Abstract
Osteoradionecrosis (ORN) is a known entity in patients with head and neck malignancy treated by radiotherapy. Involvement of mandible (0.8–37%) and maxilla (2–11%) is quiet common but upper cervical spine involvement is rare. One needs to have a high index of suspicion for the diagnosis of ORN after radiotherapy in the head and neck region. It may mimic either metastasis or an infection and needs histopathology to make definitive diagnosis. We reported the successful treatment of a patient with ORN involving upper cervical spine by posterior decompression and stabilisation. In addition, a new technique of reaching the odontoid process from posterior aspect for biopsy has been described.
Background
Osteoradionecrosis (ORN) is a known entity in patients with head and neck malignancy treated by radiotherapy.1 Involvement of mandible (0.8–37%) and maxilla (2–11%) are quiet common but upper cervical spine involvement is rare.2 3 There are only few reported cases of ORN of cervical spine in the literature.4–6 One needs to have a high index of suspicion for the diagnosis of ORN as it usually presents within 2 years after radiotherapy but it may even develop as long as 20–30 years after the initial exposure.7 It may mimic either metastasis or an infection and needs histopathology to make definite diagnosis. The bone necrosis and hypoxic environment of ORN along with soft tissue scarring can result in spinal instability. We reported the successful treatment of a patient with ORN involving upper cervical spine by posterior decompression and stabilisation. To our knowledge, this is the first report of isolated ORN of the upper cervical spine in a patient with laryngeal carcinoma treated by decompression and posterior stabilisation.
Case presentation
A 52-year-old male patient was referred in September 2010 with a 4-month history of upper cervical pain affecting his quality of life. He had squamous cell carcinoma of larynx with T2 N1 M0 staging treated by external beam radiation and chemotherapy in July 2008. He had no history of recent trauma. The main presenting symptom was severe neck pain needing to hold the weight of his head with his hands on the chin for most parts of the day. In addition, he was unable to rotate his neck as it was associated with severe pain. On physical examination, he was alert and responsive with normal gait. Motor examination of upper and lower limbs revealed normal muscle tone with grade 5/5 power in all myotomes. The patient had normal and intact tendon reflexes without any clonus. Sensory examination was normal in all dermatomes in upper and lower limbs.
Investigations
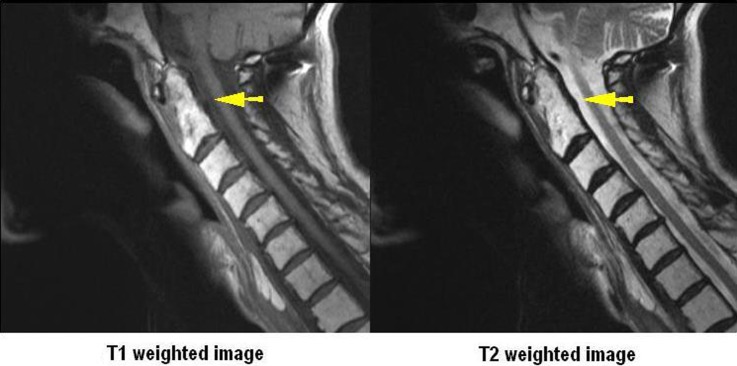
MRI of his cervical spine showed a hypodense lesion in T1-weighted images and a high-intensity signal in T2-weighted images occupying the odontoid process and also the body of C2 vertebra with expansion into the atlanto-odontoid joint anteriorly and posteriorly (figure 1). Postcontrast sequences uniformly enhanced throughout the lesion giving the picture of metastasis. Neither the CT scan revealed any fracture of odontoid process nor did it show any destructive lesion. However, it showed clivus impingement and the McGregor line was 2 mm (figure 2). Also, there was destruction of atlanto-occipital joint on the left side with severe arthritis (figure 3). The flexion-extension radiographs showed that the atlantodental interval was 5 mm and it did not change with the position (figure 4). Contrast-enhanced CT of abdomen, chest and pelvis were normal. Bone scan showed only increased uptake at C1/C2 joint where the MRI scan had previously shown the lesion. There was no other lesion in the rest of the body. Blood investigations like serum electrophoresis, urine Bence Jones protein and tumour markers were all within normal limits.
