Abstract
We report a case of a healthy young man presenting with 1-week history of diarrhoea, acute abdominal pain and weight loss. Laboratory investigation showed very high peripheral eosinophils levels. After exclusion of the other causes of eosinophilia, a histological bowel sample analysis revealed marked eosinophilic infiltration of a small bowel mucosal layer which confirmed the suspicion of eosinophilic enteritis. Unlike most of the described cases, this patient did not require any specific treatment. Eosinophilic gastroenteritis is a rare and heterogeneous disease that is probably underdiagnosed in clinical practice because it requires a high degree of suspicion and an endoscopic biopsy for definite diagnosis.
Background
Eosinophilic enteritis is a rare condition, the exact incidence of which is unknown, and fewer than 350 cases have been reported in literature.1 Despite several epidemiological and clinical features suggesting an allergic component, its aetiology is still unknown1–3 and, like our patient, there are cases with non-allergic background. The severity of its clinical presentation is variable and related to which layer of the bowel is involved and to the extension of the eosinophilic infiltration.4–6 Therefore, it is a diagnosis that should be considered in a variety of patients with gastrointestinal symptoms before making other diagnoses such as irritable bowel syndrome. Its prognosis is very good and only rarely has death been reported but morbidity can be important due to malnutrition, intestinal obstruction and perforation, if not treated.7 8
Case presentation
A healthy 18-year-old man, without known allergies, previous medication, history of drug allergy, asthma, allergic rhinitis or recent trips, presented watery diarrhoea without blood or mucus in the stool, abdominal pain and non-quantified weight loss, during 1 week. There were no relevant findings in the physical examination.
Investigations
The laboratory tests revealed a serum eosinophilia (3700 cells/μL—24%) and slightly increased serum IgE levels (220 UI/mL). The sedimentation rate, liver function, vitamin B12 and folates levels and HIV serology were negative or normal. Stool samples sent for culture, Gram stain and examination for ova and parasites were all negative.
With no definitive diagnosis a bland, soft diet, low in saturated fat and cholesterol was initiated, without an association with pharmacological therapy.
Two days later, the serum levels of eosinophils increased (10 510 cells/μL—55%) and the rest of diagnostic workup was rapidly performed.
The peripheral blood smear, bone marrow biopsy and myelogram were unrevealing. The full body CT (figure 1) showed a homogenous hepatomegaly and multiple lymph node enlargements (10–12 mm) adjacent to the coeliac trunk, lateroaortic and mesenteric arteries.
Figure 1.
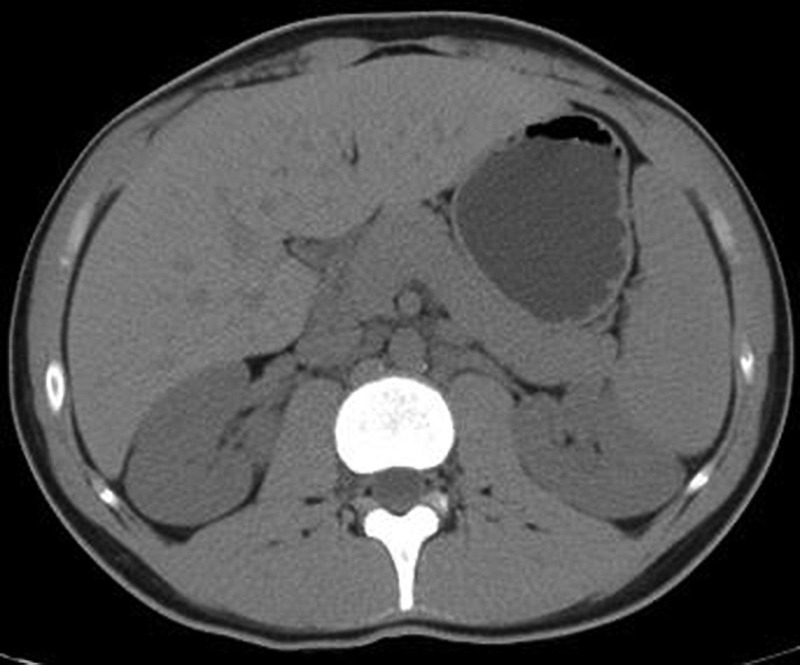
Full body CT scan—homogenous hepatomegaly and multiple lymph node enlargements (10–12 mm) adjacent to the coeliac trunk, lateroaortic and mesenteric arteries.
