Abstract
Osteoma is a benign tumour consisting of mature bone tissue. It is an uncommon lesion that occurs in the bones of the craniofacial complex. Only a few cases involving the temporomandibular joint have been reported. An osteoma of the left temporomandibular joint causing limited mouth opening in a 22-year-old man with CT findings revealing the unusual possibility in differential diagnosis of trismus.
Background
Temporomandibular joint (TMJ) disorder is rarely caused by neoplasms and pseudotumours but their early recognition is important to deliver appropriate treatment, which could have a drastic impact on the patient's quality of life. Osteoma is considered as a rare TMJ lesion as there are other tumours involving TMJ namely osteochondroma, osteoblastoma, simple bone cyst, aneurysmal bone cyst and sarcoma. Conservative management of TMJ disorder is carried out in cases of intraosseous lesion of the condyle which manifests with symptoms of painful/painless swelling, dull pain in preauricular region, clicking/popping and difficulty in mastication.1
Osteomas originate from membranous bones of the skull and face, from the cartilage or embryonal periosteum or periosteum, and structurally they are divided into cortical (ivory) osteoma, cancellous osteoma or a combination of both. Cortical type is more common in males whereas women have a high incidence of cancellous type. The mandible is more affected, especially posterior aspect of the mandible, lingual side of the ramus or inferior border below the molars. Mandibular lesions may be exophytic.2
This case reports an osteoma involving the entire bony components (craniofacial) of the TMJ; which is quite an uncommon entity.
Case presentation
A 22-year-old man presented to the outpatient department with difficulty in mouth opening since 7 years. He noticed the restriction in the mouth opening as a sudden event but could not relate this to any trauma, infection of ear, painful jaw movement, pain in other joints of long bones, etc. Difficulty in eating habits 3 months previously due to further reduction in mouth opening led him to consult a professional. Clinical examination revealed no scars over the mid-face on left side, no obvious facial asymmetry (figure 1). Palpation of TMJ region revealed restricted condylar movements on both sides, and a bony hard, non-tender swelling on left condylar region. Slight deviation of mandible towards the left on opening of the mouth (approximately 8 mm) was seen (figure 2).
Figure 1.

Extra oral picture of patient.
Figure 2.

Restricted mouth opening.
No abdominal symptoms or any skin lesions were reported by the patient, reducing the possibility of Gardner's syndrome.
Investigations
Orthopantomogram (figure 3) revealed a well-circumscribed, uniformly radiopaque, round mass on left TMJ region occupying space of the condyle, sigmoid notch and glenoid fossa; along with an exaggerated antegonial notch on left side. A thin irregular joint space can be appreciated within the substance of the mass in anteroposterior direction. Left coronoid process appears to be larger than the right.
Figure 3.

Orthopantomograph showing large radiopacity in the left temporomandibular joint region.
CT study revealed a hyperdense mass on left TMJ region measuring 3.2 cm mediolaterally and 2.5cm anteroposteriorly. Serial axial slices (figure 4A,B) show well-defined hyperdense round mass appearing to be formed from pedunculated masses around the condyle and with uniform radiodensity including the glenoid fossa superiorly to the neck of condyle inferiorly; obliterating both the anatomical structures. Frontal and sagittal multiplanar reformatted images (figures 5A,B and 6A–C) reveal a hypodense, irregular, roughly horizontal line within the mass, separating it into two parts. Other significant CT finding was the enlarged left coronoid process (figure 4A,B) and left ramus. Clinico-adiographically a provisional diagnosis of benign osteogenic tumour.
Figure 4.
