Abstract
Most data regarding survival in patients with chondrosarcoma are limited to case studies and small series performed at single institutions. A systematic review was performed to study the relationship between proposed prognostic factors and survival. Every study published in the English literature was reviewed. The mortality rates in these patients were analyzed according to modality of treatment, treatment history, histological subtype, and histological grade. A total of 560 patients with cranial chondrosarcoma were analyzed. Median follow-up time was 60 months. The 5-year mortality among all patients was 11.5% with median survival of 24 months. Mortality at 5 years was significantly greater for patients with tumors of higher grade or of the mesenchymal subtype, or had received surgical resection alone, when compared to their respective counterparts. The results of our systematic review provide useful data in predicting survival among cranial chondrosarcoma patients.
Keywords: Cranial chondrosarcoma, Survival outcomes, Systematic review
1. Introduction
Chondrosarcoma accounts for 6% of skull base neoplasms and 0.15% of all intracranial tumors 1. They are subclassified into the conventional (hyaline/myxoid), dedifferentiated, clear cell, and mesenchymal subtypes 2. In accordance with the current literature, the conventional type of chondrosarcoma is the most common cartilage tumor to develop in the skull base 3. Conventional chondrosarcoma is composed of either hyaline cartilage, myxoid cartilage or a combination of both of these matrices. The hyaline subtype is characterized by hypercellular hyaline cartilage containing cytologically atypical chondrocytes within lacunae. In contrast, the atypical chondrocytes of the myxoid subtype do not reside in lacunae but instead are enmeshed in a flocculent myxoid matrix. The mesenchymal subtype is known to display a more anaplastic appearance.
The significance of histological subtypes among chondrosarcomas has been reported; however, the prognosis is determined primarily by its World Health Organization (WHO) histological grade. The grading system consists of three categories: grade I (well differentiated), grade II (moderately differentiated) and grade III (poorly differentiated). Although malignant, the biological behavior of these tumors is characterized by potentially fatal progressive enlargement and subsequent compression or invasion of local structures such as the brain and the optic pathway, hence diplopia and headache, the two most common presenting symptoms recorded in these patients. The complete surgical resection of these tumors is most often prevented by their deep location; consequently, a combination of surgery and irradiation has become the mainstay of treatment 4-7. Factors such as pathological pattern, previous treatment (surgery or radiation therapy), degree of tumor resection and adjuvant postoperative radiation therapy have all been implicated in the prognosis of patients with chondrosarcoma.
Although most chondrosarcoma arise de novo, they are common in patients with Ollier’s disease, Maffucci syndrome, Paget’s disease and osteochondroma. One postulated theory for the development of intracranial chondrosarcoma highlights that while the bones of the skull vault develop primarily by intramembranous ossification, the bones of the skull base mature predominantly by endochondral ossification 8. Endochondral ossification is also responsible for the development of several sites in the mature skull including a large part of the petrous portion of the temporal bone, areas of the petro-occipital, spheno-occipital, and spheno-petrosal synchondrosis Intracranial chondrosarcomas might develop from the chondrocytes within rests of endochondral cartilage that may be present in these areas. Others believe that the primitive multifunctional mesenchymal cells involved in the embryogenesis of the skull base and temporal bone may be the source of these tumors. Yet other authors contend that intracranial chondrosarcomas develop from metaplastic mature fibroblasts 9,10.
Presently, there is much literature published on intracranial chondrosarcoma emphasizing the effect of histological subtypes, grading and treatment outcomes in these patients. Despite all these efforts, significant interpractitioner variability of practice approaches still persists, given that most of these studies are case studies, small to modest size case series and frequently from single institutions, and thus lack the statistical power and freedom from single surgeon bias to guide the new individual practictioner along the path of best management in the approach to these patients.
Consequently, we report a comprehensive review of the English language literature to assess survival in patients treated for intracranial chondrosarcoma and stress the relationship between the proposed prognostic factors and survival.
