Abstract
Current guidelines advocate the use of capsule endoscopy (CE) when gastroscopy and colonoscopy have failed to demonstrate the origin of occult gastrointestinal bleeding. CE has been used successfully in the diagnosis of a variety of conditions such as coeliac disease, polyposis syndromes and small bowel tumours, when routine investigations have failed to yield a diagnosis. In conditions where the diameter of the bowel lumen may be compromised, such as Crohn's disease, CE is contraindicated because of the risk of retention and/or small bowel obstruction. Here we present an unusual case where CE resulted in small bowel obstruction and perforation in a segment of small bowel which had become inflamed secondary to a carcinoid tumour.
Background
The wireless capsule endoscopy (CE) was first introduced in 1999 as a technique used to examine the small bowel.1 The original Pill Cams took approximately 60 000 images of the gastrointestinal tract at a rate of 2 images/s.2 Guidelines commissioned by the British Society of Gastroenterology suggested that CE should be used when gastroscopy and colonoscopy have failed to demonstrate the site of bleeding.3
Developed to identify sites of occult gastrointestinal bleeding, CE is now increasingly used for investigation of other conditions, including polyposis syndromes, coeliac disease and inflammatory bowel disease, as agreed on at the Fourth International Conference for capsule endoscopy.2 It has a relatively good safety profile with retention being its main complication occurring in up to 2% of patients.4 5 It has a high diagnostic yield, particularly for small bowel pathology, of approximately 55–60%.4
Case presentation
A 69-year-old man had experienced intermittent abdominal pain and loose stools for 3 years. A CT scan, with intravenous contrast, and gastroscopy demonstrated no gross abnormality and two subsequent colonoscopic examinations found only a single adenomatous polyp. A subsequent barium meal and follow-up through 1 year later was also normal.
Having previously declined CE because of anxiety regarding what the investigation entailed, he presented to clinic with worsening of his symptoms towards the end of this 3 year period. On this attendance, he described opening his bowels 20 times a day, with no blood or mucus, but had associated anorexia and had lost approximately two stones in weight. On examination his abdomen was found to be soft with mild suprapubic tenderness. Owing to the persistent nature of his symptoms, he eventually agreed to a CE.
Outcome and follow-up
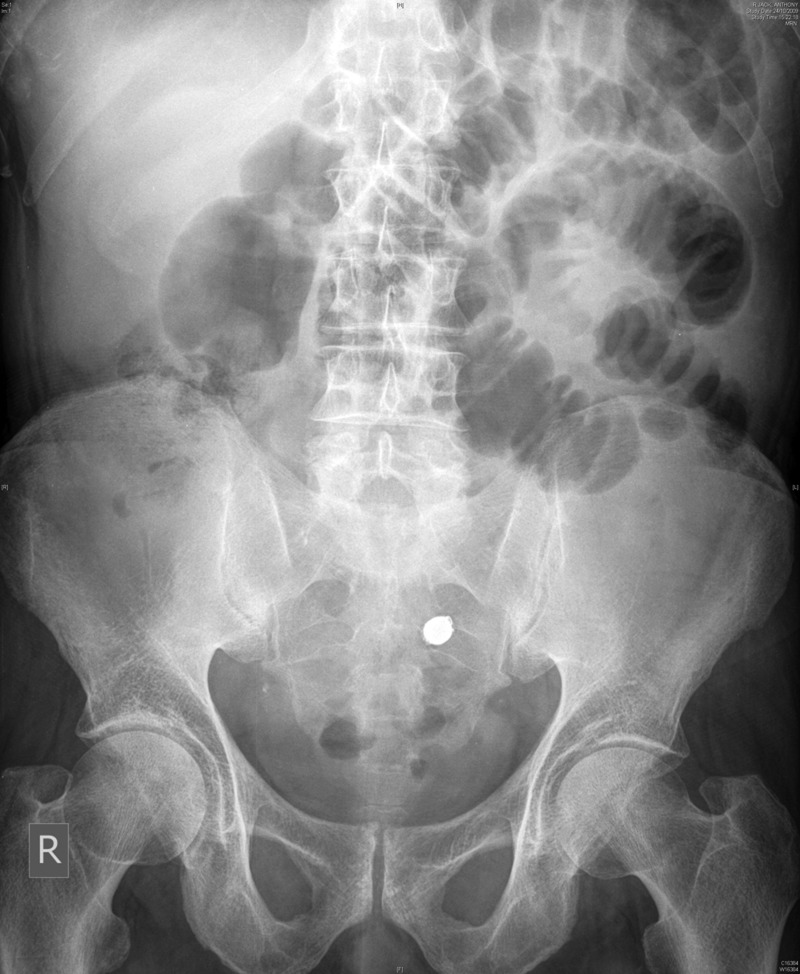
One day post-CE, the patient presented to the accident and emergency with severe abdominal pain and reduced bowel opening. On examination his abdomen was soft but tender with suprapubic fullness and high-pitched bowel sounds. Results of the CE demonstrated numerous areas of small bowel inflammatory changes and stenotic regions, features typical of severe small bowel Crohn's disease. He subsequently developed nausea and vomiting and ceased to open his bowels. Given the clinical signs and the plain abdominal film (figure 1) the impression was of incomplete small bowel obstruction precipitated by a partially impacted capsule and consequently the patient underwent a laparotomy.
