Abstract
We applied customized targeted next-generation exome sequencing (NGS) to determine if mutations in genes associated with renal malformations, Alport syndrome (AS) or nephrotic syndrome are a potential cause of renal abnormalities in patients with equivocal or atypical presentation. We first sequenced 4,041 exons representing 292 kidney disease genes in a Caucasian woman with a history of congenital vesicoureteral reflux (VUR), recurrent urinary tract infections and hydronephrosis who presented with nephrotic range proteinuria at the age of 45. Her biopsy was remarkable for focal segmental glomerulosclerosis (FSGS), a potential complication of longstanding VUR. She had no family history of renal disease. Her proteinuria improved initially, however, several years later she presented with worsening proteinuria and microhematuria. NGS analysis revealed two deleterious COL4A3 mutations, one novel and the other previously reported in AS, and a novel deleterious SALL2 mutation, a gene linked to renal malformations. Pedigree analysis confirmed that COL4A3 mutations were nonallelic and compound heterozygous. The genomic results in conjunction with subsequent abnormal electron microscopy, Collagen IV minor chain immunohistochemistry and progressive sensorineural hearing loss confirmed AS. We then modified our NGS approach to enable more efficient discovery of variants associated with AS or a subset of FSGS by multiplexing targeted exome sequencing of 19 genes associated with AS or FSGS in 14 patients. Using this approach, we found novel or known COL4A3 or COL4A5 mutations in a subset of patients with clinically diagnosed or suspected AS, APOL1 variants associated with FSGS in African Americans and novel mutations in genes associated with nephrotic syndrome. These studies demonstrate the successful application of targeted capture-based exome sequencing to simultaneously evaluate genetic variations in many genes in patients with complex renal phenotypes and provide insights into etiology of conditions with equivocal clinical and pathologic presentations.
Introduction
Glomerular dysfunction is the most common cause of end stage renal disease [1], [2]. Damage to the glomeruli can manifest in a number of ways including proteinuria, hematuria and hypertension [1], [3], [4], [5], [6], [7]. Many glomerular diseases are categorized according to well-defined histopathological patterns. For example, focal segmental glomerulosclerosis (FSGS) pattern in a biopsy can be caused by different etiologies including primary or secondary glomerular disease or reflux due to lower urinary tract malformations [8]. Newer genomic technologies including next-generation sequencing (NGS) are rapidly evolving and may provide new insights into disease pathogenesis, diagnosis, genetics or prognosis, explain histopathological findings and potentially guide therapy. However, their application to kidney disease has been limited.
We first analyzed exomes of several hundred genes using a targeted customized exome sequencing approach in a patient with a history of vesicoureteral reflux (VUR) who presented with proteinuria and FSGS on renal biopsy. We identified two deleterious nonallelic COL4A3 mutations, one novel and the other previously reported in an Alport syndrome (AS) patient. We further identified a deleterious mutation in SALL2, a gene important in early kidney development. Pedigree analysis confirmed that the COL4A3 mutations were compound heterozygous and subsequent clinical work-up confirmed dual disease, Alport syndrome and VUR. We then applied a modified targeted exome sequencing by multiplexing 19 genes and 14 patients with either well established or clinically suspected AS or FSGS to determine potential genetic cause of their diseases. Several novel and previously known COL4A mutations in AS, APOL1 G2 deletion variants in some FSGS patients and new coexisting gene mutations in proteinuria related genes (LAMA5) were identified. These studies are among the first to apply Next-gen targeted-capture exome sequencing approach in delineating genetic basis for atypical and complex renal diseases presenting as renal malformations and/or glomerular diseases.
Materials and Methods
Human Studies
Human studies were conducted according to protocols approved by the Washington University human research protection office. Patient recruitment, specimen collection and processing were done by the Washington University Kidney Translational Research Core. Samples from 15 patients were used (14 glomerular disease, 1 glomerular and renal malformation).