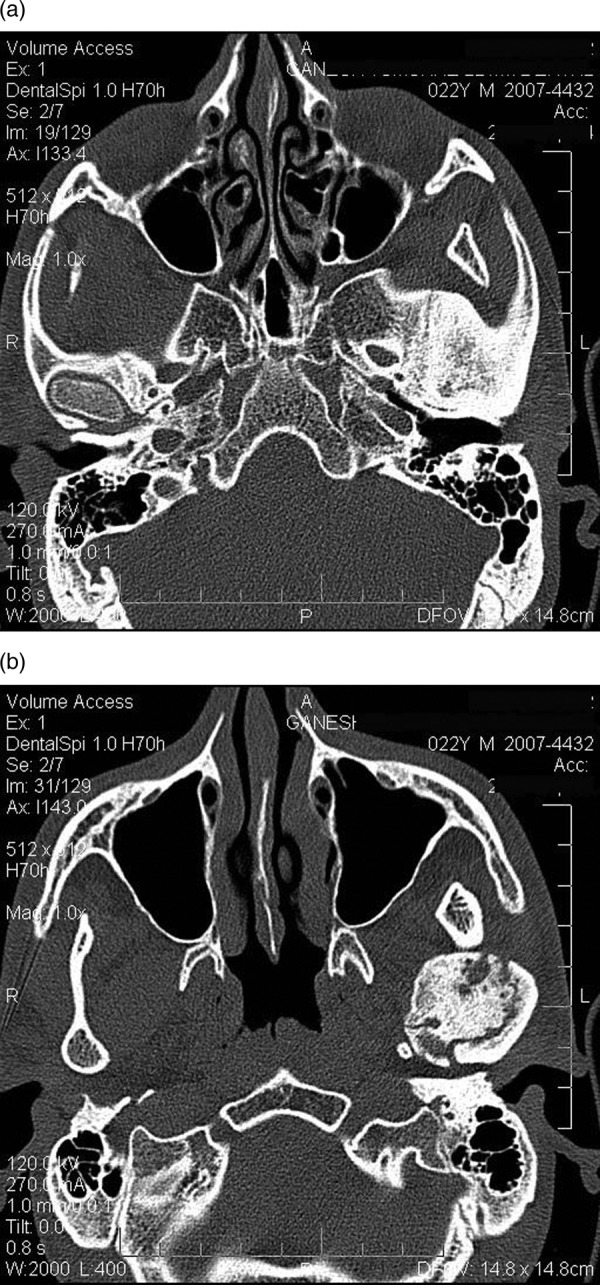
(A) Axial CT slices showing hyperdense mass of size 2.84 cm mediolaterally in left condylar region involving the sphenoid and temporal bones and (B) multiple hypodense areas, within the mass.
Figure 5.
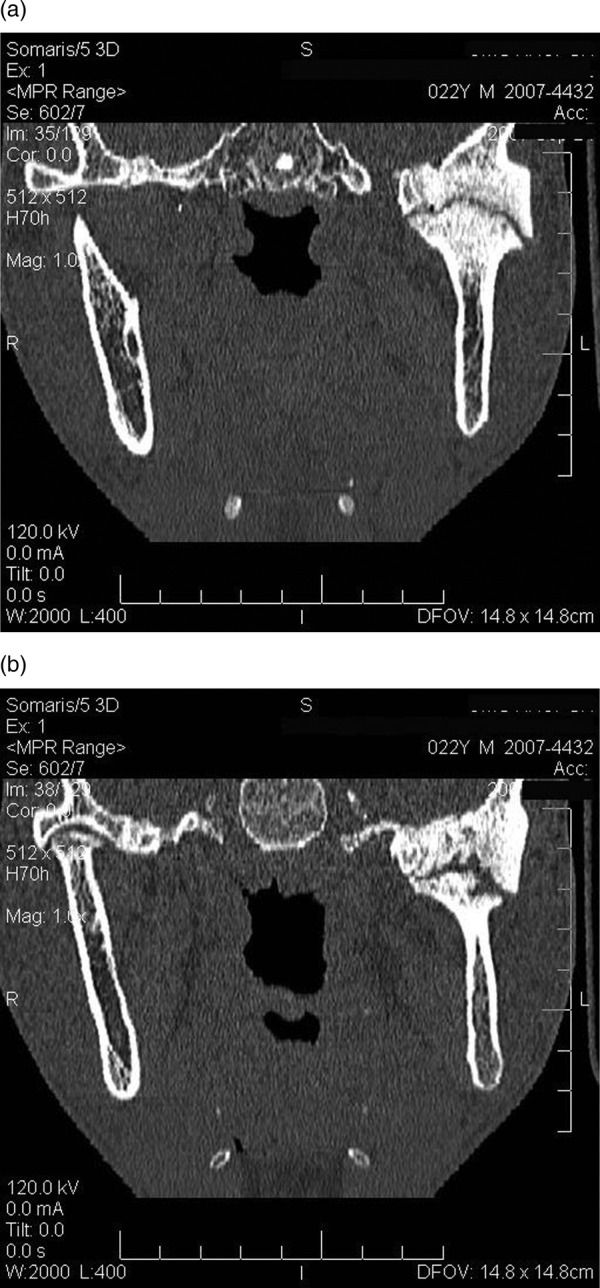
(A) Frontal slices showing hyperdense enlarged temporomandibular joint components with linear hypodense area of variable thickness and (B) hypodense area of variable thickness joint space.
