Abstract
Simultaneous bilateral spontaneous pneumothoraces (SBSP) are uncommon. This report presents the case of a previously well 19-year-old man with a diagnosis of SBSP and symptoms suggestive of occupational asthma. Despite bilateral bullectomy and pleurodesis using a video-assisted thoracoscopic surgical technique, the pneumothorax reoccurred unilaterally and open surgery was performed. This case illustrates a rare condition of bilateral pneumothoraces presenting as a first presentation of occupational asthma and the issues surrounding its management.
Background
Pneumothorax is a common presentation on the medical unit. However, when a patient presents with bilateral pneumothoraces, the signs and symptoms can be quite impressive. This case is quite unique as the history suggests signs and symptoms suggestive of occupational asthma. The patient actually presented as a first presentation with bilateral pneumothoraces and cases presenting like this are few in number. Although the management of pneumothoraces is relatively straight forward, the case highlights the need of careful assessment of patients presenting with symptoms suggestive of occupational asthma.
The patient described a 5-month history of increasing shortness of breath, wheezing and chest tightness. These symptoms were associated with sprayed paint and solvent use at work, and had worsened 2 weeks prior to admission. He had been employed for more than 6 months and had noticed a steady decline in terms of his symptoms including wheeze and shortness of breath. He also noticed that when he was off from work for any considerable period his symptoms would improve. On the day of admission, right-sided pleuritic chest pain associated with severe shortness of breath and chest tightness preceded loss of consciousness.
Case presentation
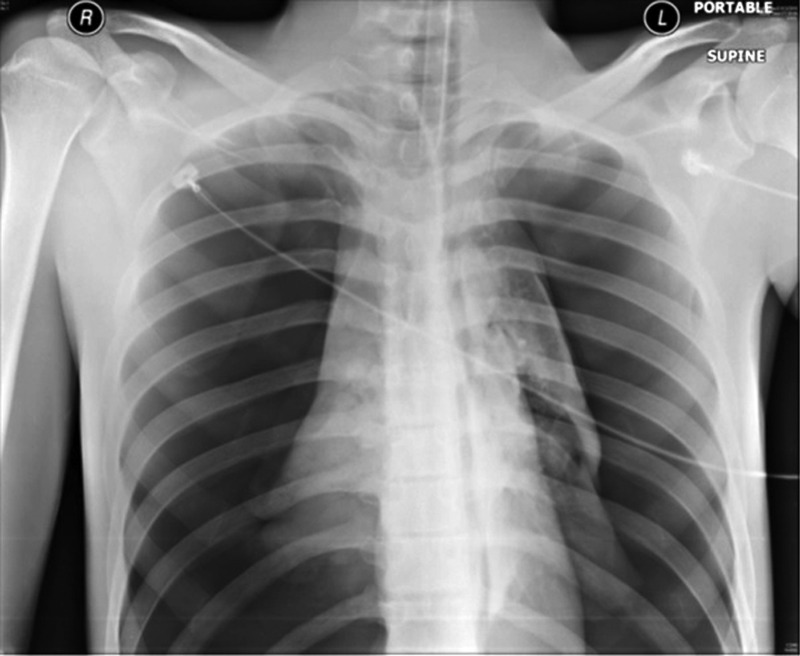
A fit and healthy 19-year-old man presented to the emergency department (ED) with a respiratory arrest. On auscultation breath sounds were absent, and endotracheal intubation was performed in the ED. Arterial blood gases performed on admission with FiO2 60% demonstrated a mixed acidosis. A portable chest radiograph postintubation revealed total bilateral pneumothoraces (figure 1). Bilateral chest drains were therefore inserted (figure 2).
Figure 1.
Supine portable chest radiograph on admission. Total bilateral pneumothorax can be seen, along with endotracheal intubation tube and ECG chest leads.
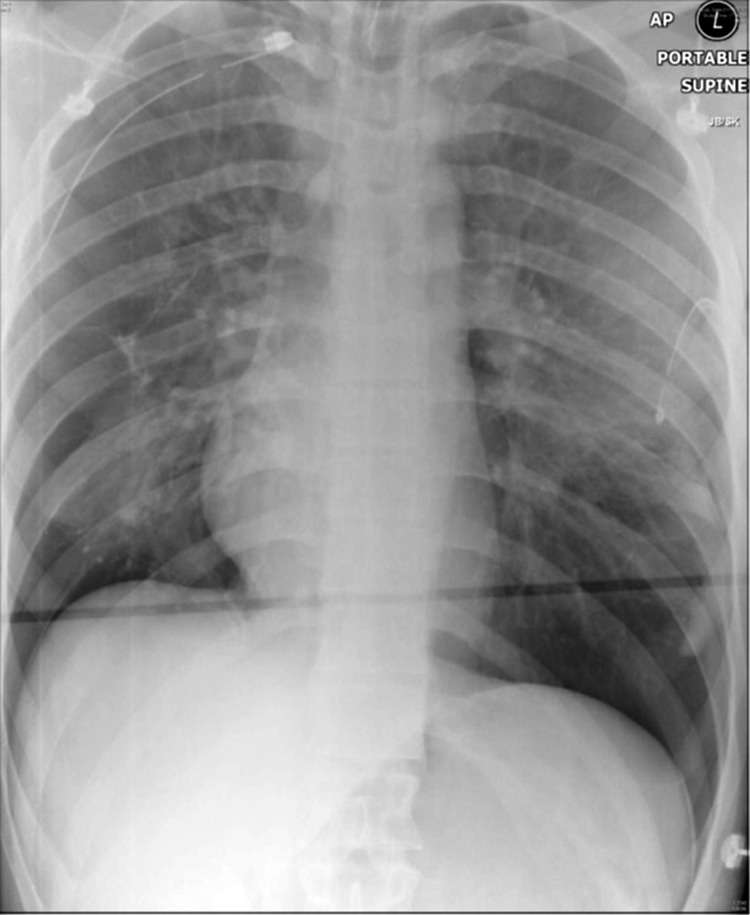
Figure 2.
