-degree burns to 50% of his total body surface area (including head, neck and both lower extremities), severe lid burns and smoke inhalation. He required prophylactic intubation and escharotomies of the lower extremities (Figs. 1A, 1B).
Fig. 1 - (A). Burn on lower extremities with escharotomies performed.

Fig. 1 - (B). Detail of burn on right internal malleolus.
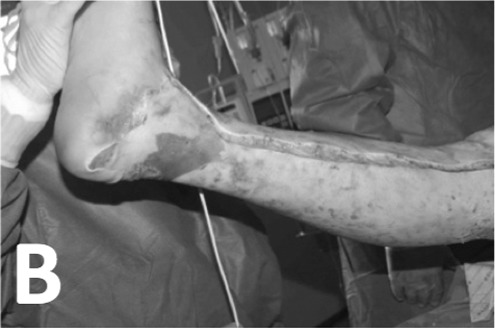
On the sixth day post-injury, we performed autografting after tangential excision of the face and neck, and debridement under tourniquet control down to the fascia of the left lower extremity. The right leg was similarly debrided and grafted on the eleventh day.
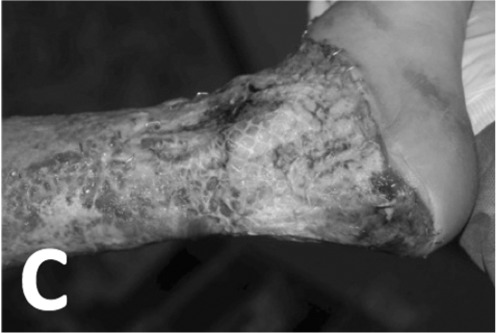
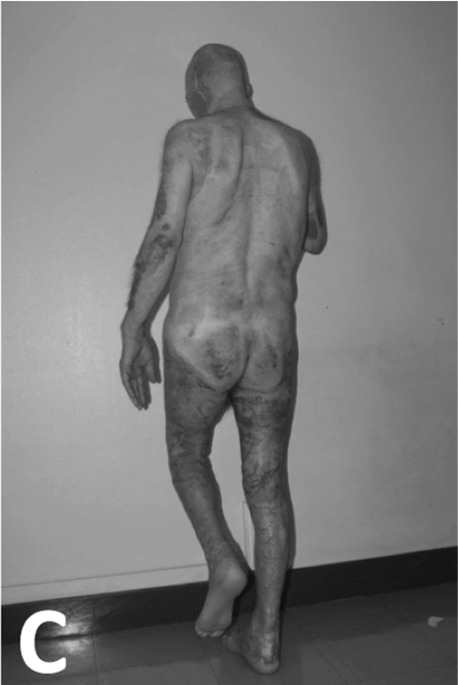
On the eighteenth day we performed skin grafting after debridement of the ankles down to the fascia and tangential debridement of the tourniquet areas over both thighs. Failed grafting of the ankles resulted in exposed necrotic tendons and malleolar periosteum (Fig. 1C).
Fig. 1 - (C). Necrosis of soft tissues of left ankle.
Different treatment options were considered. However, pedicled or perforated flaps were not feasible in this case due to the size of the defect to be covered and the fact that the potential flap donor sites had been previously debrided down to the fascia, precluding any other fascio- cutaneous flaps.
Free flaps were of doubtful indication due to the patient’s poor overall condition, complicated by sepsis from Acinetobacter baumanii and multi-resistant Pseudomonas aeruginosa.
After reviewing the literature regarding defects of this type, we elected to perform an exhaustive debridement of the necrotic tissues. This included chiselling the four malleoli and partial debridement of the anterior and posterior tibialis tendons, the short and long peroneus tendons, the common extensor digitorum and the Achilles tendons. The defect was then immediately covered with Integra®, which in turn was covered with Acticoat® (Smith&Nephew, London, UK), a nanocrystalline silver wound dressing to control the local Pseudomonas infection. Continuous NPWT at 80 mmHg was applied using the Renasys® system (Smith&Nephew, London, UK) (Fig. 2).
Fig. 2. Vacuum system over Integra® applied to both ankles.

Cleansing and dressing changes were performed twice a week. Surface swab cultures were also taken, which remained positive for multi-resistant Pseudomonas aeruginosa (Figs. 3A, 3B).
Fig. 3 - (A). Appearance of ankles 7 days after Integra® and NPWT.

Fig. 3 - (B). Appearance of ankles 13 days after Integra® and NPWT.

After three weeks of combined Integra® and NPWT, the superficial silicone layer was removed and the bed was covered with mesh autografts. After ten days, the skin graft had not taken completely and the wounds eventually required additional NPWT, and re-grafting three weeks later for healing (Fig. 3C).
Fig. 3 - (C). Grafts on eleventh day after surgery with partial take.
The patient was extubated 58 days after admission and moved to the in-patient floor on the 67th day. Rehabilitation, sitting and walking were started on the 55th, 61st and 72nd days respectively (Figs. 3D, 4A).
Fig. 3 - (D). After three weeks of additional vacuum therapy.
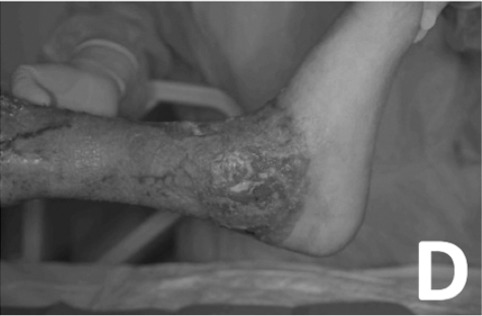
Fig. 4 - (A). Appearance of wounds 7 days after re-grafting.

