Abstract
Acute avulsions of the tibial tubercle apophysis are uncommon, with reported incidence of 0.4–2.7% of all physeal injuries. In our case the extent of the injury was not realised at first presentation and initial internal fixation was attempted. At first outpatient follow-up, repeat radiographs indicated the fracture was not reduced and further CT imaging requested. The three-dimensional CT reconstructed images provide considerably more information on the fracture pattern and retrospectively these may have been helpful during the initial procedure. Therefore we would recommend obtaining a preoperative CT scan if extension of the fracture into the tibial physis is suspected. During the second procedure arthroscopy was tried to aid fracture reduction, but visualisation of the anterior articular surface under the anterior horns of the menisci was difficult through the anterior portals with a standard 30° arthroscope and we further recommend having a 70° scope available to ensure optimal visualisation.
Background
This is a rare presentation and the fracture pattern can be misleading. With the use of 3D CT reconstructions, the exact fracture configuration can be identified and understood.
In addition having the correct equipment available in theatre, in our case a 70° arthroscope would have increased visualisation of fragment making the reduction easier.
Case presentation
A 16-year-old boy presented to the emergency department with a painful, swollen left knee caused while playing football. He stated that he was playing as goal-keeper; the ball was in his hands and as he kicked to release the ball he landed on his non-kicking left leg in full extension. He immediately heard a crack and he was unable to bear weight. He had no previous injuries to his knees and no significant medical history.
Plain radiographs were taken showing an avulsion fracture at the tibial tuberosity with extension of the fracture into the proximal tibial physis, which is seen in the paediatric due to the immature growth plate (figure 1). The patient underwent open reduction and internal fixation the following day. The fracture was exposed through a medial mini para-patellar approach with extra-articular visualisation of the fragments. Two 55 mm cannulated screws were used to fix the physis and one 45 mm cannulated screw the tibial tubercle. The intraoperative films are shown in figure 2. Postoperatively the patient was managed in a T-Rom brace, allowed to partially weight bear with the brace in full extension and was discharged on day 2.
Figure 1.
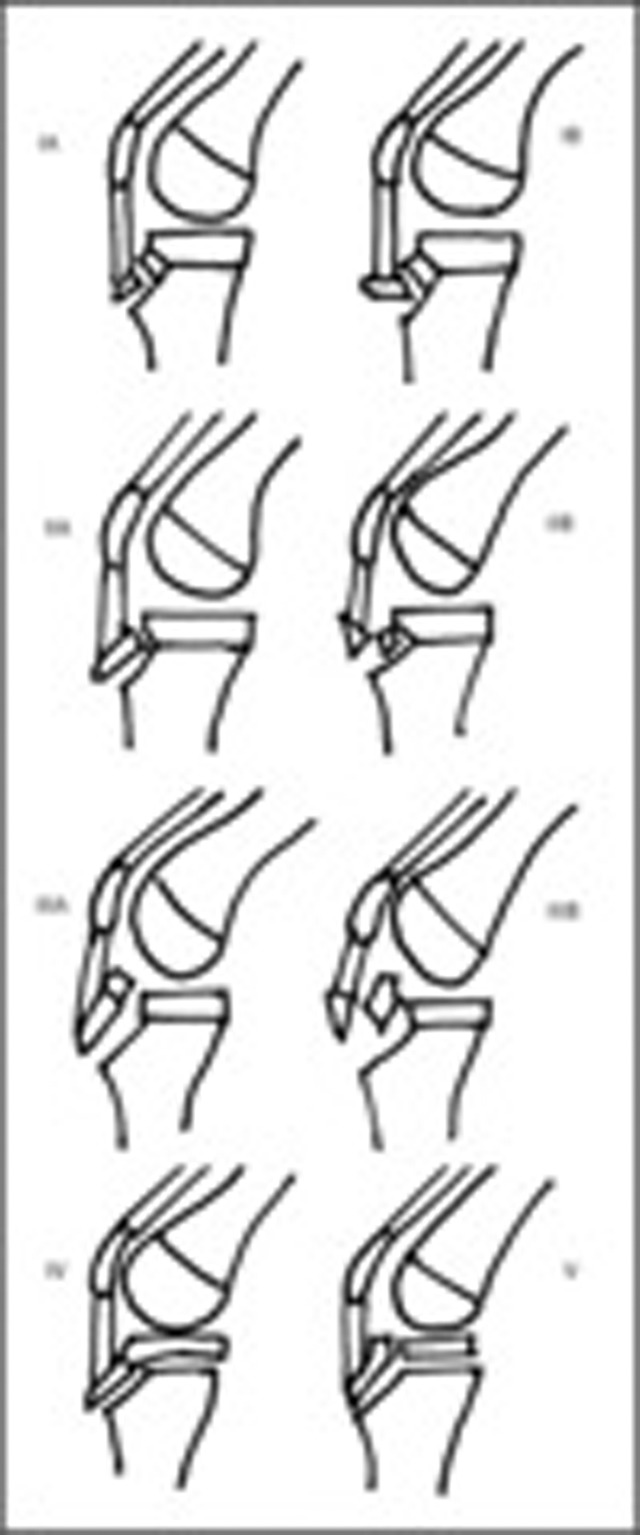
Illustrations of the modified classification of tibial tuberosity fractures.
