Abstract
Involvement of the skeletal system is a common complication of brucellosis. However, muscle involvement or paraspinal abscess formation are rare complications. Paraspinal abscess usually develops secondary to spondylitis. A case is reported here of a 33-year-old woman with symptoms of night sweats, fever and low back pain. Rose-Bengal test for brucellosis was positive and Brucella standard tube agglutination test was positive at a titre of 1/160. The diagnosis was made on MRI. The patient was treated with doxycycline and rifampin daily for 16 weeks. On day 14 of treatment, decline was observed in the patient’s symptoms. In the presence of inflammatory lower back pain and fever, brucellosis should be considered particularly in the endemic areas. Furthermore, tuberculosis should be remembered in the differential diagnosis when a spinal epidural abscess is determined.
Background
Brucellosis is a systemic disease that affects many tissues and organs, especially the reticuloendothelial and musculoskeletal systems. Spinal epidural abscess (SEA) development in brucellosis is a quite rare but serious complication. In order to avoid this complication, early diagnosis and treatment is important.
Case presentation
A 33-year-old woman was admitted to our hospital due to night sweats, fever and low back pain of 2 weeks’ duration. She was a housewife. She had recently drunk unpasteurised milk. On clinical examination, there was severe low back pain and limitation in the motion of the back in all directions. The straight leg raising test on the right side was positive in 40° elevation. Neurological examination was normal. Laboratory findings were normal, including complete blood count, rheumatoid factor, urea, creatine, aspartate aminotransferase, alanine transaminase, and erythrocyte sedimentation rate was 43 mm/h and C reactive protein 3.04 mg/dL. Rose-Bengal test for brucellosis was positive and Brucella standard tube agglutination test was positive at a titre of 1/160. In the tuberculin skin test anergy was found.
Investigations
MRI of the lumbar spine demonstrated spondylodiscitis in the L4–L5 vertebral bodies and intervertebral disc, and SEA extending to the paravertebral and anterior epidural spaces. T2-weighted MRI revealed increased heterogeneous signal intensity. A heterogeneously contrast-enhanced mass that caused root compression was also observed at the same vertebra (figures 1 and 2).
Figure 1.

MRI of the lumbar spine (T2-weighted sagittal) demonstrated spondylodiscitis in the L3–L4 vertebral bodies and intervertebral disc and spinal epidural abscess extending to the paravertebral and anterior epidural spaces (arrows).
Figure 2.
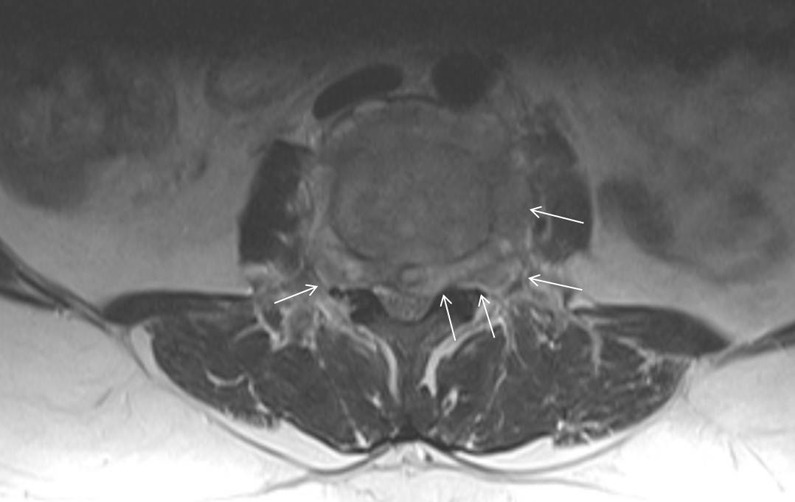
MRI of the lumbar spine (T2-weighted axial) demonstrated the spinal epidural abscess extending to the paravertebral and anterior epidural spaces (arrows).
Differential diagnosis
Tuberculosis and pyogenic infection should be remembered in the differential diagnosis when a SEA is determined.
Treatment
The patient was treated with 200 mg doxycycline and 600 mg rifampicin daily for 16 weeks.
Outcome and follow-up
There was low back pain and limitation in the motion of the back in all directions on clinical examination after 7 days of treatment with antibiotics. Neurological examination was normal. On day 14 of treatment, decline was observed in the patient’s symptoms and the patient was discharged. On the 8th and 16th weeks follow-up physical and neurological examinations were normal.