Figure 1.
Plain abdominal X-ray showing incomplete small bowel obstruction. The retained capsule is also visible in the left side of the pelvis.
At operation, a dense inflammatory mass involving the ileum was found, with evidence of localised perforation. A small bowel resection and right hemicolectomy was undertaken, resulting in a right iliac fossa jejunostomy and mucus fistula of the transverse colon. Histological examination of the resected specimen (69 cm of terminal ileum with attached caecum and ascending colon 17 cm in length) showed severe inflammation around the base of the caecum. Small bowel, covered in inflammatory exudate, was found to contain the CE obstructing the bowel lumen within a kinked segment (figure 2). This small bowel also had foci of carcinoid tumour, confirmed by immunohistochemistry, which extended into the small bowel mesentery. However, there was no evidence of metastatic disease.
Figure 2.

Resected bowel. The capsule is seen impacted proximal to the ileocaecal valve.
Discussion
This case demonstrates the occurrence of what is recognised to be the most serious adverse event secondary to CE; acute small bowel obstruction and perforation secondary to capsule retention. Although there are several reports of capsule retention occurring secondary to CE,4 6 7 there are few cases of CE resulting in a symptomatic obstruction and subsequent perforation, this being the first report of CE causing obstruction in a patient with small bowel carcinoid.7–9
CE retention and consequent obstruction facilitated identification of previously unidentified pathology in this case.6 However, evidence suggests that CE obstruction is most commonly asymptomatic and occurs secondary to various pathologies including Crohn's disease, small bowel neoplasms, NSAID induced enteropathy and stenosis following a previous surgery.4 While this case of CE related obstruction could be argued to be beneficial in that it yielded a diagnosis for the patient, obstruction is a significant procedural complication with the majority (58.7%) of capsules requiring surgical removal, often in patients whose pathologies would not ordinarily require surgical intervention.4
The case also illustrates that the small bowel remains a challenging site to accurately image, leading to greater use of CE as a sensitive modality for identifying suspected small bowel mucosal abnormalities.10 With the use of oral and intravenous contrast agents, administration techniques that facilitate greater small bowel distension and high resolution and three-dimensional imaging techniques, CT scanning is increasing in sensitivity for detection of small bowel pathology. Furthermore, MR may also have a role in demonstrating mucosal lesions of small bowel, as it allows better soft tissue characterisation, thus identifying subtle areas of abnormality.10
It is possible that the use of sequential CT/MRI may have demonstrated the subsequently found intraoperative pathology. While the initial CT, undertaken prior to diagnosis, was reported as normal, we were unable to retrieve and re-review this imaging post-diagnosis to assess for missed pathology. However, there is some evidence to suggest that even with known carcinoid tumours, their small size and slow growth frequently creates difficulty in locating them anatomically with CT imaging.11
Furthermore, in the investigation of chronic diarrhoea and non-specific abdominal pain, it is important to consider a variety of differential diagnoses including irritable bowel syndrome, inflammatory bowel disease, malabsorption syndromes, chronic infections (HIV) and rarer causes such as hyperthryroidism and carcinoid syndrome.
Carcinoid syndrome occurs in approximately 8% of patients with carcinoid and gives rise to symptoms of diarrhoea and flushing through release of serotonin.12 In cases such as this, with small bowel carcinoid, carcinoid syndrome almost exclusively occurs in the presence of liver metastases, which were absent in our patient. While carcinoid syndrome has been reported in the absence of liver metastases, it is more likely that the symptoms in this case were due to the local tumour effect. However, it is also possible that, despite symptoms resolution following surgery, the tumour was an incidental finding on CE.