Figure 2.

Initial radiographs of knee post injury.
The patient was seen routinely in the outpatient clinic a week later; he had been mobilising well with the aid of crutches and had experienced occasional pain from the knee. Repeat radiographs are shown in figure 3 and revealed displacement of the physeal fragment. A CT scan was obtained the same day which confirmed displacement of the fracture and the three-dimensional (3D) reconstructions are shown in figure 4.
Figure 3.
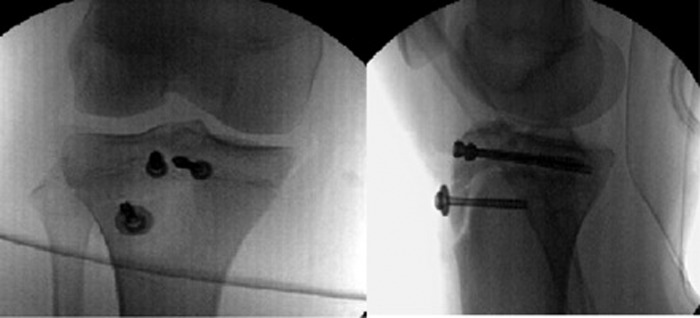
Intra-operative films of fracture fixation using three cannulated screws.
Figure 4.
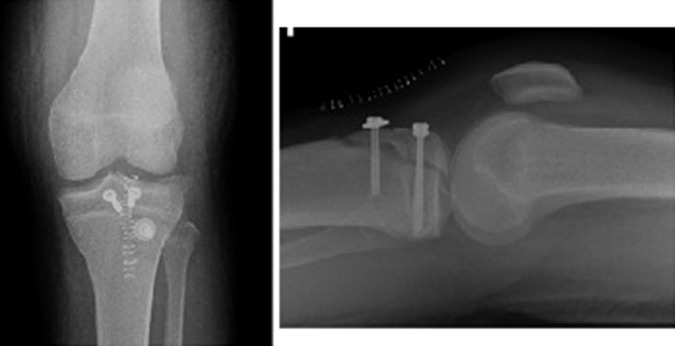
Routine radiographs at one week which suggest redisplacement of fracture.
Owing to the intra-articular displacement the patient was admitted and underwent further surgery on day 10 postinjury. The previous medial para-patellar incision was extended and to assist visualisation medial and lateral arthroscopic portals were made. Separate tibial tubercle and anterior tibial articular fragments were found with peripheral detachment of the anterior horn of the lateral meniscus. The cannulated screws were removed, the anterior fragment reduced with arthroscopic assistance using a standard 30° camera and held with two screws. The tibial tubercle was fixed with a single screw and the anterior horn of the lateral meniscus reattached with vicryl. The reduction was checked both radiologically with image intensifier and arthroscopically figure 5. Postoperatively the patient was mobilised non-weight bearing in a hinged brace blocked at 20° of extension to prevent loading the anterior tibial articular surfaces and at 70° flexion to prevent overloading the tibial tubercle. A further CT was obtained to check fracture reduction; the images are given in figure 6.