2.Methods
2.1. Article selection
Articles were identified via a Pub Med search using the key phrases “cranial chondrosarcoma,” “clival chondrosarcoma,” “skull base chondrosarcoma,” “intracranial chondrosarcoma” alone and in combination with “survival” as Boolean searches. An extensive review of cited references was performed.
Inclusion criteria were that: (i) all patients had to have follow-up data available; and (ii) articles had to have enough information for the data from each patient to be completely disaggregated.
Exclusion criteria were: (i) all articles that combined patient outcomes of chondrosarcoma and chordoma were excluded, unless there was a clear distinction between the two separate groups of patients; (ii) all chondrosarcomas originating from the head and neck were excluded; and (iii) all patients with Ollier’s disease, Maffucci syndrome (enchondroma with multiple angiomas), Paget’s disease, and osteochondroma were excluded from our analysis.
2.2. Data Extraction
Our search resulted in over 2,000 patients treated for cranial chondrosarcoma. Of these, 630 patients were completely disaggregated. Of these data for 630 patients, 560 received appropriate follow-up. All these studies were completely disaggregated and all references for these articles were further scrutinized to ensure the non-duplication of patients and the completion of a thorough and comprehensive review of the English literature.
Where patients had more than one treatment for recurrence, only the initial treatment was considered. Where the histology was confirmed without any specifications patients were classified as conventional chondrosarcoma. The age recorded for patients with recurrence was the age at first presentation.
Data were analyzed as a whole and stratified into 4 groups. The first analysis divided the data into 2 groups according to patient treatment: patients undergoing surgery only; and patients who received surgery combined with postoperative adjuvant radiation treatment. A second stratification divided data based on treatment history into 2 groups: group 1 comprised patients who had received previous treatment; and group 2, patients who were being treated for the first time. A third analysis divided patients into 2 groups based on histological subtypes: group 1 included those chondrosarcomas with conventional histology; and group 2 represented the mesenchymal subtype. The final analysis stratified the data into 3 groups according to histological grading: grade I; grade II; and grade III with each grade comprising one group.
2.3. Statistical analysis
A Pearson chi-Squared (χ2) test was used for the statistical evaluation of the data. The p value was considered significant at the 5% (0.05) level.
3. Results
A total of 560 non-duplicated chondrosarcoma patients met the inclusion criteria for this systematic review 1,11-108. The overall 5-year mortality rate among all patients was 11.4% (64 patients) with an average survival time of 53.7 months (median, 24 months). Most of the chondrosarcomas in our study involved the clivus (32%), while the second most common location was the temporo-occipital junction (27%). The most common presenting symptom was diplopia (11%), closely followed by headache (9%). Some cases in these articles were eliminated from the analysis for reasons of missing data, obscure data presentation (e.g. studies that presented chondrosarcoma and chordoma patients grouped together), and yet several others had to be excluded because they were not available in the English literature.
3.1. The Effect of Treatment on Survival
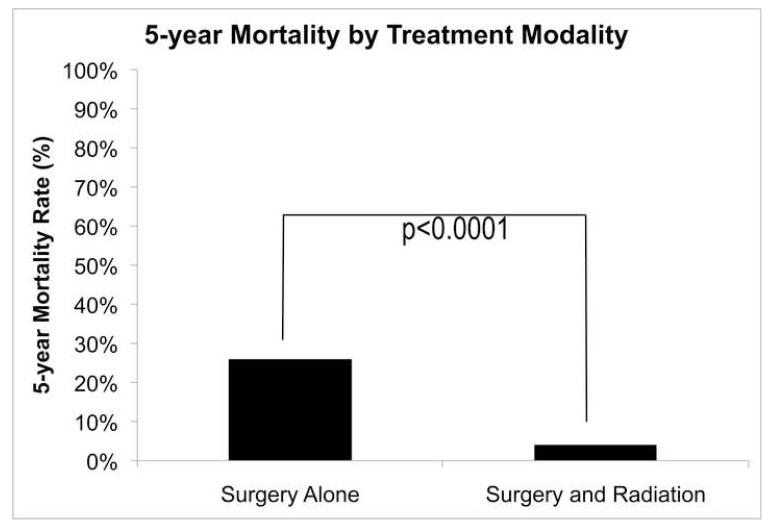
A total of 161 patients had surgery alone, while 325 patients had surgery in addition to postoperative adjuvant radiation therapy. Not surprisingly, the 5-year mortality rate was higher in the group of patients that had surgery alone (25% versus [vs.] 9%, p < 0.0001) (Fig. 1).
