Abstract
Older adults may be more vulnerable to negative health effects from alcohol as they age. Distress and adverse neighborhood conditions that provoke distress may influence drinking behavior. Using baseline data from the Baltimore Memory Study, a cohort study of adults aged 50–70 years living in 65 Baltimore City neighborhoods, we investigated the association between neighborhood psychosocial hazards (NPH) and the number of binge drinking days in the past month among non-abstainers (N = 645). We used negative binomial regression with generalized estimating equations to estimate the relative number of binge drinking days per month associated with a one standard deviation increase in NPH score. Residing in neighborhoods with more psychosocial hazards was independently associated with more binge drinking for females, but not for males. For females, each one standard deviation increase in NPH score was associated with a 1.52 relative risk of binge drinking (95 % confidence interval, 1.10, 2. 10) in the adjusted model. The findings were robust to a sensitivity analysis in which we used the average number of drinks per drinking occasion as an alternative outcome. Our findings provide evidence linking adverse neighborhood conditions with alcohol consumption in non-abstaining late middle-aged women, and suggest that late middle-aged men and women may have different reactions to adverse residential neighborhoods.
Keywords: Alcohol, Community, Neighborhood, Older adults, Urban
Introduction
Risky drinking is frequently reported among young adults.1,2 However, a recent report found that British adults 55–74 years old spent more than ten times the amount that 16–24 year olds spent on alcohol-related hospitalizations.3 In the USA, alcohol-related hospitalizations in older adults occur with a frequency similar to heart attacks.4
These findings may seem surprising given that average per-person alcohol consumption decreases, rates of binge drinking decrease, and the incidence and prevalence of alcohol abuse and dependence disorders also tend to decrease with age1,5-8 (mildly until around age 70 and more steeply thereafter),9 although not for all subgroups.10,11 Among late middle-aged U.S. adults (45–65 years), prevalence of past-year alcohol abuse or dependence is estimated to be 8.2 % for males and 2.9 % for females, 2,12 4–5 % of adults 55 and older report binge drinking in the past month,13 and 9 % of adults over age 65 consume alcohol in excess of national guidelines.14
Older adults may be more vulnerable to the negative health effects of alcohol than their younger counterparts due, in part, to interactions with prescription medications and less efficient metabolism of alcohol, which results in older adults having higher blood alcohol levels than younger adults after consuming a similar amount.7,15,16 The population attributable risk of these vulnerabilities will increase sharply with the aging of the population coupled with possibly higher drinking levels in the baby boomer and younger cohorts.1,8 To inform public health efforts to minimize drinking-related health problems, a comprehensive understanding of risk factors and risk regulators is needed.
Previous research suggests that distress is a risk factor for drinking-related health problems. The tension reduction hypothesis posits that individuals may use alcohol to reduce tension or distress.17 Congruent with this hypothesis, avoidance coping is predictive of late-life drinking.18 Older adults may more frequently experience provocations of stress such as loneliness, loss of a partner or close friend/family member, and loss of income. Loneliness has been related to risky drinking and alcohol abuse,19 loss of a partner and other non-health-related negative life events have been associated with subsequent increases in drinking and diminished declines in drinking among older adults (although evidence is mixed),11,20-22 and while high socioeconomic status (SES) is typically associated with more frequent drinking, low SES is associated with more risky/binge drinking.23
Although a potentially powerful explanation for individual drinking behavior, the tension reduction hypothesis by itself does not explain the environmental roots that give rise to the stress response and the experience of distress. Although evidence is mixed, neighborhood poverty, neighborhood disorder, deterioration of the built environment, and violence have been associated with biologic indicators of stress and depression.24-26 We hypothesize that exposure to neighborhood psychosocial hazards (relatively stable and visible features of local environments that give rise to a heightened state of fear, vigilance, and threat) may provoke a chronic state of subjective distress, which may increase alcohol consumption through mechanisms suggested in the tension reduction hypothesis.
Evidence suggests that this process may operate differently in men and women. Women may be more likely to perceive neighborhood problems as serious and may be more likely to be fearful.27 Men may be more likely to externalize their distress—for instance, by binge drinking—while women may be more likely to internalize their distress—for instance, through the development of depression and anxiety.28-31 In addition, research suggests that women spend more time in their neighborhoods and so may have greater exposure to psychosocial hazards.32,33
Examination of gender differences in the relationship between neighborhood characteristics and alcohol outcomes was one recommendation of a recent review of the literature.34 (More recent manuscripts have heeded this recommendation and have found qualitatively different effects for men and women, although the directions have been inconsistent).35-39 In the review by Karriker-Jaffe, consistent associations between neighborhood disadvantage and heavy drinking were reported.34 More recent studies not included in this review have corroborated this finding; although the frequency of alcohol use generally increases in higher SES neighborhoods, binge drinking, heavy alcohol use, and other risky drinking behaviors tend to decrease,35,40 although the evidence is mixed.41-43 Similar relationships have been found for other neighborhood measures, such as neighborhood disorder, cohesion, unemployment, and deterioration of the built environment.36,39,44-47
Although there is emerging evidence of an association between aspects of neighborhood disadvantage and drinking behavior among adults, several research gaps remain. Not only is the examination of gender differences lacking, but there is limited data on this relationship in late middle-aged and older adults.34 Furthermore, while many studies cite psychosocial stress as a possible mediator,48 we know of no study that uses a theory-guided summary measure of neighborhood psychosocial hazards. These research gaps, the vulnerability of older adults, and the rapid aging of the U.S. population motivate this study.
