Abstract
The Nine Mile phase II clone 4 (NMIIC4) strain of Coxiella burnetii is an attenuated phase II strain that has lost the genes for virulence determinant type 1 lipopolysaccharide. These bacteria were very virulent for severe combined immunodeficient (SCID) mice. The lethal dose 50 (LD50) was ∼10 bacteria. Infected SCID mice died between Day 28 and Day 53 post-infection. At termination of the experiment (Day 60) only 5 of 24 mice had survived. The degree of splenomegaly was directly related to the bacterial load in the SCID mice spleens. The NMIIC4 was avirulent in immunocompetent wild mice and bacterial DNA copies in splenic tissue were extremely low. The SCID mice that were inoculated with high doses of heat inactivated NMIIC4 C. burnetii were all alive at Day 60 and without splenomegaly. It appears that the phase I lipopolysaccharide present in virulent Nine Mile phase I but not in attenuated NMIIC4 is not the only virulence factor for C. burnetii.
Background
Coxiella burnetii is the etiologic agent of human Q fever, an infectious disease that was first reported by Derrick in Australia.1 Coxiella burnetii is a pleomorphic obligate intracellular bacterium that has two antigenic forms, naturally occurring (wild-type) phase I and attenuated (laboratory adapted) phase II. The transition from virulent phase I to non-pathogenic/avirulent phase II is caused by the loss of the methylated sugars virenose and dihydrohydroxystreptose2,3 and other sugar components of the “O” antigen side chains of the lipopolysaccharide (LPS) molecule. Such variations in the LPS of phase I and phase II bacteria are linked to shifts in antigenicity and virulence.4–6
The Nine Mile phase II clone 4 (NMIIC4) strain of C. burnetii was derived from the virulent Nine Mile phase I (NMI) strain through repeated passage in embryonated eggs and has become antigenically distinct.5 Its genome has a large deletion in an area necessary for O-antigen synthesis.7 The strain RSA541 (also known as “Crazy”) and two other phase II isolates; Nine Mile phase II clone 1 and Nine Mile Baca contained similar large deletions in their genome.7,8 However, the strain RSA514 “Crazy” shows properties similar to NMI9,10 and this observation led to speculation that there may be a basis for expression of virulence other than the phase I LPS.
The phase II LPS of C. burnetii is more readily exposed to components of the host's immune system than phase I LPS.3 Both cellular and humoral immune responses are involved in host resistance to infection by C. burnetii and both are stimulated by challenge with viable cells or vaccination.11,12 Experimental infection in severe combined immunodeficient (SCID) mice also showed that acquired immunity is essential for the host to clear infection by phase II C. burnetii. The innate immune response of SCID mice was only sufficient to slow the replication of C. burnetii but not sufficient to clear the infection.13 The pathogenicity of Q fever and the role of immune components in a wide range of immunodeficient mice infected with NMI and NMIIC4 bacteria have been described.14 The T cells were critical for clearance of NMI or NMIIC4 C. burnetii, and gamma interferon and toll-like receptor 2 were essential for the early control of infection. The B cells were important for the prevention of tissue damage.15
The avirulent NMIIC4 strain can infect and establish persistent infections in a wide variety of laboratory cell lines, and is easier to grow in culture than the wild-type phase I organism.16 The SCID mouse has no functional T and B cells17,18 and are highly susceptible to various pathogens. However, some SCID mice have been known to be “leaky” and occasionally produce small numbers of T and B cells.19 A SCID mouse model of lethal Q fever using the NMI strain of C. burnetii, has been described in Reference 20. All genogroups of C. burnetii phase I isolates produced disease in the SCID mouse model.21 Comparative virulence of phase I and II C. burnetii in immunodeficient mice has also been described in Reference 13. Cloned NMI and NMIIC4 were used in SCID and SCIDbg (lacking T, B, and NK cells) mice. That study used a fixed dose of C. burnetii and short infection time in contrast to the current study, which was carried out to determine the dose response of NMIIC4 in SCID mice over a longer experimental period, determining the quantitative bacterial load in spleen tissue and the Lethal Dose 50 (LD50) of NMIIC4.
