Abstract
A continuous rise in the rate of cesarean deliveries has been reported in many countries over recent decades. This trend has prompted the emergence of a debate on the risks and benefits associated with cesarean section. The present study was designed to estimate cesarean section rates over time during the period between 2000 and 2010 in Peru and to present outcomes for each mode of delivery. This is a secondary analysis of a large database obtained from the Perinatal Information System, which includes 570,997 pregnant women and their babies from 43 Peruvian public health facilities in three geographical regions: coast, highlands, and jungle. Over 10 years, 558,901 women delivered 563,668 infants weighing at least 500 g. The cesarean section rate increased from 25.5% in 2000 to 29.9% in 2010 (26.9% average; P < 0.01). The rate of stillbirths was lower with cesarean than vaginal deliveries (P < 0.01). On the other hand, and as expected, the rates for preterm births, twin pregnancies, and preeclampsia were higher in women who delivered by cesarean section (P < 0.01). More importantly, the rate of maternal mortality was 5.5 times higher in the cesarean section group than in the vaginal delivery group. Data suggest that cesarean sections are associated with adverse pregnancy outcomes.
Keywords: elective cesarean, emergency cesarean, geographical regions, cesarean rates over time, adverse outcomes, developing country
Introduction
The Millennium Declaration, adopted by the United Nations in 2000, set a series of Millennium Development Goals (MDGs); among them was the aim to reduce maternal mortality by three-quarters by 2015.1 There is growing consensus that a primary bottleneck in achieving MDGs is a health system that is too fragile and fragmented to deliver the appropriate volume and quality of services to those in need.2 Development of more responsive health systems appears to be prerequisite to achieving health-related MDGs.
The implementation of specific new interventions would enable health systems to better respond to the MDGs and make them more attainable. The provision of high-quality pregnancy and delivery care, including emergency obstetric assistance, is central to decreasing the maternal mortality ratio. Not only does the maternal mortality ratio need to be decreased, but also direct etiologies of maternal mortality need to be identified and addressed in order to evaluate the quality of obstetric care.3
In the region of the Americas, the main challenges in meeting the MDGs are: improving and harmonizing health information systems; designing health programs that bring together the set of services and interventions with greatest impact and according to the special characteristics of the targeted populations; strengthening the political will; and guaranteeing funding for the measures undertaken to attain the MDGs.4
Existing data in Peru, a country in South America characterized by differences in health system capacity in its three distinct geographical regions (the coast, the highlands, and the Amazon jungle), reveal that, although a substantial reduction has occurred (185 maternal deaths per 100,000 live births in 2005 to 67 per 100,000 for 2010), high maternal mortality rates still remain in rural and remote areas of the country.5,6
A continuous rise in the rate of cesarean sections has been reported in many countries over recent decades.7 This trend has prompted the emergence of a debate on the risks and benefits associated with cesarean delivery. Previously, in a study in France, cesarean section was associated with an increased risk of postpartum maternal death.8 In a cross-sectional study using data from 119 countries from 1991 to 2003, no association between cesarean section rates and maternal or neonatal mortality was shown in medium- and high-income countries; in low-income countries, however, a negative and statistically significant linear correlation was observed between cesarean section rates and neonatal mortality and between cesarean section rates and maternal mortality.9
With reference to regions as classified for the MDG reporting, maternal mortality ratios in 2005 were highest in developing regions (at 450 maternal deaths per 100,000 live births), in stark contrast to developed regions (nine) and countries of the Commonwealth of Independent States (51). Among the developing regions, sub-Saharan Africa had the highest maternal mortality ratio (at 900) in 2005, followed by South Asia (490), Oceania (430), South-Eastern Asia (300), Western Asia (160), Northern Africa (160), Latin America and the Caribbean (130), and Eastern Asia (50).10
A more recent analysis from an ecological study, based on the latest official data (2000–2009),11 is available for 124 countries and shows that the global median proportion of cesarean deliveries for this time frame was 13.8%. In countries with cesarean rates of less than 15%, higher cesarean rates were associated with lower infant, neonatal, and maternal mortality rates, and with lower rates of low birth weight. In countries with cesarean rates greater than 15%, cesarean rates were not significantly associated with infant or maternal mortality rates.11
In 2005, the World Health Organization (WHO) Global Survey on Maternal and Perinatal Health, in a multistage stratified sample obtained from 120 health facilities, comprising 24 geographic regions in eight countries in Latin America, showed that the rate of cesarean section was positively associated with adverse outcomes such as postpartum antibiotic treatment and severe maternal morbidity and mortality, even after adjustment for risk factors.12
These contrasting results point to the need to study the association between cesarean section rates and maternal health within within sub-national divisions in each country, where differences in intervening factors, such as the population’s access to health services and women’s characteristics, can be taken into account. In Peru, a middle-income country with recent improvements in the economy and the health care system, little is known about cesarean section rates over time in public health care centers nor about the association between cesarean section and maternal mortality rates.
The objective of the present study was to estimate cesarean section rates over time between 2000 and 2010 and present maternal and perinatal outcomes by mode of delivery in Peruvian public health facilities.