Fig. 1.
The effect of treatment on the 5-year mortality rate from chondrosarcoma showing that mortality was higher in patients who had undergone surgery only.
3.2. The Effect of Previous Treatment on Survival
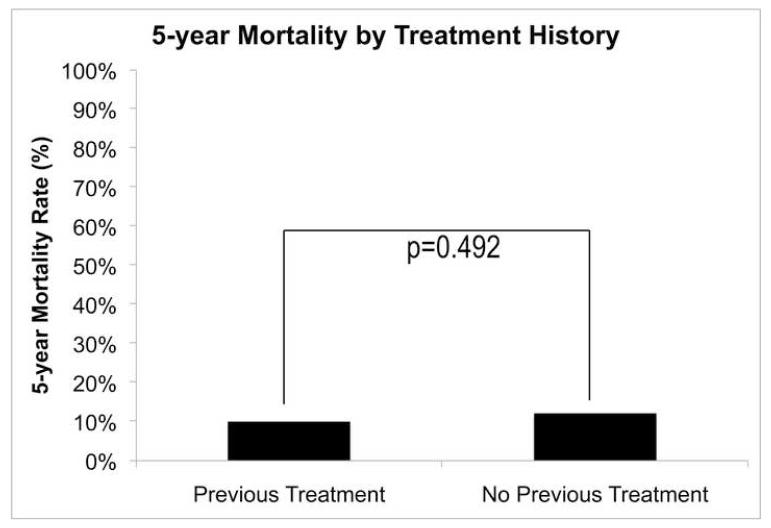
A total of 68 patients received previous treatment, while 492 patients were being treated for the first time. Surprisingly, there was no difference in mortality between these two groups of patients (10% vs. 12%, p = 0.492) (Fig. 2).
Fig. 2.
The effect of previous treatment on the 5-year mortality rate from chondrosarcoma showing that treatment history had no effect.
3.3. The Effect of Histological Subtype on Survival
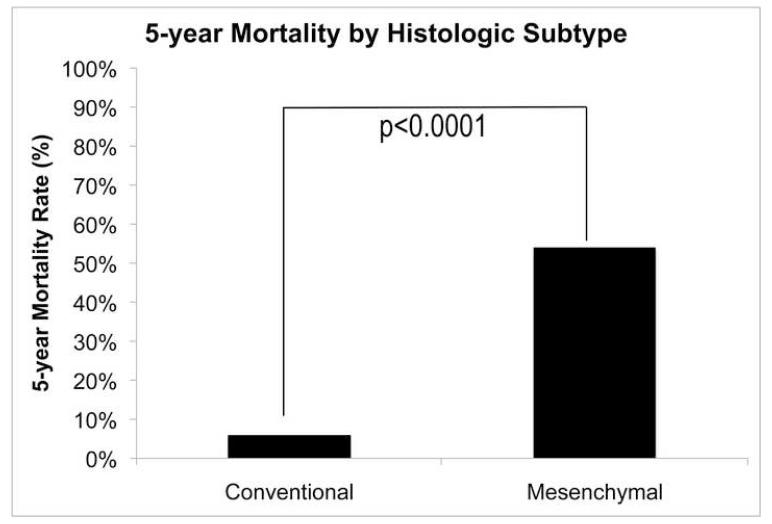
There were a total of 452 patients in our analysis who possessed chondrosarcomas of the conventional subtype, while 60 patients had the mesenchymal subtype. As expected, the mortality rate was lower among patients with the conventional subtype (6% vs. 54%, p < 0.0001) (Fig. 3).
