Abstract
There is major untapped potential to improve health in low-income communities through improved housing design, fittings, materials and construction. Adverse effects on health from inadequate housing can occur through a range of mechanisms, both direct and indirect, including as a result of extreme weather, household air pollution, injuries or burns, the ingress of disease vectors and lack of clean water and sanitation. Collaborative action between public health professionals and those involved in developing formal and informal housing could advance both health and development by addressing risk factors for a range of adverse health outcomes. Potential trade-offs between design features which may reduce the risk of some adverse outcomes whilst increasing the risk of others must be explicitly considered.
Keywords: Housing, Household energy, Sanitation, Development, Health
Introduction
Housing has historically been recognized as potentially important both for improving public health1 and advancing development, but the public health and housing communities rarely work together to ensure that the design and construction of housing capitalize on that potential. As a consequence, opportunities to address these agendas simultaneously are often lost.
The home is more than a simple shelter; it forms the foundation for household and community life. It is a place for rest and relaxation, for socializing, for everyday functions. A house needs to protect against the elements (including extreme weather); to have sound structure; to be free of hazards, including pests and disease vectors; to provide adequate facilities for sleeping, personal hygiene, the preparation and storage of food; to provide an environment for comfortable relaxation; and to offer facilities for communication and social exchange with friends, family and others.
However, the adequacy of housing is seldom assessed using such a broad definition. Even in high-income settings, decent housing is typically judged with reference to a set of minimum standards for specified hazards. For example, the UK Home Health and Safety Rating System provides a system for assessing a range of more than 20 specific health risks in the home.2 In low-income settings, many of the same hazards apply, but their nature and relative magnitudes vary. Nearly half of the world’s population survive on less than $2 per day.3 There are dramatic differences between rich and poor in energy use, wealth and health. Radically new solutions are needed rapidly to raise billions out of poverty and improve their health. This means that opportunities to exploit socioeconomic, health and environmental goals simultaneously and synergistically must be grasped.
Housing is a key development priority. Although the proportion of urban residents living in slums declined from 39 to 33 % between 2000 and 2010, the absolute numbers are increasing in part because of the rapid pace of urbanization.4 The population living in slums stands at 828 million and is set to increase further. It is anticipated that by 2030, 56 % of the developing world’s population will be living in an urban environment. Between 2010 and 2030, the urban population of Africa is likely to increase by 85 % and that of Asia by 46 %. In total, the urban population of Africa and Asia is anticipated to grow by 1.2 billion.
Housing solutions need to be affordable and acceptable to the poorest half of the world’s population. This has led to calls for a $1,000 house5 based on principles of affordability, comfort and sustainability.
This paper makes the case that housing should be both a health and development priority, and that health considerations should form a key part of any strategies to design and build/modify houses for and with disadvantaged populations. It suggests which features of housing design and services are particularly likely to improve health whilst satisfying these principles. The design features that can reduce disease and injury risk should be implemented in an integrated fashion as determined by the prevailing epidemiological patterns of disease in the community. The public health community should capitalize more fully on the opportunities to advance health through closer working with those involved in designing and constructing formal and informal housing. By working together to achieve both health and development goals, better use can be made of limited resources, and substantial burdens of disease can be averted.
Mechanisms by which Housing Affects Health
Housing can affect health in many ways, both direct and indirect, through a range of mechanisms. In some cases, there are trade-offs between design features which may reduce the risk of some adverse outcomes whilst increasing the risk of others. There are also constraints on the use of some approaches including cost and availability of materials or energy supply. Some of these issues are summarized in Table 1.
Table 1.
Framework for assessing the impact of housing features on health in low-income settings
| Housing features | Health outcomes that may be affected | Mechanisms of effects | Potential trade-offs and constraints |
|---|---|---|---|
| Lack of screened housing, ceilings and open eaves (elevated housing may also be protective) | Malaria and other VBDs, fly-borne diseases, e.g. trachoma and diarrheal diseases | Prevention of house entry by insect vectors | Reduced ventilation, increased thermal stress and indoor air pollution |
| Lack of efficient, low-emission cook stoves or clean fuels (e.g. LPG/biogas, etc.) | Acute respiratory infections in children, chronic obstructive pulmonary disease, IHD, burns/scalds, etc. | Exposure to products of incomplete combustion leading to high levels of particulates, CO, PAHs, etc.; accidents with fires | Barriers include costs (low-emission stoves, LPG) and intermittent supply of LPG |
| Lack of safe and clean (electric) lighting | Burns and household air pollution from kerosene and other lamps | Indirect effects through inability to study, lack of physical security | No or unreliable electricity supply |
| Lack of ventilation, increased albedo | Heat-related mortality and morbidity (converse in high altitude sites) | Thermal stress/cold exposure at high altitudes | See above |
| Fragile or inappropriate structure for location | At risk from extreme weather. Also, injuries, sexual violence, mental health, vector-borne diseases | Robbery, physical attack, susceptibility to landslide, flood, storm, etc. Elevated housing may also protect against some VBDs | Cost may be prohibitive, ventilation may be reduced by smaller and more secure windows, etc. |
| Lack of clean water supply, washing facilities, toilet | Diarrheal disease, trachoma, intestinal parasites, respiratory infections, etc. Improving provision of water, sanitation and hygiene can improve nutritional status by reducing malnutrition due to Diarrhea and intestinal parasites | Ingestion of pathogens; poor hygiene | Poorly maintained latrines or inadequate drainage may provide opportunities for mosquito breeding |
Protection against Heat and Cold
The first function of housing is protection against the elements, including low and high temperatures. For many low-income settings, the primary concern is protection against heat.
There is an extensive body of literature about the hazards associated with both low1,6–8 and high outdoor temperatures9,10 but surprisingly little evidence on the degree to which housing protects against such risks. Problems of indoor cold and fuel poverty8 have been the focus of public health concern in Europe11, New Zealand12 and other temperate climates, but to date of very little focus in low-income settings, even though cold is a problem of many low-income populations especially at high altitudes or high latitudes.
The studies that have attempted to quantify the variation in risks of heat-related mortality in relation to dwelling type are from high-income settings.13 Living in upper floors of older buildings confers a higher risk of heat-related death, although it may be possible to mitigate this risk by appropriate ventilation and insulation. However, even for these settings there is no quantitative evidence about health risk in relation to indoor temperature, merely an indication of more hazardous dwelling forms. In low-income settings, there is no direct evidence of this kind.