Materials and methods
This is a secondary analysis from a dataset of the Perinatal Information System (Sistema Informático Perinatal) obtained from 43 public health facilities (40 hospitals and three health centers) in Peru located in the country’s three main geographical regions, comprising the coast, the highlands, and the Amazon jungle. Data correspond to deliveries that occurred from January 1, 2000 to December 31, 2010. These health facilities are run by the Ministry of Health and serve a population of low to middle socioeconomic status, in which most individuals are without insurance, or have, at best, basic insurance.
The database included a total of 570,997 pregnant women and their newborns from 37 cities of 20 departments. From the total sample, 812 domiciliary deliveries were excluded, as were 9,625 deliveries without data for the newborn, 480 with incoherent birth weight data in relation to gestational age, and 1,179 cases of congenital malformation. The final sample included deliveries from 558,901 pregnant women.
The outcome variables studied were stillbirths, preterm births, small for gestational age, preeclampsia, and maternal mortality. Stillbirths were diagnosed when fetal deaths occurred after 20 weeks of gestation or with weights higher than 500 g. Preterm birth was defined as delivery before 37 weeks of gestational age. Preeclampsia was defined as the presence of pregnancy-induced hypertension (systolic pressure of ≥140 mmHg and/or diastolic pressure of ≥90 mmHg) and proteinuria (≥300 mg/24 hours) after 20 weeks of gestation.
Maternal mortality was defined as the death of a woman while pregnant or within 42 days of the termination of the pregnancy from any cause related to or aggravated by the pregnancy. Maternal mortality ratio was defined as the number of maternal deaths per 100,000 live births.
Elective cesarean section is a planned intervention performed prior to labor on a pregnant woman on the basis of an obstetrical or medical indication or at the request of the pregnant patient. Emergency cesarean section is performed during labor because there is threat to the life of fetus and/or mother.
Hospitals are classified according to their function and complexity. In level I, the hospital offers comprehensive ambulatory care with no major surgery and emphasis on health promotion and prevention. In level II, the hospital provides comprehensive outpatient and inpatient care in the four main specialties. Level III hospitals add more specialization (subspecialties) to the previous category.
Data were analyzed using Stata software (v 10; StataCorp LP, College Station, TX, USA). The chi-square was used for data expressed in proportions. The confidence interval (CI) was defined at 95% for each variable. Rates of cesarean section were estimated according to obstetric characteristic, geographical region, year of birth, and adverse perinatal outcomes. Estimates of crude and adjusted odds ratios (ORs) with 95% CI were computed as measures of association between the variables. Adjusted ORs were derived through logistic regression models. Significance was defined at a value P < 0.05 for all statistical analysis.
The Universidad Peruana Cayetano Heredia (Lima, Peru) institutional review board approved the protocol.
Results
Over the 10 years in the database, 558,901 women delivered 563,668 infants weighing at least 500 g. The cesarean section rate increased from 25.52% in 2000 to 29.96% in 2010 (P < 0.01) (average of 26.9%). The institutional maternal mortality ratio was 30 per 100,000 live births. There were 91 maternal deaths following elective cesarean sections and 70 maternal deaths following emergency cesarean sections. Cesarean sections in general were more frequent at the coast (32.8%) than in the highlands (23.7%) (P < 0.01) or Amazon jungle (20.6%) (P < 0.01). However, elective cesarean sections were more frequent in the jungle (58.2%) than in the highlands (56.1%) (P < 0.01) and the coast (52.1%) (P < 0.01). Cesarean section was nearly seven times more associated with a prior cesarean section (24% versus 3.6%; P < 0.01) and four times more with preeclampsia (9.5% versus 2.2%) than with a vaginal delivery; P < 0.01.
At level II and III hospitals, the highest rate of cesarean section occurred at the coast (P < 0.01), followed by the highlands and the jungle. As expected, elective cesarean sections were more frequent at level II hospitals compared to elective cesarean sections at level III (P < 0.01) (Table 1).
Table 1.