Considering the lack of diagnosis and the worsening of eosinophilia a colonoscopy was performed, which documented a nodular and grained mucosa in the distal ileum and three erosions in the caécum (figures 2 and 3). Histological findings consisted of a diffuse eosinophilic inflammatory infiltration in the mucosa also observed occasionally in the submucosal layer of the terminal ileum (figures 4 and 5). These findings associated with the exclusion of other aetiological possibilities led to the definitive diagnosis of eosinophilic enteritis.
Figure 2.
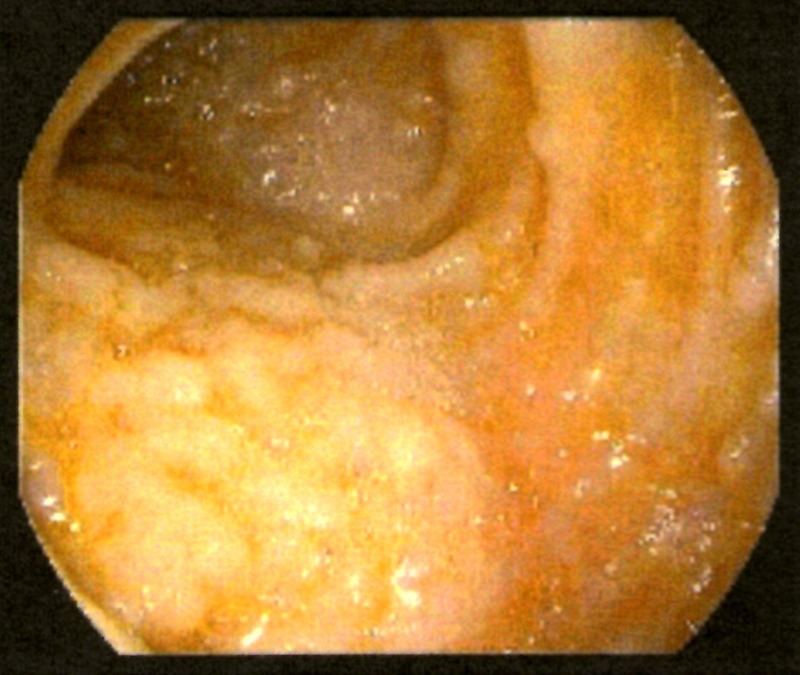
Colonoscopy—nodular and grained mucosa in the distal ileum.
Figure 3.
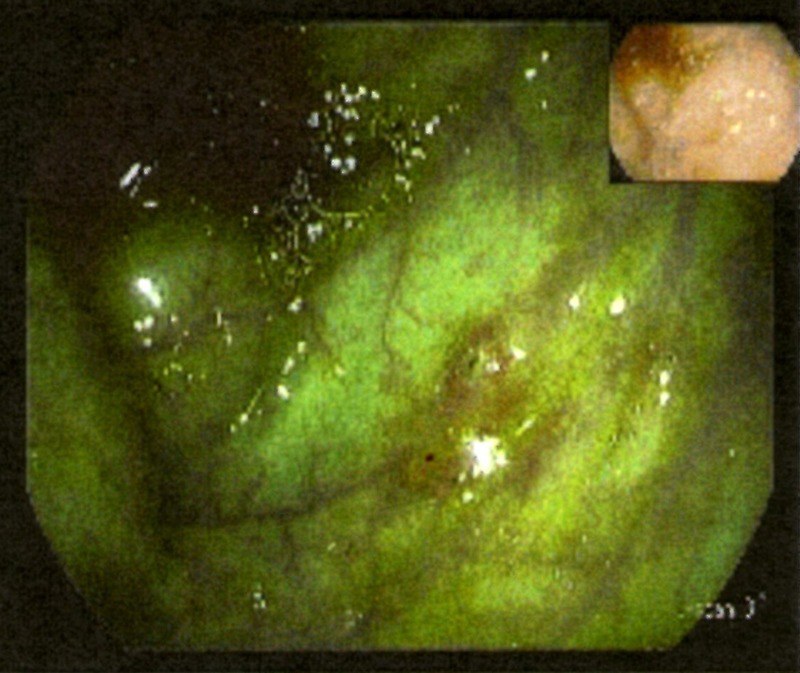
Colonoscopy—three erosions in the cécum.
