Abstract
Primary small cell carcinoma of the oesophagus is a rare, highly aggressive malignancy with diagnosis usually occurring at the most advanced stages. We report a case of small cell carcinoma of the oesophagus presenting with dysphagia and melena. A 79-year-old Caucasian man presented to an outside hospital with dizziness, light-headedness, chest pain and melena for 3 days. He had a history of intermittent dysphagia for solids and a 25-pound weight loss in the past 2 months. He underwent an esophagogastroduodenoscopy that revealed a large polypoid, well-circumscribed friable oesophageal mass causing near complete obstruction of the lumen. This mass extended into the gastric cardia. Oesophageal biopsies were consistent with small cell neuroendocrine carcinoma. He underwent chemotherapy with subsequent remission and developed recurrence of disease in the oesophagus 2 years later. Overall, the patient has had two recurrences of his disease but has survived for more than 2 years with chemotherapy alone.
Background
Small cell carcinoma of the oesophagus is a rare, highly aggressive malignancy. This patient has had two recurrences of disease despite aggressive chemotherapy regimens. However, he has survived 3 years with the disease and is still actively undergoing chemotherapy.
Case presentation
A 79-year-old Caucasian man with a past medical history significant for atrial fibrillation, chronic obstructive pulmonary disease, diabetes mellitus, prostate cancer and a history of tobacco use (50 pack-year; quit 15 years ago) presented to an outside hospital with dizziness, light-headedness, chest pain and melena for 3 days. He had a 2-month history of intermittent dysphagia for solids and a 25 pound weight loss in the past 3 weeks.
Investigations
Physical findings included pale conjunctiva, and laboratory data were as follows: haemoglobin 9.6 g/dL; platelets 186 000 µL. Contrast tomography (CT) scan of the brain showed no evidence of disease. Esophagogastroduodenoscopy (EGD) revealed a large polypoid well-circumscribed friable oesophageal mass causing near complete obstruction of the lumen. This mass extended into the gastric cardia (figure 1). Oesophageal biopsies were consistent with small cell neuroendocrine carcinoma with immunohistochemistry stains positive for chromogranin A, synaptophysin, AE1–3, CD56, and TTF-1 (figures 2–4). The patient was then evaluated by oncology and underwent a CT scan of the chest, abdomen and pelvis which revealed a distal thoracic oesophageal mass extending into the gastric cardia with associated epigastric retroperitoneal adenopathy, multiple liver lesions in both lobes worrisome for metastases, bilateral adrenal gland nodularity and iliac adenopathy with an increase in number and size of the surrounding lymph nodes.
Figure 1.

Oesophageal mass extending into the gastric cardia on esophagogastroduodenoscopy.
Figure 2.
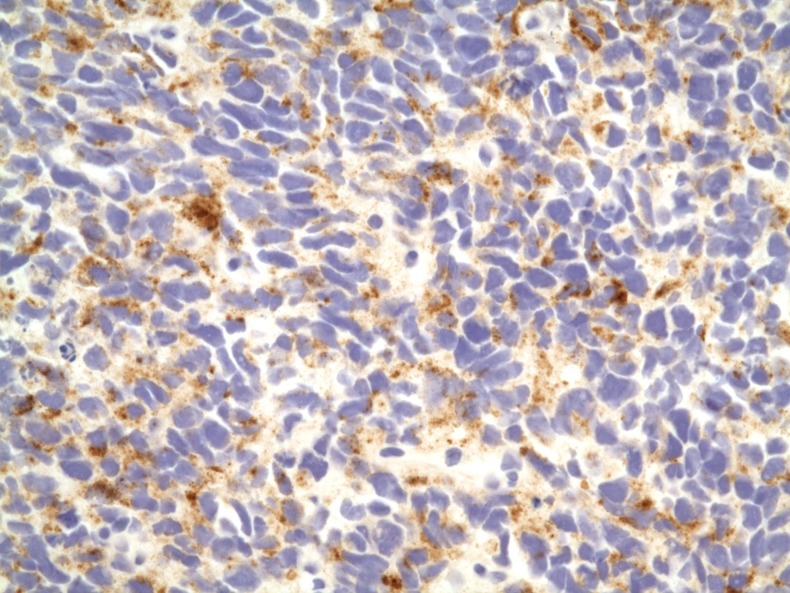
Chromogranin A stain of oesophageal biopsies ×40 magnification.
Figure 3.