Gene Selection
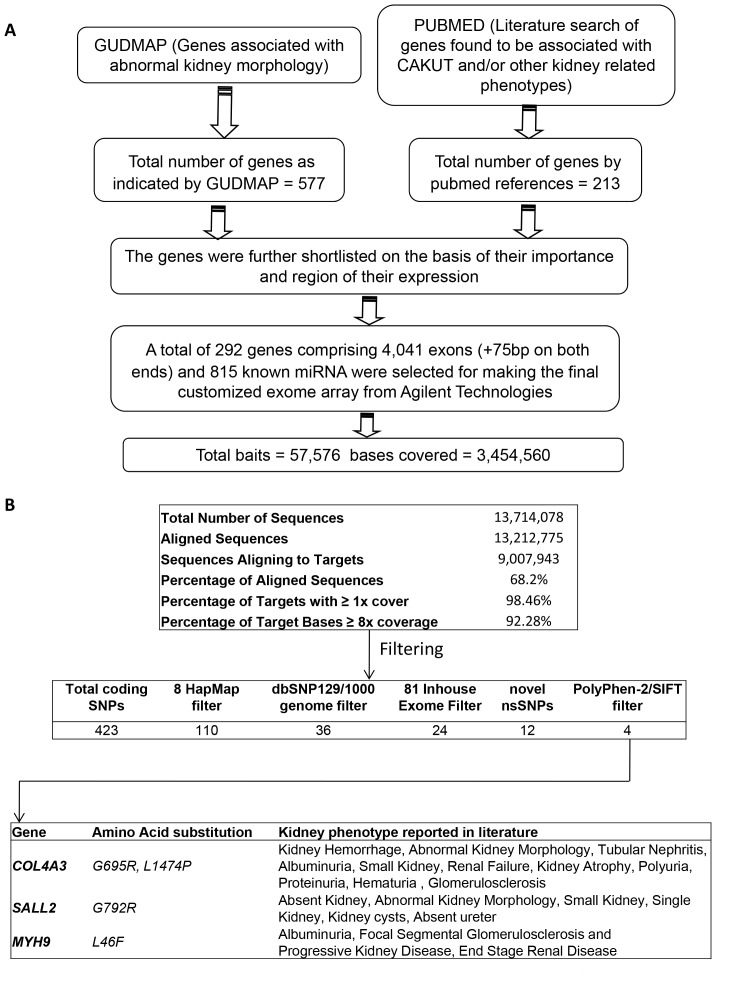
The genes selected for this study resulted from searches of public databases such as PUBMED and GUDMAP (http://www.gudmap.org/) and abstracts as of 2010 (Figure 1a). Briefly, search terms included genes associated with CAKUT and/or other kidney related phenotypes such as renal failure, abnormal kidney development, ectopic kidney, atrophic kidney, single kidney, no kidney, and kidney disease. The gene lists were further curated based on their expression patterns, functional significance in disease models and mutations in human kidney disease. A total of 292 genes comprising 4,041 exons were selected for the sequencing studies (Table S1). The genomic intervals for the shortlisted genes were selected using GRch37/hg19 version of the assembled human genome. The UCSC genome browser (http://genome.ucsc.edu/cgi-bin/hgTables?org=Human&db= hg19&hgsid = 192997943&hgta_doMainPage = 1) was used to obtain the start and end sites of each exon including known isoforms and 75 bp of flanking regions were additionally included to cover the exon-intron boundaries and the splice junctions. In some cases, 10 Kb promoter regions were also included; however, this analysis was focused on exons and flanking sequences.
Figure 1. Overview of the targeted exome sequencing pipeline and filtering strategy applied to patient with VUR and proteinuria.
(A) Criteria for gene selection for developing a custom targeted renal disease exome array. (B) Custom-exome capture sequencing metrics from the patient 1184405 and filtering approach used to identify four novel mutations in three kidney disease genes.
Custom Bait Library Generation
Bait generation and library preparation were done using the eArray tool provided by the manufacturer (Agilent technologies, (https://earray.chem.agilent.com/earray)). The baits, 120 bp each, were generated for Illumina end sequencing technology with bait tiling frequency of 2X using optimized parameters. The failed baits (632) were redesigned with the repeatmasker filter turned off. We also included baits for sequencing 815 miRNA that were already predesigned by Agilent. Library was created using Library preparation tool of Agilent for paired end sequencing. The final library generated consisted of 57,576 total functional baits that cover 3,454,560 bp of the genome. For the screening of mutations in patients with proteinuria or AS multiplexed targeted exome capture and NGS was done on a set of 19 genes (Supplemental Table S3) known or predicted to be associated with AS or proteinuria. Gene selections and library preparation were same as described above.
DNA Extraction, Library Preparation, Next-generation Sequencing and Data Filtering
Genomic DNA was obtained from the Washington University Kidney Translational Research Core. Briefly, genomic DNA was isolated from peripheral blood leukocytes using QIAamp DNA blood mini kit (Cat No 51106) according to manufacturer’s instructions. Genomic DNA for relatives was isolated from buccal cells using an over the counter mouthwash (Scope). For the patients with AS and CAKUT, library preparation targeted capture against the baits and NGS using GAIIx sequencer (Illumina) was done by the Genome Technology Access Center core facilities.
Novoalign (http://www.novocraft.com) was used for alignment of the sequencing reads and variant calling was done using SAM tools [9] as described before [10]. SNP calls were filtered against the dbSNP129 database, in-house exome data and prioritized according to importance with publicly available software tools (Figure 1b). The effect of amino acid substitution on protein function was predicted with Sorting Intolerant from Tolerant (SIFT, http://sift.jcvi.org/) and Polymorphism Phenotyping v2 (PolyPhen-2, http://genetics.bwh.harvard.edu/pph2/) [11]. Controlled access to sequencing data are available to investigators authorized to conduct human studies. Genotype data will be deposited at the European Genome-phenome Archive (EGA, http://www.ebi.ac.uk/ega/), which is hosted by the EBI, under accession number EGAS00001000560.
Sanger Sequencing
Novel or rare variants identified from exome sequencing in the patient with VUR and proteinuria were validated using Sanger sequencing. All primers used are shown in Supplemental Table S2. Sanger sequencing was performed in the tissue procurement and molecular phenotyping core at the Washington University. The data were analyzed using DNASTAR software (http://www.dnastar.com/).
Histopathology
Histopathological results were obtained from the Pathology archives of Washington University School of Medicine in St. Louis and Cornell University. These data were part of routine care involving light microscopy, immunohistochemistry and electron microscopy of renal biopsies.
