Abstract
We presented a case of a 54-year-old woman, who developed sarcoidosis uveitis while on treatment with the tumour necrosis factor α (TNFα) antagonist etanercept for rheumatoid arthritis. Her condition improved, but did not recover completely after the medication was stopped. After starting her on another TNFα antagonist, adalimumab, the uveitis recovered completely. Etanercept and adalimumab are from the same class of medication, but have different effects on other mediators and cells, which may explain these discrepancies.
Background
To our knowledge this is the first case of sarcoid uveitis associated with etanercept treatment, which recovered with adalimumab. This possible side effect of etanercept is quite unexpected because tumour necrosis factor α (TNFα) plays an important role in the pathogenesis of sarcoid granulomas. As a TNFα inhibitor, etanercept should be suitable for treatment of sarcoidosis. However, there are several published cases of sarcoidosis, developing in patients on etanercept treatment.1–3 We believe that ophthalmologists and physicians should be made aware of this possible side effect of etanercept as sarcoidosis may affect many organs in the body. For a patient who has developed uveitis after starting etanercept, starting of a different drug from the same class may prove to be safe and may even have a beneficial effect.
Case presentation
A 54-year-old woman presented as an emergency with symptoms of flashing lights, floaters and blurred vision in the upper part of the visual fields in both eyes. She suffers with rheumatoid arthritis. She was on treatment with etanercept 50 mg/week subcutaneously.
On examination her visual acuity was 6/4-3 unaided in the right eye and 6/4-2 unaided in the left eye. Colour vision, as measured by an Ishihara chart, was normal. There was a relative afferent pupillary defect in the left eye. Intraocular pressure was 18 mm Hg in the right eye and 29 mm Hg in the left eye after correction for the corneal thickness (+6 mm Hg both eyes). Anterior segment examination was normal. Examination of the posterior segment showed inflammatory cells and ‘snowballs’ in the vitreous bilaterally more in the left eye compared with the right. Cup to disc ratio was 0.2 in the right eye and 0.6 in the left. In the left eye a small optic disc pit was present. In the mid-periphery of the retina there were small disseminated chorioretinitis lesions (figures 1–4). Retinal vessels were normal. Mild anterior uveitis with 1+ cells bilaterally developed later, indicating progression to a bilateral panuveitis.
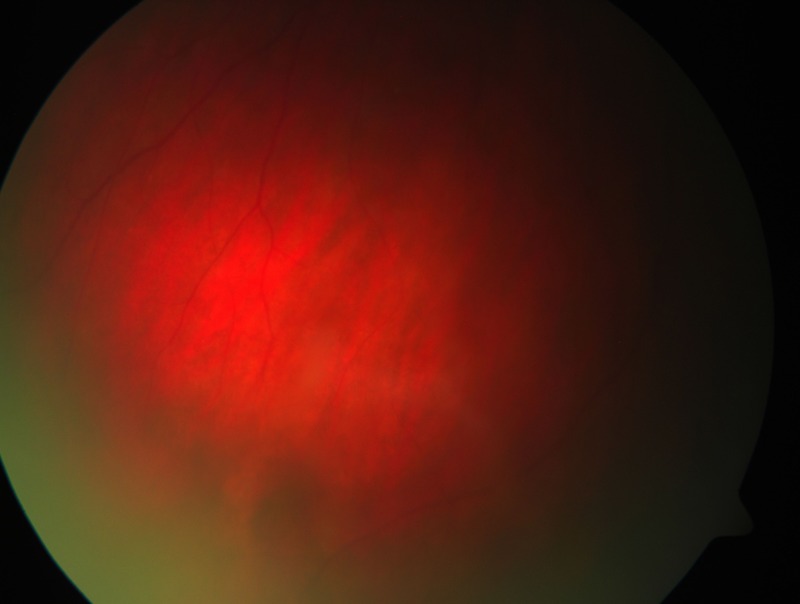
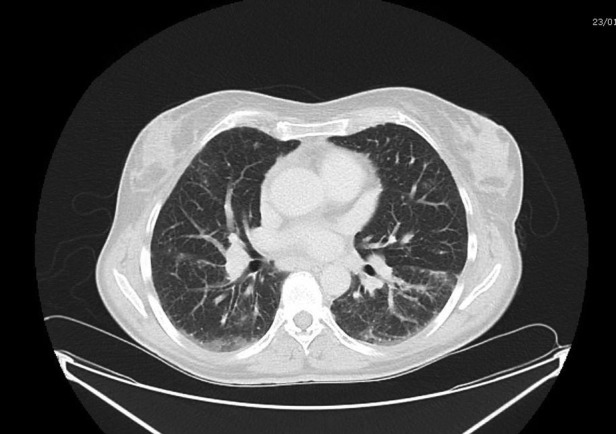
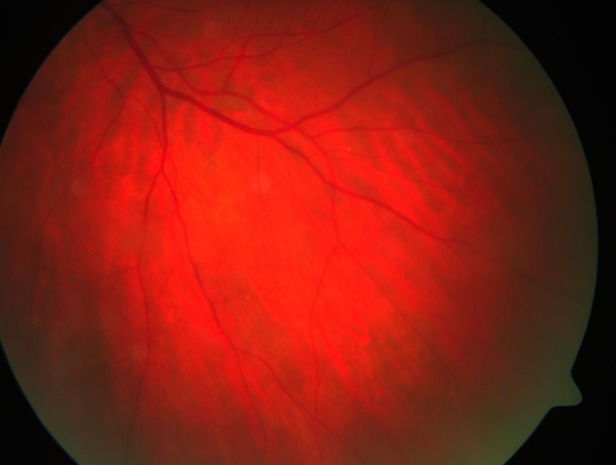
Figure 1.

Right eye at presentation.
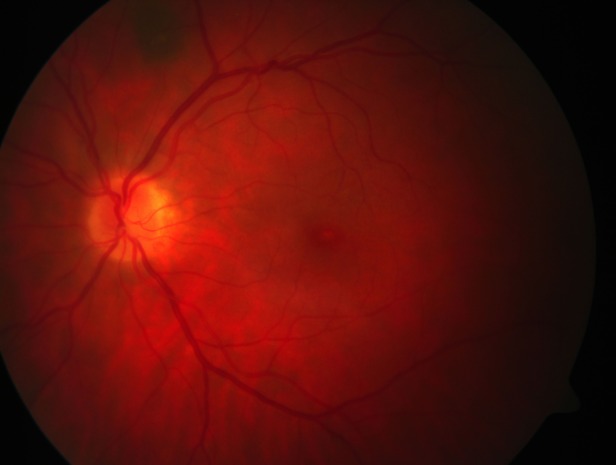
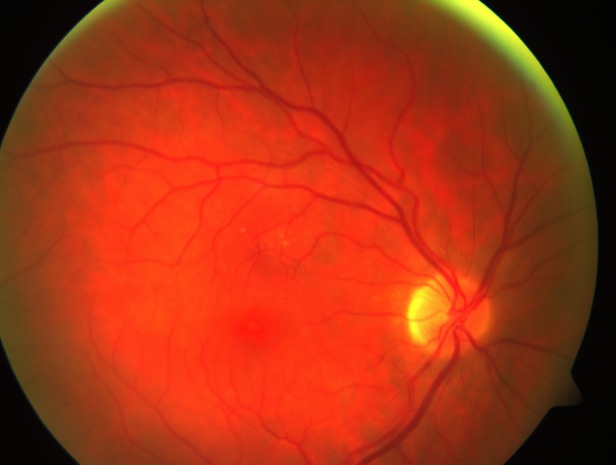
Figure 2.
Right eye periphery at presentation.