Materials and Methods
The avirulent NMIIC4 strain of Coxiella burnetii was grown in a VERO (African green monkey epithelial cell) cell line. The monolayer was scraped following the visible cytopathic effect and 10-fold dilutions of the NMIIC4 cell suspension were prepared. The bacterial load in each dilution was quantified using a quantitative real time polymerase chain reaction (qPCR) assay. A total of eight 10-fold dilutions were used (10−1 to 10−8) ranging from 4.1×107 to < 1 NMIIC4 C. burnetii per 0.1 mL of inocula Table 1.
Table 1.
Death (or terminal euthanasia) of SCID mice following intraperitoneal (i/p) inoculation of different doses of viable Coxiella burnetii NMIIC4, mortality, and Coxiella burnetii loads in the infected SCID mice spleens*
| Group | Ten-fold dilution of inocula | C. burnetii numbers per inocula (0.1 mL) | Mortality of mice | Day of mouse death | Average number of C. burnetii in mouse spleen (0.1 mL) |
|---|---|---|---|---|---|
| 1 | 10−1 | 4.1×107 | 3/3 | 28, 28, 35 | 3.2×107 |
| 2 | 10−2 | 2.8×106 | 3/3 | 30, 31, 35 | 3.9×107 |
| 3 | 10−3 | 3.8×105 | 3/3 | 28, 28, 30 | 4.5×107 |
| 4 | 10−4 | 1.9×104 | 3/3 | 32, 42, 53 | 6.8×107 |
| 5 | 10−5 | 2.4×103 | 2/3 | 37, 41 | 3.3×107 |
| 6 | 10−6 | 0.8×102 | 3/3 | 38, 39, 42 | 5.2×107 |
| 7 | 10−7 | 1.2×101 | 2/3 | 39, 46 | 4.3×107 |
| 8 | 10−8 | 1 | 0/3 | No deaths | 2.8×101 |
| Control group A (SCID mice) | 10−1 (heat killed) | 4.1×107 | 0/3 | No deaths | 1.0×103 |
| Control group B (wild mice) | 10−1 (viable) | 4.1×107 | 0/3 | No deaths | 7 |
SCID = severe combined immunodeficient; NMIIC4 = Nine Mile phase II clone 4.
Both SCID mice (NOD.CB17-prkdcSCID/Asmu) and immunocompetent wild mice were used in this experiment. The SCID mice were obtained from Monash Animal Services, Melbourne, Australia and the wild mice were purchased locally.
A Tecniplast small Isocage system (2ISO12, Tecniplast, Milan, Italy) was used for holding mice. All works were performed in a PC3 laboratory at the Department of Microbiology, Pathology North-Hunter, NSW Health Pathology, Newcastle, Australia. Animal use was approved by the “Animal Care and Ethics Committee” of the Australian Rickettsial Reference Laboratory (ARRL).
A total of 30 (27 SCID and 3 wild mice) adult female mice were housed in 10 sterile isolator cages. Eight cages containing 24 SCID mice (3 mice/cage) were allocated to determining the effect of different doses of viable avirulent NMIIC4. The cages were labeled according to the NMIIC4 dilution (10−1 to 10−8) and each mouse was inoculated intraperitoneally (i/p) with 0.1 mL of viable bacteria of appropriate dilution and defined number of bacteria (Table 1). Two control groups were used; control group A (three SCID) was a negative control and mice were inoculated i/p with 4.1×107 heat killed bacteria (10−1 dilution) per mouse. Control group B (three wild mice) was inoculated i/p with 4.1×107 viable bacteria (10−1 dilution). After inoculation, all mice were monitored daily. They had a continuous supply of food and water. The experiment continued for 60 days.