Rates of vaginal deliveries, cesarean deliveries, and elective cesarean deliveries in each Peruvian geographical region (coast, highlands, jungle) in 43 health care centers according to scarred uterus, prior pregnancies, preeclampsia, and level of the hospital in which deliveries were attended
| Population (563,668)
|
Vaginal deliveries (411,558)
|
Cesarean deliveries (all types) (152,110)
|
Elective cesarean deliveries (82,621)
|
|||
|---|---|---|---|---|---|---|
| Characteristic | N | % | n | % | n | % |
| Geographical region | ||||||
| Coast (245,385) | 164,841 | 67.2 | 80,544 | 32.8 | 41,937 | 52.1 |
| Highlands (192,530) | 146,930 | 76.3 | 45,600a | 23.7 | 25,563a | 56.1 |
| Jungle (125,753) | 99,787 | 79.4 | 25,966a,b | 20.6 | 15,121a,b | 58.2 |
| Scarred uterus | ||||||
| Coast (29,859) | 7,605 | 25.5 | 22,254 | 74.5 | 12,999 | 58.4 |
| Highlands (12,394) | 4,115 | 33.2 | 8,279a | 66.8 | 5,270 | 63.7 |
| Jungle (9,208) | 3,185 | 34.6 | 6,023a,c | 65.4 | 3,938 | 65.4 |
| Multiparous | ||||||
| Coast (144,893) | 96,489 | 66.6 | 48,404 | 33.4 | 26,845 | 55.5 |
| Highlands (114,115) | 85,222 | 76.7 | 25,893a | 23.2 | 15,295 | 59.1 |
| Jungle (83,839) | 67,034 | 80.0 | 16,805a,c | 20.0 | 10,153 | 60.4 |
| Preeclampsia | ||||||
| Coast (13,369) | 4,517 | 33.8 | 8,852 | 66.2 | 5,153 | 58.2 |
| Highlands (5,590) | 2,113 | 37.8 | 3,477a | 62.2 | 2,308 | 66.4 |
| Jungle (4,431) | 2,246 | 50.7 | 2,185a,b | 49.3 | 1,431 | 65.5 |
| Level II hospital | ||||||
| Coast (8,896) | 6,310 | 70.9 | 2,586 | 29.1 | 1,827d | 70.7 |
| Highlands (23,093) | 18,715 | 81.0 | 4,378a | 19.0 | 2,801d | 64.0 |
| Jungle (21,229) | 18,164 | 85.6 | 3,065a,c | 14.4 | 2,131d | 69.5 |
| Level III hospital | ||||||
| Coast (236,254) | 158,359 | 67.0 | 77,895 | 33.0 | 40,059 | 51.4 |
| Highlands (167,481) | 126,955 | 75.8 | 40,526a | 24.2 | 22,369 | 55.2 |
| Jungle (104,124) | 81,395 | 78.2 | 22,729a,c | 21.8 | 12,862 | 56.6 |
Notes: The sum of the first and second columns represents the total number of deliveries (vaginal and cesarean sections).
P < 0.01 with respect to deliveries at the coast;
P < 0.01 with respect to deliveries in the highlands;
P < 0.05 with respect to deliveries in the highlands;
P < 0.01 with respect to elective cesarean section deliveries observed in level III hospitals.
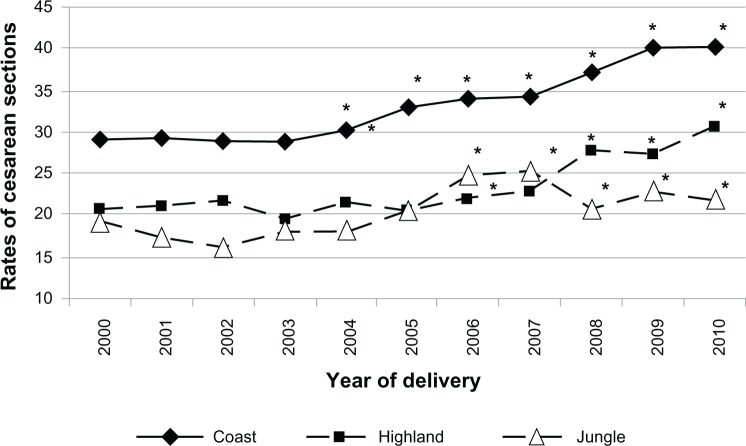
In the three geographical regions of Peru, cesarean section rates increased over time. The highest rates were observed in the coast, increasing more than 10 percent points from 2000 to 2010, to reach 40% in 2010 (P < 0.05 from 2004 to 2010, compared with 2000). In highland and jungle regions, the cesarean section rate was approximately 20% in 2000 and increased to 30% in the highlands (P < 0.05) and slightly higher than 20% in the jungle by 2010 (P < 0.05 since in 2006 the rate was much higher with respect to the year 2000) (Figure 1).
Figure 1.
Trends for cesarean section rates in Peru according to geographical region, 2000–2010.
Note: *chi-square test: P < 0.05 compared to year 2000.
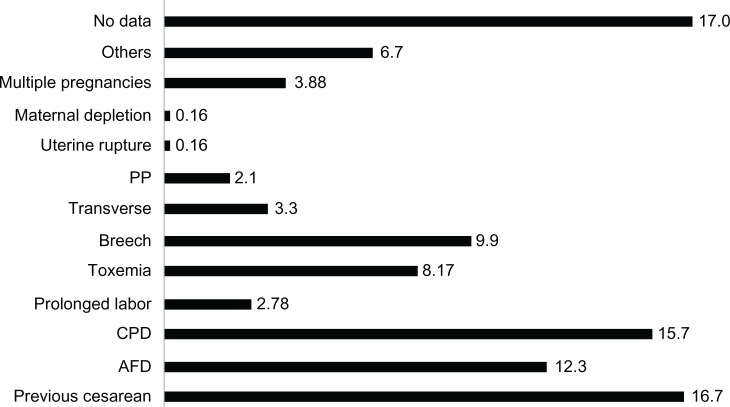
The distribution of cesarean sections by indication is presented in Figure 2. A previous cesarean section constituted the dominant indication (16.7%). Cephalopelvic disproportion, fetal suffering, the failure of trial labor, and breech presentation were other important indications for cesarean section. It is important to note that a sizable 17% of cases did not record any indication.