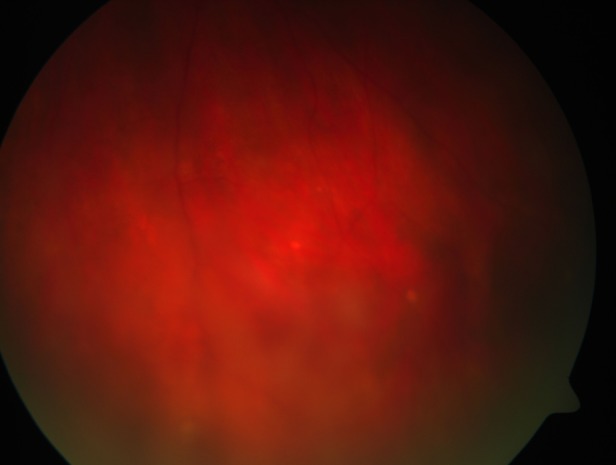
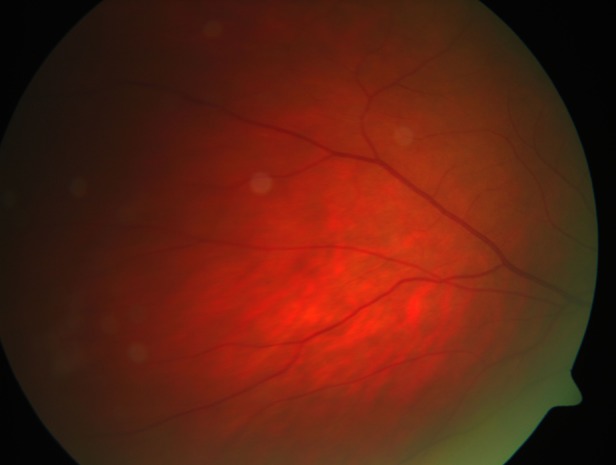
Figure 3.
Left eye at presentation.
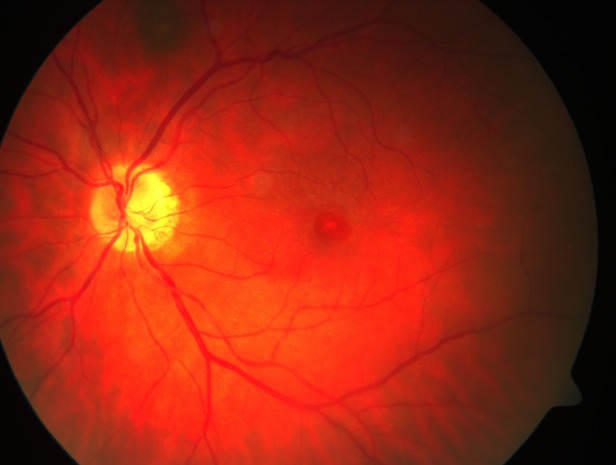
Figure 4.
Left eye periphery at presentation.
Investigations
A visual field test showed superior altitudinal scotoma in the left eye (figure 5). Serum ACE (SACE) was 187 U/L (reference 16–68 U/L) and erythrocyte sedimentation rate was 41 mm/h (reference <30 mm/h). Vitamin D/D3 ratio was 5.4 (reference 0.5–2.5). CT scan of the thorax showed hilar and mediastinal lymph node enlargement (figure 6).
Figure 5.
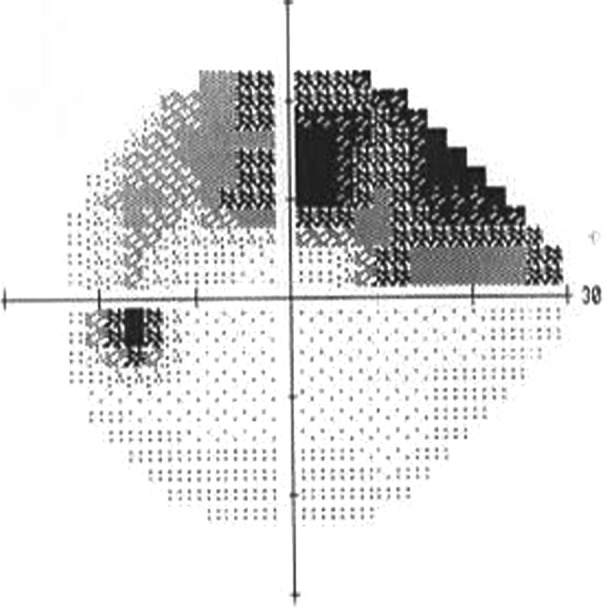
Visual field left eye at presentation.