Using baseline data from the Baltimore Memory Study, a cohort study of non-institutionalized adults aged 50–70 years living in 65 contiguous Baltimore City neighborhoods,49 our objective was to investigate the association between neighborhood psychosocial hazards and binge drinking separately for men and women. Designed with the current research gaps and challenges in mind, this study uses objective measures of the neighborhood environment and defines neighborhoods in sociologically meaningful terms.
Methods
Overview
The Baltimore Memory Study (BMS) was designed to study individual- and neighborhood-level risk factors for cognitive decline among late middle-aged to older adults living in Baltimore City. The goals and sampling and recruitment methods of the BMS cohort have been described elsewhere.49 Briefly, the BMS study area consists of 65 contiguous neighborhoods in central and north Baltimore City that were selected to have variability in demographic characteristics of interest. There are 264 neighborhoods in the City of Baltimore, which were defined in a collaborative effort between the Department of Planning and city residents in the 1970s and updated in 1990 and 2000.
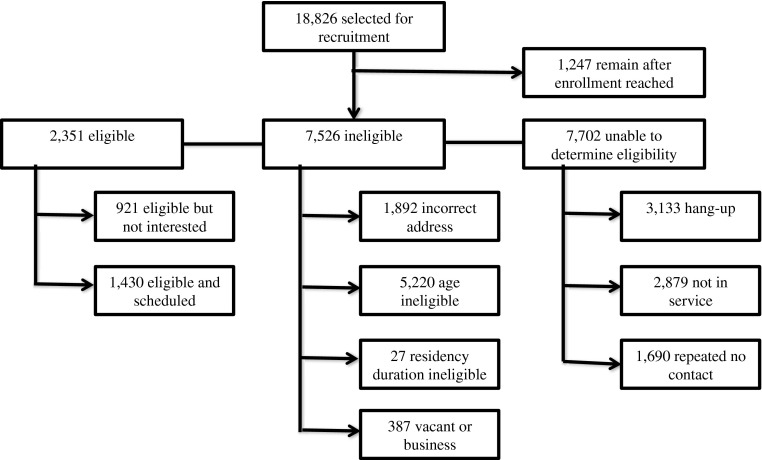
Study participants were recruited from a probability sample of all Baltimore City residential properties listed in the Department of Assessments and Taxation. Out of 1,403 eligible, sampled residents, 81.3 % (N = 1,140) agreed to participate and completed the baseline visit. Figure 1 provides more detail on sample recruitment. Eligibility criteria consisted of being 50–70 years old at baseline and having lived in the greater Baltimore area for the previous 5 years. The study was approved by the Committee on Human Research of the Johns Hopkins Bloomberg School of Public Health.
FIGURE 1.
Baltimore Memory Study participant enrollment, 2001–2002.
Neighborhood Measures
The primary exposure of interest was neighborhood psychosocial hazards (NPH), measured using a previously described scale.50 Briefly, the NPH scale is intended to measure relatively stable and visible features of residential neighborhoods that give rise to a state of heightened vigilance and fear and are hypothesized to evoke a stress response. The scale is composed of 12 indicators (percent single parent families; percent adults without high school degree or equivalent; percent adults divorced, separated or widowed; number of 911 calls; number of violent crimes; percent vacant houses; number of complaints about street conditions; number of liquor stores or off-site liquor licenses; per capita income; index of working class; percent adults unemployed; percent families in poverty) using factor analysis to measure a single construct of neighborhood psychosocial hazards. Each indicator was transformed to a z-score, and all indicators were summed to make a normally distributed scale (mean = 0.1, standard deviation = 9.6) that ranges from −19.0 to 19.2. Higher scores indicate neighborhoods with more psychosocial hazards, and lower scores indicate neighborhoods with fewer.
Data for the indicators were sourced from the 2000 U.S. Census and the Baltimore City Departments of Planning, Public Works, and Police. The U.S. Census aggregated block-level data to the 65 neighborhoods in the study area by special request. Point data, such as violent crimes, 911 calls, and off-site liquor licenses, were mapped to the appropriate neighborhood boundaries using geographic information systems (GIS).
