Abstract
Importance
Methodological limitations compromise the validity of U.S. nutritional surveillance data and the empirical foundation for formulating dietary guidelines and public health policies.
Objectives
Evaluate the validity of the National Health and Nutrition Examination Survey (NHANES) caloric intake data throughout its history, and examine trends in the validity of caloric intake estimates as the NHANES dietary measurement protocols evolved.
Design
Validity of data from 28,993 men and 34,369 women, aged 20 to 74 years from NHANES I (1971–1974) through NHANES 2009–2010 was assessed by: calculating physiologically credible energy intake values as the ratio of reported energy intake (rEI) to estimated basal metabolic rate (BMR), and subtracting estimated total energy expenditure (TEE) from NHANES rEI to create ‘disparity values’.
Main Outcome Measures
1) Physiologically credible values expressed as the ratio rEI/BMR and 2) disparity values (rEI–TEE).
Results
The historical rEI/BMR values for men and women were 1.31 and 1.19, (95% CI: 1.30–1.32 and 1.18–1.20), respectively. The historical disparity values for men and women were −281 and −365 kilocalorie-per-day, (95% CI: −299, −264 and −378, −351), respectively. These results are indicative of significant under-reporting. The greatest mean disparity values were −716 kcal/day and −856 kcal/day for obese (i.e., ≥30 kg/m2) men and women, respectively.
Conclusions
Across the 39-year history of the NHANES, EI data on the majority of respondents (67.3% of women and 58.7% of men) were not physiologically plausible. Improvements in measurement protocols after NHANES II led to small decreases in underreporting, artifactual increases in rEI, but only trivial increases in validity in subsequent surveys. The confluence of these results and other methodological limitations suggest that the ability to estimate population trends in caloric intake and generate empirically supported public policy relevant to diet-health relationships from U.S. nutritional surveillance is extremely limited.
Introduction
The rise in the population prevalence of obesity has focused attention on U.S. nutritional surveillance research and the analysis of trends in caloric energy intake (EI). Because these efforts provide the scientific foundation for many public health policies and food-based guidelines, poor validity in dietary measurement protocols can have significant long-term implications for our nation’s health.
In the U.S., population-level estimates of EI are derived from data collected as part of the National Health and Nutrition Examination Survey (NHANES), a complex, cross-sectional sample of the U.S. population. The primary method used in NHANES to approximate EI is the 24-hour dietary recall interview (24HR) [1]. The data collected are based on the subject’s self-reported, retrospective perceptions of food and beverage consumption in the recent past. To calculate EI estimates, these subjective data are translated into nutrient food codes and then assigned numeric energy (i.e., caloric) values from food and nutrient databases. Prior to 2001–2002, the NHANES relied upon databases of varying quality and composition for the post-hoc conversion of food and beverage consumption (24HR) data into energy values [2]–[5]. After 2001–2002, the NHANES and the U.S. Department of Agriculture’s (USDA) Continuing Survey of Food Intakes by Individuals were integrated into the “What We Eat in America” program [6], and the translation process was standardized via use of successive versions of the USDA’s National Nutrient Database for Standard Reference (NNBS) [7].
Misreporting
Given the indirect, pseudo-quantitative nature of the method (i.e., assigning numeric values to subjective data without objective corroboration), nutrition surveys frequently report a range of energy intakes that are not representative of the respondents’ habitual intakes [8], and estimates of EI that are physiologically implausible (i.e., incompatible with survival) have been demonstrated to be widespread [9]–[11]. For example, in a group of “highly educated” participants, Subar et al. (2003) demonstrated that when total energy expenditure (TEE) via doubly labeled water (DLW) was compared to reported energy intake (rEI), the raw correlations between TEE and rEI were 0.39 for men and 0.24 for women. Men and women underreported energy intake by 12–14% and 16–20%, respectively. The level of underreporting increased significantly after correcting for the weight gain of the sample over the study period [9], and underreporting was greater for fat than for protein, thereby providing additional support for the well-documented occurrence of the selective misreporting of specific macronutrients (e.g., fat and sugars) [12]–[15]. These results are consistent with earlier work, in which the correlations between DLW-derived TEE and seven 24HR and the average of two seven-day dietary recalls were 0.33 and 0.30, respectively [16].
Because the NHANES collected dietary data over the period in which the population prevalence of obesity was increasing, these data have been used (despite the widely acknowledged issues [17]) to examine the association of trends in EI with increments in mean population body mass index (BMI) and rates of obesity (e.g., [18]–[20]). Given that implausible rEI values and the misreporting of total dietary intake render the relationships between dietary factors, BMI and other indices of health ambiguous [21], and diminish the usefulness of nutrition data as a tool to inform public health policy, this report examines the validity of U.S. nutrition surveillance EI data from NHANES I (1971–1974) through NHANES 2010 (nine survey periods) using two protocols: the ratio of reported energy intake (rEI) to basal metabolic rate (rEI/BMR) [22], [23] and the disparity between rEI and estimated total energy expenditure (TEE) from the Institute of Medicine’s (IOM) predictive equations [24].
Methods
Population
Data were obtained from the National Health and Nutrition Examination Surveys for the years 1971–2010 [1]. The NHANES is a complex multi-stage, cluster sample of the civilian, non-institutionalized U.S. population conducted by the Centers for Disease Control and Prevention (CDC). The National Center for Health Statistics ethics review board approved protocols and written informed consent was obtained from all NHANES participants.
Inclusion Criteria
The study sample was limited to adults aged ≥20 and <74 years at the time of the NHANES in which they participated, and had a body mass index (BMI) ≥18 kg/m2, and with complete data on age, sex, height, weight, and dietary energy intake.
Dietary Data
Estimates of EI were obtained from a single 24HR from each of the nine NHANES study periods [1]. Energy content of the self-reported food consumption was determined by NHANES using nutrient databases based on previous versions of the USDA National Nutrient Database for Standard Reference (NNDS) [7].
Determination of Physiologically Credible rEI Values
The ratio of rEI to BMR (rEI/BMR) <1.35 [22], [23], [25] was used to determine EI values that were implausible. BMR was estimated via the Schofield predictive equations [26]. The <1.35 cut-off for implausible EI values was used because “it is highly unlikely that any normal, healthy free-living person could habitually exist at a PAL [i.e., TEE/BMR] of less than 1.35” [22].
It is important to note that the <1.35 cut-off does not assess all forms of misreporting (e.g., over-reporting). To avoid the confounding effects of potential over-reporting, all rEI/BMR values >2.40 [27] were excluded from analyses of underreporting. One form of misreporting that neither cut-off addresses is the underreporting of EI from a high caloric intake associated with elevated levels of physical activity.
Disparity of the rEI and Estimated Total Energy Expenditure (TEE)
In 2002, the IOM used datasets derived from studies using DLW to create factorial equations to estimate energy requirements for the US population. IOM TEE values were subtracted from the NHANES rEI to calculate disparity values. Negative values indicate underreporting.
IOM Equations for Predicting TEE Normal Weight (NW) Adults only (≥19years)
Equation 1 Men: TEE = 864– (9.72×age [y])+PA*×(14.2×weight [kg]+503×height[m]) (±202).
Equation 2 Women: TEE = 387– (7.31×age [y]+PA*×(10.8×weight [kg]+660.7×height[m]) (±156).
* Physical activity (PA) values were 1.12 and 1.14 for NW men and women, respectively. The use of these values assumes a physical activity level (PAL) of ≥1.4 and <1.6, which is indicative of a “low active” population [24].
IOM Equations for Predicting TEE Overweight (OW)/Obese (OB) Adults Only (≥19 years)
Equation 3 Men: TEE = 1086– (10.1×age [y])+PA*×(13.7×weight [kg]+416×height [m]).
Equation 4 Women: TEE = 448– (7.95×age [y])+PA*×(11.4×weight [kg]+619×height [m]).
