Abstract
A 43-year-old woman with tubercular choroidal granuloma showed poor response to conventional first-line four-drug antitubercular therapy (ATT) and corticosteroids. A therapeutic trial with intravitreal bevacizumab (1.25 mg in 0.05 mL) injections as an adjunct to ATT and corticosteroids led to a prompt initial regression of granuloma with restoration of visual acuity that was sustained for almost 2 years. A subsequent recurrence of the same lesion with evidence of enhanced vascularity was treated with intravitreal bevacizumab alone, that led to a complete regression of the granuloma with no recurrence until 1 year of follow-up.
Background
In the presence of relevant clinical findings and corroborative evidence, a favourable response to corticosteroids and antitubercular therapy (ATT) is expected in tubercular choroidal granulomas.1 While attempts are being made to elucidate the pathogenesis of intraocular tuberculosis (TB), reduced oxygen tension in choroidal granulomas and increased expression of vascular endothelial growth factor (VEGF) in the retinal pigment epithelium and photoreceptors have been demonstrated in animal models of ocular TB.2 Also, in pulmonary TB, localised tissue hypoxia in necrotic granulomas has been demonstrated in animal models.3 We report the first case of a highly vascular recurrent tubercular choroidal granuloma that was successfully treated with intravitreal injection of bevacizumab.
Case presentation
A 43-year-old woman presented with blurred vision in the right eye of 2 months duration. Before presenting to us, she had been treated for 1 month with oral corticosteroids and first-line four-drug ATT. At presentation to us, she had best-corrected visual acuity (BCVA) of 6/6 in both eyes. The intraocular pressure was 10 and 12 mm Hg in the right and left eyes, respectively. The anterior segment examination was normal in both eyes. The left eye fundus examination was normal. Fundus examination of right eye revealed vitreous cells positive, and a choroidal granuloma with surrounding subretinal exudation.
Investigations
The investigations performed elsewhere before being presented to us revealed a positive tuberculin skin test (30×30 mm), and a positive QuantiFERON-TB Gold test. The haemogram, liver function tests and high-resolution CT scan of the chest were normal.
A whole body positron emission tomography CT at our centre revealed hypermetabolic subcarinal, right tracheobronchial and cervical lymph nodes.
Treatment
The patient was continued on the same treatment. However, 6 weeks after initiation of ATT, her BCVA in the right eye worsened to counting fingers with an increased subretinal exudation. Her systemic therapy was continued and she additionally received intravitreal injection of bevacizumab (1.25 mg in 0.05 mL) in the right eye. Within 72 h, her BCVA in the right eye improved to 6/9 and there was significant reduction of subretinal fluid.