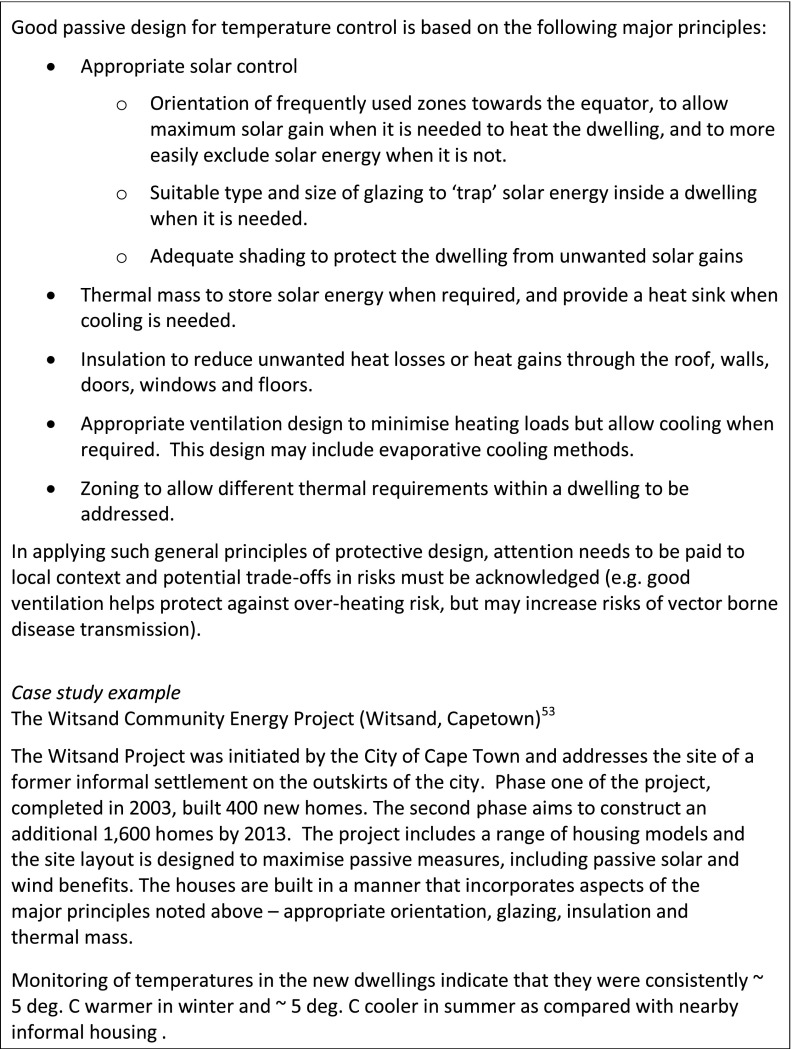
With regard to thermal ‘comfort’, it has long been known14 that occupants’ thermal responses adapt to changing ambient conditions. This makes the use of a ‘passive design’ approach more feasible which involves minimizing the energy needed to heat or cool the building whilst permitting adequate ventilation to prevent build up of indoor pollutants as outlined in Box 1.
Box 1. Protective housing design features for temperature control
Household Energy and Household Air Pollution
Energy in the home is critical for basic needs—cooking, warmth, lighting—yet well into the twenty-first century some 3 billion still rely on solid fuels (wood, dung, crop wastes, charcoal and coal) burned in open fires or traditional stoves that are highly inefficient and emit high levels of air pollution into and around the home.15 Many of these same homes, for around 1.3 billion people, have no electricity (and more have inadequate/intermittent power), and use candles or simple kerosene lamps for lighting which also cause significant pollution in the home.16 These cooking and lighting technologies also pose a high risk for burns, scalds and fires, and child poisoning from unsafe storage of liquid fuel, mainly kerosene.17 The collection of solid fuels can take as much as several hours per day17, may take children away from school and in insecure settings places women at risk of gender-based violence.
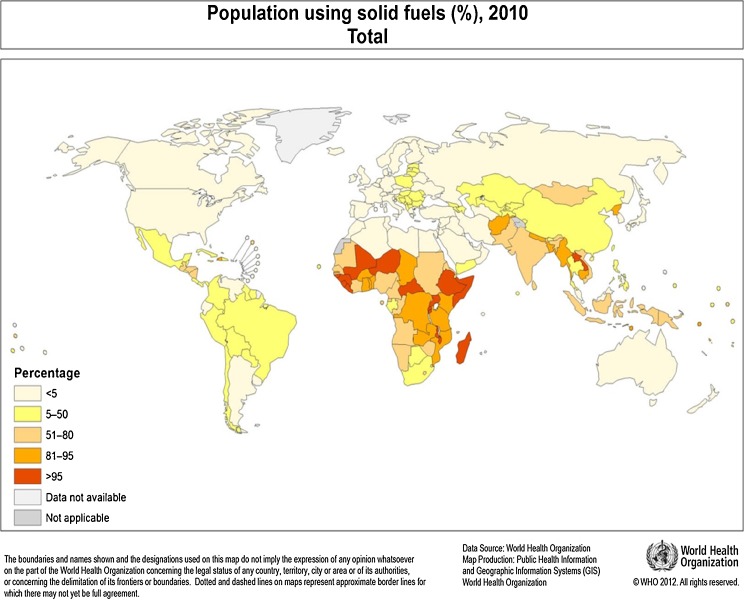
Globally, solid fuel use (SFU) is highest in developing countries (Figure 1), and is closely related to poverty16 and other associated household environmental health risks.18 SFU is greatest in rural areas, reaching 95 % or more in many sub-Saharan African countries, but is also common in urban areas with up to 70 % SFU in cities of the least developed countries.
FIGURE 1.
Percent of population using solids fuels.
The main health consequences of these patterns of energy use in developing countries arise from household air pollution (HAP), caused by the inefficient combustion of solid fuels, and also from use of kerosene. Levels of HAP in the home are high, with typical average fine particle (PM2.5) levels in the range 200–500 μg m−3, at least 20 times the WHO annual guideline level (10 μg m−3). Even when cooking takes place outdoors, exposures of women and children can be considerable. A substantial and growing body of evidence now links these exposures to a wide range of important respiratory and other health outcomes. The estimated risks obtained from published systematic reviews are summarized in Table 2 and other risks in the Appendix 1.
Table 2.
Risks of different health outcomes from exposure to solid fuel use
| Outcome | Age group | Females | Males | ||
|---|---|---|---|---|---|
| Odds ratio | 95 % CI | Odds ratio | 95 % CI | ||
| Acute lower respiratory infection78 | 0–59 months | 1.78 | 1.45, 2.18 | As for females | |
| Chronic obstructive pulmonary disease18 79 80 | Adult >15 | 2.70 | 1.95, 3.75 | 1.90 | 1.15, 3.13 |
| Lung cancer (coal use) | Adult >15 | 1.98 | 1.16, 3.36 | 1.31 | 1.05, 1.76 |
| Low birth weight81 | N/A | 1.52 | 1.28, 1.80 | As for females | |
| Mean reduction in birth weight = 93.1 g | 64.6, 121.6 | ||||
| Stillbirth81 | N/A | 1.51 | 1.23, 1.85 | As for females | |
No studies are available from developing countries on CVD end points, although effects on ‘intermediate’ stage and risk factors such as blood pressure have been reported.78,81 Based on the exposure response relationship published by Pope et al.82 on multiple source combustion pollution and CVD risk, interpolated risks consistent with the reduction in exposure to HAP of 200 μg m−3PM2.5 of 1.20 for women and 1.073 for men, respectively, have been proposed27
Pests and Disease Vectors
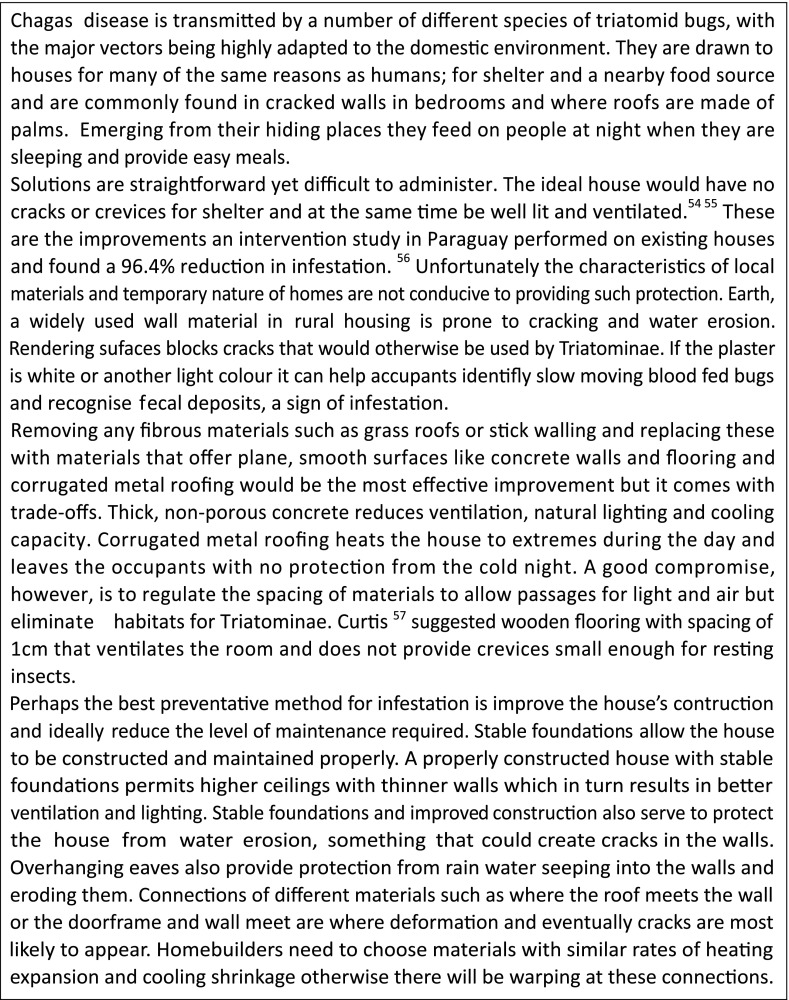
Many vector-borne diseases are transmitted indoors. Understanding how arthropods exploit our homes can provide simple ways of reducing the incidence of major vector-borne diseases like malaria19, lymphatic filariasis, Chagas disease and dengue.
