Abstract
Hypophysitis is an important differential diagnosis for a pituitary mass, especially in young women at the end of or shortly after pregnancy. It commonly results in hypopituitarism and can be differentiated from adenoma on MRI. Typical MRI characteristics of hypophysitis are symmetry, loss of posterior bright spot, intense and homogeneous gadolinium enhancement, a thickened pituitary stalk and intact sellar floor. Treatment of choice in the acute phase of a hypophysitis is corticosteroids. Adequate corticosteroid treatment may effectively buy time and avoid unnecessary surgical treatment and is related to further decrease of pituitary function, even in progressive cases of deterioration due to compression of the chiasm. Strict monitoring of the vision and a control MRI is obligatory to evaluate the treatment after 48–36 h. Tissue diagnosis is mandatory when there are multiple relapses. We present a case of progressive visual deterioration in hypophysitis, successfully treated with high-pulse dose prednisolone.
Background
Pituitary adenoma is a renowned cause of a pituitary mass. Patients typically suffer from headache, visual disturbances or a hypersecreting syndrome.1 Hypophysitis is an important differential diagnosis in patients with a pituitary mass, headache and/or visual disturbances. Hypophysitis commonly results in hypopituitarism and requires a different therapeutic approach.2–6 It is usually further categorised in lymphocytic and granulomatous hypophysitis. Lymphocytic hypophysitis, which involves the adenohypohysis, predominantly affects young women at the end of pregnancy up to 1 year postpartum and is associated with other autoimmune diseases.2–6 Granulomatous hypophysitis often presents in older patients, with more reports on men affected and is restricted to the neurohypophysis resulting in a central diabetes insipidus.2–6 An MRI can be very useful in discriminating a pituitary mass. Typical MRI characteristics of hypophysitis are symmetry, loss of posterior bright spot, intense and homogeneous gadolinium enhancement, thickened pituitary stalk and intact sellar floor.1 Adenomas are commonly larger in volume often to have eroded the sellar floor, as they are likely to be discovered later.1
Case presentation
A 27-year-old women presented with headache since 3 months, accompanied by progressive visual blurring over the course of 2 weeks. Four months ago, she had given birth to a healthy child, which she was currently breastfeeding. Her medical and family history was unremarkable. Extensive neurological examination only revealed papilloedema on the right side, yet no other focal deficits. At this point, the ophthalmologist assessed her visual acuity to be 0.8. Consecutively, a brain MRI and routine laboratory examination was ordered.
Investigations
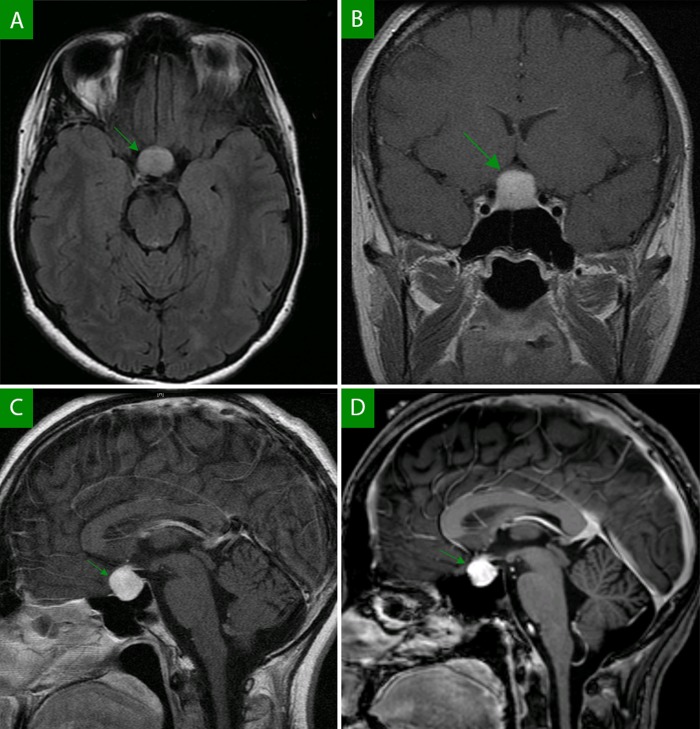
Brain MRI demonstrated a symmetric pituitary mass and intact sellar floor, with intense homogeneous gadolinium enhancement and thickened pituitary stalk (figure 1A–C).
Figure 1.
Brain MRI: axial fluid-attenuated inversion recovery-weighted image revealing an hyperintense pituitary mass (A); coronal T1-weigted and saggital T1-weighted image after gadolinium contrast (B, C), demonstrating a hyperintense pituitary mass with intense and homogeneous pituitary contrast-enhancement (B). Note the symmetrical aspect and involvement of the pituitary stalk and intact sellar floor. Saggital T1-weighted image with gadolinium contrast after 3 days of high-pulse dose corticosteroid treatment (D), demonstrating a decrease in size of the pituitary mass.
Laboratory examination revealed a normal hormonal profile except a mildly diminished T4 level of 10 (12–20 pmol/L).