Individual Measures
All other measures used for this analysis came from a structured interview administered to each participant at baseline. The method of administering these interviews has been described elsewhere.49 Briefly, a trained interviewer conducted a structured interview lasting approximately 2 h with each participant in the study clinic. The structured interviews collected basic demographic information, such as sex, age (in years), self-reported race/ethnicity (corresponding to the 2000 Census categories), residential address history, level of education (years completed and degrees/certificates attained), marital status, and household wealth (including income, transfers from social programs, and assets, in U.S. dollars). For this analysis, participant age was classified by decade—50–59 years old or 60–70 years old—because we did not believe that a 1-year change in age would appreciably influence binge drinking behavior. Continuous parameterization of age provided similar inferences (data not shown). Race/ethnicity was dichotomized to white or non-white because few individuals self-identified as other than white or African American. Level of education was analyzed as an ordinal, eight-category variable of attainment. Marital status was dichotomized to married at baseline versus not. A five-category marital status variable yielded similar inferences (data not shown). Household wealth was log-transformed and analyzed as a continuous measure. Resident addresses were mapped to the appropriate neighborhood using GIS.
Study participants were also administered the seven-item portion of the Older Adults Resources and Services scale that assesses an older adult’s ability to complete instrumental activities of daily living (IADL; e.g., preparing meals, using the telephone).51 For this analysis, individuals with a score of one or greater were classified as IADL disabled.
Alcohol consumption was also collected by self-report in the structured interview. Individuals reported whether they had drunk at least one alcoholic beverage in the past month. One alcoholic beverage is defined as one glass of wine, one can or bottle of beer, one can or bottle of wine cooler, one cocktail, or one shot of liquor. Those individuals who reported having at least one drink in the past month were then asked to report the number of days in the past month that they consumed four or more drinks on one occasion for women and six or more drinks on one occasion for men (binge drinking), thereby exceeding the 2005 gender-specific guidelines of the National Institute on Alcohol Abuse and Alcoholism.52
Our primary outcome of interest was the number of days that an individual binge drank in the past month. The average number of drinks per day on days that an individual drank was used as an alternative outcome in a pre-planned sensitivity analysis.
Statistical Methods
The objective of our analysis was to examine whether living in neighborhoods with more psychosocial hazards was associated with more binge drinking days separately for men and women. For this analysis, we excluded participants who reported having zero alcoholic drinks in the past month because we assume that they are not at risk for stress-related drinking. This method has been used previously.38,46 Out of the 1,140 BMS participants, the analyses presented here include the 673 participants who reported ever having a drink in the past month (henceforth referred to as “non-abstainers”).
Negative binomial regression with generalized estimating equations was used to estimate the association between NPH and binge drinking days. The negative binomial model was chosen because it better represents the overdispersed count data by modeling it as a Poisson-Gamma mixture. Zero-inflated Poisson and zero-inflated negative binomial models did not significantly improve model fit. Generalized estimating equations were used to account for the clustering of individuals by neighborhood.53 The regression coefficient for the exposure of interest is interpreted as the average relative number of binge drinking days per month associated with a one standard deviation increase in NPH score.
To estimate the independent contribution of NPH, we controlled for variables hypothesized to be potential confounders of the exposure–outcome (NPH–binge drinking) relationship. These included age, IADL disability, race/ethnicity, marital status, level of education, and household wealth. We hypothesized that the relationship between NPH and binge drinking operates differently for males versus females. We also hypothesized that the confounding effects of variables like marital status and level of household wealth would operate differently by sex. Therefore, instead of including multiple interaction terms in the model, we chose to model the relationship separately in males and females.
Results
Of the Baltimore Memory Study participants, 66 % were female, 11 % were disabled, 54 % were white, and 43 % were 60 years or older at baseline (Table 1). Overall, 673 (59 %) reported ever having an alcoholic drink in the past month (“non-abstainers”), and 158 (14 %) reported ever having a binge drinking episode in the past month.
Table 1.
Self-reported past-month drinking history and characteristics of study participants at enrollment: Baltimore Memory Study, 2001–2002
| Entire cohort | Abstainers | Non-abstainers | Ever binge drinkers | |
|---|---|---|---|---|
| Participants, no. (%) | 1,140 (100) | 466 (40.9) | 673 (59.0) | 158 (13.9) |
| Age (years), no. (%) | ||||
| 50–59 | 649 (56.9) | 255 (54.7) | 393 (58.4) | 98 (62.0) |
| 60–70 | 491 (43.1) | 211 (45.3) | 280 (41.6) | 60 (38.0) |
| Women, no. (%) | 749 (65.7) | 352 (75.5) | 396 (58.8) | 86 (54.4) |
| Disabled (IADL), no. (%) | 123 (10.8) | 74 (15.9) | 49 (7.3) | 11 (7.1) |
| Household wealth (log), median (IQR) | 11.84 (11.0, 12.6) | 11.42 (10.5, 12.0) | 12.16 (11.4, 13.0) | 11.9 (11.0, 12.7) |