Figure 6.
CT scan of the chest.
Differential diagnosis
The patient had bilateral panuveitis. Among patients on anti-TNFα medications there is an increased risk of activating tuberculosis.4 However, the clinical picture, the high SACE, vitamin D/D3 ratio and CT of the thorax were suggestive of sarcoidosis.
Treatment
The etanercept treatment was discontinued. The patient did not have any chest symptoms and was not treated with systemic steroids. She was started on brinzolomide 1% eye drops three times a day in the left eye and loteprednol 0.5% eye drops three times a day for both eyes.
Outcome and follow-up
After stopping the etanercept treatment her condition improved. The anterior uveitis resolved and the steroid drops were stopped. The posterior uveitis settled, but did not resolve completely.
In order to control the rheumatoid arthritis 10 months later she was started on adalimumab, another anti-TNFα medication. Two months after this the sarcoid uveitis recovered completely (figures 7–10). The intraocular pressure returned to normal without the need of further treatment.
Figure 7.
Right eye after adalimumab treatment.
Figure 8.
Right eye periphery after adalimumab treatment.
Figure 9.
Left eye after adalimumab treatment.
Figure 10.
Left eye periphery after adalimumab treatment.
Discussion
TNFα is an important factor in the inflammatory response.5 6 Its levels are increased in patients with sarcoidosis and its release is suppressed in patients with prolonged corticosteroid therapy.5 6 Etanercept is a soluble TNFα antagonist and theoretically should be effective in patients with sarcoidosis. However, a study performed by Foster et al7 concluded that there is no additional benefit over placebo in preventing relapses of sarcoid uveitis being tapered from methotrexate. Utz et al8 performed a study, which had to be terminated, because etanercept was associated with early or late treatment failure in patients with progressive stage II or III pulmonary sarcoidosis. TNFα antagonists have different effectiveness in the treatment of uveitis. Infliximab is more effective than etanercept.9 In a review of TNFα inhibitors treatment for sarcoidosis, Callejas-Rubio et al10 concluded that infliximab, and probably adalimumab, are more effective compared to etanercept. Infliximab and adalimumab are monoclonal anti-TNFα antibodies, the former being chimeric and the latter fully humanised. The discrepancies of the action of TNFα medications can be explained by their different effect on the interferon γ and T cells. In addition to TNFα, increased levels of interferon γ and T-cell response have an important role in sarcoidosis.11 Infliximab reduces the production of interferon γ, but etanercept increases it.12 In vitro experiments have shown that infliximab and adalimumab cause lysis of T-cells and monocytes expressing TNFα,13 14 but etanercept does not have such effect. A review by Tong et al15 detected 37 cases of sarcoid-like granulomas developing in patients after anti-TNFα therapy. Most of the patients were on etanercept.15 The majority of these patients improved on withdrawal of the TNFα antagonist.15
Our patient was treated with etanercept for 1 year before developing uveitis. Her condition improved without any other systemic treatment upon withdrawal of the etanercept, but did not recover completely for 10 months. She required treatment for her rheumatoid arthritis and hence was started on adalimumab. There was a temporal relationship between the start of adalimumab treatment and the complete resolution of the uveitis, suggesting that it may have suppressed the sarcoidosis activity. Burns et al16 published a case of etanercept-induced cutaneous and pulmonary sarcoid-like granulomas resolving with adalimumab. To our knowledge this is the first case describing improvement of sarcoid uveitis, associated with etanercept treatment, after switching to adalimumab therapy.
It is possible that the development of sarcoidosis may have coincided with exacerbation of her rheumatoid arthritis. However, simultaneous rheumatoid arthritis coexisting with sarcoidosis is very rare.15 There are four case reports describing such cases since 1950, but at least 34 since 2002, after TNFα inhibitors were introduced.15 This supports the notion of association between etanercept treatment and development of sarcoidosis.
Learning points.
Etanercept treatment may be associated with sarcoidosis in different organs. The unexpected onset of panuveitis in a patient with rheumatoid arthritis on a tumour necrosis factor α (TNFα) antagonist should alarm the clinician to such a possibility.
