Abstract
The study described diagnostic and therapeutic processes for an exceptional congenital female genital anomaly involving a 15-year-old girl with progressive dysmenorrhoea and intense abdominal pain, and analyses pathogenesis of embryological anomalies associated with uterine duplicity (UD). Diagnostic methodology is analysed; treatment is described; and recommendations are provided. For the study of anomalies such as UD, we recommend the use of an ultrasound, vaginoscopy, MRI and laparoscopy imaging. Keeping in mind that hemihysterectomy should only be performed in cases with endometriosis or other unusual circumstances, surgical treatment should be avoided. A complete study based on gynaecological examination and ultrasound should be performed in adolescents with severe and progressive dysmenorrhoea. Based on the findings, imaging tests such as MRI and, if necessary, laparoscopy coinciding with menstruation, should be conducted before opting for surgical treatment.
Background
Uterine duplicity (UD) is a rare congenital malformation within the group of uterine anomalies due to the absence of the ‘inducting’ function of the injured mesonephric duct on the Müllerian duct.1 Depending on the embryological development stage, different degrees of anatomical severity need to be considered. This in fact implies a variety of symptoms associated with ipsilateral renal agenesis.
It is our recommendation that the diagnostic study must be thorough and carefully conducted due to the fact that this condition usually involves young patients who are not sexually active.2 The study should include an ultrasound, vaginoscopy, MRI, an examination under anaesthesia and sometimes a laparoscopy.
We decided to document this particular case because treatment of these patients must be careful and may be expectant, or may require opening marsupialisation of the vaginal wall to drain the haematocolpos,3 4 its puncture,5 or even elimination of a cavitary rudimentary horn.
Case presentation
This case reported a 15-year-old girl with progressive dysmenorrhoea and abdominal pain since menarche (at 13 years). Her medical record revealed the absence of the right kidney and lumbar 3–5 vertebral anomalies in addition to scoliosis. Examination showed a normal phenotype, with appropriate normal pubarche, thelarche and adrenarche. External genitalia were normal and the hymen was intact.
Investigations
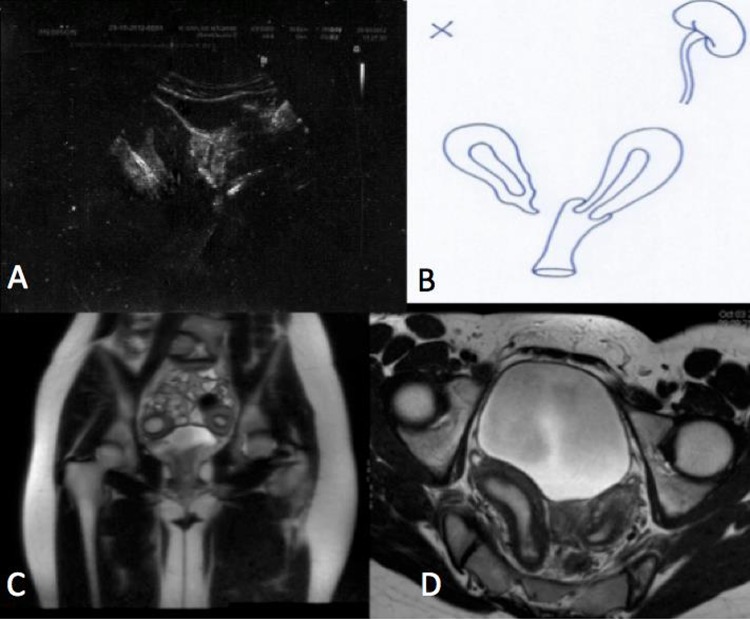
Abdominal and transrectal ultrasound revealed the presence of two clearly separated uterine bodies (figure 1) with discrete haematometra on the right side and a normal endometrium on the left side. There was no haematocolpos and both ovaries were normal. Abdominal ultrasound revealed right renal agenesis. MRI confirmed the anomaly of the last lumbar vertebrae and the ultrasound's suggestion: UD with right uterine cavity and discrete haematometra, without haematosalpinx, and ending in a small fibrous pouch (figure 1) completely separated from the left hemiuterus, which correctly terminates into a normal left hemivagina. Left renal agenesis was confirmed. A vaginoscopy during menstruation ruled out any interseptal communication, and no vaginal wall swelling was detected. The left hemivagina was normal and there was a normal cervix corresponding to the left hemiuterus.
Figure 1.