The patient was discharged from the hospital on the 92nd day after the injury, to continue rehabilitation with periodical check-ups in out-patient consultations, and to start acupressure therapy.
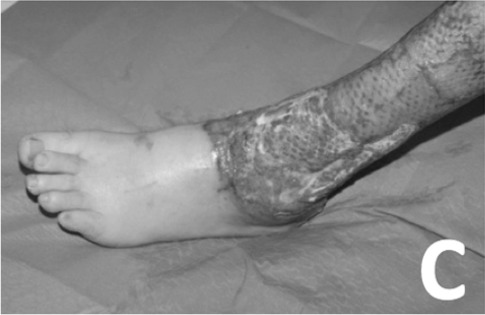
Aesthetic and functional results of the burn affected ankles are satisfactory (Figs. 4B, 4C).
Fig. 4 - (B). Detail of ankle wounds one month after discharge from hospital.

Fig. 4 - (C). Appearance and functioning of the ankle wounds one month after discharge from hospital.
Results & Discussion
Combined treatment using Integra® and NPWT allowed complete coverage of all the affected structures that could not otherwise have been covered by simple skin grafts, with preservation of joint function.
NPWT secured stability and adherence of the dermal equivalent to the surgical bed while it eliminated exudate caused the by Pseudomonas aeruginosa infection that would have been detrimental to the dermal regeneration template. Thanks to its antimicrobial effect, the use of Acticoat® dressing may have been helpful in enabling the Integra® product to take despite continuous positive swab cultures.
Although it has been reported that the combined use of Integra® and NPWT could reduce the time between the first dermal regeneration template and subsequent skin grafting to just 10 days2, we relied on general recommendations and clinical signs before applying the skin grafts.
The success rate of the combined treatment is reported to be 90%, although this figure results from observation of non-acute cases with small wounds. No findings with regards to heavily infected wounds have been reported. Despite the fact that our patient's skin graft did not take completely, and that prolonged treatment was necessary with re-grafting to achieve healing, the successful final outcome fully justifies the adoption of this method of treatment for selected acute wounds that are infected and problematic.
Conclusion
Deep and extensive burns of lower extremities present a challenge to healthcare professionals. In most cases, the best coverage is achieved by performing pedicled, perforator, propeller or microsurgical flaps. However, in some patients, due to inadequate adjacent tissues or their poor overall condition, these surgical techniques are not always feasible. In such cases, conservative therapies not are a valid option to cover bone, tendon and joint structures. Combined treatment with a dermal equivalent (Integra®) and NPWT leads to positive results and offers better conditions for healing than any single method.
Acknowledgments
Conflict of interest. All authors declare that there are no conflicts of interest and no commercial interest in the products, companies or treatments mentioned in this article.
References
- 1.Baldwin C, Potter M, Clyton E, Irvine L, Dye J. Topical negative pressure stimulates endothelial migration and proliferation: A suggested mechanism for improvement integration of Integra. Annals of Plastic Surgery. 2009 Jan;62:92–96. doi: 10.1097/SAP.0b013e31817762fd. [DOI] [PubMed] [Google Scholar]
- 2.Molnar JA, Defranzo AJ, Hadaegh A, Morykwas MJ, Shen P, Argenta LC. Acceleration of Integra incorporation in complex defects with subatmospheric pressure. Plastic and Reconstructive Surgery. 2004;113:1339. doi: 10.1097/01.prs.0000112746.67050.68. [DOI] [PubMed] [Google Scholar]
- 3.Lee LF, Porch JV, Spenler CW, Garner WL. Integra in lower extremity reconstruction after burn injury. Plastic and Reconstructive Surgery. 2008 Apr;121:1256. doi: 10.1097/01.prs.0000304237.54236.66. [DOI] [PubMed] [Google Scholar]
- 4.Jeschke MG, Rose C, Angele P, Füchtmeier B, Nerlich MN, Bolder U. Development of new reconstructive techniques: Use of Integra in combination with fibrin glue and negative-pressure for reconstruction of acute and chronic wounds. Plastic and Reconstructive Surgery. 2004 Feb;113:525–30. doi: 10.1097/01.PRS.0000100813.39746.5A. [DOI] [PubMed] [Google Scholar]
- 5.Stiefel D, Schiestl CM, Meuli M. The positive effect of negative pressure: Vacuum-assisted fixation of Integra artificial skin for reconstructive surgery. Journal of Pediatric Surgery. 2009;44:575–80. doi: 10.1016/j.jpedsurg.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Jeng JC, Fidler PE, Sokolich JC, Jaskille AM, Khan S, White PM, Stree JH, Light TD, Jordan MH. Seven years´ experience with Integra as a reconstructive tool. Journal of Burn Care Research. 2007;28:120–6. doi: 10.1097/BCR.0b013E31802CB83F. [DOI] [PubMed] [Google Scholar]
- 7.Park CA, Defranzo AJ, Marks MW, Molnar JA. Outpatient reconstruction using Integra and subatmospheric pressure. Annals of Plastic Surgery. 2009 Feb;62:164–9. doi: 10.1097/SAP.0b013e31817d87cb. [DOI] [PubMed] [Google Scholar]
- 8.Angirasa AK, Willrich A, Cooper B, Stuck R. Combining bioengineered human dermal replacement and multilayered compression dressings to manage ulcers in a person with diabetes mellitus: A case study. Ostomy Wound Management. 2006 May;52:60–4. [PubMed] [Google Scholar]