In Africa, the major vector of malaria, Anopheles gambiae, has adapted to feeding indoors, where over 80 % of transmission typically occurs. In other parts of the tropics, there tends to be a greater proportion of outdoor biting, but transmission indoors is still important, as illustrated by the successful control of malaria using long-lasting nets or indoor residual spraying. Since the home is where a large proportion of transmission occurs, changing the local architecture of houses can markedly reduce malaria transmission.19
In Africa, A. gambiae enters houses through open eaves (Figure 2), whilst culicine mosquitoes, vectors of urban lymphatic filariasis and some arboviruses, enter through the doors.20 Blocking the eaves or installing ceilings to prevent mosquitoes entering the living area are simple ways to reduce transmission.21 In a recent large-scale randomized controlled trial, house screening with untreated fly-screen mesh, installed as ceilings or as full screening on the doors and windows, reduced anaemia due to malaria in young Gambian children by around 50 %.22 Since anaemia due to malaria is a major killer of young children, house screening has the potential to substantially reduce malaria deaths in this age group. In urban Africa, malaria transmission is about 95 % lower than in rural areas23, with few vectors entering houses. Whilst there are many reasons for this, one likely explanation is that in urban situations houses are often well built having fewer entry points thus reducing the entry of mosquitoes, and thieves.
FIGURE 2.
Entry of A. gambiae through open eaves.
Raising homes above the ground on stilts may also be protective against mosquito house entry since many host-seeking mosquitoes fly less than 1 m above the ground24–26 In São Tomé, wooden houses built on stilts had half the number of A. gambiae compared with houses that were built at ground level.27 Whilst the disappearance of malaria in Europe and North America was related to a combination of factors28, it was partly due to improved housing. Screened homes helped reduce malaria in the southern USA, whilst housing people away from their animals, and building homes that were well lit, warm and airy reduced the numbers of mosquitoes resting in European houses. The decline in malaria seen in many countries over the past decade is partly a result of development and the improvement in people’s homes. The thatched-roofed housing once typical of rural Africa is far less common today than in the past. Modern metal-roofed houses with concrete walls and well-fitted windows and doors are likely to lead to fewer mosquitoes entering and resting indoors than in traditional houses. Housing features that may protect against spread of Chagas disease are described in Box 2.
Box 2. Housing measures to protect against Chagas disease
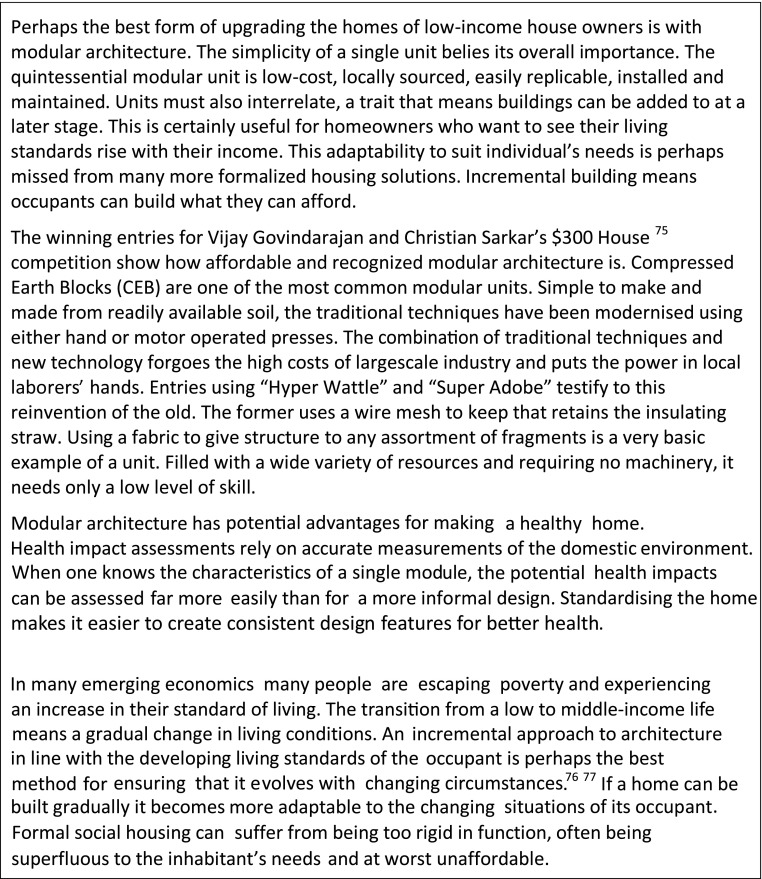
Crowding and Space
Overcrowding is not an issue of building design, but of building use: it is determined more by the lack of (economic) opportunity of the occupants than by any aspect of design or construction. There is no clear evidence-based definition of overcrowding, as the evidence of adverse health effects is consistent with a continuum of risk with increasing levels of crowding. There are also some advantages to high levels of occupancy—security, extended family social support—but these are generally outweighed by the hazards which are outlined in Box 3. In view of the lack of evidence regarding optimum levels of occupancy, rigid guidelines about space do not seem appropriate until the evidence is obtained to make this possible. However, the observation that subjective assessments of crowding and lack of privacy may increase the risk of ill health suggests housing designs should be flexible enough to cope with changes in family size for example by using modular approaches which allow extra rooms to be added when these are needed and can be afforded (see Box 4).
Box 3. Crowding and health
Box 4. Incremental and modular architecture
Damp and Mold
Damp and mold growth in the home have been consistently linked to a number of health outcomes, including nausea and vomiting and general ill health as well as respiratory illness (see also Appendix 2).29–31 Housing that is damp and prone to condensation tends to result from inadequate ventilation or insulation and to be associated with poor maintenance of the dwelling and with the socioeconomic deprivation of the householder. However, there is a dearth of evidence about the effects of damp and mold in low-income countries.