| Level of education, median (IQR)a | 4 (3, 7) | 4 (3, 6) | 6 (3, 8) | 4 (3, 7) |
| Married, no. (%) | 492 (43.2) | 181 (38.9) | 310 (46.1) | 61 (38.6) |
| Race/ethnicity, no. (%) | ||||
| Non-white | 529 (46.4) | 305 (65.5) | 224 (33.3) | 60 (38.0) |
| White | 611 (53.6) | 161 (34.6) | 449 (66.7) | 98 (62.0) |
| NPH scale, median (IQR) | −2.72 (−6.84, 5.75) | 1.33 (−5.12, 8.60) | −3.95 (−9.92, 2.71) | −2.72 (−6.86, 2.71) |
aModeled as an ordinal variable (1–8): 1 = less than high school, 2 = less than high school with GED, 3 = high school graduate, 4 = high school graduate with trade schooling, 5 = some college or associate’s degree, 6 = bachelor’s degree, 7 = bachelor’s degree with some graduate school, 8 = master’s or doctoral degree)
In the unadjusted model (Table 2), a one standard deviation increase in NPH score was associated with a 49 % increase [95 % confidence interval (CI), 8 %, 105 %] in binge drinking days per month for females and a 13 % increase (95 % CI, −16 %, 52 %) for males. We then adjusted for age, race/ethnicity, marital status, level of education, household wealth, and disability status. In the fully adjusted model (Table 2), residing in neighborhoods with higher NPH scores was independently associated with more binge drinking days per month for females, but no association was observed for males. For females, each one standard deviation increase in NPH score was associated with 52 % (95 % CI, 10 %, 110 %) more binge drinking days per month. Neither age nor race/ethnicity was independently associated with binge drinking for either sex. Household wealth was not associated with binge drinking rates for females, but greater household wealth was associated with decreased binge drinking rates in males. Higher level of education was associated with decreased binge drinking rates in females, but no association was seen for males. Disability was associated with binge drinking in both sexes, but in opposite directions. However, the small number of disabled individuals cautions against drawing conclusions from this finding.
Table 2.
Association of neighborhood psychosocial hazards scale scores with self-reported number of binge drinking episodes in the past month among non-abstainers in unadjusted and adjusted models: Baltimore Memory Study, 2001–2002; RR (95 % CI)
| Unadjusted model | Adjusted model | |||
|---|---|---|---|---|
| Females (n = 392) | Males (n = 271) | Females (n = 392) | Males (n = 271) | |
| NPH scale (1 SD) | 1.49 (1.08, 2.05) | 1.13 (0.84, 1.52) | 1.52 (1.10, 2.10)* | 0.83 (0.61, 1.12) |
| Over age 60 | 1.00 (0.52, 1.92) | 1.20 (0.62, 2.35) | ||
| Disabled (IADL) | 5.36 (1.62, 17.72)** | 0.04 (0.01, 0.28)* | ||
| Household wealth (log) | 1.14 (0.93, 1.41) | 0.70 (0.59, 0.82)* | ||
| Level of education | 0.87 (0.76, 0.99)* | 1.02 (0.86, 1.20) | ||
| Married | 0.69 (0.44, 1.07) | 0.60 (0.30, 1.20) | ||
| Non-white race | 0.83, (0.51, 1.35) | 0.94 (0.53, 1.68) | ||
*p < 0.05; **p < 0.01
Discussion
In a large probability sample of late middle-aged adults living in Baltimore City from 2001–2002, residing in neighborhoods with more psychosocial hazards was associated with more binge drinking episodes among females but not males. Previous studies have provided evidence of an association between neighborhood disadvantage and drinking behaviors,40,54,55 and several studies have shown an association between possible neighborhood psychosocial hazards—neighborhood physical decay and perceived neighborhood disorder—and drinking.39,44-46 Our results extend this literature by (1) studying the relationship among late middle-aged adults, (2) accounting for male/female differences, and (3) using a theory-guided summary measure of neighborhood psychosocial hazards.
As previously discussed, women tend to spend more time in their neighborhoods than men, tend to perceive more neighborhood problems as serious, and tend to be more fearful.27,32,33 Therefore, it is plausible that residence in a neighborhood with a given level of psychosocial hazards would engender a greater level of distress in women than it would in men. However, because women are less likely to externalize distress, we were unsure whether this distress would manifest in drinking behavior.
Our results suggest that NPH is associated in increased binge drinking for late middle-aged women—consistent with the tension reduction hypothesis. We tested the robustness of our findings by conducting several sensitivity analyses. First, we ran one model including a sex-by-NPH interaction term. This interaction term was statistically significant at the alpha = 0.05 level, thereby strengthening the evidence of a male–female difference. In another sensitivity analysis, we used an alternative outcome measure: the average number of drinks per day on days that an individual drank. Our inferences were the same as in our primary analysis, which suggests that our results do not depend entirely on our measure of alcohol consumption.
Two additional sensitivity analyses tested the robustness of our results to different inclusion criteria. Our primary analysis included study participants who reported consuming any alcoholic drink in the past month because we hypothesized this group to be at risk for using alcohol as a means to reduce psychosocial distress. It could be argued that those addicted to alcohol are not at risk for using alcohol in this way because they may be likely to drink heavily regardless of current exposure to psychosocial hazards. To test the sensitivity of our results to this assumption, we re-ran the model excluding participants who reported binge drinking on most (24 or more) days in the past month. For females, the effect size of the association between NPH and binge drinking increased slightly and remained statistically significant. There remained no effect for males.