*PA values were 1.12 and 1.16 for OW/OB men and women, respectively. The use of these values assumes a physical activity level (PAL) of ≥1.4 and <1.6, which is indicative of a “low active” population [24].
Note: age (years); weight (kg); height (m; meters); BMI = body mass index, (kg/m2), IOM = Institute of Medicine; TEE = total energy expenditure.
Anthropometry [1]
Body mass was measured to ±0.1 kg. Height was measured to ±0.1 cm. BMI was calculated as weight (kg)/height (m)2. The sample was divided into three standard BMI categories: BMI ≥18 kg/m2 and <25 kg/m2 were normal weight (NW), BMI between 25 kg/m2 and 29.9 kg/m2 were overweight (OW), and ≥30 kg/m2 were obese (OB).
Statistical Analyses
Data processing and statistical analyses were performed using SAS®, V 9.2 and SPSS® V.19 in 2012–2013. Analyses accounted for the NHANES’ complex survey design via the incorporation of stratification, clustering and post-stratification weighting to maintain a nationally representative sample for each survey period. All analyses included adjusted means, and α <0.05 (2-tailed) was used to identify statistical significance.
Results
Examination of Underreporting via rEI/BMR
Table 1 depicts the rEI/BMR values for men and women from NHANES I through NHANES 2009–2010. rEI was from NHANES 24HR data and BMR was calculated using the Schofield predictive equations [26]. Values <1.35 are considered implausible and indicative of underreporting.
Table 1. rEI/BMR values for all men and women from NHANES I through NHANES 2009–2010.
| Reported Energy Intake (rEI)/Basal Metabolic Rate (BMR) rEI/BMR >1.35 = plausible US Men & Women (20–74 years); NHANES I - NHANES 2009–2010 | ||||||
| NHANESSurvey Year | Sex | Estimate rEI/RMR (mean)* | Standard Error | 95% Confidence Interval | rEI Value Plausible Y = Yes N = No | |
| Lower | Upper | |||||
| NHANES I | Men (n = 4652) | 1.30 | 0.012 | 1.28 | 1.32 | N |
| Women (n = 7709) | 1.10 | 0.010 | 1.08 | 1.12 | N | |
| NHANES II | Men (n = 5236) | 1.28 | 0.010 | 1.26 | 1.30 | N |
| Women (n = 6006) | 1.08 | 0.008 | 1.06 | 1.09 | N | |
| NHANES III | Men (n = 6122) | 1.36b | 0.011 | 1.34 | 1.39 | Y |
| Women (n = 7127) | 1.22a | 0.009 | 1.20 | 1.24 | N | |
| NHANES I999–00 | Men (n = 1600) | 1.31 | 0.018 | 1.27 | 1.34 | N |
| Women (n = 1886) | 1.23a | 0.016 | 1.19 | 1.26 | N | |
| NHANES 2001–2002 | Men (n = 1782) | 1.31 | 0.015 | 1.28 | 1.34 | N |
| Women (n = 2029) | 1.24a | 0.011 | 1.22 | 1.26 | N | |
| NHANES 2003–2004 | Men (n = 1671) | 1.32 | 0.013 | 1.30 | 1.35 | Y |
| Women (n = 1838) | 1.23a | 0.018 | 1.20 | 1.27 | N | |
| NHANES 2005–2006 | Men (n = 1749) | 1.34c | 0.013 | 1.31 | 1.36 | Y |
| Women (n = 1998) | 1.21a | 0.014 | 1.18 | 1.24 | N | |
| NHANES 2007–08 | Men (n = 2154) | 1.27 | 0.017 | 1.24 | 1.30 | N |
| Women (n = 2306) | 1.19a | 0.020 | 1.15 | 1.23 | N | |
| NHANES 2009–2010 | Men (n = 2319) | 1.29 | 0.013 | 1.26 | 1.31 | N |
| Women (n = 2532) | 1.20a | 0.007 | 1.18 | 1.21 | N | |
| All Surveys | Men (n = 27285) | 1.31 | 0.005 | 1.30 | 1.32 | N |
| Women (n = 33431) | 1.19 | 0.005 | 1.18 | 1.20 | N | |
All estimates are weighted means.
Significantly different from NHANES I at p≤0.001 (Women).
Significantly different from NHANES I at p≤0.001 (Men).
Significantly different from NHANES I at p≤0.05 (Men).
Note: rEI was from NHANES 24HR data and BMR was calculated using the Schofield predictive equations. [26] Values <1.35 are considered implausible and indicative of underreporting. TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
Values <1.35 are not physiologically credible.
As Table 1 depicts, the 95% confidence intervals (CI) suggest that all mean rEI values for women and six of nine mean rEI values for men were apparently implausible.
Table 2 depicts the rEI/BMR index for all women by BMI categories from NHANES I through NHANES 2009–2010.
Table 2. rEI/BMR index for all women by BMI categories from NHANES I through NHANES 2009–2010.
| Reported Energy Intake (rEI)/Basal Metabolic Rate (BMR) rEI/BMR >1.35 = plausible US Women (20–74 years); NHANES I - NHANES 2009–2010 | ||||||
| NHANESSurvey Year | BMI Category | EstimaterEI/BMR(Mean)* | Standard Error | 95% Confidence Interval | rEI Value Plausible Y = Yes N = No | |
| Lower | Upper | |||||
| NHANES I | Normal (n = 4222) | 1.20 | 0.013 | 1.18 | 1.23 | N |
| Overweight (n = 2028) | 1.00 | 0.012 | 0.98 | 1.02 | N | |
| Obese (n = 1459) | 0.88 | 0.014 | 0.86 | 0.91 | N | |
| NHANES II | Normal (n = 3171) | 1.18 | 0.010 | 1.16 | 1.20 | N |
| Overweight (n = 1671) | 0.98 | 0.012 | 0.96 | 1.01 | N | |
| Obese (n = 1164) | 0.89 | 0.012 | 0.87 | 0.91 | N | |
| NHANES III | Normal (n = 2661) | 1.32 | 0.014 | 1.30 | 1.35 | Y |
| Overweight (n = 2150) | 1.18 | 0.019 | 1.14 | 1.22 | N | |
| Obese (n = 2316) | 1.07 | 0.015 | 1.04 | 1.10 | N | |
| NHANES 1999–2000 | Normal (n = 555) | 1.36 | 0.020 | 1.32 | 1.40 | Y |
| Overweight (n = 572) | 1.19 | 0.033 | 1.12 | 1.25 | N | |
| Obese (n = 759) | 1.12 | 0.030 | 1.06 | 1.18 | N | |
| NHANES 2001–2002 | Normal (n = 630) | 1.38 | 0.018 | 1.35 | 1.42 | Y |
| Overweight (n = 639) | 1.26 | 0.028 | 1.21 | 1.32 | N | |
| Obese (n = 760) | 1.08 | 0.012 | 1.05 | 1.10 | N | |
| NHANES 2003–2004 | Normal (n = 550) | 1.35 | 0.031 | 1.29 | 1.41 | Y |
| Overweight (n = 546) | 1.19 | 0.027 | 1.14 | 1.25 | N | |
| Obese (n = 742) | 1.15 | 0.026 | 1.10 | 1.20 | N | |
| NHANES 2005–2006 | Normal (n = 615) | 1.34 | 0.026 | 1.29 | 1.39 | Y |
| Overweight (n = 558) | 1.19 | 0.028 | 1.13 | 1.24 | N | |
| Obese (n = 825) | 1.10 | 0.024 | 1.05 | 1.15 | N | |
| NHANES 2007–2008 | Normal (n = 634) | 1.30 | 0.038 | 1.23 | 1.38 | Y |
| Overweight (n = 694) | 1.17 | 0.026 | 1.12 | 1.22 | N | |
| Obese (n = 978) | 1.10 | 0.020 | 1.06 | 1.14 | N | |
| NHANES 2009–2010 | Normal (n = 690) | 1.31 | 0.022 | 1.26 | 1.35 | Y |
| Overweight (n = 745) | 1.23 | 0.024 | 1.18 | 1.28 | N | |
| Obese (n = 1097) | 1.08 | 0.006 | 1.06 | 1.09 | N | |
All estimates are weighted means.