Water and Sanitation
Considerable reductions in diarrheal disease are associated with water supply and sanitation32 (Figure 3). Yet, 783 million people still lack improved provision of drinking water, and 2.5 billion lack sanitation.33,4 Considerable health benefits can be attributed to improved water supplies and sanitation: significant reductions in the risk of diarrheal disease are associated with water supply [relative risk, 0.75; 951 % confidence interval (CI), 0.62–0.91] and sanitation (relative risk, 0.68; 95 % CI, 0.53–0.87; Figure 3).32
FIGURE 3.
Results of reviews of the effect on diarrhea of water, sanitation and hygiene interventions. Results of the previous reviews are for the better quality studies. The reduction for household drinking water connections is in addition to reductions for water quality and availability of public sources. Source: Bartram & Cairncross 2010.84
However, unlike sanitation coverage, which is assessed at home, a water source is considered accessible when it is hundreds of metres from the place of use4 In practice, water usage is constrained by the time taken (mainly by women) collecting water or the high costs paid to vendors. Household water connections greatly increase domestic water consumption, and much of this additional water is used for hygiene:34 water scarcity and lack of hygiene promote endemic diarrhea, trachoma and other water and excreta-related diseases which disproportionately burden the poorest of the poor.35
Rainwater harvesting provides an alternative. A recent review suggests that rainwater consumption reduces the risk of diarrhea when compared with unimproved water supplies.36 However, rainwater from thatched roofs is not potable; it brings the risk of leptospirosis from rat urine. Where the dry season lasts several months, rainwater use requires a large storage tank, which makes rainwater collection relatively expensive, and largely confining it to the monsoon belt of Southeast Asia, and small islands.37
Trials of treating water at the point-of-use (household-level chlorination, filtration or solar disinfection) have found large reductions in diarrhea38, but this effect is not seen in blinded trials, undermining the evidence for effectiveness.39 Endemic diarrhea is more frequently water-washed (spread person-to-person through lack of hygiene) than water-borne (in drinking water). Furthermore, the effectiveness of water quality interventions depends on a possibly unrealistic level of compliance40; greater health benefits are likely from investing in water supply infrastructure. For example, as well as reducing diarrhea, uninterrupted piped water removes the need for water storage containers, common breeding sites for Aedes aegypti mosquitoes which transmit dengue viruses in urban and peri-urban areas.41
Sanitation technology can include cheaper non-sewered options such as upgraded pit latrines in which flies and odours are controlled by ventilation, or pour-flush toilets flushed by hand using a few litres of water. These require a pit emptying service when used in urban settings. Preventing direct access to fecal waste is needed to avoid creation of mosquito and fly breeding sites in latrines—primarily Culex vectors of filariasis, and in sub-Saharan Africa, the latrine fly, Chrysomya putoria, a putative vector of diarrheal disease
The benefits of sanitation accrue to the individual household, and also to the community: for example, when transmission of diarrhea and intestinal worms has been removed from the public domain, household-related risk factors for infection emerge, such as the frequency of water supply interruption, poor sullage disposal and absence of a washstand; these indicate the need for environmental interventions to address disease transmission in the home as well as the community.42,43 For example, design features of a house, such as locating a washstand within easy reach of a latrine, may enable handwashing with soap44 which can reduce diarrheal disease by up to 47 %.45
Water supply and sanitation, like the best housing, comes at a cost: in the 1920s in the UK, relocation of inhabitants from an overcrowded slum to a purpose-built modern dwelling resulted in an increase in the death rate, predominantly from infectious diseases. The high rental costs of these new properties left less money available for food, resulting in nutritional deficiencies and increased disease susceptibility.46 Household water purchase or connections to main water or sewers often cost the poor more than the wealthy and could have a similar effect.35
Cost-Effectiveness and Cost Benefits
Cost-effectiveness and cost–benefit analyses (CBA) of improved efficiency cookstoves have been reported for a range of scenarios15,16,47 and in case studies. Results, especially for CBA, are favourable, although the valuation of health benefits in CBAs has shown these to make a relatively small contribution to the overall benefit to cost ratio. The mid-range costs of improved wood-burning and charcoal-burning stoves are $15 and $14, respectively, compared with $90 for propane (LPG) and $300 for electric stoves, putting the latter two options out of the reach of many poor families without subsidies or low cost loans.47 Time efficiency and opportunity costs of time are critical factors that determine whether improved cooking technologies result in increased private returns compared with traditional cooking stoves. Although health benefits are valued by families, they may not be as important as the daily costs of fuel purchase and time spent cooking.47
The cost of full house screening is around $10 per person (assuming four people per house) and would be similar to insecticide-treated bednets or indoor residual spraying if it remained effective for 3–4 years.22 In the case of water and sanitation technologies, costs are relatively low (Table 3) but still beyond the reach of the poorest. An important question for future analysis is the potential of greater economic efficiency for integrated interventions and delivery. It is also important to evaluate the cost-effectiveness of strategies to improve access to health-enhancing housing features for the poorest including microfinance and conditional cash transfers. Subsidies of improved cooking stoves and fuel through carbon funds may be justified on the basis of greenhouse pollutant reductions but will depend on assumptions about emissions of greenhouse pollutants including black carbon47, and better data are needed for a range of technologies and locations.
Table 3.
Costs and cost-effectiveness of water supply and sanitation technologies (US dollars) (adapted from83)
| Intervention | Construction cost (US$ per capita) | Amortization lifetime (years) | Amortized annual cost (US$ per capita) | Operation and maintenance cost (US$ per capita) | Cost-effectiveness |
|---|---|---|---|---|---|
| Water supply | |||||
| House connections | 150.00 | 20 | 7.50 | 10.00 | 94.00 |
| Hand pump or standpost | 40.00 | 20 | 1.00 | 1.00 | 223.00 |
| Water regulation and advocacy | US$0.02 to US$0.10 per capita per year | 47.00 | |||
| Sanitation | ≤60.00 | 5 | ≤12.00 | n.a. | ≤270.00 |
| Sanitation promotion | 2.50 | 5 | 0.50 | n.a. | |
| Hygiene promotion | 1.00 | 5 | 0.20 | n.a. | 11.15 |
Addressing Trade-offs
It is largely accepted that our environment affects our health. Designing a dwelling can be thought of as designing a habitable internal environment which is conductive to good health.48 However the independent effect of housing on health after taking into account confounding factors such as poverty is not fully established and requires further rigorous research.49,50 When trying to implement healthy housing policy, the most feasible solution is to relate the two fields through the environment. For example, health experts are able to predict what constitutes a healthy environment, while housing experts have the ability to recreate the ideal conditions.
Creating these ideal healthy domestic conditions is about achieving equilibrium rather than simply stacking ‘positive’ healthy design features. Almost all design strategies interrelate and sometimes will unintentionally conflict. For example, screening openings may reduce the ingress of disease vectors, but they also increase the internal temperature and reduce airflow through the house. Any newly implemented strategy must therefore be considered for its unforeseen repercussions, negative or otherwise, on the entire internal environment.
These health trade-offs are perhaps the trickiest problem to deal with when creating a healthy house. Perhaps the best answer is to first categorize which design strategies reduce which health hazards and then to prioritize those design strategies that reduce the most serious health hazards to the local population. The negative impact of house screening on ventilation may be worthwhile overall if it reduces a serious threat of malaria transmission in an endemic area.
Different contexts call for different responses to health needs and different design strategies. Table 4 relates design strategies and health effects through environmental effects. It also shows how certain strategies are dependent on the regional climate and environment.