The spleens from all mice (experimental and control groups) were collected after death at Day 25 or longer after infection or after euthanasia at Day 60. Aseptic procedures were followed during removal and homogenization of each spleen in 10 mL of Hank's Balanced Salt Solution (HBSS, Gibco, Mulgrave, Australia). By weighing the spleen, splenomegaly was correlated to C. burnetii DNA concentration.
The DNA was extracted from 100 μL of each dilution of the NMIIC4-infected VERO cell culture and from each spleen homogenate of the experimental and control mice. The Qiagen Extraction Kit (Qiagen, Hilden, Germany) was used following the manufacturer's instructions. For quantification of C. burnetii specific DNA, a Com1 qPCR was used.22 The Ct values of positive qPCR samples were used to calculate the approximate copy numbers/genome equivalent in each dilution of inoculum and in each homogenized mice spleen.
The phase type of the reisolated C. burnetii was tested by PCR assays used previously in analysis of the O-antigen biosynthesis regions of phase II C. burnetii isolates.8 Four genes, CBU688 (GDP-fucose synthetase), CBU689 (GDP-mannose 4, 6-dehydratase), CBU694 (glycosyl transferase), and CBU696 (pleiotropic regulatory protein) were tested. Among these CBU688 and CBU689 genes are involved in virenose synthesis. All four genes were present in control NMI and absent in control NMIIC4 C. burnetii (Data not shown).
The Spearman-Kärber method was used to calculate the LD50 of NMIIC4 of C. burnetii in the SCID mice.
Results
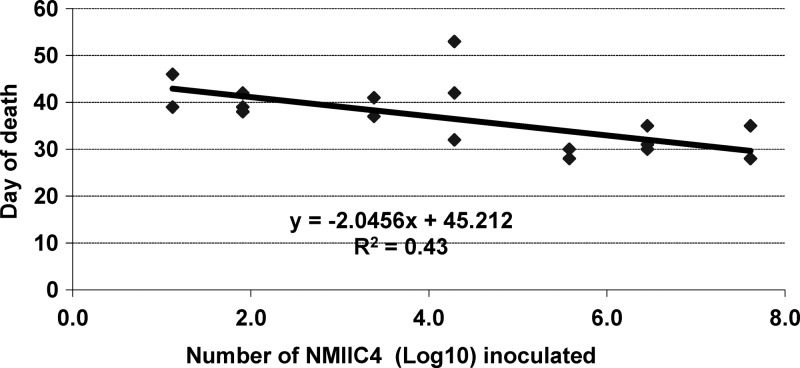
In the experimental group, SCID mice infected with eight different doses of viable NMIIC4 bacteria (from 4.1×107 to < 1) showed varying mortality over time. The first deaths were recorded at Day 28 from the highest doses of NMIIC4 and mortality continued until Day 53 with the lower doses. Out of 24 mice only five mice survived to the termination of the experiment at Day 60 (Table 1). Among these five mice three were inoculated with ∼1 bacterium and the other two received 1.2×101 and 2.4×103 bacteria, respectively. The time interval between early and late deaths was ∼15 days (Figure 1).
Figure 1.
Coxiella burnetii Nine Mile phase II clone 4 (NMIIC4) infecting doses and severe combined immunodeficient (SCID) mice day of death.
No mortality occurred in control groups A and B, i.e., SCID mice inoculated with killed NMIIC4, and wild mice inoculated with viable NMIIC4 (Table 1).
Splenomegaly was evident in all dead infected mice. The average weight of the spleens of infected SCID mice was 0.61 g, which was eight times greater than the spleens of uninfected control SCID mice (0.07 g). The qPCR results of infected SCID mice spleen tissue revealed high C. burnetii loads (3.2–6.8 × 107) per 0.1 mL spleen suspension (Table 1). However, among the five surviving mice only the mouse that received the 2.4 × 103 bacterial inoculum had splenomegaly and a high bacterial load. This mouse was sick and would likely have died within a few days. No splenomegaly was detected in control mice and the qPCR assay revealed only low copies of C. burnetii DNA in spleen tissue (Table 1).