Figure 4.
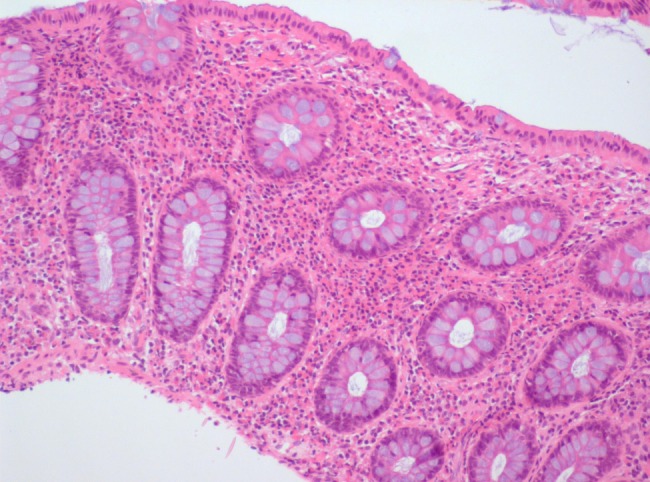
Microscopic appearance of ileum biopsy—eosinophilic inflammatory infiltration.
Figure 5.
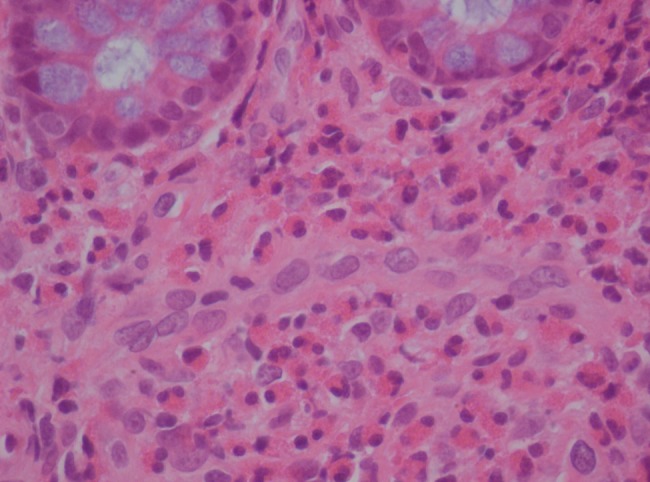
Microscopic appearance of ileum biopsy—more than 50 eosinophils per high-power field. Sometimes localised eosinophilic infiltrates may cause crypt hyperplasia, epithelial cell necrosis and villous atrophy.
Differential diagnosis
Eosinophilic gastroenteritis should always be suspected in any patient with gastrointestinal symptoms associated with peripheral eosinophilia. Nevertheless, other diseases need to be considered before making this definitive diagnosis: allergic food and drug reactions; infectious diseases such as intestinal parasites (Ancylostoma, Anisakis, Ascaris, Strongyloides, Toxocara, Trichiura, Capillaria, Trichinella, etc), fungal and HIV and other retroviral infections; haematological and neoplastic disorders such as hypereosinophilic syndromes, mastocistosis, leukaemia/lymphoma and gastric or colon cancer; irritable bowel syndrome and rheumatic diseases like the vasculitic phase of the Churg-Strauss syndrome and polyarteritis nodosa. However, differential diagnosis can be made in almost all cases by suspicion in the appropriate clinical context, simple laboratory tests and endoscopic or full thickness biopsies.
Treatment
No specific treatment was required. Only a bland, soft diet, low in saturated fat and cholesterol was prescribed.
Outcome and follow-up
A spontaneous and progressive recovery occurred with no specific treatment and in a week’s time the patient was asymptomatic with a marked declining in the peripheral eosinophilia, without evidence of the disease recurrence in the next 3 months.