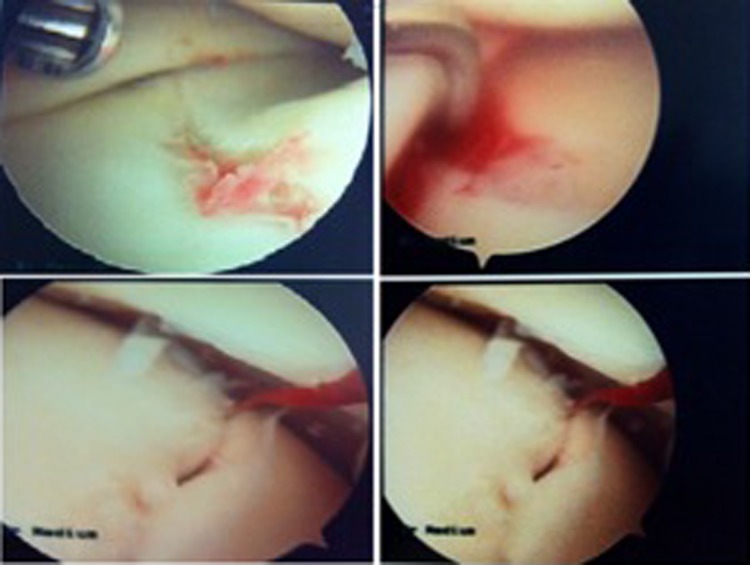
Figure 5.

CT 3-D reconstructions confirming fracture displacement.
Figure 6.
Intra-operative arthroscopic images of fracture and its reduction.
Investigations
Initial investigations included anteroposterior and lateral radiographs of the left knee in order to identify the injury. On routine follow-up, due to increasing pain repeat radiographs plus CT 3D reconstructions illustrating the exact fracture pattern and extension into the tibial physis leading to inadequate operative reduction and fixation. Repeat CT 3D reconstructions were taken after the second operation to ensure adequate reduction and alignment of articular surfaces had been achieved and maintained.
Differential diagnosis
Undisplaced avulsion of the tibial tuberosity
Displaced fracture of tibial tuberosity with physis extension
Treatment
Initial treatment of this injury would follow basic orthopaedic principles of reducing the fracture, operative fixation in this case and early rehabilitation. Understanding the exact fracture pattern is key to providing the correct procedure. As there was intra-articular extension, it was imperative to achieve direct anatomical reduction with fixation. The use of the arthroscope greatly aided this procedure.
Outcome and follow-up
With this mechanism and fracture pattern, there is a high risk of compartment syndrome. There were no signs of this in the immediate postoperative period. The patient was discharged non weight bearing with no complications and seen routinely in paediatric fracture clinic. At 2 weeks he remained pain free; at 7 weeks radiographs showed adequate healing and he was able to bear weight and began physiotherapy in a T-ROM brace. At 6 months, the patient was completely pain free and back to his regular sporting activities with full range of movement in the left knee. He planned to have the screws removed.
Discussion
Acute avulsions of the tibial tubercle are uncommon, with reported incidence of 0.4–2.7% of all epiphyseal injuries.1 2 Some authors have explained this low incidence by the lack of direct ligament attachments to the proximal tibial epiphysis.3–5 Importantly the collateral ligaments attach to the tibial metaphysis so sparing the epiphysis from any varus or valgus stress.6 7 The physis of the tibial tuberosity is composed primarily of fibrocartilage and fibrous tissue, with bone being added to the anterior portion of the tibial metaphysis by membranous bone formation.8 9 The development of the tibial tubercle shows progression from this fibrocartilage to columnar cartilage and begins proximally.10 11 These structural features would be an adaptation to the strong tensile forces exerted in this region.8 At this development stage the tubercle is at highest risk of fracture and correlates with an age of between 13 and 16 years.6 12 13
Two mechanisms for avulsion fractures have been proposed: a powerful contraction of quadriceps during extension, as seen in jumping or rapid passive flexion of the knee against contracted quadriceps, as seen in landing after a jump or fall.14 Originally these injuries were classified by Watson-Jones into three types; in type I a small fragment is avulsed from the tubercle, type II occurs when the whole tubercle is avulsed and in a type III injury, the fracture extends across the proximal physis into the knee joint.15 This classification was modified by Ogden with subdivision into groups A and B according to the level of comminution and displacement.11 A type IV was described by Ryu and Debenham when the fracture extended posteriorly through the physis16 and type V was added by McKoy and Stanitski with a combination of IIIB and IV giving rise to a Y-shaped pattern.17 These classifications are illustrated further in table 1 below and figure 7.
Table 1.