Table 4.
A framework for assessing healthy design strategies
Targeting Low-Income Groups
Targeting the poor is likely to yield the greatest benefits. So for example a program to provide clean water and sanitation together with clean household fuels and nutritional interventions to children younger than 5 in three regions (Latin America and the Caribbean, sub-Saharan Africa and South Asia) at 50 % coverage would yield 30–75 % greater heath benefits if targeted first at poor households than if the same program of interventions was targeted towards the wealthier households.18
Incorporating Socioeconomic Issues
In most city contexts, to address health concerns in housing, there is a need to incorporate many non-health issues. Often the most important is access to income-earning opportunities. Individuals or households with very limited incomes choose to live in very poor conditions (dormitories with hot beds which people rent for a few hours, on the pavement, whole households in a small room) because these allow them easy access to where they can earn incomes—often walking so there are no transport costs either. There is also the trade-off between housing quality and cost. Many low-income urban dwellers spend a significant proportion of their income on renting accommodation—and put up with poor quality overcrowded accommodation because it is cheaper and leaves more income for food purchase or other needs.51
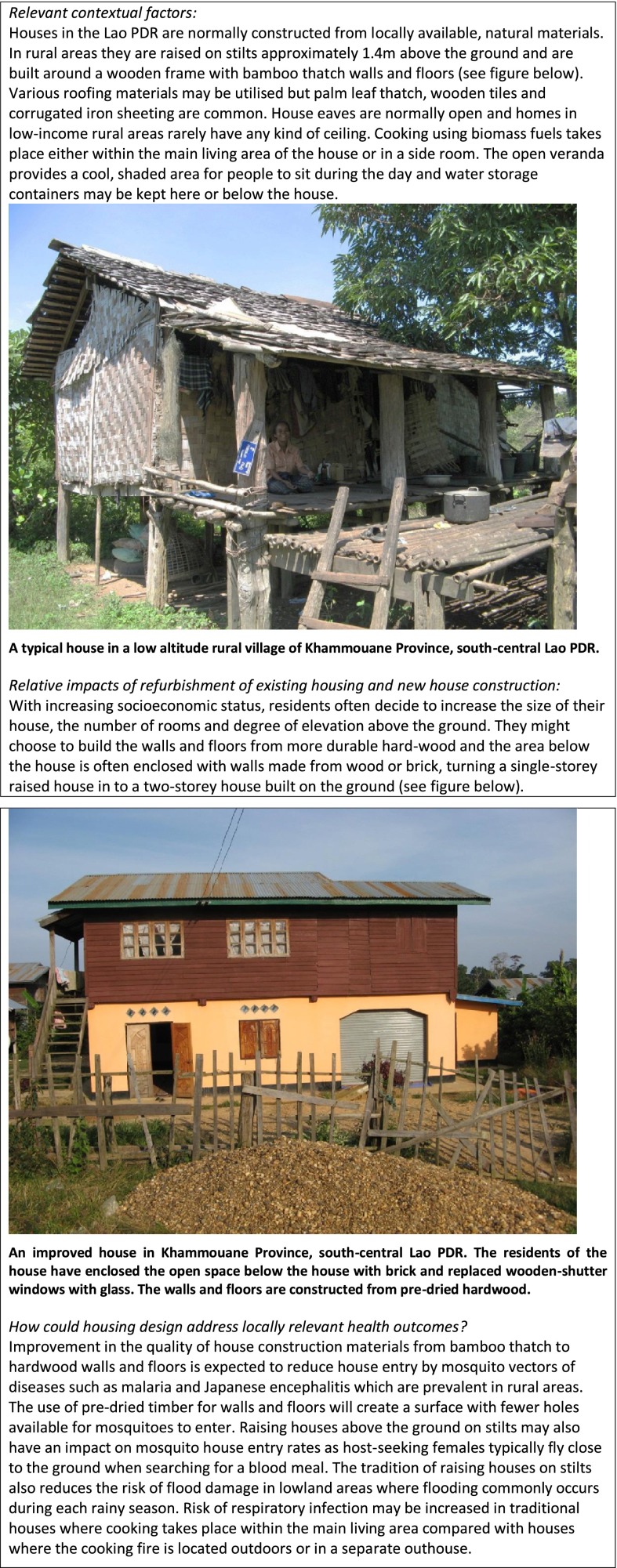
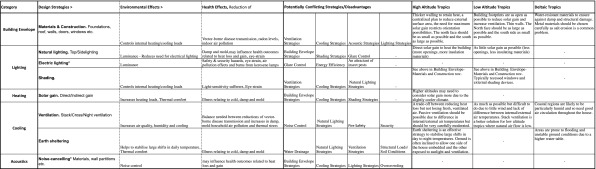
Perhaps the most successful initiatives to integrate health principles into housing improvements have been support for ‘slum’/squatter upgrading, especially where this includes good quality infrastructure provision (piped water to each home, toilets connected to sewers or septic tanks) and good quality health care and emergency services. Box 5 shows features of traditional and improved homes in Laos PDR.
Box 5. Housing case study: low altitude rural Lao PDR
Successful initiatives can also include loans to support households to improve and extend their homes. Importantly, they usually include transferring legal tenure of the homes to the occupants who may take better care of their homes than landlords. In many middle-income nations, support for in situ upgrading of informal settlements has become standard practice for municipal authorities and is no longer controversial (as it still is in much of Africa and Asia). Some of the most effective in situ upgrading has been where government agencies supported grassroots organizations within the settlements scheduled for upgrading to design and organize the work—and negotiate with the landowner for the purchase of tenure or long leases.52 Such initiatives could be combined to greater effect.
Conclusions
The rapidly increasing number of houses built in developing countries both in rural and urban areas offer real opportunities for improving health by incorporating easily installed, affordable features such as screens on doors, windows and ceilings and considering the most appropriate and affordable ways to provide water and sanitation . Encouraging development professionals, local government officials, public health experts, entomologists, architects, planners, constructors, NGOs and local communities to work together to design and construct homes that protect health is likely to reap rich rewards. Including public health considerations into training courses for these stakeholders could promote the integration of health-protecting design features into housing developments and refurbishment programmes.
Acknowledgments
We thank Richard Smith of the London School of Hygiene and Tropical Medicine for his helpful comments.
Appendix 1. Commentary on evidence relating to further health outcomes possibly associated with exposure to emissions from indoor solid fuel use
Evidence is also emerging for a number of other outcomes, which were not included in Table 1 as current evidence is limited and/or systematic reviews are not available. We are aware of one study to date of HAP exposure and CVD as an endpoint which reported an odds ratio of 2.58 (1.53, 4.32)85, but several studies of ‘intermediate’ stages and risk factors such as blood pressure have been reported. The analysis of the relationship between PM2.5 from combustion sources (outdoor pollution, second-hand smoke and active smoking) by Pope et al.82 suggests that HAP exposure (with the dose lying between second-hand and active smoking) would be associated with CVD risk.86 Based on this assumption, risks consistent with the reduction in exposure to HAP of 200 μg m−3PM2.5 of 1.204 women and 1.0734 men, respectively, have been proposed.
A small but quite consistent set of studies report an increase risk of cataract.87,88 Reviews have found inconsistent results for TB, however.89–91 There is also evidence of links with other cancers, including of the upper aero-digestive tract92,93 and carcinoma of the uterine cervix. All of these links, if confirmed, are consistent with the effects of tobacco smoke.