Figure 2.
Main indications for cesarean section rates in 43 Peruvian health facilities, 2000–2010.
Abbreviations: AFD, acute fetal distress; CPD, cephalopelvic disproportion; PP, placenta previa.
Elective cesarean rates from 2000 to 2010 in the three geographical regions in Peru followed the same pattern as for total cesarean rates (data not shown). The highest elective cesarean rates were observed at the coast (P < 0.01). Values of elective cesarean rates at the coast were higher than the total elective cesarean rates (P < 0.01). The lowest elective cesarean rates were observed in health facilities located in the Amazon region (P < 0.01). In the coast, elective cesarean section rates increased until 2009. In the highlands, elective cesarean section rates increased until 2010. In the jungle, elective cesarean section rates were maintaned from 2000 to 2007, but thereafter rates were reduced (reaching rates similar to 2010).
The rate of stillbirths was lower with cesarean section than with vaginal deliveries (P < 0.01). On the other hand, and as expected, the rates for preterm births, twin pregnancies, and preeclampsia were higher in women who delivered by cesarean section (P < 0.01). The maternal mortality rate was 5.5 times higher in the cesarean section group than in the vaginal delivery group (Table 2).
Table 2.
Rates of adverse pregnancy outcomes according to the mode of delivery (vaginal or cesarean section) in 43 health facilities in Peru, 2000–2010
| Pregnancy outcome* | Vaginal delivery (411,558)
|
Cesarean section delivery (152,110)
|
||
|---|---|---|---|---|
| n | % | n | % | |
| Stillbirth | 6,037 | 1.47 | 2,135 | 1.40 |
| Preterm delivery | 21,293 | 5.17 | 15,430 | 10.1 |
| Twin pregnancy | 3,541 | 0.86 | 5,930 | 3.9 |
| Maternal mortality | 76 | 0.02 | 165 | 0.11 |
| Preeclampsia | 8,876 | 2.16 | 14,514 | 9.54 |
Note:
chi-square test: P < 0.01 between data after vaginal and cesarean section deliveries.
We grouped the health facilities according to different levels of cesarean section rates (<10%, 10%–20%, 20%–30%, >30%) and looked for any associations with stillbirths, preterm births, preeclampsia, and maternal mortality rates (Table 3). With respect to stillbirths and preterm deliveries, health facilities with cesarean section rates over 30% were associated with lower rates of stillbirths compared to health facilities with less than 30% cesarean section rates (P < 0.0001) or compared to the group of women with vaginal delivery in the same group of health facilities (P < 0.0001). Preterm births were higher in the groups with cesarean section rates.
Table 3.
Rates of adverse pregnancy outcomes in 43 health facilities in Peru by type of delivery within each cesarean section rate (CSR) level, 2000–2010
| Health facility deliveries by CSR level (n) | Stillbirths (8,172)
|
Preterms (36,723)
|
Preeclampsia (23,390)
|
Maternal mortality (241)
|
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| CSR < 10% (2) | 1 | 1.72 | 3 | 5.17 | – | – | ||
| C-section (58) | ||||||||
| Vaginal (918) | 4 | 0.44 | 27 | 2.94 | – | – | ||
| CSR 10%–20% (12) | 341 | 1.97a | 1,937 | 11.19a | 1,579 | 9.13a | 16 | 0.09 |
| C-section (17,299) | ||||||||
| Vaginal (90,260) | 1,086 | 1.20b | 4,770 | 5.28b | 1,774 | 1.97b | 14 | 0.02b |
| CSR 20%–30% (18) | 948 | 1.52a | 6,846 | 11.00a | 5,381 | 8.64a | 75 | 0.12 |
| C-section (62,231) | ||||||||
| Vaginal (188,019) | 2,831 | 1.51 | 9,646 | 5.13b | 3,501 | 1.86b | 37 | 0.02b |
| CSR > 30% (11) | 845 | 1.17 | 6,644 | 9.16 | 7,554 | 10.42 | 74 | 0.10 |
| C-section (72,522) | ||||||||
| Vaginal (132,361) | 2,116 | 1.60b | 6,850 | 5.17b | 3,601 | 2.72b | 25 | 0.02b |
Notes: In each facility group, vaginal deliveries and their association with stillbirths, preterm births, preeclampsia, and maternal mortality were also assessed.
P < 0.0001 with respect to the value observed in the CSR > 30% group;
P < 0.0001 with respect to the adverse outcome observed after cesarean section.
Preeclampsia was more common among women who underwent a cesarean section than in those who had a vaginal delivery (P < 0.0001). In addition, preeclampsia was more common in health facilities categorized as centers with cesarean section rates >30% (P < 0.0001).
Institutional maternal mortality ratios were 108 per 100,000 for cesarean deliveries and 18 per 100,000 for vaginal deliveries (P < 0.0001). Additionally, the maternal mortality ratios between health facilities with different cesarean section rates were not statistically different (P > 0.05) (Table 3).
During the study period, cesarean deliveries after prior cesarean section increased slightly from 2006 to 2010, with the highest rates seen in the coast and the lowest rates in the Amazon basin (data not shown).