Note: rEI was from NHANES 24HR data and BMR was calculated using the Schofield predictive equations. [26] Values <1.35 are considered implausible and indicative of underreporting. TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
As Table 2 depicts, the 95% CI suggest that in 20 of the 27 measurement categories (i.e., three BMI categories and nine surveys) the rEI values were not in the physiologically plausible range. The overall mean for rEI/BMR values for the total sample of women (n = 33,431) across all NHANES was 1.19 (95% CI: 1.18, 1.20) and therefore not physiologically plausible.
Table 3 depicts the rEI/BMR index for all men by BMI categories from NHANES I through NHANES 2009–2010.
Table 3. rEI/BMR index for all men by BMI categories from NHANES I through NHANES 2009–2010.
| Reported Energy Intake (rEI)/Basal Metabolic Rate (BMR) rEI/BMR >1.35 = plausible US Men (20–74 years); NHANES I - NHANES 2009–2010 | ||||||
| NHANESSurvey Year | BMI Category | Estimate rEI/BMR (Mean)* | Standard Error | 95% Confidence Interval | rEI Value Plausible Y = Yes N = No | |
| Lower | Upper | |||||
| NHANES I | Normal (n = 2115) | 1.41 | 0.016 | 1.38 | 1.44 | Y |
| Overweight (n = 1945) | 1.24 | 0.017 | 1.21 | 1.28 | N | |
| Obese (n = 592) | 1.08 | 0.025 | 1.04 | 1.13 | N | |
| NHANES II | Normal (n = 2431) | 1.37 | 0.009 | 1.35 | 1.39 | Y |
| Overweight (n = 2111) | 1.25 | 0.015 | 1.22 | 1.28 | N | |
| Obese (n = 694) | 1.08 | 0.018 | 1.05 | 1.12 | N | |
| NHANES III | Normal (n = 2275) | 1.47 | 0.018 | 1.43 | 1.50 | Y |
| Overweight (n = 2482) | 1.35 | 0.015 | 1.32 | 1.38 | Y | |
| Obese (n = 1365) | 1.20 | 0.018 | 1.17 | 1.24 | N | |
| NHANES 1999–2000 | Normal (n = 476 ) | 1.42 | 0.020 | 1.38 | 1.46 | Y |
| Overweight (n = 655) | 1.33 | 0.022 | 1.28 | 1.37 | Y | |
| Obese (n = 469) | 1.16 | 0.036 | 1.09 | 1.23 | N | |
| NHANES 2001–2002 | Normal (n = 493) | 1.43 | 0.038 | 1.35 | 1.50 | Y |
| Overweight (n = 774) | 1.32 | 0.017 | 1.29 | 1.36 | Y | |
| Obese (n = 515) | 1.18 | 0.027 | 1.13 | 1.24 | N | |
| NHANES 2003–2004 | Normal (n = 465) | 1.46 | 0.029 | 1.41 | 1.52 | Y |
| Overweight (n = 659) | 1.35 | 0.025 | 1.30 | 1.40 | Y | |
| Obese (n = 547) | 1.18 | 0.035 | 1.11 | 1.24 | N | |
| NHANES 2005–2006 | Normal (n = 413) | 1.51 | 0.030 | 1.45 | 1.57 | Y |
| Overweight (n = 735) | 1.33 | 0.023 | 1.29 | 1.38 | Y | |
| Obese (n = 601) | 1.22 | 0.014 | 1.19 | 1.25 | N | |
| NHANES 2007–2008 | Normal (n = 539) | 1.40 | 0.038 | 1.32 | 1.47 | Y |
| Overweight (n = 835) | 1.29 | 0.017 | 1.26 | 1.32 | N | |
| Obese (n = 790) | 1.15 | 0.019 | 1.12 | 1.19 | N | |
| NHANES 2009–2010 | Normal (n = 563) | 1.38 | 0.027 | 1.33 | 1.44 | Y |
| Overweight (n = 872) | 1.35 | 0.021 | 1.31 | 1.39 | Y | |
| Obese (n = 884) | 1.16 | 0.016 | 1.13 | 1.19 | N | |
All estimates are weighted means.
Note: rEI was from NHANES 24HR data and BMR was calculated using the Schofield predictive equations. [26] Values <1.35 are considered implausible and indicative of underreporting. TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
As shown in Table 3, the 95% CI suggest that in 12 of 27 measurement categories (i.e., three BMI categories and nine surveys), the rEI values were not in the physiologically plausible range. The overall mean value for rEI/BMR for the total sample of men (n = 27,285) across all NHANES was 1.31 (95% CI: 1.30, 1.32), and therefore not in the physiologically plausible range.
Percent of Plausible Reporters
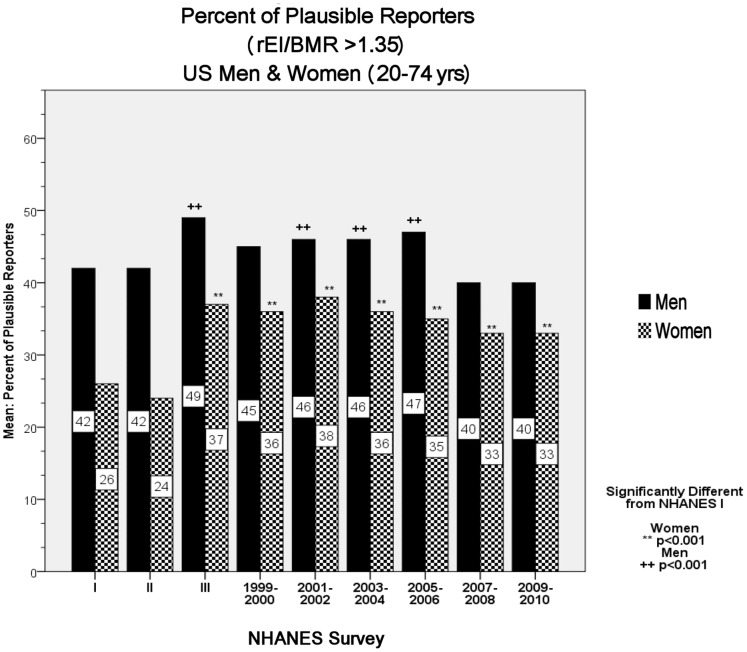
Figure 1 depicts the percent of plausible reporters (i.e., rEI/BMR >1.35) by sex from NHANES I to NHANES 2009–2010.
Figure 1. Percent of plausible reporters (i.e., rEI/BMR >1.35) by sex from NHANES I to NHANES 2009–2010; U.S. Men and women (20–74 years).
As Figure 1 depicts, across the entire study period (i.e., 1971–2010) the majority of respondents did not report plausible rEI values in any survey. When stratified by sex and BMI categories, plausible reporting in OB women ranged from a low of ∼12% in NHANES I and II to a high of 31% in NHANES 2003–2004. At no point in the history of the NHANES did more than 43% of OW and OB women report plausible values. Plausible reporting in NW women ranged from a low of 32% in NHANES II to 52% in NHANES 2001–2002. Plausible rEI values in OB men ranged from a low of 23% in NHANES II to a high of 35% in NHANES 2005–2006. At no point in the history of NHANES did more than 49% of OW and OB men report plausible rEI values.
Disparity between NHANES rEI and IOM TEE
Table 4 depicts the disparity of rEI and TEE for men and women (20–74 years). These values were calculated by subtracting the IOM TEE from the NHANES rEI. Negative values indicate the kilocalorie-per-day (kcal/day) value of underreporting.