We found that a large fraction (41 %) of this community-based cohort were abstainers who reported no alcohol consumption in the previous month. This supports national survey data showing that the percentage of late middle-aged to older adults abstaining from alcohol ranges from 42 % for those aged 50–55 years to 62 % for adults over 65 years.56 Although we hypothesized that abstainers would not be at risk for using alcohol as a tension-reduction tool, it is possible that some late middle-aged adults classified as abstainers in our primary analysis were misclassified. To assess the sensitivity of our results to these assumptions, we re-ran the model including all 1,140 participants. The effect size for females decreased by half and was no longer significant. This is expected because including a substantial fraction of the population not at risk for binge drinking will bias the effect estimate toward the null. There remained no association among males.
While our goal was to estimate the relationship between the latent construct of NPH and binge drinking, it may be informative to understand the relationships between the individual indicators used to measure NPH and binge drinking. To this end, we examined the independent association between each NPH indicator and binge drinking as a sensitivity analysis. Many of the indicators were associated with increased binge drinking in females, including indicators of neighborhood public safety (violent crimes and 911 calls), economic deprivation (percent of adults unemployed, percent families living in poverty), and social disorganization (percent single parent families and percent adults divorced, separated, or widowed). Only two indicators were associated with binge drinking in males and in the opposite direction. Percent of adults unemployed and index of working class were associated with decreased binge drinking among males. Indicators related to neighborhood physical disorder—including the number of liquor stores or off-site liquor licenses—were not independently associated with binge drinking in males or females (results not shown but available from author upon request).
Limitations
This analysis is subject to several limitations. Because this analysis was cross-sectional, we lack compelling evidence as to whether social selection, social causation, or some combination of the two was responsible for the association. However, residential stability was high among the study participants with most (74 %) living in their current residence for more than 10 years, and study eligibility criteria ensured that all participants lived in their current neighborhoods for a minimum of 5 years. Moreover, there is evidence that when individuals do move, they move to similar neighborhoods.57 Considered together, exposure to NPH appears relatively stable, so it is unlikely that its association with binge drinking could be solely attributed to social selection.
Our primary analysis was not designed to disentangle NPH and alcohol availability because the number of liquor stores or off-site liquor licenses was an indicator measuring the latent construct of NPH. Alcohol availability—particularly alcohol density—has been shown to be associated with alcohol consumption and drinking patterns, but evidence is mixed.58,59 In Baltimore, alcohol may be sold in restaurants for on-site consumption or in liquor stores for off-site consumption. Previous research into alcohol availability in Baltimore found that liquor stores are concentrated in poor, African-American communities, which may facilitate risky drinking.60 In the previously discussed sensitivity analysis in which we examined the association between each NPH indicator and binge drinking, there was no significant association between number of liquor stores/off-site licenses and binge drinking in men or women. Instead, significant associations between indicators of public safety and economic disadvantage such as unemployment and poverty suggest that binge drinking may be motivated more as a stress-reduction strategy and less by availability.
Although we did not explore mental health mediators or comorbidities in the primary analysis, depression has been hypothesized to lie on the causal pathway between NPH and binge drinking.37 Depression is also more prevalent among women, and therefore could potentially explain the sex differences we found. However, the presence of depressive symptoms, defined as a score of greater than or equal to 16 on the Centre for Epidemiological Studies-Depression Scale, was not independently associated with NPH, suggesting that it may not be a significant mediator. Moreover, when added to the primary model, our inferences were not changed, the presence of depressive symptoms was not independently associated with binge drinking, and it did not improve model fit as tested by a likelihood ratio test (results not shown but available from the author upon request).
Another limitation of this study is our imperfect measure of risky drinking. This study included quantity-frequency measures of alcohol consumption, which are not designed to capture the presence of alcohol problems, abuse, or dependence. In addition, measures of alcohol consumption in this study were self-reported, and underreporting alcohol use is problematic in retrospective surveys that ask participants about consumption patterns in the past month.61 However, similar measures of binge drinking have been used previously as a proxy for short-term harmful consumption.58 Lastly, our results may be specific to our cohort. One might find different results in a nationally representative sample of late middle-aged adults.