Supine portable chest radiograph demonstrating reinflation of the lungs following chest-drain insertion.
From 15 days after presentation, the patient underwent right-sided bullectomy and pleural abrasion using a video-assisted thoracoscopic surgery (VATS) technique followed 6 days later by left-sided VATS bullectomy and pleurectomy with talc pleurodesis. Unfortunately, 2 weeks later he was readmitted with a right pneumothorax requiring chest drain insertion (figure 3). High resolution CT revealed no obvious bullae (figures 4 and 5). The patient then underwent right thoracotomy, apical bullectomy and pleurodesis. He had remained well throughout the follow-up. His spirometry in follow-up asthma clinic showed an FEV1 90% predicted with a ratio of 85%. Although the patient had normal spirometry, he had significant symptoms that would correlate with a diagnosis of occupational asthma and his symptoms have since settled after a change in occupation.
Figure 3.
Supine portable chest radiograph demonstrating reoccurrence of the right-sided pneumothorax.
Figure 4.
High-resolution CT demonstrating reoccurrence of the right-sided pneumothorax and absence of any obvious underlying lung pathology.
Figure 5.
Chest radiograph at 4-month follow-up demonstrating the absence of pathology.
Investigations
Chest X-rays, blood gases and CT thorax.
Differential diagnosis
Bilateral pneumothoraces, possible causes in this case include occupational asthma or unilateral pneumothorax then leading to bilateral pneumothoraces secondary to intubation.
Treatment
Bilateral chest drains were inserted on admission.
About 15 days after presentation, the patient underwent right-sided bullectomy and pleural abrasion using a VATS technique followed 6 days later by left-sided VATS bullectomy and pleurectomy with talc pleurodesis.
The patient then underwent right thoracotomy, apical bullectomy and pleurodesis after a recurrence of his pneumothorax.
Outcome and follow-up
The patient had remained well throughout the follow-up. After a change in his occupation, his symptoms of asthma had resolved.
Discussion
Simultaneous bilateral spontaneous pneumothorax (SBSP) are a rare phenomenon. Only 1.3–1.9% of spontaneous pneumothorax cases present bilaterally,1 and cases of SBSP occurring in association with asthma as a first presentation are limited. The most consistently reported symptoms are sudden severe chest pain and shortness of breath; however, there is significant variability in the severity and nature of the signs and symptoms described, making imaging essential in the diagnosis of SBSP.2
From previous case studies of asthmatics presenting with bilateral pneumothoraces, 13 patients were found to have underlying lung pathology but in 20 patients no underlying problems other than subpleural blebs were identified by the authors.3–5
The aetiology in these group of patients remains unclear, however the most common suggested mechanisms include
Bronchospasm leading to air trapping causing near-simultaneous bilateral rupture of pre-existing subpleural bullae.
A unilateral tension pneumothorax leading to a pneumomediastinum, which itself allows air to penetrate the contralateral pleura, resulting in bilateral pneumothoraces.
A previously formed or congenital ‘buffalo chest’. A ‘buffalo chest’ is the presence of a pleuropleural communication in the absence of an iatrogenic cause such as surgery.6
Overall, the case presented is interesting given the fact that there was definite history with symptoms consistent with occupational asthma. The diagnosis has only been made after presentation, hence this case is different to others published as it is a first presentation of occupational asthma presenting as a bilateral pneumothoraces.
Learning points.
Consider the possibility of simultaneous bilateral spontaneous pneumothoraces (SBSP) in a patient presenting with sudden severe dyspnoea and chest pain.
The nature and severity of presentation can vary considerably; imaging is therefore essential to diagnosis.
The largest group affected by SBSP is young males without any identified lung pathology.
British Thoracic Society guidelines state that definitive treatment is recommended in cases of bilateral pneumothorax in order to reduce the risk of recurrence.
A full occupational history is essential in these patients as risk factors can easily be missed.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sayar A, Turna A, Metin M, et al. Simultaneous bilateral spontaneous pneumothorax report of 12 cases and review of the literature. Acta Chir Belg 2004;2013:572–6 [DOI] [PubMed] [Google Scholar]
- 2.Williams-Johnson J, Williams EW, Hart N, et al. Simultaneous spontaneous bilateral pneumothoraces in an asthmatic. West Indian Med J 2008;2013:508–10 [PubMed] [Google Scholar]
- 3.Hostetler MA, Davis CO. Bilateral localized tension pneumothoraces refractory to needle decompression. Pediatr Emerg Care 1999;2013:322–4 [DOI] [PubMed] [Google Scholar]
- 4.Jeffrey GS, Marlatt DC. Simultaneous bilateral spontaneous pneumothorax complicating bronchial asthma. Can Med Assoc J 1938;2013:171. [PMC free article] [PubMed] [Google Scholar]
- 5.Henry M, Arnold T, Harvey J, Pleural Diseases Group, Standards of Care Committee, British Thoracic Society BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003;2013(Suppl 2):ii39–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartin DJ, Kendall R, Boyle AA, et al. Case of the month: Buffalo chest: a case of bilateral pneumothoraces due to pleuropleural communication. Emerg Med J 2006;2013:483–6 [DOI] [PMC free article] [PubMed] [Google Scholar]