Figure 6.
(A) Sagittal slices showing obliterated joint space (B) change in the structure of the temporomandibular joint components and (C) increased size of the left coronoid process.
Histopathological examination (figure 7) revealed lamellated compact bone enclosing haversian canals, with osteocytes within the lacunae at places while empty lacunae at other places; suggestive of compact osteoma.
Figure 7.
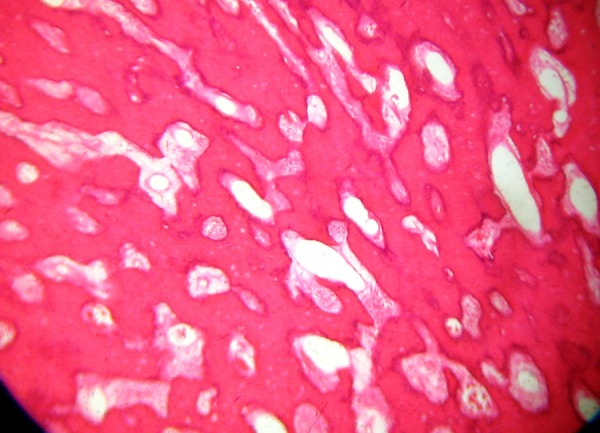
H&E-stained section showing mature lamellated compact bone.
Differential diagnosis
The differential diagnosis is established with
Exostoses—bony excrescences that cease to grow after puberty;
Osteoid osteoma and osteoblastoma—frequently painful and grow more rapidly than peripheral osteoma.
Treatment
Keeping in mind the functional problem faced by the patient, surgery was planned and condylectomy of left side was performed after a neurosurgical evaluation of the cranial components as cranial signs and symptoms were absent which deferred the invasive surgery of cranial part.
Discussion
Osteoma is a benign osteogenic tumour involving compact or cancellous bone proliferation and arising from periosteum (peripheral osteoma), endosteum (central osteoma) and even extra-skeletal soft tissue. Although the exact cause is yet not known, osteomas are formed when there is uninhibited growth in a bone.3 4 Condylar osteomas can be seen to be of two types-either proliferation of tissue causes replacement of condyle or appearing as pedunculated mass on condylar head/neck.3 Peripheral osteoma of jaw bones is not common. Very few cases of osteoma of the TMJ have been reported. Benign tumours of the TMJ tend to occur with less frequency than does malignant disease.5
Although the exact cause is unknown, belief in reactive and neoplastic theories persists. Common sites of origin being the angle, lower border or buccal aspect of the mandible and maxilla, as well as attachment areas of the masticator muscles; these sites are more prone to trauma and may give rise to reactive lesion. However, development of osteoma at other sites suggests involvement of other factors in addition to predisposition. Origin from embryological cartilaginous rests or persistent embryological periosteum has also been believed by researchers who could not get data relating to trauma or the onset of the lesion.6 7 In this patient minor trauma that was not recollected could be a possibility as the onset of lesion 7 years previously.
Trismus is a commonly found entity by the dental practitioners worldwide and osteoma of condyle must be considered as a differential in diagnosing the cause, similar to the case reported in this article. They can occur at any age but most frequently are found in individuals older than 40 years. The patient was 22-year-old when diagnosed.
Osteoma of the condyle may cause a slow, progressive shift in occlusion, with deviation of the midline of the chin towards the unaffected side, resulting in facial asymmetry and malocclusion such as cross-bite. It may produce a painless, hard swelling of the jaws causing asymmetry which may cause interference with function.7 The osteoma may be attached to the cortex by a pedicle or along a wide base. Osteoma typically will manifest as a homogeneous expansion of the mandibular condyle as compared with the contralateral side.5
Other sites include paranasal sinuses, orbital wall, temporal bone, pterygoid processes and external ear canal.7 Multiple osteomas known as osteomatosis, is seen in Gardner's syndrome which is defined as multiple osteomas of the jaws accompanied by colorectal polyps with high malignant potential, anomalies involving soft or hard tissues, congenital retinal pigment hypertrophies and multiple impacted or supernumerary teeth, enostoses or epidermoid cysts.6 7
Radiographically, it appears as a well-defined uniform radiopacity in ivory osteoma or as well-defined radiopacity with evidence of internal trabecular structure in cancellous osteoma. At their centres such masses may exhibit a mixed radiolucent-radiopaque appearance depending on the amount of marrow tissues present. Small endosteal osteomas are difficult to differentiate from foci of condensing osteitis, focal chronic sclerosing osteomyelitis or idiopathic osteosclerosis.2 3 7 Osteomas can be easily confused with complex odontomas.