Table 4. Disparity of rEI and TEE for men and women (20–74 years).
| Disparity between rEI and IOM TEE US Men & Women (20–74 years) NHANES I – NHANES 2009–2010 | ||||||
| NHANESSurvey Year | Sex | EstimaterEI minus TEE (mean)* | Standard Error | 95% Confidence Interval (CI) | Validity: 95% CI includes zero (Y = Yes, N = No) | |
| Lower | Upper | |||||
| NHANES I | Men (n = 4652) | −290.8 | 20.3 | −330.7 | −250.9 | N |
| Women (n = 7709) | −479.7 | 14.5 | −508.1 | −451.3 | N | |
| NHANES II | Men (n = 5236) | −323.2 | 17.8 | −358.1 | −288.3 | N |
| Women (n = 6006) | −505.8 | 11.6 | −528.4 | −483.1 | N | |
| NHANES III | Men (n = 6122) | −183.3b | 19.1 | −220.8 | −145.7 | N |
| Women (n = 7127) | −325.3a | 13.5 | −351.7 | −298.8 | N | |
| NHANES 1999–2000 | Men (n = 1600) | −285.3 | 37.7 | −359.3 | −211.4 | N |
| Women (n = 1886) | −328.7a | 27.3 | −382.3 | −275.1 | N | |
| NHANES 2001–2002 | Men (n = 1782) | −270.3 | 26.8 | −322.9 | −217.7 | N |
| Women (n = 2029) | −306.0a | 15.5 | −336.3 | −275.6 | N | |
| NHANES 2003–2004 | Men (n = 1671) | −255.6 | 24.7 | −304.0 | −207.3 | N |
| Women (n = 1838) | −308.2a | 27.2 | −361.5 | −254.8 | N | |
| NHANES 2005–2006 | Men (n = 1749) | −232.2 | 25.3 | −281.8 | −182.6 | N |
| Women (n = 1998) | −347.5a | 20.8 | −388.4 | −306.6 | N | |
| NHANES 2007–08 | Men (n = 2154) | −355.0 | 32.1 | −417.9 | −292.0 | N |
| Women (n = 2306) | −379.4d | 28.5 | −435.3 | −323.5 | N | |
| NHANES 2009–2010 | Men (n = 2319) | −330.9 | 22.7 | −375.4 | −286.4 | N |
| Women (n = 2532) | −366.9a | 9.8 | −386.1 | −347.7 | N | |
| All Surveys | Men (n = 27285) | −281.4 | 9.1 | −299.3 | −263.5 | N |
| Women (n = 33431) | −364.6 | 7.0 | −378.3 | −351.0 | N | |
All estimates are weighted means.
Significantly different from NHANES I at p≤0.001 (Women).
Significantly different from NHANES I at p≤0.001 (Men).
Significantly different from NHANES I at p≤0.05 (Men).
Significantly different from NHANES I at p≤0.05 (Women).
Note: TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
These values were calculated by subtracting the IOM TEE from the NHANES rEI. Negative values indicate the kilocalorie-per-day (kcal/day) value of underreporting.
As Table 4 depicts, in no survey group (i.e., men & women in 9 surveys) does the 95% CI for the disparity between rEI and TEE include zero. This suggests that that underreporting of EI occurred in both men and women, and across all surveys. The overall mean value for the disparity of rEI and IOM TEE for the total sample of women (n = 33,431) across all NHANES was −365 kcal/day (95% CI: −378, −351), or ∼18% of TEE, and for the total sample of men (n = 27,285) was −281 kcal/day (95% CI: −299, −264), or ∼10% of TEE.
When stratified by sex and BMI categories (see Tables 5 & 6), the disparities between rEI and TEE in OB women ranged from −856 kcal/day (95% CI: −902, −810), an underreporting of ∼41% of TEE, to −477 kcal/day (95% CI: −560, −394), an underreporting of 20% of TEE. The disparities between rEI and TEE in OB men ranged from −717 kcal/day (95% CI: −790, −643) in NHANES II to −464 kcal/day (95% CI: −527, −401) underreporting of 25% and 15%, respectively.
Table 5. Disparity between rEI and the TEE for women (20–74 years) by BMI categories.
| Disparity between rEI and IOM TEE; US Women by BMI categories (20–74 years) NHANES I – NHANES 2009–2010 | ||||||
| NHANESSurvey Year | BMI Category | Estimate rEI minus TEE (mean) | Standard Error | 95% Confidence Interval (CI) | Validity: 95% CI includes zero (Y = Yes, N = No) | |
| Lower | Upper | |||||
| NHANES I | Normal n = 4222) | −316.0 | 17.7 | −350.8 | −281.2 | N |
| Overweight (n = 2028) | −595.3 | 17.7 | −629.9 | −560.6 | N | |
| Obese (n = 1459) | −856.0 | 23.5 | −902.0 | −809.9 | N | |
| NHANES II | Normal (n = 3171) | −351.6 | 13.7 | −378.5 | −324.8 | N |
| Overweight (n = 1671) | −617.6 | 17.1 | −651.1 | −584.1 | N | |
| Obese (n = 1164) | −850.6 | 19.5 | −888.9 | −812.3 | N | |
| NHANES III | Normal (n = 2661) | −158.6 | 17.7 | −193.3 | −123.9 | N |
| Overweight (n = 2150) | −357.1 | 26.5 | −409.1 | −305.2 | N | |
| Obese (n = 2316) | −594.2 | 22.6 | −638.5 | −549.9 | N | |
| NHANES 1999–2000 | Normal (n = 555) | −106.0 | 27.2 | −159.3 | −52.6 | N |
| Overweight (n = 572) | −359.6 | 48.8 | −455.3 | −264.0 | N | |
| Obese (n = 759) | −530.1 | 50.2 | −628.5 | −431.6 | N | |
| NHANES 2001–2002 | Normal (n = 630) | −74.0 | 21.7 | −116.6 | −31.4 | N |
| Overweight (n = 639) | −239.6 | 38.7 | −315.5 | −163.7 | N | |
| Obese (n = 760) | −591.1 | 20.5 | −631.4 | −550.9 | N | |
| NHANES 2003–2004 | Normal (n = 550) | −116.3 | 39.2 | −193.2 | −39.4 | N |
| Overweight (n = 546) | −339.0 | 37.7 | −413.0 | −265.0 | N | |
| Obese (n = 742) | −477.1 | 42.2 | −560.0 | −394.2 | N | |
| NHANES 2005–2006 | Normal (n = 615) | −131.1 | 34.1 | −198.0 | −64.3 | N |
| Overweight (n = 558) | −342.8 | 38.0 | −417.4 | −268.3 | N | |
| Obese (n = 825) | −567.3 | 38.7 | −643.2 | −491.3 | N | |
| NHANES 2007–2008 | Normal (n = 634) | −173.2 | 52.1 | −275.4 | −71.0 | N |
| Overweight (n = 694) | −374.1 | 35.8 | −444.4 | −303.7 | N | |
| Obese (n = 978) | −567.3 | 33.2 | −632.5 | −502.1 | N | |
| NHANES 2009–2010 | Normal (n = 690) | −173.0 | 27.8 | −227.5 | −118.4 | N |
| Overweight (n = 745) | −288.9 | 34.0 | −355.7 | −222.2 | N | |
| Obese (n = 1097) | −590.5 | 14.0 | −617.8 | −563.1 | N | |
Note: BMI = body mass index; TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
These values were calculated by subtracting the IOM TEE from the NHANES rEI for each respondent. Negative values indicate the kcal/day value of underreporting.