Discussion
Eosinophilic gastroenteritis is an uncommon gastrointestinal disease which can affect patients of any age but typically appears between the third and the fifth decade with male predominance.6 9 10 Its exact prevalence and underlying molecular mechanism are unknown. However, a history of atopy or food allergies is often present.1–3
Eosinophilic enteritis is characterised by the presence of abnormal gastrointestinal symptoms, absence of an identified cause of eosinophilia, eosinophilic infiltration of the gastrointestinal tract and exclusion of the involvement of other organs.1 11
Clinical symptoms are non-specific and depend on the involved organ(s). The entire gastrointestinal tract can be affected. Clinical features are related not only to the anatomic locations of the eosinophilic infiltration but also to the depth of bowel wall involved.4–6 In the mucosal disease the most common symptoms are acute abdominal pain, nausea, vomiting, early satiety, diarrhoea and weight loss. These patients with diffuse small bowel disease can develop malabsorption. Peripheral eosinophil counts are usually elevated, ranging from 5% to 35% with an average absolute eosinophil count of 2000 cell/μL.8 Our patient presented very high levels of peripheral eosinophilia (10 510 cell/μL or 55%). Serum IgE levels can be elevated specially in children.7 12 Endoscopic examination is essential to diagnosis showing a nodular or polypoid mucosa, erythema and/or erosions. The microscopic examination of biopsy samples must reveal more than 20–25 eosinophils per high-power field.8 13 14
When eosinophilic infiltration of the muscle layer occurs it results in a thickened, rigid gut and symptoms and signs of intestinal obstruction. Stricture, perforation or obstruction of stomach, small bowel or colon can occur depending on the site of infiltration. Food intolerance or allergic history is not usually present and IgE levels are less frequent. The diagnosis is typically made after resection of small bowel for obstruction. These findings can mimic those induced by cancer, lymphoma or other malignancies. Endoscopic biopsies should be performed, but they are often non-diagnostic because mucosal involvement is lacking. In these cases, laparoscopic full thickness biopsy is usually necessary.8
Subserosal form of the disease generally presents with isolated ascites. The diagnostic feature is a marked eosinophilia, up to 88%, in the ascitic fluid. Patients in this subgroup may have an allergic background and some have elevated serum IgE. Peripheral eosinophils counts are as high as 8000 cell/μL.8 15 16
It is important to make the differential diagnosis with other diseases that present themselves with gastrointestinal symptoms and peripheral eosinophilia.2 3
Data on the natural history, treatment and prognosis are limited to case reports and retrospective series of few patients.3 17 The natural history of eosinophilic enteritis includes three different evolutionary patterns, since patients may suffer a single outbreak, a recurrent course or even chronic disease. Unlike our patient, untreated ones may rarely remit spontaneously but usually progress to severe malabsorption and malnutrition. The treatment is empirical and based on the severity of clinical manifestations. Owing to the rarity of this disease, there are no controlled treatment trials.14 In patients who are symptomatic or have evidence of malabsorption, a diet for a few weeks should be initiated. When this approach does not improve patient symptoms and peripheral eosinophilia, systemic glucocorticoids should be initiated. Steroids have been used as a traditional form of therapy to reduce the inflammatory process.18 Improvement generally occurs within 2 weeks regardless the layer of bowel involved. Although steroids should be tapered over the next weeks, some patients may need more prolonged therapy including those who have early relapse after steroid cessation.2–3 19 Other drugs have been used such as antihistamines, mast cells stabiliser and leucotriene antagonists, but their effectiveness is not known.19–23
Learning points.
Eosinophilic enteritis is a rare gastrointestinal disease of unknown aetiology.
Despite the fact that our patient has not any atopy background, a history of allergies is present in many cases.
Clinical symptoms are related to the layer and extent of bowel wall involved with eosinophilic infiltration. They are non-specific so a high degree of suspicion and an endoscopic biopsy are required for diagnosis.
Most patients respond to dietary approaches and/or oral steroids.
Untreated patients may rarely remit spontaneously or progress to severe malnutrition/obstruction.
Acknowledgments
The authors would like to acknowledge the help and guidance of Dr Cristina Poole da Costa and Dr António dos Santos Castro.