Differential diagnosis
Hypophysitis
Pituitary adenoma
Craniopharyngeoma
Meningioma
Outcome and follow-up
A diagnosis of probable hypophysitis was found. Over the course of 3 days visual acuity further decreased to 0.6; therefore, a high-pulse dose of methylprednisolone (1 g, 3 days) was immediately initiated.
Within 2 days, the headache ameliorated quickly and visual acuity improved to normal (1.0). A second MRI, 3 days after the start of methylprednisolone, demonstrated a decrease of the pituitary mass (figure 1D). Hence a thyroid suppletion and prednisolone tapering scheme were started. Unfortunately, on follow-up she developed multiple relapse. After review of the case in a tertiary centre, a biopsy of the pituitary mass was proposed. Histological analysis of the biopsy specimen proved the proposed diagnosis of lymphocytic hypophysitis. Extensive treatment with immunosuppressive drugs at relapse rendered her with panhypopituitarism and Cushing's syndrome.
Discussion
Over 400 cases of hypophysitis have been reported since its first description by Goudie en Pinkerton.1 2 However, most of the reported cases on hypophysitis are retrospective with a definite diagnosis based on histopathological findings.1–9 Gutenberg et al1 introduced an MRI score to differentiate hypophysitis from non-secreting pituitary adenoma. They reported excellent specificity, sensitivity and positive predictive value of 97%.1 In the presented case this score unequivocally favoured the diagnosis of hypophysitis. This was further supported by the hormonal profile and clinical as well as radiological response to corticosteroids.
Whereas some patients make a spontaneous recovery, corticosteroid treatment is commonly used as conservative treatment.4 5 10 Headache and mild visual disturbances are widely accepted stages, suitable for conservative treatment. Progressive visual deterioration is commonly regarded as a surgical emergency.2–6 The goal of surgery is to decrease the size of abnormal mass and to preserve normal pituitary gland. However, it introduces the risks associated with operation including decrease of pituitary function. Our case illustrates that a high-pulse dose prednisolone can effectively buy time in the acute phase of the disease. As is outlined in the presented case, tissue diagnosis is mandatory when there are multiple relapses.
Learning points.
Hypophysitis is an important differential diagnosis in patients with a pituitary mass, headache and/or visual disturbances.
Typical MRI characteristics of hypohpysitis are symmetry, loss of posterior bright spot, intense and homogeneous gadolinium enhancement, thickened pituitary stalk and intact sellar floor.
Adequate corticosteroid treatment may effectively buy time and avoid unnecessary surgical treatment and its related further decrease of pituitary function in the acute phase of hypophysitis, even in progressive cases.
Footnotes
Contributors: SHG is the primary physician in the presented case, was involved in acquisition of data analysis and interpretation. MB is the attending physician in the presented case, he contributed to critical revision of the manuscript for important intellectual content. WAN and PD were involved in case supervision and critical revision of the manuscript for important intellectual content.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gutenberg A, Larsen J, Lupi I, et al. A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. AJNR Am J Neuroradiol 2009;2013:1766–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molitch ME, Gillam MP. Lymphocytic hypophysitis. Horm Res 2007;2013(Suppl 5):145–50 [DOI] [PubMed] [Google Scholar]
- 3.Laws ER, Vance ML, Jane JA., Jr Hypophysitis. Pituitary 2006;2013:331–3 [DOI] [PubMed] [Google Scholar]
- 4.Rivera JA. Lymphocytic hypophysitis: disease spectrum and approach to diagnosis and therapy. Pituitary 2006;2013:35–45 [DOI] [PubMed] [Google Scholar]
- 5.Bellastella A, Bizzarro A, Coronella C, et al. Lymphocytic hypophysitis: a rare or underestimated disease? Eur J Endocrinol 2003;2013:363–76 [DOI] [PubMed] [Google Scholar]
- 6.Ng WH, Gonzales M, Kaye AH. Lymphocytic hypophysitis. J Clin Neurosci 2003;2013:409–13 [DOI] [PubMed] [Google Scholar]
- 7.Landek-Salgado MA, Gutenberg A, Lupi I, et al. Pregnancy, postpartum autoimmune thyroiditis, and autoimmune hypophysitis: intimate relationships. Autoimmun Rev 2010;2013:153–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rumana M, Kirmani A, Khursheed N, et al. Lymphocytic hypophysitis with normal pituitary function mimicking a pituitary adenoma: a case report and review of literature. Clin Neuropathol 2010;2013:26–31 [DOI] [PubMed] [Google Scholar]
- 9.Carmichael JD. Update on the diagnosis and management of hypophysitis. Currt Opin Endocrinol, Diabetes, Obes 2012;2013:314–21 [DOI] [PubMed] [Google Scholar]
- 10.Curto L, Torre ML, Cotta OR, et al. Lymphocytic hypophysitis: differential diagnosis and effects of high-dose pulse steroids, followed by azathioprine, on the pituitary mass and endocrine abnormalities—report of a case and literature review. Sci World J 2010;2013:126–34 [DOI] [PMC free article] [PubMed] [Google Scholar]