Sanger Sequencing Validation of the APOL1 Deletion in African American Focal Segmental Glomerulosclerosis (FSGS) Patients
To confirm the APOL1deletion variation (rs71785313), also known as G2, in the two African American (AA) FSGS patients, Sanger sequencing was performed using the APOL1_I/D_rs71785313 primer set (Supplemental Table S2). The same primer set was used to determine the allelic frequency of the deletion in a set of African-American FSGS patients and unrelated controls.
Results
Clinical Phenotype of a Patient with Unexplained Proteinuria
We enrolled a Caucasian woman (patient 1184405) whose past medical history is significant for vesicoureteral reflux (VUR) diagnosed at age two, several urinary tract infections and hydronephrosis. At age 45 she presented with nephrotic range proteinuria and hypertension but no evidence of hematuria. Her kidney biopsy showed histopathologic changes that suggested focal segmental glomerulosclerosis (FSGS), however, immunohistochemical and electron microscopy studies were inconclusive. She has no family history of renal disease. Her proteinuria initially improved on oral steroids but later required additional immunosuppressants due to worsening creatinine; proteinuria range was 2+ to 3+. It was unclear from the clinical course if the patient had primary or secondary FSGS, for example, due to VUR or another disease. At age 48 she presented with worsening proteinuria, her repeat biopsy showed FSGS, and the electron microscopy findings were suggestive of hereditary nephritis. The patient consented to participate in studies to investigate potential molecular-genetic causes of her kidney disease that may help clarify or provide insights into the underlying etiology of her renal dysfunction.
Deleterious Mutations in COL4A3, MYH9 and SALL2 in the Patient 1184405
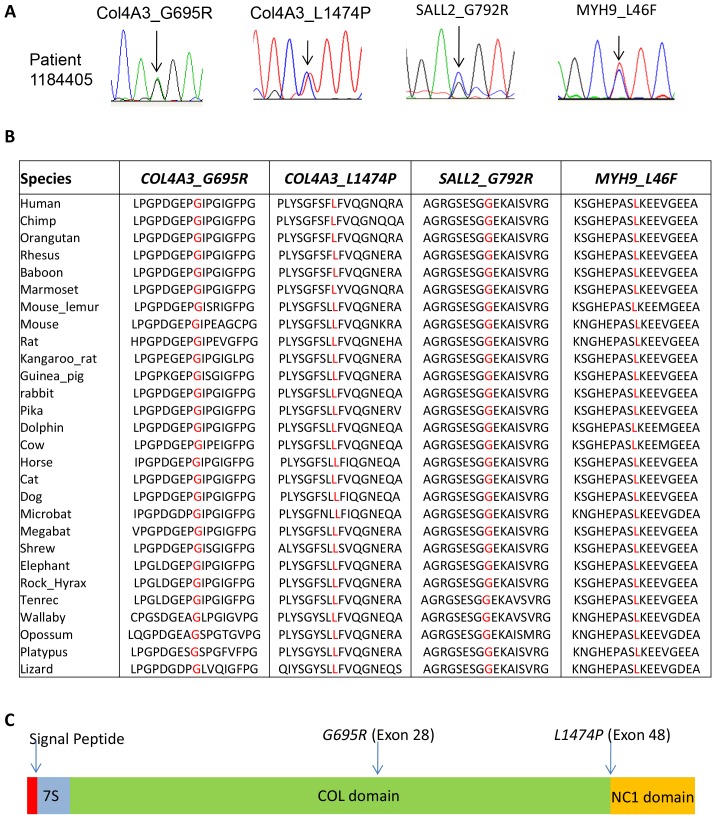
To identify gene defects that may uncover potential cause of CAKUT or proteinuria that lead to kidney dysfunction in the patient 1184405 we sequenced the coding region and exon-intron splice junctions of 292 genes most likely associated with renal anomalies or glomerular disease using NGS (see methods). Sequencing results showed high depth of coverage with more than 90% of the targeted region sequenced at a depth of 8-fold or greater (Figure 1b). To prioritize identification of mutations that are the most deleterious we adopted a filtering strategy to focus on non-synonymous novel deleterious variants using a combination of filtering against SNP databases, in-house unrelated non-kidney disease exomes and bioinformatic software tools Polyphen2 and SIFT (Figure 1b) [10]. We discovered four novel non-synonymous mutations: COL4A3_G695R, COL4A3_L1474P, MYH9_L46F and SALL2_G792R that were all predicted to be damaging (Figure 1b). All four mutations were confirmed by Sanger sequencing (Figure 2a). Bioinformatic analysis revealed that the mutated residues were conserved across species (Figure 2b). The COL4A3 mutations were in a highly conserved glycine rich region and in an important functional domain (Figure 2c).
Figure 2. Validation and evolutionary conservation of the identified mutations in the patient with VUR and proteinuria.
(A) Sanger sequencing analysis confirms the novel COL4A3 mutations, COL4A3_G/A_G695R and COL4A3_T/C_L1474P, the SALL2_G/C_G792R and the MYH9_C/T_L46F mutations in the patient 1184405. (B) Multi species alignment shows that both the COL4A3 mutation reference amino acids Col4A3_ 695_G and Col4A3_1474_L, the SALL2_G792R and the MYH9_L46F are highly conserved among species. (C) Schematic representation of Human COL4A3 gene with the discovered mutations in patient 1184405. The domains are: signal peptide domain (red), the N terminal 7S domain (blue), the central triple helix collagenous (COL) domain (green) and the carboxy-terminal non-collagenous (NC1) domain (yellow).