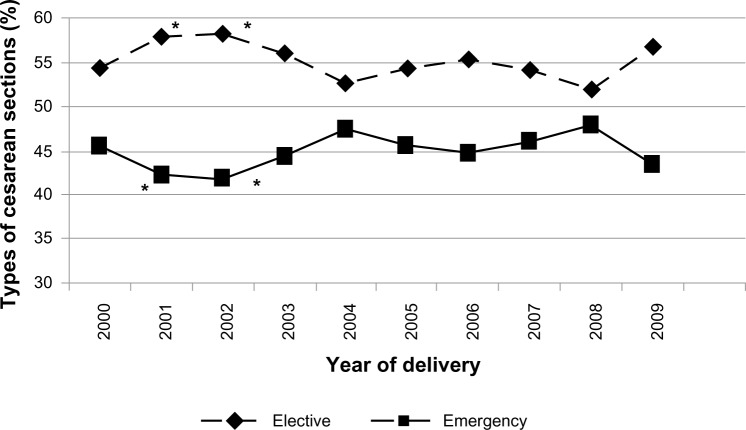
Comparing rates of elective and emergency cesarean sections, Figure 3 shows that elective cesarean section rates were higher in the years 2001 and 2003 with respect to year 2000 (P < 0.05), but, thereafter, the values remained similar to those in year 2000 (P > 0.05).
Figure 3.
Trends for elective and emergency cesarean deliveries in 43 Peruvian health care centers, 2000–2010.
Note: *chi-square test: P < 0.05 compared to year 2000.
Given the findings about maternal mortality displayed in Table 3, a logistic regression analysis was performed for several characteristics. Analyses showed that elective cesarean section (P = 0.001), emergency cesarean section (P = 0.001) (compared to vaginal delivery), living in the highland (P = 0.001) or Amazon jungle regions (P = 0.003) (compared to the coast; P = 0.012), and receiving care in a level I or III hospital (compared to level II) were associated with higher ORs for maternal mortality, whereas previous cesarean section was associated with lower ORs for maternal mortality (P = 0.012) (Table 4). After adjusting for confounders (age, body mass index, anemia, preeclampsia, prenatal care, twin pregnancy, and urinary tract infections), elective and emergency cesarean both had more than four times the ORs for maternal mortality than with vaginal delivery.
Table 4.
ORs for maternal mortality associated with cesarean deliveries in 43 Peruvian health care centers, 2000–2010
| Characteristic | Maternal mortality
|
||||
|---|---|---|---|---|---|
| ORc | P | ORa | P | 95% CI | |
| Mode of delivery | |||||
| Vaginal | 1.0 | – | 1.0 | – | – |
| Elective cesarean | 6.10 | 0.001 | 4.45 | 0.001 | 3.21 6.18 |
| Emergency cesarean | 5.61 | 0.001 | 4.82 | 0.001 | 3.44 6.75 |
| Geographical region | |||||
| Coast | 1.0 | – | 1.0 | – | – |
| Highlands | 1.34 | 0.04 | 1.83 | 0.001 | 1.35 2.48 |
| Jungle | 1.10 | 0.57 | 1.69 | 0.003 | 1.19 2.40 |
| Previous cesarean | |||||
| No | 1.0 | – | 1.0 | – | – |
| Yes | 1.05 | 0.823 | 0.56 | 0.012 | 0.36 0.88 |
| Hospital level | |||||
| I | 7.71 | 0.027 | 5.55 | 0.012 | 1.46 21.0 |
| II | 1.0 | – | 1.0 | – | – |
| III | 3.01 | 0.004 | 2.37 | 0.017 | 1.16 4.08 |
Notes: Logistic regression model adjusted by age, body mass index, anemia, preeclampsia, prenatal care, twin pregnancy, urinary tract infections, and previous cesarean delivery.
Abbreviations: CI, confidence interval; OR, odds ratio; ORa, adjusted OR; ORc, crude OR.
Discussion
The cesarean section rates in this study are comparable to others in Latin American countries.12 The mean cesarean section rate in Peru for the period 2000–2010 in 43 public health facilities was found to be 26.9%. WHO recommends maintaining cesarean delivery rates to between 5% and 15% of total births: the lower limit represents the expected rate of interventions to prevent maternal mortality and/or severe morbidity, and the upper is the limit above which no improvements in maternal and neonatal health outcomes can be expected to be observed.13
Thus, the rate of cesarean sections in these Peruvian facilities exceeds the currently recommended cesarean section rates at population level. This could be due in part to the fact that several of them may be referral hospitals, which receive relatively more cases with complications than the average hospital.
In Peru, data from 2008 show that 58% of the population were not covered by any type of social insurance (private or public) and needed to use the services offered by the Ministry of Health through the public health system. With respect to the population with insurance (42%), 20% was covered by the social security system (EsSalud), 18% by the Integrated Health Insurance (issued by the Ministry of Health), 2% by private insurance, and 2% by the military and police forces.6
As observed in other countries,7 cesarean section rates in public health care centers in Peru has increased over time, but also differentially between geographical regions, with the highest rates found in maternity units located in the coast and the lowest in the Amazon jungle. A key finding was the high contribution of elective cesarean sections to the total cesarean delivery rates observed in Peru (54.3%).