(A) Abdominal ultrasound with haematometra of the right hemiuterus and clear separation of the left uterine body. (B) Diagram of the congenital anomaly after performing the ultrasound and MRI. (C) MRI T2 coronal image showing two uterine bodies. (D) MRI T1 axial image showing the distension of the right endometrial cavity and the separation of both hemiuteri. On the right is the uterus with haematometra and cervicovaginal agenesis. On the left is a normal uterus communicated with an unobstructed hemivagina.
Examination under anaesthesia and diagnostic/therapeutic laparoscopy were performed on the third day of menstruation. A large quantity of menstrual blood throughout the peritoneal cavity, endometriotic spots, UD and normal ovaries (figure 2) were confirmed.
Figure 2.
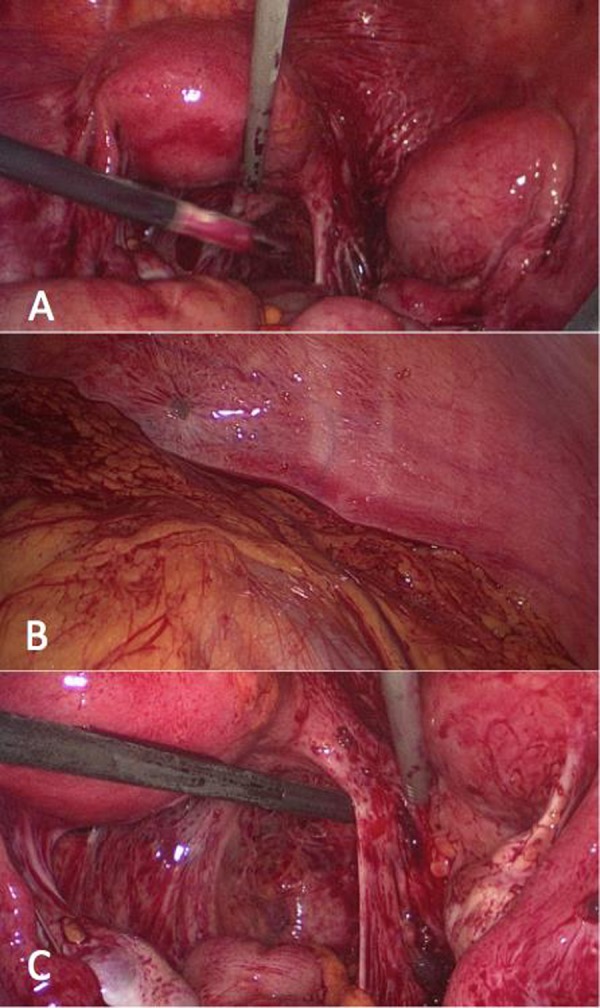
(A) Laparoscopy showing the two separated hemiuteri. (B) Retrograde menstrual blood from the right hemiuterus was found throughout the entire abdominal cavity. Signs of peritoneal endometriosis can be seen. (C) Further signs of peritoneal endometriosis and peritoneal anomalies (Allen-Master syndrome).
Treatment
A right hemihysterectomy and salpingectomy were performed (figure 3), confirming the cervicovaginal atresia and discrete haematometra described in MRI (figure 4).
Figure 3.
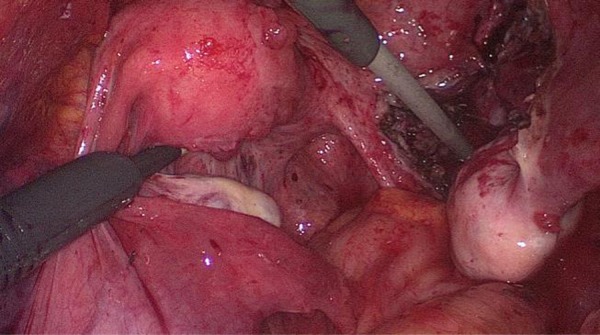
Treatment was a right hemihysterectomy and salpingectomy. This is how the lesser pelvis remained following surgery.
Figure 4.