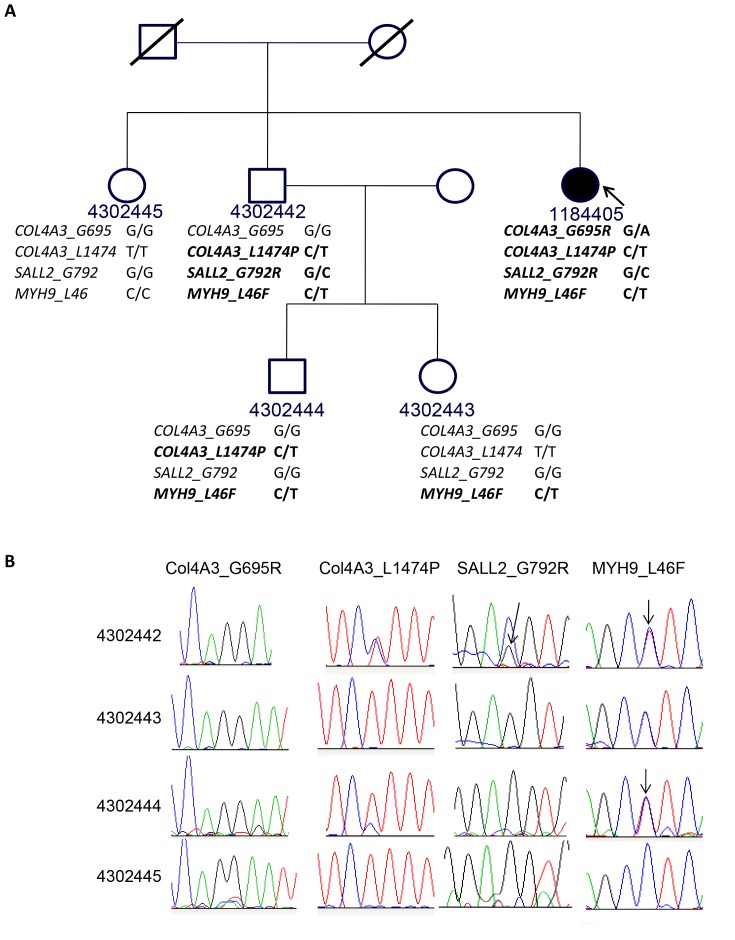
Pedigree Analysis of the Four Deleterious Mutations in Patient 1184405
The presence of COL4A3 mutations suggested Alport syndrome in this patient as a likely cause of proteinuria (see below). We next performed studies to determine the inheritance pattern of the deleterious mutations found in patient 118405. Consent was obtained from the available family members (Figure 3). Sanger sequencing was performed on their genomic DNA to detect COL4A3-G695R and COL4A3-L1474P mutations. None of the family members harbored both COL4A3 mutations suggesting the possibility that they are on separate alleles in the index patient (Figure 3a,b). The COL4A3-L1474P mutation was found in an unaffected brother and his son with unknown disease status. The COL4A3-G695R mutation was not present in any of the family members studied indicating the possibility of a de novo change. Mutation analysis of SALL2 and MYH9 was also performed by Sanger sequencing in all the available family members and none of the family members harbored all four mutations (Figure 3a and 3b).
Figure 3. Pedigree analysis of the index patient with proetinuria and VUR.
(A) Pedigree of the family of the index patient (1184405, arrow) shows presence of Col4A3_T/C_L1474P variant in one unaffected brother (4302442) and nephew (4302444), but absent in the unaffected sister (4302445) and niece (4302443); while the other damaging variant Col4A3_G/A_G695R is present only in the patient. The SALL2 deleterious mutation SALL2_G/C_G792R is present in the patient and one unaffected brother (4302442) while the MYH9_C/T_L46F mutation is present in all but one affected family member (4302445). (B) Sanger sequencing analysis confirms the status of the novel COL4A3 mutations Col4A3_G/A_G695R and Col4A3_C/T_L1474P, and the SALL2_G/C_G792R and MYH9_C/T_L46F mutations in the relatives of patient 1184405. The Col4A3_T/C_L1474P heterozygous variant was present in one unaffected brother (4302442) and nephew (4302444), but absent the unaffected sister (4302445) and niece (430443). The mutation Col4A3_G/A_G695R was absent in all other family members. The SALL2_G/C_G792R mutation was present only in the unaffected brother 4302442 while the MYH9_C/T_L46F mutation was more common and was present in everyone except the unaffected sister 4302445.