Table 6. Disparity between rEI and the TEE for all men (20–74 years) by BMI categories.
| Disparity between rEI and IOM TEE; US Men by BMI categories (20–74 years) NHANES I – NHANES 2009–2010 | ||||||
| NHANESSurvey Year | BMI Category | Estimate rEI minus TEE (mean) | Standard Error | 95% Confidence Interval (CI) | Validity: 95% CI includes zero (Y = Yes, N = No) | |
| Lower | Upper | |||||
| NHANES I | Normal (n = 2115) | −96.3 | 26.8 | −149.0 | −43.6 | N |
| Overweight (n = 1945) | −374.7 | 30.8 | −435.1 | −314.2 | N | |
| Obese (n = 592) | −702.1 | 49.7 | −799.7 | −604.5 | N | |
| NHANES II | Normal (n = 2431) | −178.7 | 15.9 | −209.9 | −147.6 | N |
| Overweight (n = 2111) | −367.6 | 27.0 | −420.5 | −314.6 | N | |
| Obese (n = 694) | −716.5 | 37.3 | −789.8 | −643.3 | N | |
| NHANES III | Normal (n = 2275) | −8.8 | 31.1 | −69.8 | 52.2 | Y |
| Overweight (n = 2482) | −191.5 | 27.9 | −246.3 | −136.7 | N | |
| Obese (n = 1365) | −494.4 | 38.0 | −569.0 | −419.9 | N | |
| NHANES 1999–2000 | Normal (n = 476 ) | −87.2 | 34.8 | −155.6 | −18.8 | N |
| Overweight (n = 655) | −221.8 | 41.5 | −303.3 | −140.2 | N | |
| Obese (n 469) | −590.9 | 76.8 | −741.6 | −440.2 | N | |
| NHANES 2001–2002 | Normal (n = 493) | −64.1 | 63.1 | −188.0 | 59.9 | Y |
| Overweight (n = 774) | −229.2 | 29.5 | −287.1 | −171.3 | N | |
| Obese (n = 515) | −527.5 | 55.3 | −636.1 | −418.9 | N | |
| NHANES 2003–2004 | Normal (n = 465) | −6.8 | 47.3 | −99.6 | 86.0 | Y |
| Overweight (n = 659) | −175.4 | 46.9 | −267.4 | −83.4 | N | |
| Obese (n = 547) | −549.8 | 72.0 | −691.1 | −408.5 | N | |
| NHANES 2005–2006 | Normal (n = 413) | 70.4 | 53.0 | −33.7 | 174.5 | Y |
| Overweight (n = 735) | −222.4 | 39.7 | −300.3 | −144.4 | N | |
| Obese (n = 601) | −464.2 | 32.1 | −527.2 | −401.2 | N | |
| NHANES 2007–2008 | Normal (n = 539) | −117.9 | 64.8 | −245.2 | 9.3 | Y |
| Overweight (n = 835) | −286.7 | 31.3 | −348.1 | −225.2 | N | |
| Obese (n = 790) | −608.0 | 42.2 | −690.8 | −525.2 | N | |
| NHANES 2009–2010 | Normal (n = 563) | −154.4 | 43.5 | −239.8 | −69.1 | N |
| Overweight (n = 872 ) | −178.9 | 42.1 | −261.5 | −96.4 | N | |
| Obese (n = 884) | −590.9 | 32.9 | −655.4 | −526.4 | N | |
Note: BMI = body mass index; TEE = estimated total energy expenditure; IOM = Institute of Medicine; rEI = reported energy intake; BMR = Basal Metabolic Rate calculated via Schofield predictive equation.
These values were calculated by subtracting the estimated IOM TEE from the NHANES rEI for each respondent. Negative numbers indicate the kcal/day value of underreporting.
Trends in Underreporting
After the removal of over-reporters, both protocols, that is rEI/BMR (Figure1) and the disparity between rEI and IOM TEE ( Table 4) exhibited significant decreases in underreporting from NHANES II and NHANES III (p<0.001). There were significant negative linear trends for both men and women in changes in underreporting total caloric intake from NHANES I to NHANES 2009–2010 (rEI/BMR: p<0.001, and disparity: p = 0.028).
Trends in Over-reporting
Across the study period, approximately 4.9% of men and 2.9% of women reported rEI/BMR values suggestive of over-reporting (i.e., rEI/BMR >2.4) with no significant trends. The greatest increase in the percentage of over-reporters between survey periods occurred from NHANES II to NHANES III, with men increasing from 4.1% to 6.4%, and women from 1.7% to 3.4% (both p<0.001). The greatest absolute percentage of over-reporters was in NHANES III, with 6.4% of men over-reporting and NHANES 2003–2004, with 3.9% of women over-reporting.
Discussion
Validity of NHANES EI Data
Our results suggest that across the 39-year history of U.S. nutrition surveillance research, rEI data on the majority of respondents (67.3% of women and 58.7% of men) were not physiologically plausible. The historical average rEI/BMR values for all men and women were 1.31 and 1.19 respectively ( Table 1 ). These values are indicative of substantial underreporting. The expected average values for healthy, free living men and women are ∼1.55, with a range of >1.35 to <2.40 [23], [27]. In no survey did at least 50% of the respondents report plausible EI values ( Figure 1 ). These data are consistent with previous research demonstrating that the misreporting of EI in nutrition surveys is widespread [9], [11], [28]–[34]. Goldberg et al. (1991) demonstrated that in 37 studies across 10 countries, >65% of the mean rEI/BMR values were below the study-specific plausibility cut-off [23]. In addition to the extensive underreporting in our sample, 4.9% of men and 2.9% of women reported rEI/BMR values suggestive of over-reporting (i.e., rEI/BMR >2.40).
Disparity between NHANES rEI and IOM Derived TEE
Throughout the study period (i.e., 1971–2010) the disparity between rEI and TEE values were large and variable across BMI and sex categories suggesting substantial systematic biases in underreporting ( Tables 4, 5, 6). The overall mean disparity values for men and women were −281 kcal/day and −365 kcal/day, respectively. The greatest mean disparity values were −717 kcal/day (25% of TDEE) and −856 kcal/day (41% of TEE) in OB men and women, respectively.
Trends in the Validity and Inferences from NHANES rEI Data
As depicted in Tables 1 and 2, and Figure 1, there were large decreases in underreporting between NHANES II and NHANES III. This is clearly evidenced by the increase in rEI/BMR index ( Table 1), the large and significant increase in the percent of plausible reporters (Figure1), and the reduction in the disparity between NHANES rEI and NAS/IOM EER ( Table 4). This decrement in underreporting between NHANES II and subsequent surveys across all sex and BMI categories is likely the result of improvements in survey protocols for NHANES III, such as the inclusion of more days of dietary recall (i.e., weekends), automated multi-pass methodology, and increased staff training and quality control (see [35]), The extent of these improvements is notable; for example, the percentage of OB women reporting implausible values decreased from ∼88% in NHANES II to 74% in NHANES III.
These changes in measurement protocols led to an apparent increase in mean rEI values that has been reported as an actual increase in population-level EI despite caveats that the “Interpretation of trends in energy and nutrient intakes is difficult when methodologic changes occur between surveys” [36]. Nevertheless, Briefel and Johnson state (without caveat) in their abstract, “During the 30-year period, mean energy intake increased among adults…” [37]. The data presented in the present report refute this inference. When the NHANES dietary measurement protocols were altered after NHANES II, the improved method captured a higher percentage of actual intakes. The apparent increase in mean rEI was merely an artifact of improved measurement protocols and not indicative of a true increase in caloric consumption. Despite this fact, the apparent increase has been regularly published and uncritically accepted as a true upward trend in caloric consumption (e.g., [37], [38]) and the cause of the obesity epidemic (e.g., [39], [40]).