Figure 1.

T1-weighted image showing horizontal rim of marrow sparing above the inferior end plate (yellow arrow). Osteoradionecrosis involving dens on T1-weighted image and T2-weighted image (white arrows). T2 images also show bulging of posterior longitudinal ligament.
Figure 2.
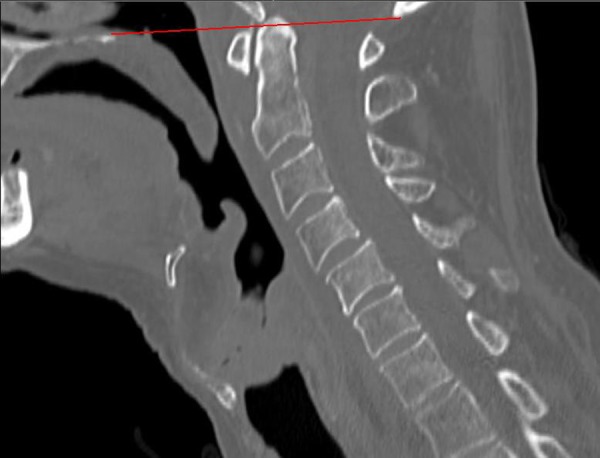
CT scan showing clivus impingement and normal McGregor's line (red line).
Figure 3.
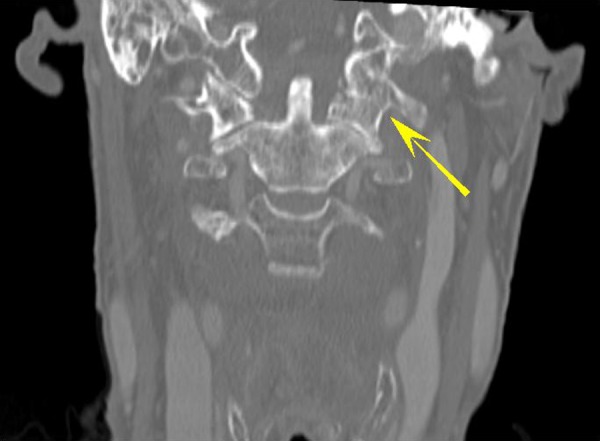
CT scan showing arthritic involvement of left atlanto-occipital joint (yellow arrow).
Figure 4.
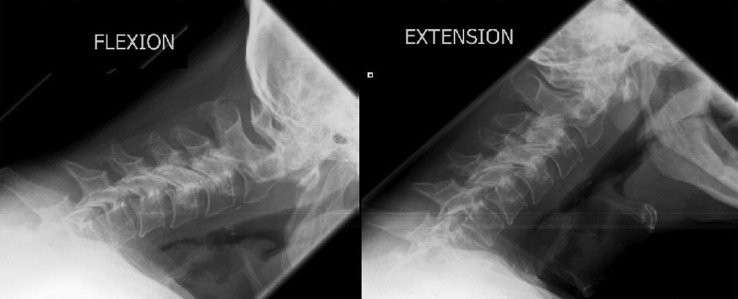
Flexion and extension X-rays of cervical spine.
Differential diagnosis
Metastasis, osteoarthritis.
Treatment
Oncology multidisciplinary meeting concluded that this was metastasis and wanted a biopsy for further management. Biopsy of the odontoid was performed through a right-sided anterior approach as for an odontoid screw. During procedure it was noted that the tissues were woody hard because of previous radiotherapy. The biopsy did not reveal any evidence of malignancy but showed features of chronic inflammation.
A decision to perform occipitocervical fusion was made as the symptoms could still come from the clivus impingement and the destroyed atlanto-occipital joint. The degree of osteoarthritis on the left atlanto-occipital joint was grade 3 and the right atalnto-occipital joint was grade 1 as per the Lakshmanan classification.8 Also, the oncologists requested another biopsy sample from the odontoid lesion. Hence, while performing the posterior occipitocervical fusion, as initial drill for Magerl type C1/C2 screw reached the past posterior border of the odontoid, the drill was exchanged with a wire followed by insertion of Harlow wood biopsy cannula (figure 5). The wire was then removed and Harlow wood biopsy cannula was medialised as much as possible to reach the odontoid process to get a biopsy. The posterior occipitocervical fusion was completed up to C3 with lateral mass screws at C3 (figure 6). A posterior upper cervical spine decompression along with foramen magnum decompression was performed. The biopsy results revealed intertrabecular fibrous tissue impregnated with haemosiderin from the first biopsy.