In Peru, the population with the least resources is located in the jungle,14 and it is in this region that the lowest rates of cesarean sections were observed. This may indicate inequities in the use of cesarean sections in particular and of health care in general.15 The finding that relatively higher rates of elective cesarean section were observed in the jungle seems to be due to the fact that level III hospitals in the jungle have more elective cesarean sections than level III hospitals at the coast or in the highlands; the reasons for this are, however, unknown.
In the poorest countries of the world, mostly in sub-Saharan Africa, large segments of the population have almost no access to potentially life-saving cesarean sections.16,17 On the other hand, the Latin America region presents the highest average of deliveries by cesarean section worldwide. Large inequities are present, however, and cesarean section rates are lowest in Haiti, where less than 2% of deliveries occur by cesarean section, and highest in Brazil, Mexico, and Chile.17 In Brazil, about 40% of deliveries occur by cesarean section, which represents the highest rate worldwide.17 Peru’s latest (2012) national estimate of the proportion of deliveries by cesarean section is 25% (and 49% among the wealthier women) and it leans towards the high end of Latin American countries.14 In this context, our study adds to the literature documenting inequities not only between countries, but also within a country.
In 1985, WHO stated that “There is no justification for any region to have cesarean section rates higher than 10%–15%.”18 This recommendation was based on the scarce data available at the time, which did not demonstrate any benefits from higher rates of cesarean section in relation to maternal or perinatal mortality at population or hospital level. Very low and very high rates of cesarean section can be dangerous, but the “optimal” or “ideal” rate is unknown and may depend on the setting, patient circumstances, and availability of resources. There is global concern about the existence of cesarean section on demand, and it is important to understand the modifiable causes of rising cesarean section rates. In order to propose and implement effective measures to reduce or increase cesarean section rates where necessary, it is first essential to identify what groups of women are undergoing cesarean sections and to investigate the underlying reasons for trends in different settings. This requires the use of a classification system to monitor and compare cesarean section rates in a standardized, reliable, consistent, and action-oriented manner. In 2011, investigators from WHO reviewed several systems and identified the Robson system as the best one for this purpose. Many facilities and studies are implementing this system, which is helping to understand better the subpopulations and conditions associated with this procedure.19
A previous cesarean section has been reported as an important risk factor for delivering by cesarean section in subsequent pregnancies in countries with high cesarean rates,20 a factor that could be modified with appropriate policy and guidelines. As seen in another study,21 when cesarean delivery was medically indicated, the dominant indication was a cicatricial uterus. Currently, there are a number of recommended ways by which to encourage vaginal delivery in women with prior cesarean section.22,23 Similarly, our study shows that, in Peru, one of the main indications for cesarean section was a previous cesarean section. However, 17% of cesarean sections have no indications. It is possible that these could be normal pregnancies that ended in cesarean sections without medical indication.
Our study also shows a relative proportion of elective cesarean sections higher than expected (>50%). This is extremely high compared to other settings, such as Bangladesh, where elective cesarean sections were reported to be 30% of all cesarean sections.24 In Dublin, Ireland, the proportion of elective cesarean sections between January 1 and December 31, 2009, was also less than 50% in relation to emergency operations.25 Requests for cesarean section have been observed more commonly in private clinics.26 However, our study included public health facilities serving low-middle and low socioeconomic status populations, in which insurance schemes (eg, social security or private insurance) are uncommon. Hence, it is worth investigating further the conditions under which these operations are performed and the responsibility and role of the medical profession in these high rates of elective cesarean section.
Increased rates of cesarean section in private clinics in Peru have also occurred as an effect of the 1997 health reform. This health reform, by improving medical insurance and liberalizing access of the population to the private sector, may have increased physicians’ incentives to use cesarean section, raising rates from 28% to 53% in the private sector. Comparable trends in cesarean section rates have been observed in Latin American countries that implemented similar reforms in their private sector.26
In a recent worldwide study, 47.2% of the studied countries had cesarean section rates that exceeded 15%. Countries in Latin America and the Caribbean, along with countries in Europe, North America, and Oceania, had the highest rates. In this study, an inverse association between cesarean section rates and maternal mortality was observed for all regions except Europe.27 This is not the case with the data from Peru, where we have observed a direct association between cesarean section rates and maternal mortality. This could suggest that the quality of health services and of the procedure in particular may not be adequate. However, further research is required to demonstrate this hypothesis. Moreover, from 165 maternal deaths associated with cesarean sections, 91 were associated with elective cesarean sections. In addition, the rate of maternal mortality was higher with primary cesarean sections than those with a previous cesarean section. This finding is of critical significance if elective procedures may not have followed a medical indication.