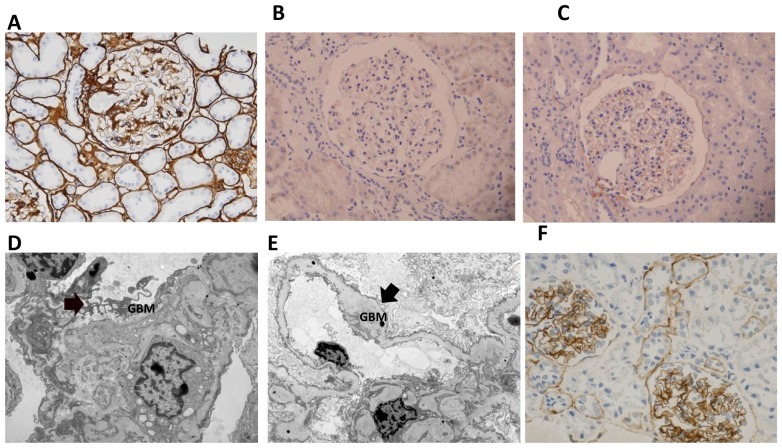
Immunohistochemistry and Electron Microscopy Confirm Collagen Defects
At age 52 the patient [1184405] presented with proteinuria (3+) and hematuria (1+) and reported hearing loss of two years duration. A kidney biopsy was performed to confirm hereditary nephritis (AS) as a cause of her worsening renal dysfunction. Light microscopy was remarkable for FSGS. We performed COL4α1, COL4α3 and COL4α5 immunohistochemistry and found strong COL4α1 immunoreactivity in the glomerular capillary loops, and tubular basement membrane, weak COL4α5 in glomerular capillary loops and basement membrane of distal tubules and no COL4α3 immunoreactivity (Figure 4). EM showed glomerular basement membrane thickening and laminations alternating with areas of thinning, findings consistent with AS.
Figure 4. Results of immunostaining with antibodies against α1, α3, and α5 chains of type IV collagen in the AS/VUR patient.
(A) ColIVα1 expression is strong and consistent in the basement membranes (BM) of the glomeruli and the tubules; typically it is absent in adult glomeruli. Images show absent α3IV (B) and weak α5IV (C) staining in the glomerular BMs. (D&E) Electron micrograph from this patient shows segmental glomerular basement membrane (GBM) lamellation and outpouching (D arrow) and irregular thickening (E arrow) of the GBM characteristic of AS. COL4α3 immunostaining in control shows the normal tubular and capillary loop distribution for comparison (F).
Custom Next-generation Sequencing of Candidate Proteinuria Genes Simultaneously in Several Patients (Multi-indexed) Provides Genetic Evidence for Cause of Alports or FSGS
We next extended our above analysis to a modified NGS approach to identify mutations in a selected group of genes associated with proteinuria in patients with clinically diagnosed Alports or FSGS or cases in which diagnosis was equivocal (see Table 1 for patient characteristics). We sequenced coding region of a set of 19 genes (Supplementary Table 3) in nine patients with a clinical diagnosis of hereditary nephritis or AS and five FSGS patients. One of the patients with FSGS diagnosis (07-0430-01590) is a relative of another patient with AS (07-0430-02009). As indicated in Table 1, some of these patients had established AS based on family history or pathological findings while in others there was a family history of kidney disease but no pathologically or genetically confirmed AS. The FSGS patients were selected to serve as negative controls for COL4 mutations and to determine if variations in genes associated with proteinuria may explain the etiology in some of these patients. We applied a multiindexing approach where each patient’s DNA was coded with a unique tag (index) so the targeted exomes from all the patients could be simultaneously sequenced. NGS metrics revealed greater than 200-fold average coverage and 95% of the region of interest was covered at a depth of 40X or greater (Supplementary table 4). Using the same filtering approach as for the patient with Alports and VUR above we found COL4A3, COL4A4 and/or COL4A5 novel or rare mutations in 6 out of 9 unrelated patients with known or equivocal AS and novel LAMA5 mutations in 3 out of 4 FSGS patients (Table 1). Two relatives (07-0430-02009 and 07-0430-01590) were included and the same COL4A5-G1161E mutation was independently identified providing credence to our approach. Among these, patient 07-0430-01590 is the grandmother of 07-0430-02009 and did not previously have AS diagnosis and is clinically phenotyped as FSGS. Based on bioinformatics predictions a number of these variants were predicted to be probably damaging using the PolyPhen 2 software (Table 1). No small indels or exon deletions were present in the Collagen 4A3, A4 or A5 genes. Visual inspection of the mutations identified by SAMtools confirmed the base calls made. We also detected a previously reported 6 bp deletion in APOL1 (G2 variant) that is associated with the development of FSGS in African Americans [12] and verified this variant using Sanger sequencing.
Table 1. Clinical characteristics of patients that underwent validation of custom multindexed targeted exome sequencing of 19 genes.