Discussion
Brucellosis is one of the zoonotic infections widely seen around the world. It is transmitted by contact with secretions of infected animals or consumption of unpasteurised milk and cheese. Because of high morbidity, brucellosis is one of the public health problems leading a significant economic loss in developing countries.1 In endemic areas, incidence is between 1–200 and 100 000.2 Brucellosis is endemic in the Middle East, in South and Central America and the eastern Mediterranean region, where Turkey is located.3 Brucellae are aerobic, facultative intracellular, Gram-negative coccobacilli.4 Osteoarticular involvement is the most common complication and includes spondylitis, sacroiliitis and arthritis. Spondylitis is its most prevalent clinical form in adults and a serious complication of brucellosis may occur more common in patients not treated effectively or in the elderly. The lumbar spine is more often affected than thoracic and cervical spine. Sacroiliitis and arthritis due to Brucella infection usually seen in the first three decades, although spinal brucellosis often affects older people.5
SEA usually develops secondary to spondylitis and is seen extremely rare. The incidence of SEA has been reported as 1/10 000 hospital admission.6 Staphylococcus aureus is the pathogen in the 60% of the SEA.7 The most common sources of infection are skin abscesses and furuncles. Immunocompromised patients with diabetes mellitus, alcoholism or chronic renal failure are at risk. Spinal procedures such as epidural anaesthesia or analgesia, spinal surgery or trauma are the other risk factors. In 20% of cases a predisposing factor cannot be found.8 Infection of the epidural space occurs by haematogenous spread or local spread from adjacent tissues.9 Several cases of brucellosis-related epidural abscess have been reported in the literatüre.3 9–11 Osteomyelitis frequently occurs as localised brucellosis in the vertebrae, with the lumbosacral area the most frequent site. The incidence of spondylitis in Brucellar infection is about 10%, however, development of SEA is rare but the formation of SEA has been reported in less than 1.5% of the neurological complications and generally this is associated with spondylitis.4 9 10
In the cases of SEA due to Brucella infection, spinal pain with palpation, local tenderness or fever can be seen clinically. However, these findings are not specific. In our case, the symptoms were inflammatory backache, spinal pain with palpation, radiating pain in the right leg and limitation in the motion of the waist. These symptoms persisted for 2 weeks. There were no systemic symptoms except fever. Diagnosis of Brucella infection requires isolation of the bacterium from blood or tissue samples. Erythrocyte sedimentation rate and C reactive protein are usually increased, but non-specific symptoms. The Rose-Bengal test is a rapid slide-type agglutination assay performed with a stained Brucella abortus suspension at pH 3.6–3.7 and plain serum. Because of its simplicity, it is often used as a screening test in human brucellosis and would be optimal for small laboratories with limited means. Despite the use of Rose-Bengal test as a screening test, the standard tube agglutination (STA) test at a titre of 1/160 has very high sensitivity and specificity.4 In our case blood culture and Rose-Bengal test was positive and the titre of STA test was 1/160.
MRI is the best diagnostic imaging method for SEA. Spondylodiscitis, spinal cord and nevre root compression can be determined with an MRI. Typical MRI findings of Brucella spondylitis can be observed within a month after the onset of symptoms.12
Diagnosis and treatment of vertebrae infections due to tuberculosis or Brucella infection is quite difficult. Because they are both intracellular pathogens and it is difficult to isolate and determine them in a short time. They may cause neurological complications and abnormal posture due to vertebrae destruction. Therefore, to make the correct diagnosis of spine infections due to tuberculosis and Brucella infection is essential in endemic areas.13 In chronic brucellosis, it is less likely to produce the organism from blood and bone marrow because there is often vertebral involvement existing. In vertebral infections due to Brucella infection and tuberculosis, the diagnosis is made by clinical, laboratory and radiological findings because it is often difficult to reach infected area and produce microorganisms. In spondylitis due to tuberculosis, CT or MRI can demonstrate large abscesses with attached rims and marked encroachment in spinal canal; however in Brucella spondylitis, endplate defect like Schmorl's nodule, muscle fat line deletion, formation of paraspinal granulation tissue, intervertebral disc space narrowing and gas in the vertebral disc can be determined.14 In spondylitis due to Brucella, vertebral collapse, angulations and abscess formation of vertebral column are not often observed. In our case, as opposed to the noticeable findings of Brucella spondylitis, abscess formation was determined.
Treatment of Brucella spondylitis should contain dual antibiotic therapy and duration of the treatment should be 12 weeks.15 It is shown that doxycycline (200 mg/day, 12 weeks) and streptomycin (1 g/day intramuscularly, the first 14–21 days) therapy is more effective than doxycycline–rifampicin (15 mg/kg/day) combination.16 However, doxycycline and rifampicin are an oral regimen preferred particularly in areas with less well-developed health infrastructure.17 As an alternative therapy ciprofloxacin (1000 mg/day) and rifampicin (15 mg/kg/day) combination can be used for at least 12 weeks.16
Treatment period is as important as the selection of the antimicrobial agent. In a meta-analysis it is shown that 43% of patients treated for less than 6 weeks, and 17% of patients treated longer than 12 weeks, treated unsuccessfully.17 In our case, at the end of the 16 weeks of treatment, the patient's symptoms recovered completely.