Outcome and follow-up
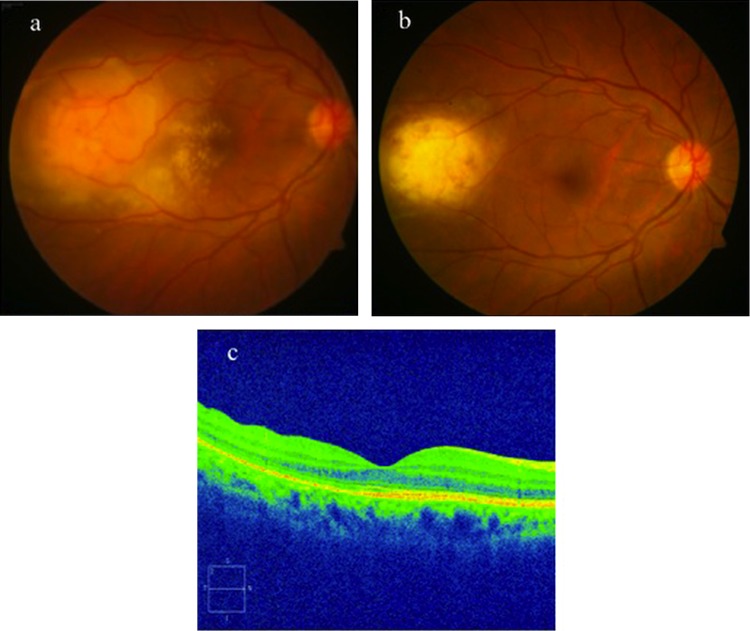
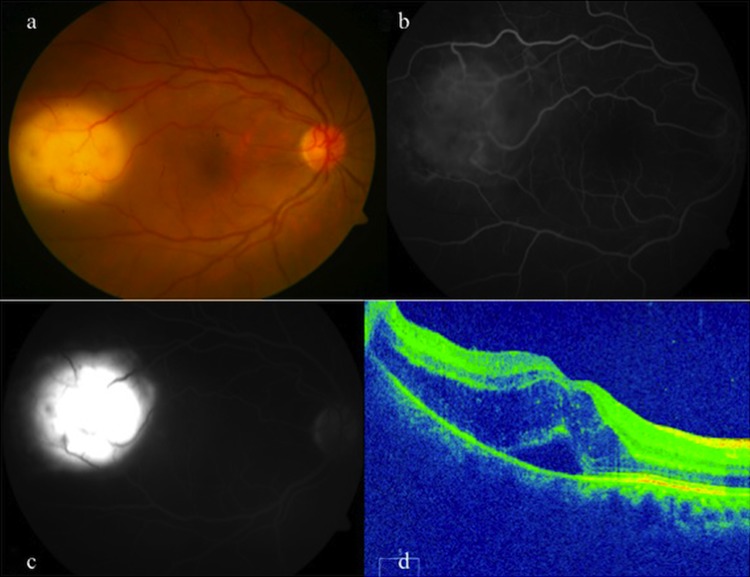
However, at 8 weeks, her BCVA deteriorated again (6/18) and the subretinal fluid increased (figure 1A). She received another intravitreal injection of bevacizumab. The subretinal fluid decreased but persisted on optical coherence tomography (OCT). Speculating drug-resistance at 12 weeks of starting first-line ATT, in consultation with the internist, she was started on second-line ATT. Two weeks after starting second-line ATT, the persistence of subretinal exudation prompted a repeat intravitreal bevacizumab injection. Two weeks following the third injection, her BCVA improved to 6/9 and there was minimal subfoveal fluid on OCT. Subsequently, intravitreal injections of bevacizumab were repeated four weekly (a total of five injections) up to 6 months of follow-up till the OCT showed complete resolution of subretinal fluid. Oral corticosteroids were continued in maintenance dose up to 1 year. At 1-year follow-up, her BCVA was 6/6 in the right eye and the granuloma had completely regressed (figure 1B,C). Second-line ATT was given for 18 months. At 2.5 years of follow-up, she reported decreased vision in the same eye of 5 days duration. Her BCVA in the right eye had decreased to 6/60. Fundus revealed reactivation of the previous lesion that showed extensive leakage of dye on fluorescein angiography, suggestive of enhanced vascularity of the granuloma (figure 2A–D). She received two more injections of intravitreal bevacizumab at four weekly intervals in the right eye that led to complete resolution of the granuloma. At 3.5-year follow-up, the BCVA in right eye was 6/6 and the granuloma remained regressed (figure 3A,B).
Figure 1.
(A–C) Fundus photograph of the right eye of a 43-year-old woman showing an active choroidal granuloma with surrounding subretinal exudation (A). At 1-year follow-up, the granuloma regressed completely (B) with resolution of subretinal fluid as seen on optical coherence tomography (C).
Figure 2.
(A–D) The right eye fundus photograph at 2.5 years of follow-up showing recurrence of the choroidal granuloma (A). Fluorescein angiography showed an increasing vascularity of granuloma in early (B) and late (C) phases. Optical coherence tomography showed presence of intraretinal fluid and subretinal fluid (D).
Figure 3.
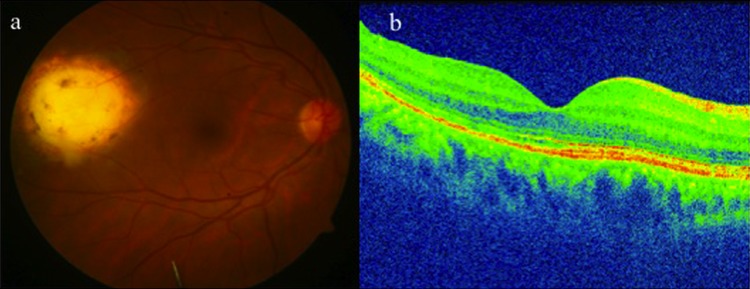
(A and B) The right eye at 3.5 years of follow-up showing the regressed granuloma (A) following intravitreal bevacizumab injection. Optical coherence tomography showing resolution of subretinal fluid (B).