| Participant ID | Diagnosis | Age enrolled | Age diagnosed | Gender | Race | Novel deleterious Mutations | PolyPhen-2scores ofNovelMutations | RareDeleteriousMutations(MAF<0.05) | Family History | Biopsy (initial clinical presentation) |
| 07-0430-01196 | Alport’s syndrome/ESRD | 47 | 10 | F | C | COL4A5-G1030S | 1 | father, sister andpaternal uncle allon Hemodialysis. Fatherdiagnosed for Alport’s.Two sons withpresumed Alport’s | biospy at age 10, inconclusive (proteinuria) | |
| 07-0430-01724 | Alport’s sydrome | 8 | 4 | M | C | rs1800516 | 3 brother withAlport’s Syndrome | skin negative for COL4A5 (hematuria) | ||
| 07-0430-02009 | horseshoe kidney/Crohn’s/alport’s | 16 | 6 | F | C | COL4A5-G1161E | 1 | rs13027659 | Grandmother07-0430-00730 hasESRD/FSGS | Alport Syndrome (GN) |
| 07-0430-01590 | ESRD, Grandmother of07-0430-2009 | 53 | 11 | F | C | COL4A5-G1161E, NPHS1-N188I | 1, 0.57 | maternal uncle and 2cousins died of renalfailure | FSGS (proteinuria) | |
| 07-0430-00730 | Hereditary nephritis | 70 | 44 | M | C | brother with renal transplant | no biopsy (ESRD) | |||
| 07-0430-01161 | Hereditary nephritis | 71 | 56 | F | C | multiple familymembers with kidney transplants | no biopsy (ESRD) | |||
| 07-0430-01559 | Hereditary nephritis | 60 | 48 | F | C | likely secondary FSGS | no biopsy (Cr 1.8) | |||
| 07-0430-01722 | Hereditary nephritis | 75 | 60 | M | C | COL4A3-S1147F, COL4A4-P1587R | 0.655, 0.913 | brother and sister withESRD due to presumedhereditary nephritis | no biopsy (ESRD) | |
| 07-0430-02027 | hereditary nephritis | 46 | 35 | M | C | rs1800516 | aunt on Hemodialysisand cousin with kidneydisease | no biopsy (ESRD) | ||
| 07-0430-00597 | alport’s syndrome | 19 | 6 | M | C | mother withinterrupted COL4A5 staining inskin biopsy | skin negative for COL4A5 (proteinuria) | |||
| 07-0430-00016 | FSGS | 38 | 27 | F | AA | LAMA5-S1469A, LAMA5-V2440I | 0.99, 0.65 | rs34728338, rs36121515, rs80109666 | Father with CKD,diabetes | FSGS (proteinuria) |
| 07-0430-00033 | persumed FSGS | 62 | 20 | M | AA | PLCE1-L2173R, LAMA5-G3685R | 0.999, 1.0 | no family history | no biopsy (inc Cr, HTN) | |
| 07-0430-00048 | persumed FSGS | 45 | 33 | M | C | CAPN12-R229C, LAMA5-E2908V | 1.0, 0.81 | no family history | normal COL4A5 (HTN) | |
| 07-0430-00099 | persumed FSGS | 44 | 32 | M | AA | ACTN4-V801M | 0.013 | Father with ESRD,presumed to haveDiabetes Mellitus | biospy inconclusive (proteinuria) |
Participants in italics are relatives in which the same mutation was found.
Discussion
We applied targeted custom exome capture and next-generation sequencing and identified known and/or novel variants in patients with complex kidney disease or where clinicopathological and genetic correlations were discordant. We first applied our strategy to a 54 year old patient with congenital VUR who presented with heavy proteinuria and diagnosis of FSGS. We discovered COL4A3 mutations that in conjunction with subsequent clinical, family and pathological data undoubtedly identify her as an index case of atypical presentation of AS. We also identified a deleterious SALL2 mutation as a potential cause of her VUR and an unexpected novel MYH9 mutation in the same patient. These results demonstrated the power of targeted exome sequencing on selected genes simultaneously to help understand a complex kidney phenotype in a patient and diagnose AS in the absence of typical symptoms or family history. We further showed that this approach is suitable for screening for mutations in selected genes that are associated with glomerular disorders in patients suspected to have AS or FSGS clinically, or detection of G1 or G2 APOL1 variants in African Americans. The studies suggest that sequencing of a defined set of genes in patients with glomerular diseases or CAKUT may help in early diagnosis and management particularly in complex cases.
We selected several hundred genes important in kidney development and glomerular diseases to identify mutations that may provide insights into the presence of a congenital anomaly (VUR, hydronephrosis) and proteinuria in a patient where the etiology of either entity was unclear since FSGS pattern can be observed in obstructive or reflux nephropathy or primary glomerular diseases. Sequencing of these candidate genes most likely associated with kidney defects and proteinuria revealed 2 mutations in COL4A3 gene, a gene associated with Alport syndrome and SALL2, a gene associated with urinary tract development. Genomic studies confirmed AS in the index patient with no family history of kidney disease, late age of onset, heavy proteinuria, and no hematuria on initial presentation. The patient developed hematuria, sensorineural hearing loss and showed pathological findings characteristic of AS several years after the initial onset of proteinuria. Dysfunction of any of the three-collagen IV genes, COL4A3, COL4A4 and COL4A5, disrupts proper heterotrimer formation resulting in failure to deposit normal collagen matrix in the glomerular basement membrane and disruption of the filtration barrier. Absence of COL4A3 and COL4A5 immunolabeling in the patient’s biopsy further confirmed that the COL4A3 mutations are causative. Pedigree analysis indicated that the two COL4A3 mutations are on different alleles and compound heterozygous. About 15% of AS cases are thought to exhibit autosomal recessive mode of inheritance [13]. Two of this patient’s relatives had COL4A3-L1474P mutation. Whether the second COL4A3-G695R mutation occurred de novo or was inherited is unclear as the samples from the parents were not available. The relatives with the mutations are reportedly healthy indicating that presence of both the mutations is necessary for developing the disease or there could be other modifiers. In this regard, it was interesting that this patient also had a MYH9-L46F mutation. Mutations in MYH9 have been associated with hearing disorders, kidney defects and thrombocytopenia [14], [15]. We found that the patient’s platelet volume was low, but she did not have thrombocytopenia. Since some of the features of AS [16], [17] and patients with MYH9 mutations overlap, it is possible that this patient disease phenotype is a result of interactions between these two genes. No other family members had all three mutations suggesting that only collectively they are penetrant. While both SALL2 and MYH9 mutations likely contribute to the complex phenotype in this patient, biological studies using model systems would be needed to support if these are sufficient or necessary for the phenotype observed. Early onset AS is often associated with large exon deletions, nonsense mutations or splice site changes. The patient had late onset of glomerular disease, which is consistent with the missense COL4A mutations.