Fig. 3.
The effect of histological subtype on the 5-year mortality rate showing that mortality was lower among patients with the conventional chondrosarcoma subtype.
3.4. The Effect of Histological Grade on Survival
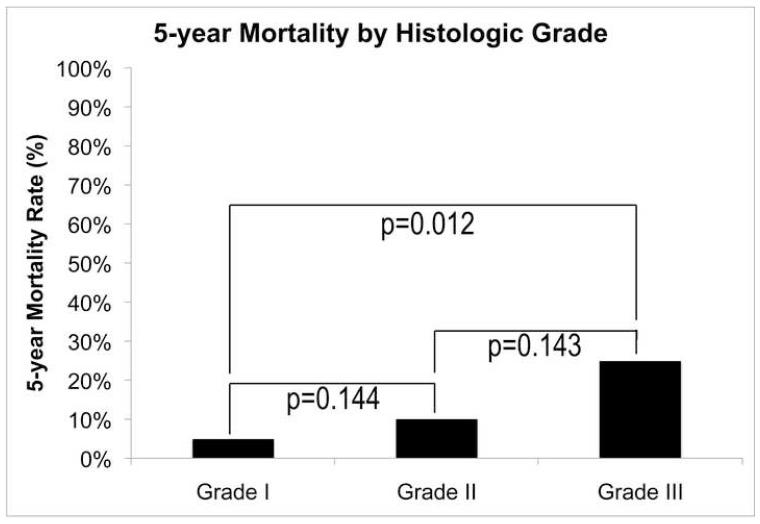
A total of 364 patients had grade I, 80 patients had grade II, and 8 patients had grade III chondrosarcoma. Not surprising, the lowest mortality rate was among the patients with grade I (5%), and the highest mortality rate was observed in the grade III group (25%), with the grade II in the middle with a 10% mortality (5% vs. 10%, p = 0.144; 10% vs. 25%, p = 0.143; 5% vs. 25%, p < 0.012) (Fig. 4).
Fig. 4.
The effect of histological grade on the 5-year mortality rate showing that mortality increased with a corresponding increase in World Health Organization grade (I–III) chondrosarcoma.
4. Discussion
The prognosis of patients with intracranial chondrosarcoma is strongly influenced by several significant factors. These factors include the use of postoperative adjuvant radiation therapy, pathological pattern, previous treatment (surgery or radiation therapy) and extent of tumor removal. However, local recurrence is considered by many to be the most significant predictor of mortality in these patients. For this reason, the review of literature on this topic reveals a large number of publications put forth by many different observers, but there have been few if any efforts to combine this research to achieve the statistical power needed to determine the appropriate methods to manage these tumors. In this study we performed a meta-analysis of survival in a large population of patients who has undergone treatment for intracranial chondrosarcomas.
The overall 5-year mortality among patients in our study was 11%, with an average survival time of 53.7 months (median, 24 months). This percentage was almost identical to those quoted in the literature For instance, Oghalai et al.109 in his study involving 33 patients with skull base chondrosarcomas had an overall mortality of 15%. The high survival rate among these patients was even further emphasized by Colli and Al-Mefty110 and by Oghalai et al. 109 on two separate occasions who revealed 5-year survival rates of 100% and 85%, respectively. . For comparison, the survival for chondrosarcoma that is remote from the cranium, such as the spine, is about 41% 111,112
Our study found that chondrosarcoma patients treated with surgery alone demonstrated a 5-year mortality rate of 26%, while the implementation of postoperative adjuvant radiation therapy reduced this mortality rate dramatically to 4%. These numbers were not surprising because many recent studies have stated, without reservation, that meticulous surgical resection together with postoperative radiotherapy provides the best long-term outcomes for these patients. One such study by Isaacson et al. 113 in 2007 clearly states that radiation therapy is an important adjunctive therapy in the management of chondrosarcomas; a study by Neff et al. 114 in 2002 asserts that postoperative radiation therapy may be beneficial in these patients.