Patients on one TNFα antagonist, who develop sarcoidosis can be switched successfully to another medication from the same class. Ophthalmologists and physicians should now be made aware of a possible complication of etanercept therapy.
Footnotes
Contributors: All the authors have a substantial contribution in the concept and design, drafting and final approval of this article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fonollosa A, Artaraz J, Les I, et al. Sarcoid intermediate uveitis following etanercept treatment: a case report and review of the literature. Ocul Immunol Inflamm 2012;2013:44–8 [DOI] [PubMed] [Google Scholar]
- 2.Suzuki J, Goto H. Uveitis associated with sarcoidosis exacerbated by etanercept therapy. Jpn J Ophthalmol 2009;2013:439–40 [DOI] [PubMed] [Google Scholar]
- 3.Hashkes PJ, Shajrawi I. Sarcoid-related uveitis occurring during etanercept therapy. Clin Exp Rheumatol 2003;2013:645–6 [PubMed] [Google Scholar]
- 4.Gómez-Reino JJ, Carmona L, Valverde VR, et al. Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicentre active-surveillance report. Arthritis Rheum 2003;2013:2122–7 [DOI] [PubMed] [Google Scholar]
- 5.Baughman RP, Strohofer SA, Buchsbaum J, et al. Release of tumor necrosis factor by alveolar macrophages of patients with sarcoidosis. J Lab Clin Med 1990;2013:36–42 [PubMed] [Google Scholar]
- 6.Ziegenhagen MW, Benner UK, Zissel G, et al. Sarcoidosis: TNF-alpha release from alveolar macrophages and serum level of sIL-2R are prognostic markers. Am J Respir Crit Care Med 1997;2013:1586–92 [DOI] [PubMed] [Google Scholar]
- 7.Foster CS, Tufail F, Waheed NK, et al. Efficacy of etanercept in preventing relapse of uveitis controlled by methotrexate. Arch Ophthalmol 2003;2013:437–40 [DOI] [PubMed] [Google Scholar]
- 8.Utz JP, Limper AH, Kalra S, et al. Etanercept for the treatment of stage II and III progressive pulmonary sarcoidosis. Chest 2003;2013:177–85 [DOI] [PubMed] [Google Scholar]
- 9.Galor A, Perez VL, Hammel JP, et al. Differential effectiveness of etanercept and infl iximab in the treatment of ocular inflammation. Ophthalmol 2003;2013:2317–23 [DOI] [PubMed] [Google Scholar]
- 10.Callejas-Rubio JL, López-Pérez L, Ortego-Centeno N. Tumor necrosis factor-alpha inhibitor treatment for sarcoidosis. Ther Clin Risk Manag 2008;2013:1305–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prasse A, Georges CG, Biller H, et al. Th1 cytokine pattern in sarcoidosis is expressed by bronchoalveolar CD4+ and CD8+ T cells. Clin Exp Immunol 2000;2013:241–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallis RS, Ehlers S. Tumor necrosis factor and granuloma biology:explaining the differential infection risk of etanercept and infliximab. Semin Arthritis Rheum 2005;2013(5 Suppl 1):34–8 [DOI] [PubMed] [Google Scholar]
- 13.Moustou A-E, Matekovits A, Dessinioti Cet al. Cutaneous side effects of anti-tumor necrosis factor biologic therapy: a clinic review. J Am Acad Dermatol 2009;2013:486. [DOI] [PubMed] [Google Scholar]
- 14.Sieper J, Van den Brande J. Diverse effects of infliximab and etanercept on T lymphocytes. Semin Arthritis Rheum 2005;2013:23–7 [DOI] [PubMed] [Google Scholar]
- 15.Tong D, Manolios N, Howe G. et al. New onset sarcoid-like granulomatosis developing during anti-TNF therapy: an under-recognised complication. Intern Med J 2012;2013:89–94 [DOI] [PubMed] [Google Scholar]
- 16.Burns AM, Green PJ, Pasternak S. Etanercept-induced cutaneous and pulmonary sarcoid-like granulomas resolving with adalimumab. J Cutan Pathol 2012;2013:289–93 [DOI] [PubMed] [Google Scholar]