Kerosene is used for cooking and/or lighting fuel by some 500 million homes and has often been grouped with ‘clean’ fuels, but there are concerns about emissions as well as safety. One recent study reported a very elevated risk of TB associated with kerosene use for lighting and cooking94, and this fuel is well recognized as serious risk for burns, fires and child poisoning.95 Population data on burns and scalds are lacking. A high proportion of the 200,000 annual global burn deaths occur in developing countries, mostly in the home and associated with both liquid and solid fuel use. For every death, there are many more severe injuries, which are often inadequately treated, with severe lifelong consequences for disability and stigma. Electric lighting, whether powered through external connection or in-home solar photovoltaic units, will not only avoid the risk of burns and poisoning but also has zero emissions at the point of use (home).
Intervention studies are beginning to provide evidence that reducing exposure impacts positively on a number of these conditions. The RESPIRE trial has shown a one third reduction in severe pneumonia with use of a chimney stove that halved child exposure (OR = 0·67 (0·45–0·98) p = 0.042)96, while three cohort studies of the impacts of the Chinese national improved stove programme have shown substantial reductions of 25–50 % in lung cancer, COPD97 and adult pneumonia mortality for long-term improved stove users in coal-burning areas.
Although significant challenges in achieving large scale, exclusive use of much cleaner stoves and fuels remain, renewed efforts coordinated by the UN Foundation Alliance for clean cookstoves98 are underway to address the critical technological, financing and market development issues involved. Delivery of cleaner, safer and more efficient household energy solutions as part of an integrated health home package including water and sanitation may offer synergistic benefits in terms of health and programmatic efficiency99, but robust empirical evidence is not yet available.
Questions have been raised about whether a reduction in smoke in the home may increase the risk of vector-borne disease. A systematic review found that, while biting may increase, disease transmission was not affected.100
Appendix 2. Humidity, condensation and mold
Humidity in the dwelling can cause condensation which encourages the growth of fungal spores. Damp is also associated with an increase in house dust mites. Both of these are known allergens. This suggests a causal link between respiratory disease, in particular asthma, and damp and mold.29 In addition, there is an observed dose–response relationship noted with this finding: asthma severity increasing with increasing levels of damp and mold in the home. House dust mites require warmth and humidity to thrive, ideally between 23 and 25 °C with 80–90 % humidity. Keeping a dwelling between 40 and 60 % humidity and improving ventilation decrease the number of mites.
Mold growth occurs when the ventilation is poor and the humidity levels are high. Intervention studies have shown that increasing ventilation and reducing humidity can decrease mold.
Studies use different methods of characterising mold—experts or self-reporting and many do not include confounding factors such as smoking or house type. Even so, there is still a consistent and significant relationship found between respiratory symptoms and damp and mold in dwellings. Whether this is an exacerbation of existing disease or the initiation of new disease is as yet unclear. Reduction of exposure to house dust mites also requires user behaviour for adequate airing of bedding, washing and the fitting of pillow and mattress covers which is unlikely to be practical in low-income settings. Structural factors such as consistent heating and good ventilation do play a role in keeping the exposure down, and further research is needed to better understand the health implications in low-income settings.
References
- 1.Braubach M, et al. Environmental burden of disease associated with inadequate housing. Methods for quantifying health impacts of selected housing risks in the WHO European Region. Summary report. Bonn: World Health Organization; 2010. [Google Scholar]
- 2.Ormandy D, et al. Statistical evidence to support the housing health & safety rating system. Vol. 1— project report. London: Office of the Deputy Prime Minister; 2003. [Google Scholar]
- 3.United Nations. Resource for speakers. Vital statistics. Food. 24 May 2012 [cited 2012]; Available from: http://www.un.org/en/globalissues/briefingpapers/food/vitalstats.shtml
- 4.United Nations. Millennium Development Goals 2015. We can end poverty.http://www.un.org/millenniumgoals/environ.shtml Accessed 6 March 2012. [cited 6 March 2012]; Available from: http://www.un.org/millenniumgoals/environ.shtml
- 5.Massachusetts Institute of Technology MIT 1k house. Available from: http://web.mit.edu/cre/research/1k-house-project.html Accessed 11 February 2012
- 6.Mercer JB. Cold—an underrated risk factor for health. Environ Res. 2003;92(1):8–13. doi: 10.1016/S0013-9351(02)00009-9. [DOI] [PubMed] [Google Scholar]
- 7.Analitis A, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168(12):1397–1408. doi: 10.1093/aje/kwn266. [DOI] [PubMed] [Google Scholar]
- 8.Hills J. Fuel poverty: the problem and its measurement. CASE report 69. London: LSE for the Department of Energy and Climate Change; 2011. [Google Scholar]
- 9.McMichael AJ, et al. International study of temperature, heat and urban mortality: the ‘ISOTHURM’ project. Int J Epidemiol. 2008;37(5):1121–1131. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- 10.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 11.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Commun Health. 2003;57(10):784–789. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Butler S, et al. Problems with damp and cold housing among Pacific families in New Zealand. N Z Med J. 2003;116(1177):U494. [PubMed] [Google Scholar]
- 13.Vandentorren S, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16(6):583–591. doi: 10.1093/eurpub/ckl063. [DOI] [PubMed] [Google Scholar]
- 14.Humphreys MA. Outdoor temperatures and comfort indoors. Build Res Pract. 1978;6(2):92–105. [Google Scholar]
- 15.Mehta S, Shahpar C. The health benefits of interventions to reduce indoor air pollution from solid fuel use: a cost-effectiveness analysis. Energy Sustain Dev. 2004;8:53–59. doi: 10.1016/S0973-0826(08)60466-4. [DOI] [Google Scholar]
- 16.Hutton G, et al. Evaluation of the costs and benefits of household energy and health interventions at global and regional levels. Geneva: World Health Organisation; 2006. [Google Scholar]
- 17.Bruce N, et al. et al. In: Indoor air, in disease control priorities in developing countries. 2. Jamison DT, et al.et al., editors. New York: Oxford University Press and World Bank; 2006. [Google Scholar]
- 18.Gakidou E, et al. Improving child survival through environmental and nutritional interventions: the importance of targeting interventions toward the poor. JAMA. 2007;298(16):1876–1887. doi: 10.1001/jama.298.16.1876. [DOI] [PubMed] [Google Scholar]
- 19.Lindsay SW, Emerson PM, Charlwood JD. Reducing malaria by mosquito-proofing houses. Trends Parasitol. 2002;18(11):510–514. doi: 10.1016/S1471-4922(02)02382-6. [DOI] [PubMed] [Google Scholar]
- 20.Njie M, et al. Importance of eaves to house entry by anopheline, but not culicine, mosquitoes. J Med Entomol. 2009;46(3):505–510. doi: 10.1603/033.046.0314. [DOI] [PubMed] [Google Scholar]
- 21.Atieli H, et al. House design modifications reduce indoor resting malaria vector densities in rice irrigation scheme area in western Kenya. Malar J. 2009;8(1):108. doi: 10.1186/1475-2875-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kirby MJ, et al. Effect of two different house screening interventions on exposure to malaria vectors and on anaemia in children in The Gambia: a randomised controlled trial. Lancet. 2009;374(9694):998–1009. doi: 10.1016/S0140-6736(09)60871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hay SI, et al. Urbanization, malaria transmission and disease burden in Africa. Nat Rev Microbiol. 2005;3(1):81–90. doi: 10.1038/nrmicro1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillies MT, Wilkes TJ. The vertical distribution of some West African mosquitoes (Diptera, Culicidae) over open farmland in a freshwater area of the Gambia. Bull Entomol Res. 1976;66(01):5–15. doi: 10.1017/S0007485300006441. [DOI] [Google Scholar]
- 25.Snow WF. The vertical distribution of flying mosquitoes (Diptera: Culicidae) near an area of irrigated rice-fields in the Gambia. Bull Entomol Res. 1979;69(04):561–571. doi: 10.1017/S0007485300020113. [DOI] [Google Scholar]
- 26.Snow WF. Further observations on the vertical distribution of flying mosquitoes (Diptera: Culicidae) in West African savanna. Bull Entomol Res. 1982;72(04):695–708. doi: 10.1017/S0007485300008725. [DOI] [Google Scholar]
- 27.Charlwood JD, et al. Raised houses reduce mosquito bites. Malar J. 2003;2(1):45. doi: 10.1186/1475-2875-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Zulueta J. Malaria and ecosystems: from prehistory to posteradication. Parassitologia. 1994;36(1–2):7–15. [PubMed] [Google Scholar]
- 29.Peat JK, Dickerson J, Li J. Effects of damp and mould in the home on respiratory health: a review of the literature. Allergy. 1998;53(2):120–128. doi: 10.1111/j.1398-9995.1998.tb03859.x. [DOI] [PubMed] [Google Scholar]
- 30.Sahakian NM, Park JH, Cox-Ganser JM. Dampness and mold in the indoor environment: implications for asthma. Immunol Allergy Clin North Am. 2008;28(3):485–505. doi: 10.1016/j.iac.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 31.WHO guidelines for indoor air quality: selected pollutants. Geneva: WHO; 2010. [PubMed] [Google Scholar]
- 32.Fewtrell L, et al. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5(1):42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 33.Joint Monitoring Program. Progreess on drinking water and sanitation. 2012 update. 2012, UNICEF and WHO.