Surgical treatment is indicated in case of persistence or progression of neurological deficit, spinal instability and progressive collapse of vertebrae and non-responsiveness to antimicrobial therapy.16 Lesions due to Brucella infection are generally encapsulated, elastic, moderately vascular and adherent to neural structures thus complicating the dissection from neural elements. Iatrogenic transmission of organism into the cerebrospinal fluid could lead to neurobrucellosis.10
In conclusion, epidural abscess in brucellosis is a rare but progressive disease that can lead to spinal cord compression and permanent paralysis. Therefore, in the presence of inflammatory lower back pain and fever, brucellosis should be considered particularly in the endemic areas. Furthermore, tuberculosis and pyogenic infection should be remembered in the differential diagnosis when SEA is determined.
Learning points.
Brucellosis should be considered in the differential diagnosis of painful vertebral syndromes in endemic areas.
Brucella spondylitis and abscess is suspected, MRI should be applied and appropriate treatment should be initiated as soon as possible.
Tuberculosis and pyogenic infection should be remembered in the differential diagnosis when spinal epidural abscess is determined.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bosilkovski M, Dimzova M, Grozdanovski K. Natural history of brucellosis in an endemic region in different time periods. Acta Clin Croat 2009;2013:41–6 [PubMed] [Google Scholar]
- 2.Stanek G, Strle F. Lyme borreliosis. Lancet 2003;2013:1639–47 [DOI] [PubMed] [Google Scholar]
- 3.Gorgulu A, Albayrak BS, Gorgulu E, et al. Spinal epidural abscess due to Brucella. Surg Neurol 2006;2013:141–6 [DOI] [PubMed] [Google Scholar]
- 4.Solera J, Lozano E, Martinez-Alfaro E, et al. Brucellar spondylitis: review of 35 cases and literature survey. Clin Infect Dis 1999;2013:1440–9 [DOI] [PubMed] [Google Scholar]
- 5.ChelliBouaziz M, Ladeb MF, Chakroun M, et al. Spinal brucellosis: a review. Skeletal Radiol 2008;2013:785–90 [DOI] [PubMed] [Google Scholar]
- 6.Tacconi L, Johnston FG, Symon L. Spinal epidural abscess—review of 10 cases. Acta Neurochir (Wien) 1996;2013:520–3 [DOI] [PubMed] [Google Scholar]
- 7.Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM 2008;2013:1–12 [DOI] [PubMed] [Google Scholar]
- 8.Gellin BG, Weingarten K, Gamache FW, Jr, et al. Epidural abscess. In: Scheld WM, Whitley RJ, Durack DT. eds. Infections of the central nervous system. 2nd edn Philadelphia: Lippincott-Raven Publishers, 1997:507 [Google Scholar]
- 9.Izci Y. Lumbosacral spinal epidural abscess caused by Brucella melitensis. Acta Neurochir (Wien) 2005;2013:1207–9; discussion 9 [DOI] [PubMed] [Google Scholar]
- 10.Daglioglu E, Bayazit N, Okay O, et al. Lumbar epidural abscess caused by Brucella species: report of two cases. Neurocirugia (Astur) 2009;2013:159–62 [DOI] [PubMed] [Google Scholar]
- 11.Paz JF, Alvarez FJ, Roda JM, et al. Spinal epidural abscess caused by Brucella: case report. J Neurosurg Sci 1994;2013:245–9 [PubMed] [Google Scholar]
- 12.Pina MA, Ara JR, Modrego PJ, et al. Brucellar spinal epidural abscess. Eur J Neurol 1999;2013:87–9 [DOI] [PubMed] [Google Scholar]
- 13.Colmenero JD, Jimenez-Mejias ME, Sanchez-Lora FJ, et al. Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: a descriptive and comparative study of 219 cases. Ann Rheum Dis 1997;2013:709–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharif HS, Aideyan OA, Clark DC, et al. Brucellar and tuberculous spondylitis: comparative imaging features. Radiology 1989;2013:419–25 [DOI] [PubMed] [Google Scholar]
- 15.Colmenero JD, Ruiz-Mesa JD, Plata A, et al. Clinical findings, therapeutic approach, and outcome of brucellar vertebral osteomyelitis. Clin Infect Dis 2008;2013:426–33 [DOI] [PubMed] [Google Scholar]
- 16.Alp E, Doganay M. Current therapeutic strategy in spinal brucellosis. Int J Infect Dis 2008;2013:573–7 [DOI] [PubMed] [Google Scholar]
- 17.Pappas G, Seitaridis S, Akritidis N, et al. Treatment of brucella spondylitis: lessons from an impossible meta-analysis and initial report of efficacy of a fluoroquinolone-containing regimen. Int J Antimicrob Agents 2004;2013:502–7 [DOI] [PubMed] [Google Scholar]