Footnotes
Contributors: All authors contributed to the clinical evaluation of the patient and to the diagnostic and therapeutic approach. They were also a great help in the bibliographic research and images collection.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Baig MA, Qadir A, Rasheed J, et al. A review of eosinophilic gastroenteritis. J Natl Med Assoc 2006;2013:1616–19 [PMC free article] [PubMed] [Google Scholar]
- 2.Mendez N, Chavez NC, Vasquez G, et al. Eosinophilic gastroenteritis: a review. Dig Dis Sci 2007;2013:2904–11 [DOI] [PubMed] [Google Scholar]
- 3.Khan S. Eosinophilic gastroenteritis. Best Pract Res Clin Gastroenterol 2005;2013:177–98 [DOI] [PubMed] [Google Scholar]
- 4.Doggui MH, Ben YL, Mohsni S, et al. Eosinophilic gastroenteritis with ascites: a case report. Tunis Med 2008;2013:600–3 [PubMed] [Google Scholar]
- 5.González HM, Ruiz MR, Rosales SA, et al. Primary sclerosing cholangitis of small ducts, associated with eosinophilic gastroenteritis: case report and literature review. Rev Gastroenterol Mex 2008;2013:242–6 [PubMed] [Google Scholar]
- 6.Khan S, Orenstein SR. Eosinophilic gastroenteritis. Gastroenterol Clin North Am 2008;2013:333–48 [DOI] [PubMed] [Google Scholar]
- 7.Klein NC, Hargrove RL, Sleisenger MH, et al. Eosinophilic gastroenteritis. Medicine 1970;2013:299. [DOI] [PubMed] [Google Scholar]
- 8.Talley NJ, Shorter RG, Phillips SF, et al. Eosinophilic gastroenteritis: a clinical pathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut 1990;2013:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daneshjoo R, Taller NJ. Eosinophilic gastroenteritis. Curr Gastroenterol Rep 2002;2013:366–72 [DOI] [PubMed] [Google Scholar]
- 10.Chen MJ, Chu CH, Lin SC, et al. Eosinophilic gastroenteritis: clinical experience with 15 patients. World J Gastroenterol 2003;2013:2813–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou HB, Chen JM, Du Q. Eosinophilic gastroenteritis with ascites and hepatic dysfunction. World J Gastroenterol 2007;2013:1303–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foroughi S, Foster B, Kim N, et al. Anti-IgE treatment of eosinophil-associated gastrointestinal disorders. J Allergy Clin Immunol 2007;2013:594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller S. Classification of eosinophlic gastrointestinal diseases. Best Pract Res Clin Gastroenterol 2008;2013:1372–5 [DOI] [PubMed] [Google Scholar]
- 14.Freeman HJ. Adult eosinophilic gastroenteritis and hypereosinophilic syndromes. World J Gastroenterol 2008;2013:6771–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maeshima A, Murakami H, Sadakata H, et al. Eosinophilic gastroenteritis presenting with acute panceatitis. J Med 1997;2013:265–72 [PubMed] [Google Scholar]
- 16.Eusher E, Vaswani K, Frankel W. Eosinophilic pancreatitis: a rare entity that can mimic a pancreatic neoplasm. Ann Diagn Pathol 2000;2013:379–85 [DOI] [PubMed] [Google Scholar]
- 17.Fleischer MD, Atkins D. Evaluation of the patient with suspected eosinophilic gastrointestinal disease. Immunol Allergy Clin North Am 2009;2013:53–63 [DOI] [PubMed] [Google Scholar]
- 18.Sheikh RA, Prindiville TP, Pecha RE, et al. Unusual presentationsof eosinophilic gastroenteritis: case series and review of literature. World J Gastroenterol 2009;2013:2156–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foroughi S, Prussin C. Clinical management of eosinophilic gastrointestinal disorders. Curr Allergy Asthma Rep 2005;2013:259–61 [DOI] [PubMed] [Google Scholar]
- 20.Gioacchino M, Pizzicannella G, Fini N, et al. Sodium cromoglycate in the treatment of eosinophilic gastroenteritis. Allergy 1990;2013:161–6 [DOI] [PubMed] [Google Scholar]
- 21.Melamed I, Feanny SJ, Sherman PM, et al. Benefit of ketotifen in patients with eosinophilic gastroenteritis. Am J Med 1991;2013:310–14 [PubMed] [Google Scholar]
- 22.Schwartz DA, Pardi DS, Murray JA. Use of montelukast as steroid-sparing agent for recurrent eosinophilic gastroenteritis. Dig Dis Sci 2001;2013:1787. [DOI] [PubMed] [Google Scholar]
- 23.Shirai T, Hashimoto D, Suzuki K, et al. Successful treatment of eosinophilic gastroenteritis with suplatast tosilate. J Allergy Clin Immunol 2001;2013:924–5 [DOI] [PubMed] [Google Scholar]