Nonetheless, the epitome of the idea regarding high survival and low mortality in chondrosarcoma patients is a study managed by Rosenberg et al. 115 in 1999. This is the largest study, to date, on chondrosarcoma of the skull base in which treatment was carried out at a single institution. This study consists of 200 patients and quotes 5-year and 10-year disease-specific survival rates of both 99%, when surgery is combined with high-dose fractionated proton beam radiation. Although our survival rate (89%) is slightly lower than theirs, this can most likely be attributed to the combination of all the different type of radiation therapy into one large group to maximize the statistical power in our study. In our study, the history of previous treatment did not prove to be a significant indicator of mortality. This coincides with a study done in 2005, which also did not find any correlation between patients undergoing previous treatments and mortality 109. On the contrary, Tzortzidis et al. 116 revealed in 2006, that patients who required multiple operations had a diminished disease-free survival.
The four major subtypes of histological classification are: conventional, mesenchymal, clear cell and dedifferentiated. The review of literature revealed no clear cell or dedifferentiated subtypes occurring intracranially. Consequently, our analysis included only the mesenchymal and conventional subtypes. In our study, those patients possessing chondrosarcomas of the conventional subtype had a 6% 5-year mortality, while those chondrosarcoma demonstrating the mesenchymal subtype carried a much higher mortality rate of 54%. This was expected since the mesenchymal subtype indicated worse clinical behavior and poorer prognosis than conventional histology according to Oikawa et al. 117 Furthermore, according to Koch et al. 2000118, labeled mesenchymal histology as well as grade of the tumor were cardinal factors that portends a poor prognosis. This grading system is important because it reflects prognosis based on tumor biology distinct from its location or stage of presentation 114. Evans et al. 119 reported five-year survival rates of chondrosarcomas grade I, II, and III to be 90%, 81%, and 43%, respectively. Our study demonstrated 5-year survival rates of 95%, 90%, and 75% for grades I, II, and III, respectively. In comparison, chordomas, another intracranial skull base tumor, do not appear to have histology as a signifigant prognostic factor, but for chordoma, age might be an important variable in survival 110,120-124.
Although adjuvant radiation therapy appears to reduce the mortality rate of chondrosarcomas, further investigations into the usefulness of adjuvant therapy for low-grade chondrosarcomas must be performed. It is possible that low-grade chondrosarcomas have good survival prognosis with surgery alone and be better served with resection without immediate radiotherapy or with delayed adjuvant radiation.
The wide heterogeneity of the articles included in our systematic review precluded us from further stratification and analysis. Prospective studies could be designed to further investigate survival after treatment for intracranial chondrosarcoma. Inconsistently assessed and reported variables cannot be analyzed with regression and is problematic with the heterogeneic nature of the reported literature. Aggregated systematic reviews may help to identify important prognostic factors and clinically relevant indicators for survival 125,126. There are, although, several inherent limitations with systematic reviews 127. One clear limitation is that the systematic data is only as good as its composite studies, and may inherently reflect source study biases. However, the large number of patients in our analytic review helps to mitigate the biases and dilutes the inherent error of any particular article.
In conclusion, we report our results from a comprehensive systematic review of the English language literature regarding survival among cranial chondrosarcoma patients. It is our hope that by using such a substantially large data set we are able to minimize the effect of individual surgeons and the bias of any individual institution on the outcome of these patients and thereby create a more objective protocol for clinicians managing these patients.