Changes in Underreporting and Public Policy Recommendations
In addition to the ubiquity of misreporting, there is strong evidence that the reporting of ‘socially undesirable’ (e.g., high fat and/or high sugar) foods has changed as the prevalence of obesity has increased [12]–[15]. Additionally, research has demonstrated that interventions emphasizing the importance of ‘healthy’ behaviors may lead to increased misreporting as participants alter their reports to reflect the adoption of the ‘healthier’ behaviors independent of actual behavior change [17], [41]. It appears that lifestyle interventions “teach” participants the socially desirable or acceptable responses [17], [42]. As such, the ubiquity of public health messages to ‘eat less and exercise more’ may induce greater levels of misreporting and may explain the recent downward bias in both self-reported EI [20] and body weight [17], [43], especially given that social desirability bias is often expressed in the underreporting of calorically dense foods [44].
Selective misreporting of specific macronutrients has important ramifications for epidemiological research and nutrition surveillance. Heitmann and Lissner (2005) demonstrated that the selective misreporting of dietary fat by groups at an increased risk of chronic non-communicable diseases may result in an overestimated association between fat consumption and disease [45]. If the potentially negative effects of high-fat diets are overestimated due to selective misreporting, current recommendations for fat intake may be overly conservative [45].
Additional Systematic Biases of Nutrition Surveillance Data
In addition to known sources of systematic reporting error, there are numerous sources of systematic bias in nutrition surveillance research protocols that are not addressed via our data. Another potentially large source of error is the translation of food and beverage consumption data (e.g. 24HR) into nutrient energy values via nutrient composition databases. The accuracy of this translation relies on a number of assumptions that are rarely justified. As cited earlier, research on misreporting shows that reports do not accurately reflect the quantity or number of foods consumed, and are not representative of usual intakes [12]–[15], [46]–[50]. Given that the basic methodological assumptions are violated, it is not surprising that research has demonstrated that food data to nutrient energy conversions are “riddled with potential pitfalls at all stages” that “hamper the interpretability of the results” [51]–[53], and represent a major source of systematic error in national nutrition surveillance efforts [2].
Throughout its history, the NHANES has relied upon databases of varying quality and composition for the post-hoc conversion of food and beverage consumption (i.e., 24HR) data into energy values [2]–[5], [53]. This makes the analysis of trends extremely complex because the nutrient energy (i.e., caloric) values in the databases varied considerably over time [54], [55]. Additionally, research has demonstrated that the energy content of restaurant food (and especially fast-food outlets) vary significantly when compared to the industry values used in the NNDS [56], and an internal quality review of NHANES 2003–2004 data led to ∼400 substantive changes in nutrient and energy values. [57]. The result of these limitations are discussed in detail elsewhere, see [4], [5], [58].
As with the improvements in the NHANES survey protocols, the progressive alterations to the nutrient database combined with changes in the types of foods that are available for consumption led to artifactual differences in nutrient and energy consumption estimates that frustrate efforts to examine trends in caloric consumption [58]. To account for these changes, researchers must maintain the real differences in the composition of foods while correcting for artifactual differences attributable to improvements in the quality of nutrient data [58]. Given the lack of comprehensive crossover studies and metrics for adjustment as the food and nutrient databases evolved, papers examining trends in caloric consumption must be treated with skepticism [51], [58].
Commercially Prepared Foods and Meals Away From Home
One of the most prominent systematic errors from 24HR data-to-nutrient energy conversions is due to the increased reliance on the food service industry and the substantial rise in meals eaten ‘away from home’[59]–[61]. As stated previously, the vast majority of foods and beverages in the NNDS have not been evaluated empirically and research has demonstrated that the energy and macro/micro nutrient content of commercially prepared foods varies significantly compared to the industry values used in the NNDS [56]. When foods or commodities are not in the database, substitutions are necessitated. For these interpolations to be accurate, the analogues must be similar in composition to the consumed food or beverage. This is extremely difficult to perform in practice because no two foods or commodities are identical, and local vs. imported foods/commodities differ significantly. For example, in survey data collection, knowledge of the specific preparation and cut of beef are essential since the energy content of generic beef substitutions may differ dramatically (e.g., 166 kcals per 100 grams in round steak to 257 kcals in top sirloin [62]) [63], [64]. Given these realities, USDA estimates of caloric consumption may be increasingly inaccurate as the number of food and beverages supplied by the commercial sector expands rapidly.
Recent research has attempted to quantify the changes in consumer packaged foods and beverages, and their impact on the American diet [65]. Nevertheless, these efforts suffer from the same limitations as all food data-to-nutrient energy value conversions via nutrient composition databases. Additionally, the translation of “as-purchased” foods and beverages (using information from the commercial sector) to “as-consumed” energy and macro/micronutrient content for national surveillance relies on the accurate quantification of food preparation and waste [65]. Unfortunately, these data are limited and highly variable [52], [66]. In a report from the USDA’s Economic Research Service, Muth et al. (2011) state that the current data are incomplete and overstate actual consumption because the level of “documentation of food losses… ranged from little to none for estimates at the retail and customer levels.” [67]. These results clearly demonstrate the conceptual and methodological complexity of translating food and beverage purchases into nutrient energy and macro/micronutrient intake in the context of a rapidly evolving food supply.
Methods of Adjustment for Systematic Biases
There are various methods that attempt to improve estimates of caloric consumption derived from self-reported dietary intake [32], [68]–[72]. While these methods may improve the shape of the distribution of the estimates, none can address the significant systematic biases described in this report. For example, the National Research Council and the Iowa State University methods provide significantly improved estimates of the shape of the distribution, but do not substantially improve estimates of mean energy intake (10–15% underestimation) or protein consumption (6–7% underestimation) [70]. 291.
Strengths and Limitations
A strength of the present study was the use of the established rEI/BMR method for the determination of physiologically implausible EI values. We used a liberal cutoff (i.e., <1.35) that is below the study-specific theoretical cutoff for our smallest sub-group (i.e., n >400). The use of the more conservative cutoff of rEI/BMR <1.50 recommended by Goldberg et al., (1991) [22] increased underreporting by 10% in women and 7% in men across all surveys. A second strength was the use of a rEI/BMR >2.4 for the elimination of potential over-reporters to correct the limitations of previous research [29].
Finally, the use of the IOM factorial equations for estimating TEE for specific subgroups (i.e., OW & OB respondents) in the calculation of disparity values is a significant strength. The results of this additional protocol demonstrated significant underreporting in all surveys, and that the disparity values closely paralleled the implausible values in 15 of the 18 sub-groups (i.e., men & women in 9 surveys). The close agreement between these two dissimilar protocols increases confidence in our results and conclusions.
A potential limitation to our analysis was the use of the Schofield predictive equation for estimating BMR. The Schofield predictive equations may overestimate BMR in some populations [73], [74]. If the Schofield equation overestimated BMR, a greater percentage of survey respondents would be classified as under-reporters. To address this potential limitation, we performed the analyses using the Mifflin equation [75], which has been validated in OW and OB populations such as the U.S [74]. The results of those analyses were similar to those obtained using the Schofield equation, with substantial underreporting (>50%) in all surveys, significant trends in changes in underreporting, and a small increase in over-reporting. To remain consistent with past research on implausible rEI and underreporting [29], [33], we chose to present the results from the Schofield predictive equations.
Conclusions
Throughout its history, NHANES dietary measurement protocols have failed to provide accurate estimates of the habitual caloric consumption of the U.S. population. Furthermore, successive changes to the nutrient databases used for the 24HR data-to-energy conversations and improvements in measurement protocols make it exceedingly difficult to discern temporal patterns in caloric intake that can be related to changes in population rates of obesity. As such, there are no valid population-level data to support speculations regarding trends in caloric consumption and the etiology of the obesity epidemic. Because under-reporting and physiologically implausible rEI values are a predominant feature of U.S. nutritional surveillance, the ability to generate empirically supported public policy and dietary guidelines relevant to the obesity epidemic based on these data is extremely limited.
Acknowledgments
The data used in this study are available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm
Funding Statement
This study was funded via an unrestricted research grant from The Coca-Cola Company. The sponsor of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
References
- 1.CDC (2012) National Health and Examination Survey. Atlanta, GA: Centers for Disease Control and Prevention.