Strengths
This study has two key strengths. First, this study was designed with the intent of examining aspects of the neighborhood physical and sociological environments that place residents at differential risk for unhealthy behaviors and illness. To this end, neighborhoods were classified using geographic boundaries that were defined by the City of Baltimore and its residents—as opposed to using U.S. Census tract or block group designations. Defining geographic boundaries in this way has the advantage of reducing non-differential misclassification of the exposure of interest—NPH—and thus providing less dilute effect estimates.62
The NPH scale is another strength. Many neighborhood research studies measure exposure through resident perceptions. This strategy can result in dependent measurement error when the exposure and outcome measures originate from the same source.25 Furthermore, resident perceptions of the neighborhood are socially constructed, and some have argued that they should not be treated as “unambiguous indicators of neighborhood ecology.”63 In contrast, the NPH scale is composed of objective indicators of psychosocial hazards sourced from the U.S. Census and Baltimore City Departments of Police, Planning, and Public Works. This scale is well established; it has been described and used in previous literature to represent neighborhood-level exposures to psychosocial hazards in this same study population, and has been shown to have both main effects with health outcomes and exhibit effect modification of other exposures in their relation with health outcomes in prior analyses.50,64
Conclusion
Older adults are the fastest growing subset of the population, and they are also increasingly vulnerable to the deleterious health effects of alcohol consumption. Thus, preventing alcohol-related health problems among this population will likely assume greater urgency in the coming years. Older adults may also be vulnerable to neighborhood effects as their mobility decreases.65 This context coupled with our findings suggest that the neighborhood environment may be a potentially powerful intervention target for improving the health of late middle-aged adults—especially women. While there is no quick fix for neighborhood psychosocial hazards, some are amenable to change through policy. For example, Detroit’s current mayor initiated an aggressive campaign to demolish 10,000 vacant houses in his 4-year term.66 Several cities, including Chicago, Los Angeles, and New York City, adopted aggressive misdemeanor policing policies in the 1990s aimed at reducing neighborhood crime and physical decay.67 Thus, it may be possible to use policy to improve place. Such interventions may engender positive public health effects that extend well beyond drinking behavior.
Acknowledgments
The authors would like to acknowledge the Baltimore Memory Study participants and study team.
This research was supported in part by the Division of Intramural Research Programs at the National Institute of Mental Health. The Baltimore Memory Study was supported by grants R01 AG19604 from the National Institute of Aging. National Institute of Aging had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report, and in the decision to submit the paper for publication.
References
- 1.Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alcohol. 1997;58(5):464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- 2.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Triggle N. Baby boomer alcohol harm 'more likely than in young'. BBC News. October 11, 2012. www.bbc.co.uk/news/health-19913431. Accessed 26 Nov 2012.
- 4.Adams WL, Yuan Z, Barboriak JJ, Rimm AA. Alcohol-related hospitalizations of elderly people. Prevalence and geographic variation in the United States. JAMA. 1993;270(10):1222–1225. doi: 10.1001/jama.1993.03510100072035. [DOI] [PubMed] [Google Scholar]
- 5.Crum RM, Chan YF, Chen LS, Storr CL, Anthony JC. Incidence rates for alcohol dependence among adults: prospective data from the Baltimore epidemiologic catchment area follow-up survey, 1981–1996. J Stud Alcohol. 2005;66(6):795–805. doi: 10.15288/jsa.2005.66.795. [DOI] [PubMed] [Google Scholar]
- 6.Karlamangla A, Zhou K, Reuben D, Greendale G, Moore A. Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction. 2006;101(1):91–99. doi: 10.1111/j.1360-0443.2005.01299.x. [DOI] [PubMed] [Google Scholar]
- 7.Gurnack AM. Older Adults' Misuse of Alcohol, Medicines, and Other Drugs: Research and Practice Issues. New York: Springer; 1997. [Google Scholar]
- 8.Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort modelling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction. 2009;104(1):27–37. doi: 10.1111/j.1360-0443.2008.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brennan PL, Schutte KK, Moos RH. Patterns and predictors of late-life drinking trajectories: a 10-year longitudinal study. Psychol Addict Behav. 2010;24(2):254–264. doi: 10.1037/a0018592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caetano R, Kaskutas LA. Changes in drinking patterns among whites, blacks and Hispanics, 1984–1992. J Stud Alcohol. 1995;56(5):558–565. doi: 10.15288/jsa.1995.56.558. [DOI] [PubMed] [Google Scholar]
- 11.Platt A, Sloan FA, Costanzo P. Alcohol-consumption trajectories and associated characteristics among adults older than age 50. J Stud Alcohol Drugs. 2010;71(2):169–179. doi: 10.15288/jsad.2010.71.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falk DE, Yi HY, Hiller-Sturmhofel S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Res Health. 2006;29(3):162–171. [PMC free article] [PubMed] [Google Scholar]