Acknowledgement
The authors gratefully acknowledge the following sources of support: Howard Hughes Medical Institute Research Training Fellowship – SJH, National Research Service Award – IY, Khatib Endowed Chair – ATP
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cianfriglia F, Pompili A, Occhipinti E. Intracranial malignant cartilaginous tumours. Report of two cases and review of literature. Acta Neurochir (Wien) 1978;45:163–175. doi: 10.1007/BF01774391. [DOI] [PubMed] [Google Scholar]
- 2.Dorfman H. Mosby; Bone Tumors. St. Louis: 1998. [Google Scholar]
- 3.Korten AG, ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 1998;65(1):88–92. doi: 10.1136/jnnp.65.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Austin-Seymour M, Munzenrider J, Goitein M, et al. Fractionated proton radiation therapy of chordoma and low-grade chondrosarcoma of the base of the skull. J Neurosurg. 1989;70(1):13–17. doi: 10.3171/jns.1989.70.1.0013. [DOI] [PubMed] [Google Scholar]
- 5.Gay E, Sekhar LN, Rubinstein E, et al. Chordomas and chondrosarcomas of the cranial base: results and follow-up of 60 patients. Neurosurgery. 1995;36(5):887–896. doi: 10.1227/00006123-199505000-00001. discussion 896-887. [DOI] [PubMed] [Google Scholar]
- 6.Sen CN, Sekhar LN, Schramm VL, Janecka IP. Chordoma and chondrosarcoma of the cranial base: an 8-year experience. Neurosurgery. 1989;25(6):931–940. doi: 10.1097/00006123-198912000-00013. discussion 940-931. [DOI] [PubMed] [Google Scholar]
- 7.Stapleton SR, Wilkins PR, Archer DJ, Uttley D. Chondrosarcoma of the skull base: a series of eight cases. Neurosurgery. 1993;32(3):348–355. doi: 10.1227/00006123-199303000-00003. discussion 355-346. [DOI] [PubMed] [Google Scholar]
- 8.Lau DP, Wharton SB, Antoun NM, Bottrill ID, Moffat DA. Chondrosarcoma of the petrous apex. Dilemmas in diagnosis and treatment. J Laryngol Otol. 1997;111(4):368–371. doi: 10.1017/s002221510013734x. [DOI] [PubMed] [Google Scholar]
- 9.Coltrera MD, Googe PB, Harrist TJ, et al. Chondrosarcoma of the temporal bone. Diagnosis and treatment of 13 cases and review of the literature. Cancer. 1986;58(12):2689–2696. doi: 10.1002/1097-0142(19861215)58:12<2689::aid-cncr2820581224>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 10.Seidman MD, Nichols RD, Raju UB, Mehta B, Levy HG. Extracranial skull base chondrosarcoma. Ear Nose Throat J. 1989;68(8):626–632. 635. [PubMed] [Google Scholar]
- 11.Baehring J, Piepmeier J, Duncan C, Ogle E, Kim J, Liebsch N. Chondrosarcoma of the skull base. J Neurooncol. 2006;76(1):49. doi: 10.1007/s11060-005-5981-3. [DOI] [PubMed] [Google Scholar]
- 12.Seth H, Singh M. Intracranial mesenchymal chondrosarcoma. Acta Neuropathol. 1973;24(1):86–89. doi: 10.1007/BF00691422. [DOI] [PubMed] [Google Scholar]
- 13.Wojno K, Hruban RH, Garin-Chesa P, Huvos AG. Chondroid chordomas and low-grade chondrosarcomas of the craniospinal axis. An immunohistochemical analysis of 17 cases. Am J Surg Pathol. 1992;16(12):1144–1152. doi: 10.1097/00000478-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Masuzawa T, Nakahara N, Saito K, Sato F. Parasellar chondrosarcoma - case report. Neurol Med Chir. 1986;26(1):44–48. doi: 10.2176/nmc.26.44. [DOI] [PubMed] [Google Scholar]
- 15.Hassounah M, Al-Mefty O, Akhtar M, Jinkins JR, Fox JL. Primary cranial and intracranial chondrosarcoma. A survey. Acta Neurochir. 1985;78(3-4):123–132. doi: 10.1007/BF01808691. [DOI] [PubMed] [Google Scholar]