From our experience in this case, we would therefore advocate the use of CE in cases where more recognised modalities such as endoscopy and CT scanning have not resulted in a diagnosis. Patency capsules have been suggested as an alternative to CE in patients with obstructive symptoms.13 As many trials have suggested, while it allows us to select those in whom CE will be safe, it may still result in temporary obstructive symptoms.14 However, this may be less likely to subsequently cause perforation or necessitate emergent operative intervention.15
Learning points.
Capsule endoscopy is a useful tool for investigating small bowel pathology, particularly when other modalities have failed.
Obstruction, capsule retention and emergency surgery are serious, but infrequent, complications of capsule endoscopy.
It is essential to thoroughly consent patients for such procedures and inform them of potential complications.
Chronic diarrhoea has various differential diagnoses and it is important to consider rare causes such as carcinoid.
Footnotes
Contributors: RS contributed in conception, design and drafting article. LT contributed in drafting, critical review and redrafting article. AW was involved in concept and design, drafting and critical review of the article. MS was involved in critical review and final approval of the article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Iddan G, Meron G, Glukhovsky A, et al. Wireless capsule endoscopy. Nature 2000;2013:417. [DOI] [PubMed] [Google Scholar]
- 2.Eliakim R. Video capsule endoscopy of the small bowel. Curr Opin Gastroenterol 2010;2013:129–33 [DOI] [PubMed] [Google Scholar]
- 3.Sidhu R, Sanders DS, Morris AJ, et al. Guidelines on small bowel enteroscopy and capsule endoscopy in adults. Gut 2008;2013:125–36 [DOI] [PubMed] [Google Scholar]
- 4.Liao Z, Gao R, Xu C, et al. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc 2010;2013:280–6 [DOI] [PubMed] [Google Scholar]
- 5.Rondonotti E, Soncini M, Girelli C, et al. Small bowel capsule endoscopy in clinical practice: a multicenter 7-year survey. Eur J Gastroenterol Hepatol 2010;2013:1380–6 [DOI] [PubMed] [Google Scholar]
- 6.Cheifetz AS, Lewis BS. Capsule endoscopy retention: is it a complication? J Clin Gastroenterol 2006;2013:688–91 [DOI] [PubMed] [Google Scholar]
- 7.Majeski J. Endoscopic capsule retention in an intestinal anastomosis. Int Surg 2009;2013:254–7 [PubMed] [Google Scholar]
- 8.Boysen M, Ritter M. Small bowel obstruction from capsule endoscopy. West J Emerg Med 2010;2013:71–3 [PMC free article] [PubMed] [Google Scholar]
- 9.Levsky JM, Milikow DL, Rozenblit AM, et al. Small bowel obstruction due to an impacted endoscopy capsule. Abdom Imaging 2008;2013:579–81 [DOI] [PubMed] [Google Scholar]
- 10.Mohanty AP. Small bowel imaging. Medicine 2011:350–421857367 [Google Scholar]
- 11.Horton KM, Kamel I, Hofmann L, et al. Carcinoid tumours of the small bowel: a multitechnique imaging approach. AJR Am J Roentgenol 2004;2013:559–67 [DOI] [PubMed] [Google Scholar]
- 12.Soga J, Yakuwa Y, Osaka M. Carcinoid syndrome: a statistical evaluation of 748 reported cases. J Exp Clin Cancer Res 1999;2013:133–41 [PubMed] [Google Scholar]
- 13.Spada C, Riccioni ME, Costamagna G. The new, dissolving patency capsule: a safe and effective tool to avoid the complication of retained video capsules. J Clin Gastroenterol 2008;2013:761–2 [DOI] [PubMed] [Google Scholar]
- 14.Parikh DA, Parikh JA, Albers GC, et al. Acute small bowel perforation after wireless capsule endoscopy in a patient with Crohn's disease: a case report. Cases J 2009;2013:7607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gay G, Delvaux M, Laurent V, et al. Temporary intestinal occlusion induced by a ‘patency capsule’ in a patient with Crohn's disease. Endoscopy 2005;2013:174–7 [DOI] [PubMed] [Google Scholar]