Early diagnosis of AS, a rare disorder with frequency of 1∶50,000, is clinically important for counseling and clinical management. Existing common methods to diagnose AS include DHPLC and Sanger sequencing. However the large gene size and high number of exons in each of the COL4 family genes (51 in COL4A5, 48 in COL4A4 and 52 in COL4A3), and absence of any mutation hotspot poses difficulties in timely diagnosis and is costly for researches interested in delineating pathogenetic mechanisms. Recently Artuso et al., applied amplicon based NGS of just the COL4A3 genes in AS [18]. While this approach is preferable to the older methods, in atypical cases and in cases where pathology is equivocal such as segmental COL4A3, 4 or 5 staining or insufficient material, information on additional genes (several hundred or less than 30) that may be contributing is needed. Our approach is more efficient and economical as the dynamic range of number of genes to be surveyed can be easily scaled and it allows for indexing (see below) where several patients or family members can be simultaneously evaluated.
Our multiplexed NGS experiments were conducted on 14 patient samples with 19 genes commonly associated with AS or FSGS including steroid resistant nephrotic syndrome. The advantage was that all samples could be simultaneously sequenced and analyzed for variations in these genes at an average read depth of 200X thus significantly increasing the efficiency of obtaining sequence data. We find this approach preferable when the focus is evaluation of small number of genes as an underlying cause of a clinical condition. We focused on AS and included patients with well-documented clinical history and diagnosis. We also included some patients with presumed diagnosis of hereditary nephritis or family history of kidney disease. Our customized exome capture array harbored a subset of genes associated with AS and nephrotic syndrome and confirmed known or novel mutations in COL4A3, A4 or A5 in four of the five AS patients. Some patients did not have established family history of AS. In two of these patients, we successfully identified novel or known variants that explain their disease. The patients in whom we did not identify deleterious COL4A mutations suggest either that these patients need reevaluation of clinical diagnosis or there are changes in COL4A gene structures that were not identified here. For example, structural changes in the genome and changes in non coding regions will be missed with current method. FSGS patients were included to serve as negative control for AS and to identify any new mutations in FSGS associated genes. The discovery of novel variants in the LAMA5 gene has not been reported before. Interestingly three out of five FSGS patients had a novel LAMA5 mutation predicted to be deleterious. LAMA5 is important in maintaining the glomerular filtration barrier integrity [19]; however to our knowledge it has not been associated with FSGS previously. Two of the FSGS patients also harbor mutations in PLCE1, NPHS1 and ACTN4 genes respectively. These genes are associated with FSGS [20], [21], [22], [23] and suggesti that these variants contribute to the disease. It is possible that some of these could be neutral or beneficial or deleterious mutations. We have included prediction scores (Table 1), but unequivocal proof of causation versus neutral variations would require efficient biological validation strategies. Our methods also successfully identified variants that are associated with FSGS in African Americans further portraying the versatile application of NGS in diagnoses and discovery of variants associated with AS or FSGS.
The candidate gene capture and NGS approach we applied is robust in identifying deleterious mutations in different kidney diseases and more importantly if these mutations can provide insights into disease process. This is the first application of this approach to a complex kidney disease presentation and AS, and detecting defined variants associated with FSGS or Alports. Our study demonstrates an integrated approach that utilizes biological and clinicopathologic information in screening defined set of genes for gleaning insights into disease etiology using NGS. These strategies should pave the way to clinical sequencing and high throughput mutation discovery studies compared to single gene approaches that are now inefficient and costly.
Supporting Information
List of 292 candidate genes shortlisted for exome sequencing studies in the patient with VUR and proteinuria.
(XLS)
List of primers for validation of COL4A3, SALL2, MYH9 and APOL1 gene variations using Sanger sequencing.
(XLS)
List of 19 candidate genes shortlisted for custom multiindexed exome sequencing.able.
(XLSX)
Coverage metrics for 19 gene custom exomes nex-gen sequencing in patients with suspected Alports.
(XLSX)
Acknowledgments
We thank Daniel Martin and Devin Luckett for specimen processing and DNA preparations. We thank Dr. Davis Windus for many helpful suggestions. We are grateful to all the patients who volunteered for this study and their selfless contribution.