Modified classification of tibial tuberosity (TT) fractures
| Types | TT | Epiphyseal portion (EP) |
|---|---|---|
| IA | Fracture minimally displaced | No disruption |
| IB | Fracture displaced anteriorly and proximally | No disruption |
| IIA | Fracture at junction of TT and EP | No disruption |
| IIB | Fracture comminuted and displaced proximally | No disruption |
| IIIA | Fracture into joint line with EP as composite unit | Disrupted |
| IIIB | Fracture comminuted and displaced proximally | Disrupted |
| IV | Fracture extension transversely through proximal tibial physis with displacement of fracture fragment | Disrupted |
Figure 7.

CT 3-D reconstructions confirming satisfactory reduction.
Early literature on these cases focused on associated soft tissue injuries including; patellar or quadriceps avulsion, collateral or cruciate ligament ruptures and meniscal injuries.18–21 A number of case reports and series have described the association between tibial avulsion fractures with proximal bony injuries.22–25 Owing to the presence of fibrocartilage at the tibial tuberosity, physeal injury is uncommon in young children; however, during adolescence the fibrocartilage is gradually replaced with columnar cartilage and is at increased risk of injury. When they occur these fractures usually propagate along the physeal extension beneath the tibial tuberosity so displacing the tibial epiphysis and tuberosity as one unit.11
Tibial tuberosity fractures with physeal extension tend to be unstable making maintenance of an adequate reduction difficult.6 Fractures mostly result in anterior, anterolateral or anteromedial displacement of the epiphysis and physis relative to the metaphysis.1 Open reduction and internal fixation is recommended whenever the physis is severely displaced or comminuted, that is, in types IIB, IIIA, IIIB and IV.17 The surgical aim must be to restore both the extensor mechanism and the congruency of the knee joint. In the case reports described the majority of the cases reported are fixed using cannulated screws.22–25
In our case the extent of the injury was not realised at first presentation and internal fixation was attempted with an extra-articular approach and without further investigations. Unfortunately the fracture was found to be displaced 1 week postoperatively and the patient had to undergo further surgery to correct this displacement. This report highlights the role CT can play in these cases. The two 3D reconstructed images provide considerably more information on the fracture pattern than the plain radiographs. We would recommend obtaining a preoperative CT scan if extension of the fracture into the tibial physis is suspected. This allows appreciation of the fracture configuration prior to surgery and aids planning of the reduction and fixation methods. This use of CT imaging in complex fracture patterns is also recommended by other authors.26 During the second operation, arthroscopy was used to ensure accurate fracture reduction, an approach recommended previously.25 We had difficulty visualising the anterior articular surface under the anterior meniscal horns with a 30° scope. A 70° arthroscope would have helped tackle this difficulty and should have allowed the surgeon to visualise the anterior joint surface more easily. In type III injuries the tuberosity fracture propagates into the anterior tibial physis and the ability to see this area intra-operatively allows the surgeon to confirm fracture reduction. We would recommend that before attempting fixation of these injuries a 70° arthroscope is available to ensure optimal reduction.
Learning point.
- Tibial tuberosity fractures with extension into the tibial physis are rare, and appreciating fracture patterns from plain radiographs alone may be difficult. We recommend the following in order to achieve direct anatomical reduction:
- A pre-operative CT scan with 3D reconstructions to fully appreciate the fracture configuration;