In the C. burnetii isolated from the spleens of the SCID mice, all four phase I LPS genes were absent, indicating that these C. burnetii cells used in phase II (i.e., NMIIC4) confirming that no switch to virulent phase I had occurred in vivo.
Discussion
The NMIIC4 resulted in 79% (19 of 24) mortality in the SCID mice with an LD50 of ∼10 C. burnetii. Hence, it was very virulent for SCID mice. Our previous study with phase I C. burnetii Australian isolates revealed an LD50 of 1 bacterium for SCID mice.23 Had we allowed the experiment to have continued for more than 60 days, we may have approached a similar LD50 for the NMIIC4 strain.
The SCID mouse model, using the NMI strain of C. burnetii has been described for lethal Q fever, indicating that the SCID mouse is highly susceptible to C. burnetii. The immunodeficiency of the SCID mouse host enhances the severity of Q fever.20 Phase II attenuated strains have also been used to infect gene knockout mice,15 SCID, and SCIDbg mice.13 The NMIIC4 caused a febrile response in gamma interferon knockout mice and toll-like receptor 2 knockout mice. In that study the same SCID model and identical NMIIC4 strain were used, but the study was stopped at Day 28 and a fixed dose (104 C. burnetii, i/p) was used for infection. Based on our current study, that dose of bacteria needs more than 28 days duration of infection to show an effect. In that study the highest dose (4×107) also showed no effect in the first 28 days. Such variations in the dose and duration of infection may be because some SCID mice strains are known to be “leaky” and occasionally produce small numbers of T and B cells.19 However, we were not able to determine the “leakiness” of our experimental SCID mice.
Until now the full length LPS I of NMI was the only known virulence factor of C. burnetii.10 The avirulent NMIIC4 contains truncated LPS II and has a large chromosomal deletion that eliminates open reading frames involved in the biosynthesis of terminal O antigen sugars, including the rare sugar virenose. This current study confirms that, despite the absence of the O antigen biosynthesis region, the NMIIC4 shows virulence properties of phase I. An earlier study on another Nine Mile variant (RSA 514 “Crazy”), which has a similar large deletion to the NMIIC4 strain, also showed virulence properties of phase I. Both studies support the speculation that there must be an additional basis to phase I virulence.7,8 We confirmed that the reisolated NMIIC4 from the experimentally infected SCID mice were still in phase II but further investigation on the genomic and phenotypic properties of the NMIIC4 strain may explain the mechanism for expression of its phase I-like virulence. However, it cannot be due solely to phase I LPS.
In conclusion, it can be stated that 1) NMIIC4 was highly virulent for SCID mice (LD50 = 10) and mortality was related to dose; 2) splenomegaly was evident in all dead infected SCID mice, with high loads of NMIIC4; 3) the NMIIC4 had no effect on immunocompetent wild mice. The NMIIC4 bacteria were lethal to SCID mice despite this bacterium not containing phase I LPS. Other (as yet unidentified) virulence factor(s) of C. burnetii are probably involved in the pathogenesis of Q fever and further studies are required to elucidate the full genomic and phenotypic basis of virulence in C. burnetii.
ACKNOWLEDGMENTS
We acknowledge the scientific assistance of Allana Cooper and Yazid Abdad, Department of Microbiology, James Cook University, QLD, and Australian Rickettsial Reference Laboratory, Barwon Health, VIC, Australia.
Footnotes
Financial support: John Ferguson and Rodney Givney, Division of Microbiology, Pathology North-Hunter, John Hunter Hospital, NSW, Australia, are also acknowledged for their valuable funding contributions.