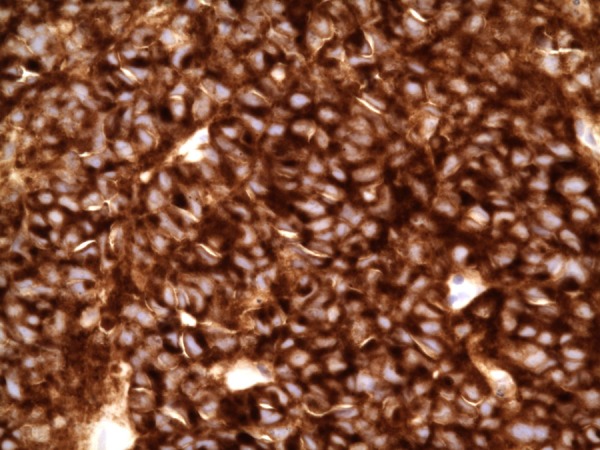
Synaptophysin stain of oesophageal biopsies ×40 magnification.
Figure 4.
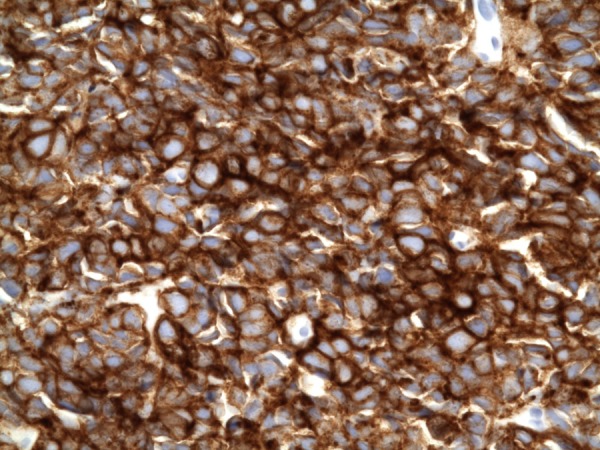
CD56 stain of oesophageal biopsies ×40 magnification.
Treatment
The patient received induction chemotherapy with carboplatin and etoposide. The chemotherapy was decided on based on previous cases that reported success with this regimen1 2 and at the discretion of the oncology team. An EGD 1 year later showed no evidence of oesophageal mass. Biopsies performed at the lower third of oesophagus were negative. Approximately 4 months later, he developed symptoms of dysphagia, and a repeat CT scan revealed evidence of a mass at the distal oesophagus as well as interval enlargement of several gastroesophageal and gastrohepatic lymph nodes. Hepatic lesions were stable. The patient underwent chemotherapy again with six cycles of carboplatin and etoposide. Repeat imaging several months later showed significant regression of the oesophageal tumour. Two months later, a CT scan of the chest, abdomen and pelvis showed increase in the size of gastroesophageal and gastrohepatic lymph nodes. At this time, salvage chemotherapy with topotecan was initiated with palliation as the goal of treatment. The patient underwent three courses of topotecan, but the gastrohepatic adenopathy and oesophageal mass continued to increase in size. Another course of carboplatin and etoposide was then started. Clinically, the patient has been doing fairly well with mild side effects from chemotherapy including fatigue and anaemia.
Outcome and follow-up
Given that the patient continues to have dysphagia and has refused the placement of a stent, the next step is to consider radiation if repeat imaging does not show a decrease in gastrohepatic lymphadenopathy. Overall, the patient has had two recurrences of disease but has survived for 3 years with chemotherapy alone.
Discussion
Oesophageal cancer is more common in men and is the seventh leading cause of cancer death among men in the USA. Squamous cell carcinoma and adenocarcinoma are the two most common oesophageal malignancies with small cell carcinoma accounting for less than 4% of all oesophageal malignancies.3 Small cell carcinomas are among the most highly malignant, poorly differentiated and aggressive of the neuroendocrine tumours.4 Small cell carcinoma of the oesophagus is an extremely rare malignancy with fewer than 300 cases described in the literature since it was first described in 1952 by McKeown.5 Primary small cell carcinoma of the oesophagus is histologically characterised by neuroendocrine-like architectural patterns with immunohistochemical staining for common small cell carcinoma markers including chromogranin, synaptophysin, AE1-3, CD56 and TTF-1.6 Small cell carcinoma of the oesophagus has characteristics similar to that of small cell carcinoma of the lung with early dissemination and treatment which is modelled after treatment of the small cell lung cancer.3 The tumour most commonly occurs during the sixth to eighth decades of life. The presenting symptoms of patients with small cell carcinoma of the oesophagus are usually vague and include dysphagia, weight loss, abdominal pain and chest pain with dysphagia.7 The mean interval from the onset of symptoms to diagnosis is approximately 4 months.8 Small cell carcinoma of the oesophagus is usually located in the middle and lower third of the oesophagus. The diagnosis is established by endoscopy and biopsy although imaging studies can also be helpful to identify the presence of a mass. Small cell cancer of the gastrointestinal tract has a propensity to metastasise early. In fact, a metastatic dissemination is noted at initial diagnosis in 31–90% of cases when the oesophagus is identified as the primary site. The liver, adrenal glands and lymph nodes are the most frequently involved metastatic sites.8 Given the aggressive nature of small carcinoma of the oesophagus with limited treatment options, the median survival is usually ≤12 months even with limited-stage disease,9 10 but there have been case reports of patients surviving for longer.3 11
Owing to its histological similarity with small cell cancer of the lung, small cell cancer of the oesophagus has been treated with a multimodality approach involving chemotherapy combined with radiation therapy. A combination of standard chemotherapy, cisplastin and etoposide, in addition to radiation therapy may offer the best possibility for long-term survival.11–13 There are no published guidelines for endoscopic surveillance of individuals surviving longer than the expected duration which is less than 12 months.14 Small cell carcinoma of the oesophagus is a rare, highly aggressive malignancy. While our patient's presentation showed limited extent of disease, he has had two recurrences despite aggressive chemotherapy regimens. However, he has survived 3 years and is still actively undergoing chemotherapy. Our patient is still asymptomatic from a dysphagia standpoint and has not had any further gastrointestinal bleeding. This patient is unique not only in his presentation with an upper gastrointestinal bleed as a manifestation of his disease, but it also provides useful clinical information regarding the variable natural history and overall prognosis of the disease.