- Use of an arthroscope intraoperatively to aid and confirm the accuracy of reduction.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shelton WR, Canale ST. Fractures of the tibia through the proximal tibial epiphyseal cartilage. J Bone Joint Surg 1979;2013:167–73 [PubMed] [Google Scholar]
- 2.Bolesta MJ, Fitch RD. Tibial tubercle avulsions. J Pediatr Orthop 1986;2013:186–92 [DOI] [PubMed] [Google Scholar]
- 3.Aitken AP. Fractures of the proximal tibial epiphysial cartilage. Clin Orthop 1965;2013:92–7 [PubMed] [Google Scholar]
- 4.Aitken AP, Ingersoll RE. Fractures of the proximal tibial epiphyseal cartilage. J Bone Joint Surg 1956;2013:787–96 [PubMed] [Google Scholar]
- 5.Smillie IS. Injuries to the knee joint. 4th edn Edinburgh: Churchill Livingstone, 1970:202–5 [Google Scholar]
- 6.Burkhart SS, Peterson HA. Fractures of the proximal tibial epiphysis. J Bone Joint Surg 1979;2013:1000–2 [PubMed] [Google Scholar]
- 7.Ogden JA, Southwick WO. Osgood-Schlatter's disease and tibial tuberosity development. Clin Orthop 1976;2013:180–6 [PubMed] [Google Scholar]
- 8.Ogden JA, Hempton RF, Southwick WO. Development of the tibial tuberosity. Anat Rec 1975;2013:431–45 [DOI] [PubMed] [Google Scholar]
- 9.Ehrenborg G. The Osgood-Schlatter lesion. A clinical and experimental study. Acta Chir Scan 1962;2013:1–36 [PubMed] [Google Scholar]
- 10.Ogden JA, Tross RB, Murphy MJ. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg 1980;2013:205–15 [PubMed] [Google Scholar]
- 11.Ergun M, Taskiran E, Ozgurbuz C. Simultaneous bilateral tibial tubercle avulsion in a basketball player. Knee Surg Sports Traumatol Arthrosc 2003;2013:163–6 [DOI] [PubMed] [Google Scholar]
- 12.Mosier SM, Stanitski CLL. Acute tibial tubercle avulsion fractures. J Pediatr Orthop 2004;2013:181–4 [DOI] [PubMed] [Google Scholar]
- 13.Hamilton SW, Gibson PH. Simultaneous bilateral avulsion fractures of the tibial tuberosity in adolescence: a case report and review of over 50 years of literature. Knee 2006;2013:404–7 [DOI] [PubMed] [Google Scholar]
- 14.Watson-Jones R. Fractures and joint injuries. vol 2013, 5th edn Baltimore: Williams & Wilkins, 1976:1048–50 [Google Scholar]
- 15.Ryu RKN, Debenham JO. An unusual avulsion fracture of the proximal tibial epiphysis. Clin Orthop 1985;2013:181–4 [PubMed] [Google Scholar]
- 16.McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am 2003;2013:397–403 [DOI] [PubMed] [Google Scholar]
- 17.Choi NH, Kim NM. Tibial tuberosity avulsion fracture combined with meniscal tear. Arthroscopy 1999;2013:766–9 [DOI] [PubMed] [Google Scholar]
- 18.Falster O, Hasselbach H. Avulsion fracture of the tibial tuberosity with combined ligament and meniscal tear. Am J Sports Med 1992;2013:82–3 [DOI] [PubMed] [Google Scholar]
- 19.Lipscomb AB, Gilbert PP, Johnston RK, et al. Fracture of the tibial tuberosity with associated ligamentous and meniscal tears. A case report. J Bone Joint Surg Am 1984;2013:790–2 [PubMed] [Google Scholar]
- 20.Mayba II. Avulsion fracture of the tibial tubercle apophysis with avulsion of patellar ligament. J Pediatr Orthop 1982;2013:303–5 [DOI] [PubMed] [Google Scholar]
- 21.Ozer H, Turanli S, Baltaci G, et al. Avulsion of the tibial tuberosity with a lateral plateau rim fracture: case report. Knee Surg Sports Traumatol Arthrosc 2002;2013:310–12 [DOI] [PubMed] [Google Scholar]
- 22.Abalo A, Akakpo-numado KG, Dossim A, et al. Avulsion fractures of the tibial tubercle. J Orthop Surg (Hong Kong) 2008;2013:308–11 [DOI] [PubMed] [Google Scholar]
- 23.Frey S, Hosalkar H, Cameron DB, et al. Tibial tuberosity fractures in adolescent. J Child Orthop 2008;2013:469–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brey JM, Conoley J, Canale ST, et al. Tibial tuberosity fractures in adolescents: is a posterior metaphyseal fracture component a predictor of complications? J Pediatr Orthop 2012;2013:561–6 [DOI] [PubMed] [Google Scholar]
- 25.Slobogean GP, Mulpuri K, Alvarez CM, et al. Comminuted simultaneous bilateral tibial tubercle avulsion fractures: a case report. J Orthop Surg 2006;2013:319–21 [DOI] [PubMed] [Google Scholar]
- 26.Jalgaonkar AA, Dachepalli S, Al Watter Z, et al. Atypical tibial tuberosity fracture in an adolescent. Orthopaedics 2011;2013:215–18 [DOI] [PubMed] [Google Scholar]