Authors' addresses: Aminul Islam, Department of Microbiology, Pathology North- Hunter, NSW Health Pathology, John Hunter Hospital, HRMC, Australia, E-mail: aminul.islam@hnehealth.nsw.gov.au. Michelle Lockhart and John Stenos, Geelong Hospital, Australian Rickettsial Reference Laboratory, Geelong, Victoria, Australia, E-mails: michelle.g.lockhart@gmail.com and johns@barwonhealth.org.au. Stephen Graves, Geelong Hospital, Australian Rickettsial Reference Laboratory, Geelong, Victoria, Australia, and Hunter Area Pathology Service, Department of Microbiology, Newcastle, New South Wales, Australia, E-mail: Stephen.graves@hnehealth.nsw.gov.au.
References
- 1.Derrick EH. ‘Q’ fever, a new fever entity: clinical features, diagnosis and laboratory investigation. Med J Aust. 1937;11:281–299. doi: 10.1093/clinids/5.4.790. [DOI] [PubMed] [Google Scholar]
- 2.Ftacek P, Skultety L, Toman R. Phase variation of Coxiella burnetii strain Priscilla: influence of this phenomenon on biochemical features of its lipopolysaccharide. J Endotoxin Res. 2000;6:369–376. [PubMed] [Google Scholar]
- 3.Slaba KA, Hussein A, Palkovic P, Horváth V, Toman R. Studies on the immunological role of virenose and dihydrohydroxystreptose present in the Coxiella burnetii phase I lipopolysaccharide. Ann N Y Acad Sci. 2003;990:505–509. doi: 10.1111/j.1749-6632.2003.tb07419.x. [DOI] [PubMed] [Google Scholar]
- 4.Amano KI, Williams JC, Missler SR, Reinhold VN. Structure and biological relationships of Coxiella burnetii lipopolysaccaharides. J Biol Chem. 1987;262:4740–4747. [PubMed] [Google Scholar]
- 5.Hackstadt T, Peacock MG, Hitchcock PJ, Cole RL. Lipopolysaccharide variation in Coxiella burnetii: intrastrain heterogeneity in structure and antigenicity. Infect Immun. 1985;48:359–365. doi: 10.1128/iai.48.2.359-365.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hackstadt T. Antigenic variation in the phase I lipopolysaccharide of Coxiella burnetii isolates. Infect Immun. 1986;52:337–340. doi: 10.1128/iai.52.1.337-340.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoover T, Culp D, Vodkin M, Williams J, Thompson H. Chromosomal DNA deletions explain phenotypic characteristics of two antigenic variants, phase II and RSA 514 (crazy), of the Coxiella burnetii nine mile strain. Infect Immun. 2002;70:6726–6733. doi: 10.1128/IAI.70.12.6726-6733.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denison AM, Massung RF, Thompson HA. Analysis of the O-antigen biosynthesis regions of phase II Isolates of Coxiella burnetii. FEMS Microbiol Lett. 2007;267:102–107. doi: 10.1111/j.1574-6968.2006.00544.x. [DOI] [PubMed] [Google Scholar]
- 9.Vodkin MH, Williams JC. Overlapping deletion in two spontaneous phase variants of Coxiella burnetii. J Gen Microbiol. 1986;132:2587–2594. doi: 10.1099/00221287-132-9-2587. [DOI] [PubMed] [Google Scholar]
- 10.Moos A, Hackstadt T. Comparative virulence of intra- and interstrain lipopolysaccharide variants of Coxiella burnetii in the guinea pig model. Infect Immun. 1987;55:1144–1150. doi: 10.1128/iai.55.5.1144-1150.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waag DM, England MJ, Pittet ML. Comparative efficacy of a Coxiella burnetii chloroform: methanol residue (CMR) vaccine and a licensed cellular vaccine (QVax) in rodents challenged by aerosol. Vaccine. 1997;15:1779–1783. doi: 10.1016/s0264-410x(97)00107-2. [DOI] [PubMed] [Google Scholar]