Learning points.
Oesophageal carcinoma is a primary oesophageal malignancy with squamous cell and adenocarcinoma as the two most common subtypes.
Primary small cell carcinoma of the oesophagus is a rare, highly aggressive malignancy with diagnosis usually occurring at the most advanced stages.
There are no published guidelines for endoscopic surveillance of individuals with small cell oesophageal cancer surviving longer than the expected duration which is less than 12 months.
If the patient develops alarm symptoms including dysphagia and anaemia, we would then consider repeating an upper endoscopy for direct visualisation.
Footnotes
Contributors: TS and KF contributed to the patient care and writing of this paper. EA contributed to the writing and review of this case.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Aizawa R, Takakura K, Kubo Y, et al. A case of primary small cell carcinoma of the esophagus responding remarkably to carboplatin (CBDCA)+etoposide (VP-16) combination therapy and radiation therapy. Nihon Shokakibyo Gakkai Zasshi 2009;2013:1334–42 [PubMed] [Google Scholar]
- 2.Makino H, Tajiri T, Onda M, et al. Effectiveness of preoperative chemotherapy using carboplatin (CBDCA) and surgery against an esophageal small cell carcinoma. Dis Esophagus 2002;2013:237–41 [DOI] [PubMed] [Google Scholar]
- 3.Gollard R, Ellis C, VanderHarten C. Small cell/neuroendocrine tumors of the esophagus: presentation of two cases and review of the literature. Tumori 2010;2013:780–3 [DOI] [PubMed] [Google Scholar]
- 4.Ku GY, Minsky BD, Rusch VW, et al. Small-cell carcinoma of the esophagus and gastroesophageal junction: review of the Memorial Sloan-Kettering experience. Ann Oncol 2008;2013:533–7 [DOI] [PubMed] [Google Scholar]
- 5.Mckeown F. Oat-cell carcinoma of the oesophagus. J Path Bacteriol 1952;2013:889–91 [DOI] [PubMed] [Google Scholar]
- 6.Yun J, Zhang M, Hou J, et al. Primary small cell carcinoma of the esophagus: clinicopathological and immunohistochemical features of 21 cases. BMC Cancer 2007;2013:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z, Ma J, Yang J, et al. Primary small cell carcinoma of esophagus: report of 9 cases and review of literature. World J Gastroenterol 2004;2013:3680–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennouna E, Bardet P, Deguiral P, et al. Small cell carcinoma of the esophagus. Am J Clin Oncol 2000;2013:455–9 [DOI] [PubMed] [Google Scholar]
- 9.Lu XJ, Luo JD, Ling Y, et al. Management of small cell carcinoma of esophagus in China. J Gastrointest Surg 2013;2013:1181–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu Y, Qui B, Liu H, et al. Primary small cell carcinoma of the esophagus: review of 64 cases from a single institution. Dis Esophagus. Published Online First: 3 May 2013;10.111/dote.12069 [DOI] [PubMed] [Google Scholar]
- 11.Muguruma K, Ohira M, Tanaka H, et al. Long-term survival of advanced small cell carcinoma of the esophagus after resection: a case report. Anticancer Res 2013;2013:595–600 [PubMed] [Google Scholar]
- 12.Brenner B, Tang LH, Klimstra DS, et al. Small cell carcinomas of the gastrointestinal tract: a review. J Clin Oncol 2004;2013:2730–9 [DOI] [PubMed] [Google Scholar]
- 13.Casas F, Ferrer F, Farrus B, et al. Primary small cell carcinoma of the esophagus: a review of the literature with emphasis on therapy and prognosis. Cancer 1997;2013:1366–72 [PubMed] [Google Scholar]
- 14.Pazdur R. Cancer management: a multidisciplinary approach: medical, surgical and radiation oncology. 7th edn October 2003