- 2. Blair D (1992) Dietary methodology issues related to energy balance measurement for NHANES III. Vital & Health Statistics 4: 43–50. [PubMed] [Google Scholar]
- 3. Phillips KM, Patterson KY, Rasor AS, Exler J, Haytowitz DB, et al. (2006) Quality-control materials in the USDA National Food and Nutrient Analysis Program (NFNAP). Anal Bioanal Chem 384: 1341–1355. [DOI] [PubMed] [Google Scholar]
- 4.Weihrauch JL (1992) Problems in Energy Calculations. In: USDA, editor; Baltimore, Maryland. Human Nutrition Informatuion Service, HNIS.
- 5. Perloff B, Ahuja JK (1998) Development and maintenance of nutrient databases for national dietary surveys. Public Health Rev 26: 43–47. [PubMed] [Google Scholar]
- 6. Dwyer J, Picciano MF, Raiten DJ (2003) Collection of food and dietary supplement intake data: What We Eat in America-NHANES. J Nutr 133: 590S–600S. [DOI] [PubMed] [Google Scholar]
- 7.USDA (2012) National Agricultural Library National Nutrient Database for Standard Reference.
- 8. Black AE, Cole TJ (2001) Biased over- or under-reporting is characteristic of individuals whether over time or by different assessment methods. J Am Diet Assoc 101: 70–80. [DOI] [PubMed] [Google Scholar]
- 9. Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, et al. (2003) Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol 158: 1–13. [DOI] [PubMed] [Google Scholar]
- 10. Schoeller DA (1995) Limitations in the assessment of dietary energy intake by self-report. Metabolism 44: 18–22. [DOI] [PubMed] [Google Scholar]
- 11. Huang TTK, Roberts SB, Howarth NC, McCrory MA (2005) Effect of Screening Out Implausible Energy Intake Reports on Relationships between Diet and BMI. Obesity Research 13: 1205–1217. [DOI] [PubMed] [Google Scholar]
- 12. Goris AH, Westerterp-Plantenga MS, Westerterp KR (2000) Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr 71: 130–134. [DOI] [PubMed] [Google Scholar]
- 13. Scagliusi FB, Polacow VO, Artioli GG, Benatti FB, Lancha AH Jr (2003) Selective underreporting of energy intake in women: magnitude, determinants, and effect of training. J Am Diet Assoc 103: 1306–1313. [DOI] [PubMed] [Google Scholar]
- 14. Lissner L, Heitmann BL, Bengtsson C (2000) Population studies of diet and obesity. Br J Nutr 83 Suppl 1S21–24. [DOI] [PubMed] [Google Scholar]
- 15. Heitmann BL, Lissner L, Osler M (2000) Do we eat less fat, or just report so? Int J Obes Relat Metab Disord 24: 435–442. [DOI] [PubMed] [Google Scholar]
- 16. Hebert JR, Ebbeling CB, Matthews CE, Hurley TG, Ma Y, et al. (2002) Systematic errors in middle-aged women's estimates of energy intake: comparing three self-report measures to total energy expenditure from doubly labeled water. Ann Epidemiol 12: 577–586. [DOI] [PubMed] [Google Scholar]
- 17. Schoeller DA, Thomas D, Archer E, Heymsfield SB, Blair SN, et al. (2013) Self-report-based estimates of energy intake offer an inadequate basis for scientific conclusions. Am J Clin Nutr 97: 1413–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Austin GL, Ogden LG, Hill JO (2011) Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971–2006. The American Journal of Clinical Nutrition 93: 836–843. [DOI] [PubMed] [Google Scholar]
- 19. Skinner AC, Steiner MJ, Perrin EM (2012) Self-reported energy intake by age in overweight and healthy-weight children in NHANES, 2001–2008. Pediatrics 130: e936–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford ES, Dietz WH (2013) Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr. [DOI] [PMC free article] [PubMed]
- 21. McCrory MA, McCrory MA, Hajduk CL, Roberts SB (2002) Procedures for screening out inaccurate reports of dietary energy intake. Public Health Nutr 5: 873–882. [DOI] [PubMed] [Google Scholar]
- 22. Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, et al. (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45: 569–581. [PubMed] [Google Scholar]
- 23. Black AE, Goldberg GR, Jebb SA, Livingstone MB, Cole TJ, et al. (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 2. Evaluating the results of published surveys. Eur J Clin Nutr 45: 583–599. [PubMed] [Google Scholar]
- 24.IOM (2005) Report of the Panel on Macronutrients: Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). Washington D.C.: The National Academies Press.
- 25.Livingstone MBE, Black AE (2003) Markers of the Validity of Reported Energy Intake. 895S–920S. [DOI] [PubMed]
- 26. Schofield WN, Schofield C, James WPT (1985) Basal metabolic rate–review and prediction, with an annotated bibliography of source material. Human nutrition Clinical nutrition 39C: 1–96. [PubMed] [Google Scholar]
- 27.FAO/WHO/UNU (2004) Human energy requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. Rome World Health Organization, Food and Agriculture Organization of the United Nations, United Nations University.
- 28. Heerstrass DW, Ocke MC, Bueno-de-Mesquita HB, Peeters PH, Seidell JC (1998) Underreporting of energy, protein and potassium intake in relation to body mass index. Int J Epidemiol 27: 186–193. [DOI] [PubMed] [Google Scholar]
- 29. Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K (1997) Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr 65: 1203S–1209S. [DOI] [PubMed] [Google Scholar]
- 30. Johansson L, Solvoll K, Bjorneboe GE, Drevon CA (1998) Under- and overreporting of energy intake related to weight status and lifestyle in a nationwide sample. Am J Clin Nutr 68: 266–274. [DOI] [PubMed] [Google Scholar]
- 31. Okubo H, Sasaki S (2004) Underreporting of energy intake among Japanese women aged 18–20 years and its association with reported nutrient and food group intakes. Public Health Nutr 7: 911–917. [DOI] [PubMed] [Google Scholar]
- 32.Yanetz R, Kipnis V, Carroll RJ, Dodd KW, Subar AF, et al.. (2008) Using biomarker data to adjust estimates of the distribution of usual intakes for misreporting: application to energy intake in the US population. J Am Diet Assoc 108: 455–464; discussion 464. [DOI] [PubMed]
- 33. Ferrari P, Slimani N, Ciampi A, Trichopoulou A, Naska A, et al. (2002) Evaluation of under- and overreporting of energy intake in the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr 5: 1329–1345. [DOI] [PubMed] [Google Scholar]
- 34. Becker W, Foley S, Shelley E, Gibney M (1999) Energy under-reporting in Swedish and Irish dietary surveys: implications for food-based dietary guidelines. Br J Nutr 81 Suppl 2S127–131. [DOI] [PubMed] [Google Scholar]
- 35.McDowell M, Briefel RR, Buzzard IM, Gardner SN, Warren RA, et al. (1994) The Dietary Collection System–An Automated Interview and Coding System for NHANES III; accessed 11/12/2012; available @ CDC website: www.cdc.gov/nchs/tutorials/dietary/additionalresources/NNDB94.pdf.Centers for Disease Control and Prevention, National Center for Health Statistics.
- 36.McDowell MA (1994) Update on the Third National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention, National Center for Health Statistics. Available: www.nutrientdataconf.org/pastconf/ndbc19/6-5_mcdowell.pdf. Accessed 2012 Jun 11.