- 12.Zhang GQ, Samuel JE. Identification and cloning potentially protective antigens of Coxiella burnetii using sera from mice experimentally infected with Nine Mile phase I. Ann N Y Acad Sci. 2003;990:510–520. doi: 10.1111/j.1749-6632.2003.tb07420.x. [DOI] [PubMed] [Google Scholar]
- 13.Andoh M, Russell-Lodrigue KE, Zhang G, Samuel JE. Comparative virulence of phase I and II Coxiella burnetii in immunodeficient mice. Ann N Y Acad Sci. 2005;1063:167–170. doi: 10.1196/annals.1355.026. [DOI] [PubMed] [Google Scholar]
- 14.Andoh M, Zhang G, Russell-Lodrigue KE, Shive HR, Weeks BR, Samuel JE. T cells are essential for bacterial clearance, and gamma interferon, tumor necrosis factor alpha, and B cells are crucial for disease development in Coxiella burnetii infection in mice. Infect Immun. 2007;75:3245–3255. doi: 10.1128/IAI.01767-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochoa-Repáraz J, Sentissi J, Trunkle T, Riccardi C, Pascual DW. Attenuated Coxiella burnetii phase II causes a febrile response in gamma interferon knockout and Toll-like receptor 2 knockout mice and protects against reinfection. Infect Immun. 2007;75:5845–5858. doi: 10.1128/IAI.00901-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller JD, Curns AT, Thompson HA. A growth study of Coxiella burnetii Nine Mile phase I and phase II in fibroblasts. FEMS Immunol Med Microbiol. 2004;42:291–297. doi: 10.1016/j.femsim.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Bosma GC, Custer RP, Bosma MJ. A severe combined immunodeficiency mutation in the mouse. Nature. 1983;301:527–530. doi: 10.1038/301527a0. [DOI] [PubMed] [Google Scholar]
- 18.Dorshkind K, Keller GM, Phillips RA, Miller RG, Bosma GC, O’Toole M, Bosma MJ. Functional status of cells from lymphoid and myeloid tissues in mice with severe combined immunodeficiency disease. J Immunol. 1984;132:1804–1808. [PubMed] [Google Scholar]
- 19.Bosma GC, Fried M, Custer RP, Carroll A, Gibson DM, Bosma MJ. Evidence of functional lymphocytes in some (Leaky) SCID mice. J Exp Med. 1988;167:1016–1033. doi: 10.1084/jem.167.3.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andoh M, Naganawa T, Hotta A, Yamaguchi T, Fukushi H, Masegi T, Hirai K. SCID mouse model for lethal Q fever. Infect Immun. 2003;71:4717–4723. doi: 10.1128/IAI.71.8.4717-4723.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russell-Lodrigue KE, Andoh M, Poels MW, Shive HR, Weeks BR, Zhang GQ, Tersteeg C, Masegi T, Hotta A, Yamaguchi T, Fukushi H, Hirai K, McMurray DN, Samuel JE. Coxiella burnetii isolates cause genogroup-specific virulence in mouse and guinea pig models of acute Q fever. Infect Immun. 2009;77:5640–5650. doi: 10.1128/IAI.00851-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lockhart M, Graves S, Banazis M, Fenwick S, Stenos J. A comparison of methods for extracting DNA from Coxiella burnetii as measured by a duplex qPCR assay. Lett Appl Microbiol. 2011;52:514–520. doi: 10.1111/j.1472-765X.2011.03034.x. [DOI] [PubMed] [Google Scholar]
- 23.Lockhart MG, Islam A, Graves GR, Fenwick S, Stenos J. Detecting and Measuring Small Numbers of viable Coxiella burnetii. FEMS Immunol Med Microbiol. 2012;64:61–65. doi: 10.1111/j.1574-695X.2011.00898.x. [DOI] [PubMed] [Google Scholar]