- 13.Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289(1):70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 14.Merrick EL, Horgan CM, Hodgkin D, et al. Unhealthy drinking patterns in older adults: prevalence and associated characteristics. J Am Geriatr Soc. 2008;56(2):214–223. doi: 10.1111/j.1532-5415.2007.01539.x. [DOI] [PubMed] [Google Scholar]
- 15.Culberson JW. Alcohol use in the elderly: beyond the CAGE. Part 1 of 2: prevalence and patterns of problem drinking. Geriatrics. 2006;61(10):23–27. [PubMed] [Google Scholar]
- 16.Vestal RE, McGuire EA, Tobin JD, Andres R, Norris AH, Mezey E. Aging and ethanol metabolism. Clin Pharmacol Ther. 1977;21(3):343–354. doi: 10.1002/cpt1977213343. [DOI] [PubMed] [Google Scholar]
- 17.Conger JJ. Alcoholism: theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Q J Stud Alcohol. 1956;17(2):296–305. [PubMed] [Google Scholar]
- 18.Moos RH, Schutte K, Brennan P, Moos BS. Ten-year patterns of alcohol consumption and drinking problems among older women and men. Addiction. 2004;99(7):829–838. doi: 10.1111/j.1360-0443.2004.00760.x. [DOI] [PubMed] [Google Scholar]
- 19.Akerlind I, Hornquist JO. Loneliness and alcohol abuse: a review of evidences of an interplay. Soc Sci Med. 1992;34(4):405–414. doi: 10.1016/0277-9536(92)90300-F. [DOI] [PubMed] [Google Scholar]
- 20.Brennan PL, Schutte KK, Moos RH. Reciprocal relations between stressors and drinking behavior: a three-wave panel study of late middle-aged and older women and men. Addiction. 1999;94(5):737–749. doi: 10.1046/j.1360-0443.1999.94573712.x. [DOI] [PubMed] [Google Scholar]
- 21.Glass TA, Prigerson H, Kasl SV, Mendes de Leon CF. The effects of negative life events on alcohol consumption among older men and women. J Gerontol B Psychol Sci Soc Sci. 1995;50(4):S205–S216. doi: 10.1093/geronb/50B.4.S205. [DOI] [PubMed] [Google Scholar]
- 22.Graham K, Schmidt G. Alcohol use and psychosocial well-being among older adults. J Stud Alcohol. 1999;60(3):345–351. doi: 10.15288/jsa.1999.60.345. [DOI] [PubMed] [Google Scholar]
- 23.Dawson DA, Grant BF, Chou SP, Pickering RP. Subgroup variation in U.S. drinking patterns: results of the 1992 national longitudinal alcohol epidemiologic study. J Subst Abuse. 1995;7(3):331–344. doi: 10.1016/0899-3289(95)90026-8. [DOI] [PubMed] [Google Scholar]
- 24.Bird CE, Seeman T, Escarce JJ, et al. Neighbourhood socioeconomic status and biological 'wear and tear' in a nationally representative sample of US adults. J Epidemiol Community Health. 2010;64(10):860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 26.Nazmi A, Roux AD, Ranjit N, Seeman TE, Jenny NS. Cross-sectional and longitudinal associations of neighborhood characteristics with inflammatory markers: findings from the multi-ethnic study of atherosclerosis. Health Place. 2010;16(6):1104–1112. doi: 10.1016/j.healthplace.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanson RF, Smith DW, Kilpatrick DG, Freedy JR. Crime-related fears and demographic diversity in Los Angeles County after the 1992 civil disturbances. J Community Psychol. 2000;28(6):607–623. doi: 10.1002/1520-6629(200011)28:6<607::AID-JCOP5>3.0.CO;2-Y. [DOI] [Google Scholar]
- 28.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiat. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 29.Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Pers Indiv Differ. 2001;30(7):1245–1259. doi: 10.1016/S0191-8869(00)00106-9. [DOI] [Google Scholar]
- 30.Rosenfield S, Vertefuille J, McAlpine DD. Gender stratification and mental health: an exploration of dimensions of the self. Soc Psychol Q. 2000;63(3):208–223. doi: 10.2307/2695869. [DOI] [Google Scholar]
- 31.Trickett PK, Mcbridechang C. The developmental impact of different forms of child-abuse and neglect. Dev Rev. 1995;15(3):311–337. doi: 10.1006/drev.1995.1012. [DOI] [Google Scholar]
- 32.Kwan M-P. Gender, the home-work link, and space-time patterns of nonemployment. Econ Geogr. 1999;75(4):370–394. doi: 10.2307/144477. [DOI] [Google Scholar]
- 33.Murtagh KN, Hubert HB. Gender differences in physical disability among an elderly cohort. Am J Public Health. 2004;94(8):1406–1411. doi: 10.2105/AJPH.94.8.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karriker-Jaffe KJ. Areas of disadvantage: a systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug Alcohol Rev. 2011;30(1):84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karriker-Jaffe KJ, Zemore SE, Mulia N, Jones-Webb R, Bond J, Greenfield TK. Neighborhood disadvantage and adult alcohol outcomes: differential risk by race and gender. J Stud Alcohol Drugs. 2012;73(6):865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuipers MA, van Poppel MN, van den Brink W, Wingen M, Kunst AE. The association between neighborhood disorder, social cohesion and hazardous alcohol use: a national multilevel study. Drug Alcohol Depend. 2012;126(1–2):27–34. doi: 10.1016/j.drugalcdep.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 37.Matheson FI, White HL, Moineddin R, Dunn JR, Glazier RH. Drinking in context: the influence of gender and neighbourhood deprivation on alcohol consumption. J Epidemiol Community Health. 2012;66(6):e4. doi: 10.1136/jech.2010.112441. [DOI] [PubMed] [Google Scholar]