- 34.Cairncross S, Feachem R. Environmental health engineering in the tropics. An introductory text. 2. Chichester: Wiley; 1993. [Google Scholar]
- 35.Cairncross S. Water supply and the urban poor. In: Cairncross S, Hardoy JE, Satterthwaite D, eds. The poor die young: housing and health in Third World cities. London: EarthScan Publications; 1990. Chapter 5, p. 109–126.
- 36.Dean J, Hunter PR. Risk of gastrointestinal illness associated with the consumption of rainwater: a systematic review. Environ Sci Technol. 2012;46(5):2501–2507. doi: 10.1021/es203351n. [DOI] [PubMed] [Google Scholar]
- 37.Daoud AK, et al. Quality assessment of roof-harvested rainwater in the West Bank, Palestinian Authority. J Water Health. 2011;9(3):525–533. doi: 10.2166/wh.2011.148. [DOI] [PubMed] [Google Scholar]
- 38.Clasen T, et al. Interventions to improve water quality for preventing diarrhoea: systematic review and meta-analysis. BMJ. 2007;334(7597):782. doi: 10.1136/bmj.39118.489931.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmidt WP, Cairncross S. Household water treatment in poor populations: is there enough evidence for scaling up now? Environ Sci Technol. 2009;43(4):986–992. doi: 10.1021/es802232w. [DOI] [PubMed] [Google Scholar]
- 40.Brown J, Clasen T. High adherence is necessary to realize health gains from water quality interventions. PLoS One. 2012;7(5):e36735. doi: 10.1371/journal.pone.0036735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cordeiro R et al. Spatial distribution of the risk of dengue fever in southeast Brazil, 2006–2007. BMC Public Health, 2011. 11. [DOI] [PMC free article] [PubMed]
- 42.Moraes LR, Cancio JA, Cairncross S. Impact of drainage and sewerage on intestinal nematode infections in poor urban areas in Salvador, Brazil. Trans R Soc Trop Med Hyg. 2004;98(4):197–204. doi: 10.1016/S0035-9203(03)00043-9. [DOI] [PubMed] [Google Scholar]
- 43.Cairncross S, et al. The public and domestic domains in the transmission of disease. Trop Med Int Health. 1996;1(1):27–34. doi: 10.1046/j.1365-3156.1996.d01-9.x. [DOI] [PubMed] [Google Scholar]
- 44.Curtis V, et al. Hygiene: new hopes, new horizons. Lancet Infect Dis. 2011;11(4):312–321. doi: 10.1016/S1473-3099(10)70224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3(5):275–281. doi: 10.1016/S1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 46.M’Gonigle GCM. Nutrition; the position in England to-day. London: Industrial Christian Fellowship; 1936. [Google Scholar]
- 47.Jeuland MA, Pattanayak SK. Benefits and costs of improved cookstoves: assessing the implications of variability in health, forest and climate impacts. PLoS One. 2012;7(2):e30338. doi: 10.1371/journal.pone.0030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. Health principles of housing. 1989 [cited 29 May 2012]; Available from: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Health+principles+of+housing#0
- 49.Health impact assessment of housing improvements. A guide. Glasgow: Public Health Institute of Scotland; 2003. [Google Scholar]
- 50.Wilkinson D. Poor housing and ill health. A summary of researach evidence. Edinburgh: Scottish Office Central Research Unit; 1999. [Google Scholar]
- 51.Mitlin D, Satterthwaite D. Urban poverty in the global south: scale and nature. London: Routledge; 2012. [Google Scholar]
- 52.Boonyabancha S. Baan Mankong: going to scale with ‘slum’ and squatter upgrading in Thailand. Environ Urban. 2005;17(1):21–46. [Google Scholar]
- 53.Zero Carbon Compendium. Witsand Community Energy Project. [cited 27 May 2012]; Exemplar Project Case Studies of the Zero Carbon Compendium]. Available from: http://www.lowcarbonhomesworldwide.com/case-studies/countries/south-africa.html
- 54.Briceno-Leon R. Rural housing for control of Chagas disease in Venezuela. Parasitol Today. 1987;3(12):384–387. doi: 10.1016/0169-4758(87)90252-3. [DOI] [PubMed] [Google Scholar]
- 55.Cecere MC, et al. Effects of partial housing improvement and insecticide spraying on the reinfestation dynamics of Triatoma infestans in rural northwestern Argentina. Acta Trop. 2002;84(2):101–116. doi: 10.1016/S0001-706X(02)00183-3. [DOI] [PubMed] [Google Scholar]
- 56.de Arias Rojas A, et al. Chagas disease vector control through different intervention modalities in endemic localities of Paraguay. Bull World Health Organ. 1999;77(4):331–339. [PMC free article] [PubMed] [Google Scholar]
- 57.Curtis CF. Appropriate technology in vector control. Boca Raton: CRC Press; 1990. [Google Scholar]
- 58.Fuller-Thomson E, Hulchanski JD, Hwang S. The housing/health relationship: what do we know? Rev Environ Health. 2000;15(1–2):109–133. doi: 10.1515/reveh.2000.15.1-2.109. [DOI] [PubMed] [Google Scholar]
- 59.Burger H, Kaiser HE. Crowding. In Vivo. 1996;10(2):249–253. [PubMed] [Google Scholar]
- 60.Egbagbe EE, Okojie OH, Amaize E. Epidemiology of pulmonary tuberculosis in University of Benin Teaching Hospital and Central Hospital, Benin City. Nig Q J Hosp Med. 2011;21(2):159–162. [PubMed] [Google Scholar]
- 61.Elender F, Bentham G, Langford I. Tuberculosis mortality in England and Wales during 1982–1992: its association with poverty, ethnicity and AIDS. Soc Sci Med. 1998;46(6):673–681. doi: 10.1016/S0277-9536(97)00178-0. [DOI] [PubMed] [Google Scholar]
- 62.Baker M, et al. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatr Infect Dis J. 2000;19(10):983–990. doi: 10.1097/00006454-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 63.Moodley JR, Coetzee N, Hussey G. Risk factors for meningococcal disease in Cape Town. S Afr Med J. 1999;89(1):56–59. [PubMed] [Google Scholar]
- 64.Homoe P, Christensen RB, Bretlau P. Acute otitis media and sociomedical risk factors among unselected children in Greenland. Int J Pediatr Otorhinolaryngol. 1999;49(1):37–52. doi: 10.1016/S0165-5876(99)00044-0. [DOI] [PubMed] [Google Scholar]
- 65.Milne A, et al. A seroepidemiological study of the prevalence of hepatitis B infections in a hyperendemic New Zealand community. Int J Epidemiol. 1987;16(1):84–90. doi: 10.1093/ije/16.1.84. [DOI] [PubMed] [Google Scholar]
- 66.McCallion WA, et al. Helicobacter pylori infection in children: relation with current household living conditions. Gut. 1996;39(1):18–21. doi: 10.1136/gut.39.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brown LM. Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev. 2000;22(2):283–297. doi: 10.1093/oxfordjournals.epirev.a018040. [DOI] [PubMed] [Google Scholar]