Figure 5.
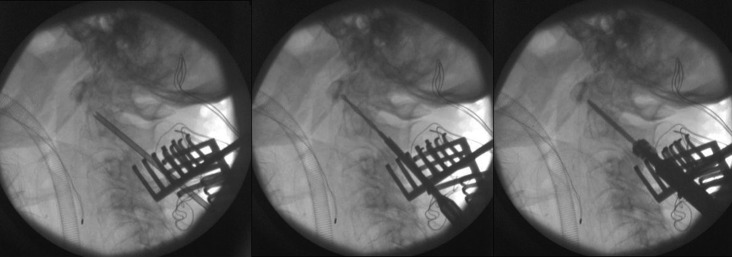
Biopsy from C2 followed by insertion of screw.
Figure 6.

X-ray after posterior atlanto-occipital stabilisation.
Outcome and follow-up
The patient's symptoms improved dramatically immediately after surgery and he did not had to hold his head with his hands anymore. The interval MRI scans performed at 3 months of follow-up showed that the atlanto-odontoid mass had regressed completely. Also, the signal changes in T1-weighted image and T2-weighted image improved (figure 7). One-year follow-up MRI scans confirmed the complete clearance of the mass with normal signal changes in the odontoid process.
Figure 7.
T1-weighted image and T2-weighted image showing resolution of lesion (yellow arrows).
Discussion
Survival of patients with head and neck malignancies has improved with time due to recent development in the diagnostic and treatment modalities. With increased survival there is an increase in the post-treatment morbidity and ORN is one of them. ORN sometimes becomes difficult to diagnose due to its long incubation period after the radiation or due to its unusual site and presentation. Wong et al9 defined ORN as the slow-healing, radiation-induced ischaemic necrosis of bone associated with soft tissue necrosis of variable extent occurring in the absence of local primary tumour necrosis, recurrence or metastatic disease. ORN is classified into three types as proposed by Marx with type 1 developing quickly after radiation therapy, type 2 develops late however after a traumatic event and type 3 occurs spontaneously between 6 months and 3 years after radiation therapy.10 Our case seems to be type 3 as it developed late after radiation therapy and there was no history of any traumatic event. High index of suspicion and early diagnosis is the key for successful outcome.
With the history of irradiation for laryngeal carcinoma in our patient and the rare site of lesion at the cervical spine, the differential diagnosis included metastasis, radiation-induced neoplasm, infection and ORN. The ideal imaging modality in these cases is MRI of cervical spine. Various retrospective case series have shown ORN to be quite distinct on MRI.3 11 In one such series, Wu et al3 noticed ORN to show significantly more contagious involvement of atlantoaxial or atlanto-occipital bones with intervening joint change, vertebral body collapse and bilateral symmetrical involvement. On the other hand, tumour recurrence was found to primarily affect posterior arch or multiple cervical vertebra, paraspinal mass lesion or epidural involvement and even cervical lymphadenopathy.3 Involvement of C2 dens with or without body with a characteristic horizontal rim of marrow preservation above the inferior endplate is considered typical for osteoradionecrosis.11 This horizontal rim of marrow preservation is also seen in MRI of our case (figure 1). However in our case, a layer of enhancing soft tissue causing displacement of posterior longitudinal ligament was also seen. In addition, there was also bulging of anterior longitudinal ligament with thickening of left prevertebral space. And hence, a metastasis cannot be ruled out. Thus a biopsy was performed which not only confirmed the diagnosis but also resulted in core decompression of the lesion. In our case ORN was confirmed histologically by the presence of necrotic bone, fibrosis and plasmacytic infiltrate.