Panoramic radiography, CT, MRI and radionuclide scanning (scintigraphy) have been utilised for imaging of osteomas of the TMJ region. CT being the most reliable and useful in locating the nidus of the lesion. Activity in the lesion is diagnosed by scintigraphy.7–10
Structurally, osteomas can be divided into three types those composed of compact bone (ivory), those composed of cancellous bone, and those composed of a combination of compact and cancellous bone. Cortical (compact)-type osteomas develop more often in men, whereas women have the highest incidence of the cancellous type. This case was a male patient with compact osteoma.
Surgical removal of the nidus and some of the surrounding normal bone is the usual treatment.2–4 10 After the nidus is removed, all symptoms eventually disappear. The precise localisation of the nidus is important for its complete removal, curettage should be used only in anatomical sites where anatomical excision is not possible. Incompletely excised lesions can recur. The persistence of clinical symptoms, particularly pain hints that the nidus was not completely removed. Radiation should not be used in the treatment of osteoma.4
Learning points.
Temporomandibular joint (TMJ) lesions should be diagnosed at an early stage for effective management.
TMJ tumours, although rare, must be kept in the differential diagnosis of the TMJ disorders.
TMJ tumours in later stages can produce trismus, slow-progressive shift in midline with deviation of chin to unaffected side.
Useful imaging modalities in diagnosis are plain radiography, CT, MRI and radionuclide scanning.
Surgical removal of nidus is must to avoid recurrence.
Footnotes
Contributors: All the authors were involved in the treatment of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Park W, Nam W, Park H, et al. Intraosseous lesion in mandibular condyle mimicking temporomandibular disorders: report of 3 cases. J Orofac Pain 2008;2013:65–70 [PubMed] [Google Scholar]
- 2.Siar CH, Jalil AA, Ram S, et al. Osteoma of the condyle as the cause of limited mouth opening: a case report. J Oral Sci 2004;2013:51–3 [DOI] [PubMed] [Google Scholar]
- 3.Yonezu H, Wakoh M, Otonari T, et al. Osteoma of mandibular condyle as cause of acute pain & limited mouth opening: case report. Bull Tokyo Dent Coll 2007;2013:193–7 [DOI] [PubMed] [Google Scholar]
- 4.Yang C, Qiu WL. Osteoid osteoma of the eminence of temporomandibular joint. Br J Oral Maxillofac Surg 2001;2013:404–6 [DOI] [PubMed] [Google Scholar]
- 5.Kademani D, Bevin C. A mass in the temporomandibular joint. J Am Dent Assoc 2008;2013:301–3 [DOI] [PubMed] [Google Scholar]
- 6.Kaya GŞ, Ömezli MM, Şipal S, et al. Gigantic peripheral osteoma of the mandible: a case report. J Clin Exp Dent 2010;2013:e160–2 [Google Scholar]
- 7.Bulut E, Acikgoz A, Ozan B, et al. Large peripheral osteoma of the mandible: a case report. Int J Dent 2010;2013:834761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donohué-Cornejo A, Franco Garrocho LE, Albarrán-Vergara S, et al. Active giant peripheral osteoma of the mandible. Presentation of one case with follow-up to 6 years. J Clin Exp Dent 2010;2013:e212–14 [Google Scholar]
- 9.Ida M, Kurabayashi T, Takahashi Y, et al. Osteoid osteoma in the mandible. Dentomaxillofac Radiol 2002;2013:385–7 [DOI] [PubMed] [Google Scholar]
- 10.Kumar SM, Kumar PM, Mouli PEC, et al. Osteoid osteoma in mandible: a rare case report with literature review. J Indian Aca Oral Med Radiol 2012;2013:223–5 [Google Scholar]