The maternal mortality rate in Peru has fallen by 50% over the period between 2000 and 2011. A comparison of maternal mortality ratios from three Demographic and Family Health Surveys (La Encuesta Demográfica y de Salud Familiar [ENDES]) shows that maternal mortality ratios fell from 265 per 100,000 live births in the 1996 survey to 185 in 2000 and to 93 deaths per 100,000 live births in the 2011 survey.14
According to the United Nations, Peru, despite the progress, still has a maternal mortality rate that is among the highest in the Americas.10 Hence, it is important to identify causes of this elevated maternal mortality ratio. Although cesarean sections were associated in this analysis with high mortality rates, it is necessary to analyze the severity of cases that undergo cesarean section compared to vaginal delivery. Since data from the Perinatal Information System do not allow this type of comparison, further studies need to conduct an in-depth analysis of factors associated with maternal deaths in Peru. Analysis of this type should include a review of indications for cesarean section and the conditions and circumstances in which they are performed.
Through the National Institute of Health of the Ministry of Health, research priorities that have been identified in Peru for the period 2010–2014. These are research to address the problems of human health resources; research to recognize mental health problems; impact evaluations of the social programs for reduction of child malnutrition; impact evaluations of the social programs for actual interventions in maternal mortality; and operational research and impact evaluations of interventions in communicable diseases.28 Results from our study will be of importance when looking at programs aimed at reducing high rates of cesarean sections, particularly when the procedure is medically unjustified.
Factors involved in the rise of deliveries by cesarean section are multiple and may need a multifaceted approach, because no single strategy is likely to be effective or lead to sustained change.29 This is particularly true in countries such as Peru, in which access to health services remains unequal, both within and between different geographical regions. Further studies are needed to ascertain the burden faced by both disadvantaged as well as more better-off women in relation to their exposure to cesarean sections and ultimately to adverse outcomes of pregnancy.
An important caveat of this study is that, for medically indicated cesarean sections, the observed increased risk of worse maternal outcomes could be attributed to the baseline conditions that caused the procedure to be undertaken and not to the procedure itself, and thus a causal relationship between cesarean sections and the outcomes cannot be proposed. This double causality problem could be solved by focusing on women with “no indicated risk.”30 Although we have assessed through logistic regression the crude and adjusted ORs for maternal mortality after controlling for type of delivery (vaginal births, elective cesarean sections, and emergency cesarean sections), we have found that, in both cases of cesarean section, the OR increased four times the value on women with no indicated risk (vaginal delivery). However, we recognize that a limitation of the study is not being able to distinguish between high-risk and low-risk pregnancies. An additional limitation of our study is that, although we adjusted for some potential confounding factors, there may be other factors about which we had no information and could not adjust for.
Conclusion
This study shows that cesarean section rates in the network of investigated Peruvian Public Health hospitals exceed the internationally recommended rates and that the rates are increasing over time, elective cesarean sections being more common than emergency procedures. Differences exist between geographical regions, which likely reflect different practices and capacities, with higher rates observed at the coast than in the highlands and Amazon areas. It is likely that many deliveries in public hospitals are of high risk. In Peru, in 2008, 11% of deliveries still occurred in the home.31 It is plausible, therefore, that many high-risk births are referred to public hospitals, and, as a consequence, cesarean section and maternal mortality rates are higher in public hospitals.
Acknowledgments
The present study was supported by a grant from UNDP/UNFPA/UNICEF/WHO/Work Bank Special Programme of Research Development and Research Training in Human Reproduction at WHO. The funding sources had no involvement in the design, analysis, or reporting of this study.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.United Nations Millennium Declaration Resolution adapted by the General Assembly; 55th Session of the United Nations General Assembly; September 18, 2000; New York. [Google Scholar]
- 2.Travis P, Bennett S, Haines A, et al. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364(9437):900–906. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- 3.Estimates developed by WHO, UNICEF, UNFPA and The World Bank. World Health Organization; Geneva, Switzerland: 2010. World Health Organization Trends in Maternal Mortality: 1990 to 2008. [Google Scholar]
- 4.Torres C, Mújica OJ. Health, equity, and the Millennium Development Goals. Rev Panam Salud Publica. 2004;15(6):430–439. doi: 10.1590/s1020-49892004000600012. Spanish. [DOI] [PubMed] [Google Scholar]
- 5.Alcalde-Rabanal JE, Lazo-González O, Nigenda G. The health system of Peru. Salud Publica Mex. 2011;53(Suppl 2):s243–s254. Spanish. [PubMed] [Google Scholar]