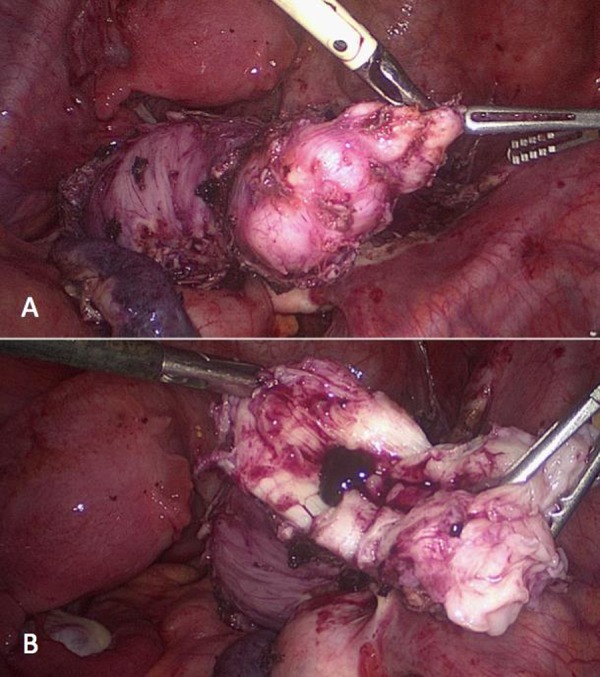
(A) The right hemiuterus ended in a non-cavitated fibrous tissue. (B) The haematometra was confirmed once the hemiuterus was opened.
Outcome and follow-up
The postoperative course was satisfactory; and after 2 months from surgery, the young woman had two normal menses and was thrilled with the results.
Discussion
UD, with one hemiuteri having a blind hemivagina (or cervicovaginal atresia) along with ipsilateral renal agenesis, is an uncommon anomaly. Müllerian expression of mesonephric anomalies with absence of the Wolffian duct opening to the urogenital sinus results in a blind or atresic vagina and sprouting of the ureteral bud that leads to renal agenesis. UD occurs due to the lack of stimulation of the mesonephric ducts on the Müllerian ducts. If there is ectopic sprouting of the ureteral bud, renal hypoplasia could result in renal agenesis along with the appearance of an open ectopic ureter in the blind vagina. Additionally, if this blind vagina is associated with some anomaly in urogenital sinus development, a congenital vesicovaginal fistula (pseudofistula with menouria) may result.1 2
Müllerian anomalies are present in 2–3% of women of childbearing age,4 5 one-half with renal agenesis and very few with complete separation of both hemiuteri. Commonly, they are associated with other congenital anomalies such as vertebral anomalies.
UD occurs in up to five different clinical varieties.1 The one corresponding to this particular case is the complete unilateral vaginal agenesis, or cervicovaginal, without communication between both hemiuteri. Others do have communication between both hemiuteri, but they do not present dysmenorrhoea, and the hysterosalpingogram image resembles a bicornis-unicollis uterus.1 Others are bicornuate uteri or uteri didelphys associated with large haematocolpos in a blind hemivagina and the corresponding ipsilateral renal agenesis that do present dysmenorrhoea, pain and abdominal masses. Cases with an atresic hemivagina and communicated hemiuteri are less affecting, and could result in certain swelling in the anterolateral wall of the vagina like Gartner's pseudocyst; the patients present postmenstrual spotting and abdominal pain. This entity has been described as the Herlyn-Werner-Wunderlich syndrome, which can involve up to 10% of those belonging to the group of Müllerian anomalies.4 5 The fifth anatomoclinical entity is that presenting a small intervaginal opening or a high septum by abnormal reabsorption of the vaginal septum; it is symptomless, although it can refer dyspareunia and have reproductive problems or pregnancies with breech presentations.1
UD with ipsilateral renal agenesis belongs to group 2 of the classification by Acién.1 It must be distinguished from group 3, which contains cases of isolated anomalies of the Müllerian ducts, Müllerian tubercle, or both (unicornuate uterus, uterus didelphys, Rokitansky, etc.),1 without renal agenesis or hypoplasia. These entities have normally been described and classified according to the system of the American Fertility Society6 7 that are not based on the embryological origin of the entity like that of Acién.1
The young woman in our case under study had not had sexual intercourse but the abdominal and transrectal route for the three-dimensional (3D) ultrasound (figure 1) allowed verification of a clear separation between the two uterine bodies and the absence of haematocolpos. Del Vescovo et al4 recommend ultrasound as a first diagnostic step, although confirmation by MRI and laparoscopy are the definitive techniques. Bermejo et al8 propose ultrasound, especially 3D, as evidence of high sensitivity and its advantage for providing clear correlation with MRI8; although limited by observers’ skill levels, the difficulty of the transrectal route in young women whose hymens are intact, and the need for a good scanner. In the case presented, the ultrasound was very useful and had a high correlation with the findings from surgery. Outpatient vaginoscopy is a basic complementary examination that is performed without complications and it is also easy to perform, inexpensive and helpful with differential diagnosis.2
MRI with contrast defined the different anatomical planes with separation of the two hemiuteri and clearly showed the right cervicovaginal agenesis (figure 1). Additionally, it confirmed the renal agenesis, ruling out renal hypoplasia and the ectopic ureter that may appear in some cases with mixed anomalies that are expressed with menouria.2
With the assumption of UD without communication between the hemiuteri, and facing suspected endometriosis (progressive dysmenorrhoea), examination under anaesthesia and laparoscopy were performed. Laparoscopy confirmed a diffuse endometriosis (figure 2), observing Allen-Master peritoneal defects with recent retrograde menstrual blood (third menstrual day). The hemihysterectomy was performed without difficulty. The atresic vagina was a short fibrous cord ending at a point not in contact with the normal left hemivagina (figure 3). The histopathology was of a normal myometrium, endometrial shedding, small haematometra and cervical and vaginal agenesis.