- 68.Marsh A, et al. Housing deprivation and health: a longitudinal analysis. Hous Stud. 2000;15(3):411–428. doi: 10.1080/02673030050009258. [DOI] [Google Scholar]
- 69.Thomson H, et al. The health impacts of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009;99(Suppl 3):S681–S692. doi: 10.2105/AJPH.2008.143909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Evans GW, Maxwell LE, Hart B. Parental language and verbal responsiveness to children in crowded homes. Dev Psychol. 1999;35(4):1020–1023. doi: 10.1037/0012-1649.35.4.1020. [DOI] [PubMed] [Google Scholar]
- 71.Evans GW, et al. Chronic residential crowding and children’s well-being: an ecological perspective. Child Dev. 1998;69(6):1514–1523. [PubMed] [Google Scholar]
- 72.Fuller TD, et al. Chronic stress and psychological well-being: evidence from Thailand on household crowding. Soc Sci Med. 1996;42(2):265–280. doi: 10.1016/0277-9536(95)00089-5. [DOI] [PubMed] [Google Scholar]
- 73.Emond AM, et al. The effects of housing on the health of preterm infants. Paediatr Perinat Epidemiol. 1997;11(2):228–239. doi: 10.1046/j.1365-3016.1997.d01-15.x. [DOI] [PubMed] [Google Scholar]
- 74.Schluter PJ, et al. Housing and sudden infant death syndrome. The New Zealand Cot Death Study Group. N Z Med J. 1997;110(1047):243–246. [PubMed] [Google Scholar]
- 75.Govindarajan V and C Sarkar. $300 House. 2011 [cited 29 May2012]; Available from: http://www.300house.com/cgi-bin/mt/mt-search.cgi?blog_id=2&tag=%24300%20House&limit=20
- 76.Hernandez F, et al. Rethinking the informal city. Critical perspectives from Latin America. 2010: Berghahn Books.
- 77.Kwok AG, Grondzik WT. The green studio handbook—environmental strategies for schematic design. Oxford: Architectural Press; 2007. [Google Scholar]
- 78.Dherani M, et al. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in under-5 children: systematic review and meta-analysis. Bull World Health Organ. 2008;86(5):390–398. doi: 10.2471/BLT.07.044529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kurmi OP, et al. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65(3):221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 80.Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66(3):232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- 81.Pope DP, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. 2010;32(1):70–81. doi: 10.1093/epirev/mxq005. [DOI] [PubMed] [Google Scholar]
- 82.Pope CA, 3rd, et al. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure–response relationships. Environ Health Perspect. 2011;119(11):1616–1621. doi: 10.1289/ehp.1103639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cairncross S, Valdmanis V. Water supply, sanitation and hygiene promotion. In: Jamison DT, Breman JG, Measham AR, et al. eds. Disease Control Priorities in Developing Countries 2nd ed. Washington DC: The World Bank; 2006. Chapter 41, pp. 771–792.
- 84.Bartram J, Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7(11):e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee MS, et al. In-home solid fuel use and cardiovascular disease: a cross-sectional analysis of the Shanghai Putuo study. Environ Health. 2012;11:18. doi: 10.1186/1476-069X-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Smith KR, Peel JL. Mind the gap. Environ Health Perspect. 2010;118(12):1643–1645. doi: 10.1289/ehp.1002517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pokhrel AK, et al. Case–control study of indoor cooking smoke exposure and cataract in Nepal and India. Int J Epidemiol. 2005;34(3):702–708. doi: 10.1093/ije/dyi015. [DOI] [PubMed] [Google Scholar]
- 88.Zodpey SP, Ughade SN. Exposure to cheaper cooking fuels and risk of age-related cataract in women. Indian J Occup Environ Med. 1999;3(4):159–161. [Google Scholar]
- 89.Slama K, et al. Indoor solid fuel combustion and tuberculosis: is there an association? Int J Tuberc Lung Dis. 2010;14(1):6–14. [PubMed] [Google Scholar]
- 90.Kan X, et al. Indoor solid fuel use and tuberculosis in China: a matched case–control study. BMC Publ Health. 2011;11:498. doi: 10.1186/1471-2458-11-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gninafon M, et al. Exposure to combustion of solid fuel and tuberculosis: a matched case–control study. Eur Respir J. 2011;38(1):132–138. doi: 10.1183/09031936.00104610. [DOI] [PubMed] [Google Scholar]
- 92.Kaplan C. Indoor air pollution from unprocessed solid fuels in developing countries. Rev Environ Health. 2010;25(3):221–42. doi: 10.1515/REVEH.2010.25.3.221. [DOI] [PubMed] [Google Scholar]
- 93.Sapkota A, et al. Indoor air pollution from solid fuels and risk of hypopharyngeal/laryngeal and lung cancers: a multicentric case–control study from India. Int J Epidemiol. 2008;37(2):321–328. doi: 10.1093/ije/dym261. [DOI] [PubMed] [Google Scholar]
- 94.Pokhrel AK, et al. Tuberculosis and indoor biomass and kerosene use in Nepal: a case–control study. Environ Health Perspect. 2010;118(4):558–564. doi: 10.1289/ehp.0901032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Peck MD, et al. Burns and fires from non-electric domestic appliances in low and middle income countries. Part I. The scope of the problem. Burns. 2008;34(3):303–311. doi: 10.1016/j.burns.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 96.Smith KR, et al. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet. 2011;378(9804):1717–1726. doi: 10.1016/S0140-6736(11)60921-5. [DOI] [PubMed] [Google Scholar]
- 97.Chapman RS, et al. Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ. 2005;331(7524):1050. doi: 10.1136/bmj.38628.676088.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Global Alliance for Clean Cookstoves (An initiative led by the United Nations Foundation). [cited 2012 29 May 2012]; Available from: http://www.cleancookstives.org
- 99.Combined household water treatment and indoor air pollution projects in urban Mambanda, Cameroon and rural Nyanza, Kenya. Geneva: WHO; 2011. [Google Scholar]
- 100.Biran A, et al. Smoke and malaria: are interventions to reduce exposure to indoor air pollution likely to increase exposure to mosquitoes? Trans R Soc Trop Med Hyg. 2007;101(11):1065–1071. doi: 10.1016/j.trstmh.2007.07.010. [DOI] [PubMed] [Google Scholar]