- 38.Mulia N, Karriker-Jaffe KJ. Interactive influences of neighborhood and individual socioeconomic status on alcohol consumption and problems. Alcohol Alcohol. 2012;47(2):178–186. doi: 10.1093/alcalc/agr168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Praag L, Bracke P, Christiaens W, Levecque K, Pattyn E. Mental health in a gendered context: gendered community effect on depression and problem drinking. Health Place. 2009;15(4):990–998. doi: 10.1016/j.healthplace.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 40.Cerda M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. 2010;21(4):482–489. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Connolly S, O'Reilly D, Rosato M, Cardwell C. Area of residence and alcohol-related mortality risk: a five-year follow-up study. Addiction. 2011;106(1):84–92. doi: 10.1111/j.1360-0443.2010.03103.x. [DOI] [PubMed] [Google Scholar]
- 42.Giskes K, Turrell G, Bentley R, Kavanagh A. Individual and household-level socioeconomic position is associated with harmful alcohol consumption behaviours among adults. Aust N Z J Public Health. 2011;35(3):270–277. doi: 10.1111/j.1753-6405.2011.00683.x. [DOI] [PubMed] [Google Scholar]
- 43.Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role? Int J Epidemiol. 2005;34(4):772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- 44.Bernstein KT, Galea S, Ahern J, Tracy M, Vlahov D. The built environment and alcohol consumption in urban neighborhoods. Drug Alcohol Depend. 2007;91(2–3):244–252. doi: 10.1016/j.drugalcdep.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 45.Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med. 2005;61(5):965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 46.Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103(8):1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin EY, Witten K, Casswell S, You RQ. Neighbourhood matters: perceptions of neighbourhood cohesiveness and associations with alcohol, cannabis and tobacco use. Drug Alcohol Rev. 2012;31(4):402–412. doi: 10.1111/j.1465-3362.2011.00385.x. [DOI] [PubMed] [Google Scholar]
- 48.Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among black, Hispanic, and white Americans: findings from the 2005 U.S. National Alcohol Survey. J Stud Alcohol Drugs. 2008;69(6):824–833. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwartz BS, Glass TA, Bolla KI, et al. Disparities in cognitive functioning by race/ethnicity in the Baltimore Memory Study. Environ Health Perspect. 2004;112(3):314–320. doi: 10.1289/ehp.6727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glass TA, Rasmussen MD, Schwartz BS. Neighborhoods and obesity in older adults: the Baltimore Memory Study. Am J Prev Med. 2006;31(6):455–463. doi: 10.1016/j.amepre.2006.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fillenbaum GG. Multidimensional Functional Assessment of Older Adults: The Duke Older Americans Resources and Services Procedures. Hillsdale: L. Erlbaum Associates; 1988. [Google Scholar]
- 52.Helping Patients Who Drink Too Much: A Clinician's Guide. Rockville: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 53.Liang KY, Zieger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- 54.Jones-Webb R, Snowden L, Herd D, Short B, Hannan P. Alcohol-related problems among black, Hispanic and white men: the contribution of neighborhood poverty. J Stud Alcohol. 1997;58(5):539–545. doi: 10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- 55.Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults' outcomes. Soc Sci Med. 2004;59(11):2271–2284. doi: 10.1016/j.socscimed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 56.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. HHS Publication No. SMA 11-4658. Rockville, MD; 2011.
- 57.Massey DS, Gross AB, Shibuya K. Migration, segregation, and the geographic concentration of poverty. Am Sociol Rev. 1994;59(3):425–445. doi: 10.2307/2095942. [DOI] [Google Scholar]
- 58.Kavanagh AM, Kelly MT, Krnjacki L, et al. Access to alcohol outlets and harmful alcohol consumption: a multi-level study in Melbourne, Australia. Addiction. 2011;106(10):1772–1779. doi: 10.1111/j.1360-0443.2011.03510.x. [DOI] [PubMed] [Google Scholar]
- 59.Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol Alcohol. 2009;44(5):500–516. doi: 10.1093/alcalc/agp054. [DOI] [PubMed] [Google Scholar]
- 60.LaVeist TA, Wallace JM., Jr Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51(4):613–617. doi: 10.1016/S0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- 61.Stockwell T, Donath S, Cooper-Stanbury M, Chikritzhs T, Catalano P, Mateo C. Under-reporting of alcohol consumption in household surveys: a comparison of quantity-frequency, graduated-frequency and recent recall. Addiction. 2004;99(8):1024–1033. doi: 10.1111/j.1360-0443.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- 62.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 63.Sampson RJ, Raudenbush SW. Seeing disorder: neighborhood stigma and the social construction of "broken windows". Soc Psychol Q. 2004;67:319–342. doi: 10.1177/019027250406700401. [DOI] [Google Scholar]
- 64.Glass TA, Bandeen-Roche K, McAtee M, Bolla K, Todd AC, Schwartz BS. Neighborhood psychosocial hazards and the association of cumulative lead dose with cognitive function in older adults. Am J Epidemiol. 2009;169(6):683–692. doi: 10.1093/aje/kwn390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Glass TA, Balfour JL. Neighborhoods, aging and functional limitations. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. New York: Oxford University Press; 2003. pp. 303–334. [Google Scholar]
- 66.Kahn H. Destroying Detroit (in order to save it). GQ. May 2011.
- 67.Harcourt BE, Ludwig J. Broken windows: new evidence from New York City and a five-city social experiment. Univ Chic Law Rev. 2006;73:271–320. [Google Scholar]