Some studies question the effectiveness and benefits of the excision of a rudimentary hemiuterus for dysmenorrhoea.4 However, in this particular case, we believe that the findings observed during laparoscopy demonstrated a clear relationship between the presence of that hemiuterus with a blind vagina and incipient endometriosis. Therefore, the hemihysterectomy was considered convenient. The actual clinical improvement in the young woman confirms that this treatment was reasonable. Grimbizis and Campo7 defend the laparoscopic hemihysterectomy choice in IVa classification cases (duplication with dysplastic hemiuterus but with haematometra). Del Vescovo4 feels the same way, confirming its valuable use in cases of endometriosis. Tzialidou-Palermo et al3 perform a comparative analysis of therapeutic strategies, but in 99% of the cases the surgery was about the intervaginal septum, and only two cases required the Strassman technique.
Learning points.
All gynaecologists should consider that intense dysmenorrhoea and abdominal pain in adolescent girls and young women might be caused by congenital genitourinary anomalies.
Uterine duplicity with a hemiuterus having cervicovaginal atresia and retrograde menstruation is a rare anomaly related with mesonephric anomalies, associated with ipsilateral renal agenesis and other malformations such as those skeletal.
Thorough diagnostic studies are essential before proposing treatment. Abdominal and transrectal ultrasound, vaginoscopy, and MRI are indispensable tests.
Treatment should be meditated, preceded by careful examination under anaesthesia, and through laparoscopic surgery previously agreed upon by both the young female as well as her parents, considering the advantages and disadvantages of hemihysterectomy with salpingectomy.
Footnotes
Contributors: JCM-E wrote the case. AP-M reviewed and submitted the manuscript. ABO-G got the references and HB-G worked with JCM-E in getting the clinical data of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned, externally peer reviewed.
References
- 1.Acién P, Acién M. The history of female genital tract malformation classifications and proposal of an updated system. Hum Reprod Update 2011;2013:693–705 [DOI] [PubMed] [Google Scholar]
- 2.Martínez Escoriza JC, Lobato JJ, Lorda E, et al. Congenital vesicovaginal fistula with menouria. An anomaly of the urogenital sinus. Eur J Obstet Gynecol Reprod Biol 2011;2013:472–5 [DOI] [PubMed] [Google Scholar]
- 3.Tzialidou-Palermo I, von Kaisenberg CS, García-Rocha GJ, et al. Diagnostic challenges of hemihematocolpos and dysmenorrhea in adolescents: obstructed hemivagina, didelphys or bicornuate uterus and renal aplasia is a rare female genital malformation. Arch Gynecol Obstet 2012;2013:785–91 [DOI] [PubMed] [Google Scholar]
- 4.Del Vescovo R, Battisti S, Di Paola V, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging 2012;2013:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox D, Ching BH. Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J Radiol Case Rep 2012;2013:9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimbizis GF, Campo R. Congenital malformations of the female genital tract: the need for a new classification system. Fertil Steril 2010;2013:401–7 [DOI] [PubMed] [Google Scholar]
- 7.Grimbizis GF, Campo R. Clinical approach for the classification of congenital uterine malformations. Gynecol Surg 2012;2013:119–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bermejo C, Martínez Ten P, Cantarero R, et al. Three-dimensional ultrasound in the diagnosis of Müllerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet Gynecol 2010;2013:593–601 [DOI] [PubMed] [Google Scholar]