ORN can be associated with cervical instability and may possibly result in paralysis if remains untreated.12 In our case, ORN of upper cervical spine led to the symptoms related to atlanto-occipital joint destruction on the left side along with clivus impingement. When surgery is contemplated, the surgical approach must be selected bearing in mind the possibility of radiation changes to local tissues resulting in numerous potential complications. In our patient, cervical spine stabilisation was achieved by posterior approach with posterior occipitocervical fusion and decompression (figure 6). The patient subsequently had marked resolution of symptoms and even the lesion regressed gradually after the occipitocervical fusion. It is however difficult to speculate the cause of resolution of atlanto-odontoid mass which could well be due to the stability given by the occipitocervical fusion or possibly secondary to core decompression or may even be spontaneous. This is evident in 3 months of postoperative MRI.
We have also described a new technique of reaching the odontoid process from posterior aspect for biopsy. Confirmation seen in the histology during the second histopathological examination of the specimen shows haemosiderin deposition on top of other findings similar to the first histopathological specimen obtained anteriorly. The haemosiderin deposition was from the trauma of the first biopsy performed anteriorly resulting in bleeding inside the bone.
Learning points.
Osteoradionecrosis (ORN), although rare, is a known entity in patients with head and neck malignancy treated by radiotherapy.
One should have a high index of suspicion in diagnosing ORN in patients postradiotherapy as it can mimic metastasis.
Histopathological diagnosis is must for confident diagnosis of ORN.
Footnotes
Contributors: AR wrote the major portion of the manuscript. MI provided support with formatting the figures and literature search. PL provided support in reviewing the manuscript and provided valuable advice in proof reading the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg 1983;2013:283–8 [DOI] [PubMed] [Google Scholar]
- 2.Sanger JR, Matloub HS, Yousif NJ, et al. Management of osteoradionecrosis of the mandible. Clin Plast Surg 1993;2013:517–30 [PubMed] [Google Scholar]
- 3.Wu LA, Liu HM, Wang CW, et al. Osteoradionecrosis of the upper cervical spine after radiation therapy for head and neck cancer: differentiation from recurrent or metastatic disease with MR imaging. Radiology 2012;2013:136–45 [DOI] [PubMed] [Google Scholar]
- 4.Donovan DJ, Huynh TV, Purdom EB, et al. Osteoradionecrosis of the cervical spine resulting from radiotherapy for primary head and neck malignancies: operative and nonoperative management. Case report. J Neurosurg Spine 2005;2013:159–64 [DOI] [PubMed] [Google Scholar]
- 5.Lim AA, Karakla DW, Watkins DV. Osteoradionecrosis of the cervical vertebrae and occipital bone: a case report and brief review of the literature. Am J Otolaryngol 1999;2013:408–11 [DOI] [PubMed] [Google Scholar]
- 6.Ng RL, Beahm E, Clayman GL, et al. Simultaneous reconstruction of the posterior pharyngeal wall and cervical spine with a free vascularized fibula osteocutaneous flap. Plast Reconstr Surg 2002;2013:1361–5 [DOI] [PubMed] [Google Scholar]
- 7.Costantino PD, Friedman CD, Steinberg MJ. Irradiated bone and its management. Otolaryngol Clin North Am 1995;2013:1021–38 [PubMed] [Google Scholar]
- 8.Lakshmanan P, Jones A, Howes J, et al. CT evaluation of the pattern of odontoid fractures in the elderly—relationship to upper cervical spine osteoarthritis. Eur Spine J 2005;2013:78–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong JK, Wood RE, McLean M. Conservative management of osteoradionecrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;2013:16–21 [DOI] [PubMed] [Google Scholar]
- 10.Kouyoumdjian P, Gille O, Aurouer N, et al. Cervical vertebral osteoradionecrosis: surgical management, complications and flap coverage—a case report and brief review of the literature. Eur Spine J 2009;2013:258–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.King AD, Griffith JF, Abrigo JM, et al. Osteoradionecrosis of the upper cervical spine: MR imaging following radiotherapy for nasopharyngeal carcinoma. Eur J Radiol 2010;2013:629–35 [DOI] [PubMed] [Google Scholar]
- 12.van Wyk FC, Sharma MP, Tranter R. Osteoradionecrosis of the cervical spine presenting with quadriplegia in a patient previously treated with radiotherapy for laryngeal cancer: a case report. J Med Case Rep 2009;2013:7262. [DOI] [PMC free article] [PubMed] [Google Scholar]