- 6.World Health Organization . Maternal, Newborn and Child Survival. Washington DC: World Health Organization and UNICEF; 2012. Building a Future for Women and Children: The 2012 Report. Countdown to 2015. [Google Scholar]
- 7.Niino Y. The increasing cesarean rate globally and what we can do about it. Biosci Trends. 2011;5(4):139–150. doi: 10.5582/bst.2011.v5.4.139. [DOI] [PubMed] [Google Scholar]
- 8.Deneux-Tharaux C, Carmona E, Bouvier-Colle MH, Bréart G. Postpartum maternal mortality and cesarean delivery. Obstet Gynecol. 2006;108(3 Pt 1):541–548. doi: 10.1097/01.AOG.0000233154.62729.24. [DOI] [PubMed] [Google Scholar]
- 9.Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, Bergel E. Cesarean section rates and maternal and neonatal mortality in low-,medium-, and high-income countries: an ecological study. Birth. 2006;33(4):270–277. doi: 10.1111/j.1523-536X.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Maternal Mortality in 2005. Estimates developed by WHO, UNICEF, UNFPA and the World Bank; Geneva: Switzerland: 2007. p. 39. [Google Scholar]
- 11.Volpe FM. Correlation of Cesarean rates to maternal and infant mortality rates: an ecologic study of official international data. Rev Panam Salud Publica. 2011;29(5):303–308. doi: 10.1590/s1020-49892011000500001. [DOI] [PubMed] [Google Scholar]
- 12.Villar J, Valladares E, Wojdyla D, et al. WHO 2005 global survey on maternal and perinatal health research group Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–1829. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 13.Chalmers B, Mangiaterra V, Porter R. WHO principles of perinatal care: the essential antenatal, perinatal, and postpartum care course. Birth. 2001;28:202–207. doi: 10.1046/j.1523-536x.2001.00202.x. [DOI] [PubMed] [Google Scholar]
- 14.Instituto Nacional de Estadística e Informática . Perú: Encuesta Demográfica y de Salud Familiar (ENDES) 2011. [Peru: national population and family health 2011] Lima: INEI; 2012. p. 438. Spanish. [Google Scholar]
- 15.Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012;206(4):331. e1–e19. doi: 10.1016/j.ajog.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 16.Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries: a retrospective analysis. Lancet. 2006;368:1516–1523. doi: 10.1016/S0140-6736(06)69639-6. [DOI] [PubMed] [Google Scholar]
- 17.Betrán AP, Merialdi M, Lauer JA, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21(2):98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization Appropriate technology for birth. Lancet. 1985;2:436–437. [PubMed] [Google Scholar]
- 19.Torloni MR, Betran AP, Souza JP, et al. Classifications for cesarean section: a systematic review. PLoS One. 2011;6(1):e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyle A, Reddy UM. Epidemiology of cesarean delivery: the scope of the problem. Semin Perinatol. 2012;36(5):308–314. doi: 10.1053/j.semperi.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Messaoudi F, Yazidi M, Ben Jemaa S, et al. Cesarean deliveries in the maternity of military hospital of Tunis. Indication and prognosis: about 5008 cases. Tunis Med. 2007;85(8):659–664. French. [PubMed] [Google Scholar]
- 22.Basic E, Basic-Cetkovic V, Kozaric H, Rama A. Ultrasound evaluation of uterine scar after Cesarean section and next birth. Med Arh. 2012;66(3 Suppl 1):41–44. doi: 10.5455/medarh.2012.66.s41-s44. [DOI] [PubMed] [Google Scholar]
- 23.Yokoi A, Ishikawa K, Miyazaki K, Yoshida K, Furuhashi M, Tamakoshi K. Validation of the prediction model for success of vaginal birth after cesarean delivery in Japanese women. Int J Med Sci. 2012;9(6):488–491. doi: 10.7150/ijms.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saha L, Chowdhury SB. Study on primary cesarean section. Mymensingh Med J. 2011;20(2):292–297. [PubMed] [Google Scholar]
- 25.Turner MJ. The use of quality control performance charts to analyze cesarean delivery rates nationally. Int J Gynaecol Obstet. 2011;113(3):175–177. doi: 10.1016/j.ijgo.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 26.Arrieta A. Health reform and cesarean sections in the private sector: the experience of Peru. Health Policy. 2011;99:124–130. doi: 10.1016/j.healthpol.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 27.Zizza A, Tinelli A, Malvasi A, et al. Caesarean section in the world: a new ecological approach. J Prev Med Hyg. 2011;52(4):161–173. [PubMed] [Google Scholar]
- 28.Caballero P, Yagui M, Espinoza M, et al. Regional and national priorities in health research, Peru 2010–2014: a process with a participative and decentralist approach. Rev Peru Med Exp Salud Publica. 2010;27(3):398–411. doi: 10.1590/s1726-46342010000300013. Spanish. [DOI] [PubMed] [Google Scholar]
- 29.Main EK, Morton CH, Melsop K, Hopkins D, Giuliani G, Gould JB. Creating a public agenda for maternity safety and quality in cesarean delivery. Obstet Gynecol. 2012;120(5):1194–1198. doi: 10.1097/aog.0b013e31826fc13d. [DOI] [PubMed] [Google Scholar]
- 30.MacDorman MF, Declercq E, Menacker F, Malloy MH. Infant and neonatal mortality for primary cesarean and vaginal births to women with “no indicated risk,” United States, 1998–2001 birth cohorts. Birth. 2006;33(3):175–182. doi: 10.1111/j.1523-536X.2006.00102.x. [DOI] [PubMed] [Google Scholar]
- 31.Instituto Nacional de Estadística e Informática . Perú: Nacimientos, 2005–2008. Dirección Técnica de Demografía e Indicadores Sociales. [Peru: births, 2005–2008 Technical direction, demographic and social indicators] Lima: INEI; 2010. p. 185. Spanish. [Google Scholar]