- 37. Briefel RR, Johnson CL (2004) Secular trends in dietary intake in the United States. Annu Rev Nutr 24: 401–431. [DOI] [PubMed] [Google Scholar]
- 38. CDC (2004) Trends in intake of energy and macronutrients–United States, 1971–2000. MMWR Morb Mortal Wkly Rep 53: 80–82. [PubMed] [Google Scholar]
- 39. Finkelstein EA, Ruhm CJ, Kosa KM (2005) Economic causes and consequences of obesity. Annu Rev Public Health 26: 239–257. [DOI] [PubMed] [Google Scholar]
- 40. Cutler DM, Glaeser EL, Shapiro JM (2003) Why Have Americans Become More Obese? Journal of Economic Perspectives v17: 93–118. [Google Scholar]
- 41. Taber DR, Stevens J, Murray DM, Elder JP, Webber LS, et al. (2009) The effect of a physical activity intervention on bias in self-reported activity. Ann Epidemiol 19: 316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Racette SB, Schoeller DA, Kushner RF, Neil KM (1995) Exercise enhances dietary compliance during moderate energy restriction in obese women. Am J Clin Nutr 62: 345–349. [DOI] [PubMed] [Google Scholar]
- 43. Shiely F, Hayes K, Perry IJ, Kelleher CC (2013) Height and weight bias: the influence of time. PLoS One 8: e54386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hebert JR, Clemow L, Pbert L, Ockene IS, Ockene JK (1995) Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int J Epidemiol 24: 389–398. [DOI] [PubMed] [Google Scholar]
- 45. Heitmann BL, Lissner L (2005) Can adverse effects of dietary fat intake be overestimated as a consequence of dietary fat underreporting? Public Health Nutr 8: 1322–1327. [DOI] [PubMed] [Google Scholar]
- 46. Goris AH, Westerterp KR (1999) Underreporting of habitual food intake is explained by undereating in highly motivated lean women. J Nutr 129: 878–882. [DOI] [PubMed] [Google Scholar]
- 47. Johansson G, Wikman A, Ahren AM, Hallmans G, Johansson I (2001) Underreporting of energy intake in repeated 24-hour recalls related to gender, age, weight status, day of interview, educational level, reported food intake, smoking habits and area of living. Public Health Nutr 4: 919–927. [DOI] [PubMed] [Google Scholar]
- 48. Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, et al. (1992) Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med 327: 1893–1898. [DOI] [PubMed] [Google Scholar]
- 49. McGowan MJ, Harrington KE, Kiely M, Robson PJ, Livingstone MB, et al. (2001) An evaluation of energy intakes and the ratio of energy intake to estimated basal metabolic rate (EI/BMRest) in the North/South Ireland Food Consumption Survey. Public Health Nutr 4: 1043–1050. [DOI] [PubMed] [Google Scholar]
- 50. Trabulsi J, Schoeller DA (2001) Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab 281: E891–899. [DOI] [PubMed] [Google Scholar]
- 51. Kelly A, Becker W, Helsing E (1991) Food Balance Sheets. In: Food and health data: Their use in nutirition policy-making: WHO Regional Publications, European Series, No Becker W, Helsing E, editors. 34: 39–48. [PubMed] [Google Scholar]
- 52. Kohlmeier L (1991) Problems and pitfalls of food-to-nutrient conversion. In: Food and health data: Their use in nutirition policy-making: WHO Regional Publications, European Series, No Becker W, Helsing E, editors. 34: 73–84. [PubMed] [Google Scholar]
- 53. Kelly A, Becker W (1991) Nutrition information systems and data quality requirements. In: Food and health data: their use in nutrition policy-making: WHO Regional Publications, European Series, No Becker W, Helsing E, editors. 34: 15–24. [PubMed] [Google Scholar]
- 54. Ahuja JKC, Goldman JD, Perloff BP (2006) The effect of improved food composition data on intake estimates in the United States of America. Journal of Food Composition and Analysis 19 Supplement: S7–S13 [Google Scholar]
- 55. Ahuja JKC, Lemar L, Goldman JD, Moshfegh AJ (2009) The impact of revising fats and oils data in the US Food and Nutrient Database for Dietary Studies. Journal of Food Composition and Analysis 22 Supplement: S63–S67 [Google Scholar]
- 56. Urban LE, McCrory MA, Dallal GE, Das SK, Saltzman E, et al. (2012) Accuracy of stated energy contents of restaurant foods. Jama 306: 287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ahuja JKC, Perloff BP (2008) Quality control procedures for the USDA Food and Nutrient Database for Dietary Studies nutrient values. Journal of Food Composition and Analysis 21 Supplement: S119–S124 [Google Scholar]
- 58. Guenther PM, Perloff BP, Vizioli TL Jr (1994) Separating fact from artifact in changes in nutrient intake over time. J Am Diet Assoc 94: 270–275. [DOI] [PubMed] [Google Scholar]
- 59. Guthrie JF, Lin BH, Frazao E (2002) Role of food prepared away from home in the American diet, 1977–78 versus 1994–96: changes and consequences. J Nutr Educ Behav 34: 140–150. [DOI] [PubMed] [Google Scholar]
- 60. Stewart H, Yen ST (2004) Changing household characteristics and the away-from-home food market: a censored equation system approach. Food Policy 29: 643–658. [Google Scholar]
- 61.Stewart H, Blisard N, Bhuyan, Nayga RMJ (2012) The Demand for Food Away From Home. Full-Service or Fast Food? In: USDA, editor. Electronic Report from the Economic Research Service: Economic Research Service.
- 62.USDA (2011) Nutrient Data Set for Retail Beef Cuts. Beltsvile, MD: Nutrient Data Laboratory (NDL), Agricultural Research Service, U.S. Department of Agriculture.
- 63. Smith AM, Harris KB, Haneklaus AN, Savell JW (2011) Proximate composition and energy content of beef steaks as influenced by USDA quality grade and degree of doneness. Meat Sci 89: 228–232. [DOI] [PubMed] [Google Scholar]
- 64. O'Neil CE, Zanovec M, Keast DR, Fulgoni VL 3rd, Nicklas TA (2011) Nutrient contribution of total and lean beef in diets of US children and adolescents: National Health and Nutrition Examination Survey 1999–2004. Meat Sci 87: 250–256. [DOI] [PubMed] [Google Scholar]
- 65. Slining MM, Ng SW, Popkin BM (2013) Food companies' calorie-reduction pledges to improve U.S. diet. Am J Prev Med 44: 174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.FAO (2001) Food Balance Sheets: A handbook. Rome, Italy: Food and Agriculture Organization of the United Nations.
- 67.Muth MK, Karns SA, Nielsen SJ, Buzby JC, Wells HF (2011) Consumer-Level Food Loss Estimates and Their Use in the ERS Loss-Adjusted Food Availability Data. USDA Economic Research Service, Technical Bulletin (TB-1927). 123 p. [Google Scholar]
- 68. Nusser SM, Carriquiry AL, Dodd KW, Fuller WA (1996) A Semiparametric Transformation Approach to Estimating Usual Daily Intake Distributions. Journal of the American Statistical Association 91: 1440–1449. [Google Scholar]
- 69. Dodd KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, et al. (2006) Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc 106: 1640–1650. [DOI] [PubMed] [Google Scholar]
- 70. Freedman LS, Midthune D, Carroll RJ, Krebs-Smith S, Subar AF, et al. (2004) Adjustments to improve the estimation of usual dietary intake distributions in the population. J Nutr 134: 1836–1843. [DOI] [PubMed] [Google Scholar]
- 71. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, et al. (2010) A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 29: 2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.IOM (2003) Dietary Reference Intakes: Applications in Dietary Planning: The National Academies Press. [PubMed]
- 73. Frankenfield D, Roth-Yousey L, Compher C (2005) Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc 105: 775–789. [DOI] [PubMed] [Google Scholar]
- 74. Frankenfield DC, Rowe WA, Smith JS, Cooney RN (2003) Validation of several established equations for resting metabolic rate in obese and nonobese people. J Am Diet Assoc 103: 1152–1159. [DOI] [PubMed] [Google Scholar]
- 75. Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, et al. (1990) A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 51: 241–247. [DOI] [PubMed] [Google Scholar]