Discussion
Bevacizumab (Avastin; Genentech, Inc, South San Francisco, California, USA), is a humanised monoclonal antibody against VEGF. Induced by hypoxia, VEGF is a multifunctional cytokine. It plays a critical role in cell proliferation and survival, and maintenance of choriocapillaries.4 Intravitreal anti-VEGF agents are commonly used in the treatment of vascular and inflammatory ocular diseases.
VEGF has been used as a biomarker for active TB disease in pulmonary as well as extrapulmonary sites.5 6 Recent research has focused on its role as a therapeutic target to prevent tissue damage due to infection by Mycobacterium tuberculosis. In active ocular TB, intraocular anti-VEGF therapy possibly restores the breakdown of blood retinal barrier and reduces granuloma vascularity, as hypothesised by Thayil et al.2
There are several management issues in this patient that need elaboration.
Six weeks after initiating ATT and oral corticosteroids, she showed progressive worsening of the exudative response with significant decrease in visual acuity. Possibly, this exudative response was either a paradoxical reaction to the ATT often seen in TB disease that generally responds to increased dosing of corticosteroids, or was due to an increased vascularity of the granuloma. The latter appears more convincing, which became evident by the dramatic response to the intravitreal bevacizumab therapy by way of reduction in the subretinal exudation and restoration of vision. However, the response was transient and was not sustained, raising the possibility of a drug-resistant TB disease. In hindsight, perhaps the empirical second-line ATT was initiated too early, rather, it was not even required, because further injections of intravitreal bevacizumab that were repeated four weekly even after starting second-line ATT led to complete resolution of the subretinal fluid with BCVA 6/6. Not only did the exudation resolve, it also remained regressed for 2 years following the anti-VEGF therapy. Development of a recurrence almost 1 year after stopping second-line ATT was managed by intravitreal anti-VEGF therapy alone with two injections that led to maintenance of remission of the granuloma for 1 year. We believe that enhanced vascularity of the granuloma may be responsible for its so-called recurrence and does not necessarily mean reactivation of the infection. The prompt response to intravitreal anti-VEGF therapy in our patient, restoration of visual acuity and maintenance of remission of the disease that showed a recalcitrant course not responding to conventional anti-inflammatory therapy with first-line as well as second-line ATT suggests a potential use for this drug in choroidal inflammation due to tubercular aetiology.
Learning points.
A tubercular choroidal granuloma can pose a significant therapeutic challenge.
Highly vascular nature of the tuberculoma is evident clinically by fundus fluorescein angiography.
Increased expression of vascular endothelial growth factor within the retinal layers in an animal model of ocular tuberculosis suggests its potential use as a suitable therapeutic target.
Intravitreal bevacizumab in addition to systemic corticosteroids and antitubercular therapy led to prompt regression of the granuloma and prevented visual loss.
Intravitreal bevacizumab may be a useful adjunct in the management of a vascular choroidal granuloma.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gupta V, Gupta A, Sachdeva N, et al. Successful management of tubercular subretinal granulomas. Ocul Immunol Inflamm 2006;2013:35–40 [DOI] [PubMed] [Google Scholar]
- 2.Thayil SM, Albini TA, Nazari H, et al. Local ischemia and increased expression of vascular endothelial growth factor following ocular dissemination of Mycobacterium tuberculosis. PLoS ONE 2011;2013:e28383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Via LE, Lin PL, Ray SM, et al. Tuberculous granulomas are hypoxic in guinea pigs, rabbits, and nonhuman primates. Infect Immun 2008;2013:2333–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marneros AG, Fan J, Yokoyama Y, et al. Vascular endothelial growth factor expression in the retinal pigment epithelium is essential for choriocapillaries development and visual function. Am J Pathol 2005;2013:1451–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsuyama W, Hashiguchi T, Matsumoro K, et al. Increased serum level of vascular endothelial growth factor in pulmonary tuberculosis. Am J Respir Crit Care Med 2000;2013:1120–2 [DOI] [PubMed] [Google Scholar]
- 6.Husain N, Awasthi S, Haris M, et al. Vascular endothelial growth factor as a marker of disease activity in neurotuberculosis. J Infect 2008;2013:114–19 [DOI] [PubMed] [Google Scholar]