Funding Statement
This work was supported by National Institutes of Health (NIH) George M. O’Brien Center for Kidney Disease Research (P30-DK079333) to Washington University, Children Discovery Institute grant MDII2009177 (SJ) and renal division. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Gipson D, Chin H, Presler T, Jennette C, Ferris M, et al. (2006) Differential risk of remission and ESRD in childhood FSGS. Pediatric Nephrology 21: 344–349. [DOI] [PubMed] [Google Scholar]
- 2. Mitsnefes M, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: A report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). American Journal of Kidney Diseases 45: 309–315. [DOI] [PubMed] [Google Scholar]
- 3. Troyanov Sp, Wall CA, Miller JA, Scholey JW, Cattran DC, et al. (2005) Focal and Segmental Glomerulosclerosis: Definition and Relevance of a Partial Remission. Journal of the American Society of Nephrology 16: 1061–1068. [DOI] [PubMed] [Google Scholar]
- 4. Velosa JA, Holley KE, Torres VE, Offord KP (1983) Significance of proteinuria on the outcome of renal function in patients with focal segmental glomerulosclerosis. Mayo Clin Proc 58: 568–577. [PubMed] [Google Scholar]
- 5. Savige J, Rana K, Tonna S, Buzza M, Dagher H, et al. (2003) Thin basement membrane nephropathy. Kidney Int 64: 1169–1178. [DOI] [PubMed] [Google Scholar]
- 6. Dische FE, Weston MJ, Parsons V (1985) Abnormally thin glomerular basement membranes associated with hematuria, proteinuria or renal failure in adults. Am J Nephrol 5: 103–109. [DOI] [PubMed] [Google Scholar]
- 7. Kashtan CE (2004) Familial hematuria due to type IV collagen mutations: Alport syndrome and thin basement membrane nephropathy. Curr Opin Pediatr 16: 177–181. [DOI] [PubMed] [Google Scholar]
- 8.Liapis H, Gaut JP (2012) The renal biopsy in the genomic era. Pediatr Nephrol. [DOI] [PubMed]
- 9. Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, et al. (2009) The Sequence Alignment/Map format and SAMtools. Bioinformatics 25: 2078–2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chatterjee R, Ramos E, Hoffman M, Vanwinkle J, Martin DR, et al. (2012) Traditional and targeted exome sequencing reveals common, rare and novel functional deleterious variants in RET-signaling complex in a cohort of living US patients with urinary tract malformations. Hum Genet 131: 1725–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, et al. (2010) A method and server for predicting damaging missense mutations. Nat Meth 7: 248–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cooke JN, Bostrom MA, Hicks PJ, Ng MC, Hellwege JN, et al. (2012) Polymorphisms in MYH9 are associated with diabetic nephropathy in European Americans. Nephrol Dial Transplant 27: 1505–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cook C, Friedrich CA, Baliga R (2008) Novel COL4A3 mutations in African American siblings with autosomal recessive Alport syndrome. Am J Kidney Dis 51: e25–28. [DOI] [PubMed] [Google Scholar]
- 14. Althaus K, Greinacher A (2009) MYH9-related platelet disorders. Semin Thromb Hemost 35: 189–203. [DOI] [PubMed] [Google Scholar]
- 15. Zhang Y, Conti MA, Malide D, Dong F, Wang A, et al. (2011) Mouse models of MYH9-related disease: mutations in nonmuscle myosin II-A. Blood 119: 238–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gleeson MJ (1984) Alport’s syndrome: audiological manifestations and implications. J Laryngol Otol 98: 449–465. [DOI] [PubMed] [Google Scholar]
- 17. Alves FR, Ribeiro Fde A (2008) Clinical data and hearing of individuals with Alport syndrome. Braz J Otorhinolaryngol 74: 807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Artuso R, Fallerini C, Dosa L, Scionti F, Clementi M, et al. (2012) Advances in Alport syndrome diagnosis using next-generation sequencing. Eur J Hum Genet 20: 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Goldberg S, Adair-Kirk TL, Senior RM, Miner JH (2010) Maintenance of glomerular filtration barrier integrity requires laminin alpha5. J Am Soc Nephrol 21: 579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boyer O, Benoit G, Gribouval O, Nevo F, Pawtowski A, et al. (2010) Mutational analysis of the PLCE1 gene in steroid resistant nephrotic syndrome. J Med Genet 47: 445–452. [DOI] [PubMed] [Google Scholar]
- 21. Koziell A, Grech V, Hussain S, Lee G, Lenkkeri U, et al. (2002) Genotype/phenotype correlations of NPHS1 and NPHS2 mutations in nephrotic syndrome advocate a functional inter-relationship in glomerular filtration. Hum Mol Genet 11: 379–388. [DOI] [PubMed] [Google Scholar]
- 22. Santin S, Garcia-Maset R, Ruiz P, Gimenez I, Zamora I, et al. (2009) Nephrin mutations cause childhood- and adult-onset focal segmental glomerulosclerosis. Kidney Int 76: 1268–1276. [DOI] [PubMed] [Google Scholar]
- 23. Choi HJ, Lee BH, Cho HY, Moon KC, Ha IS, et al. (2008) Familial focal segmental glomerulosclerosis associated with an ACTN4 mutation and paternal germline mosaicism. Am J Kidney Dis 51: 834–838. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of 292 candidate genes shortlisted for exome sequencing studies in the patient with VUR and proteinuria.
(XLS)
List of primers for validation of COL4A3, SALL2, MYH9 and APOL1 gene variations using Sanger sequencing.
(XLS)
List of 19 candidate genes shortlisted for custom multiindexed exome sequencing.able.
(XLSX)
Coverage metrics for 19 gene custom exomes nex-gen sequencing in patients with suspected Alports.
(XLSX)