- 16.Bahr A, Gayler BW. Cranial chondrosarcoma. Report of four cases and review of the literature. Radiology. 1977;124(1):151–156. doi: 10.1148/124.1.151. [DOI] [PubMed] [Google Scholar]
- 17.Frank G, Sciarretta V, Calbucci F, Farneti G, Mazzatenta D, Pasquini E. The endoscopic transnasal transsphenoidal approach for the treatment of cranial base chordomas and chondrosarcomas. Neurosurgery. 2006;59(1):ONS50–57. doi: 10.1227/01.NEU.0000219914.17221.55. [DOI] [PubMed] [Google Scholar]
- 18.Lin E, Ray ME, Telian SA. Cochlear implantation with ipsilateral petroclival chondrosarcoma. Otol Neurotol. 2006;27(3):337–341. doi: 10.1097/00129492-200604000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Wanebo J, Bristol RE, Porter RR, Coons SW, Spetzler RF. Management of cranial base chondrosarcoma. Neurosurgery. 2006;58(2):249–255. doi: 10.1227/01.NEU.0000194834.74873.FB. [DOI] [PubMed] [Google Scholar]
- 20.Inenaga C, Morii K, Tamura T, Tanaka R, Takahashi H. Mesenchymal chondrosarcoma of the sellar region. Acta Neurochir (Wien) 2003;145(7):593–597. doi: 10.1007/s00701-003-0059-5. [DOI] [PubMed] [Google Scholar]
- 21.Neff B, Sataloff RT, Storey L, Hawkshaw M, Spiegel JR. Chondrosarcoma of the skull base. Laryngoscope. 2002;112(1):134–139. doi: 10.1097/00005537-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Crockard H, Cheeseman A, Steel T, Revesz T, Holton JL, Plowman N, Singh A, Crossman J. A multidisciplinary team approach to skull base chondrosarcomas. Journal of Neurosurgery. 2001;9(2):184–189. doi: 10.3171/jns.2001.95.2.0184. [DOI] [PubMed] [Google Scholar]
- 23.Amirjamshidi A, Abbassioun K. Radiation-induced tumors of the central nervous system occuring in childhood and adolescence. Four unusual lesions in three patients and a review of the literature. Childs Nerv Syst. 2000;16(7):390–397. doi: 10.1007/s003819900125. [DOI] [PubMed] [Google Scholar]
- 24.Korten A, ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 1998;65(1):88–92. doi: 10.1136/jnnp.65.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blevins N, Jackler RK, Kaplan MJ, Gutin PH. Combined transpetrosal-subtemporal craniotomy for clival tumors with extension into the posterior fossa. Laryngoscope. 1995;105(9 Pt 1):975–982. doi: 10.1288/00005537-199509000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Yoshimoto T, Sawamura Y, Ikeda J, Ishii N, Abe H. Successful chemoradiation therapy for high-grade skull base chondrosarcoma in a child. Childs Nerv Syst. 1995;11(4):250–253. doi: 10.1007/BF00277662. [DOI] [PubMed] [Google Scholar]
- 27.Reid C, Fagan PA, Turner J. Low-grade myxoid chondrosarcoma of the temporal bone: differential diagnosis and report of two cases. Am J Otol. 1994;15(3):419–422. [PubMed] [Google Scholar]
- 28.Stapleton S, Wilkins PR, Archer DJ, Uttley D. Chondrosarcoma of the skull base: a series of eight cases. Neurosurgery. 1993;32(3):348–355. doi: 10.1227/00006123-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Eavey R, Janfaza P, Chapman PH, Swearingen B, Liebsch N, Weber A, Davis KR, Ferguson WS. Skull base dumbbell tumor: surgical experience with two adolescents. Ann Otol Rhinol Laryngol. 1992;101(11):939–945. doi: 10.1177/000348949210101110. [DOI] [PubMed] [Google Scholar]
- 30.Colak A, Berker M, Saglam S, Onol B. Chondrosarcoma of the temporal bone in an infant: case report and review of the literature. Neurosurgery. 1992;31(5):956–957. [PubMed] [Google Scholar]
- 31.Morimoto T, Sasaki T, Takakura K, Ishida T. Chondrosarcoma of the skull base: report of six cases. Skull Base Surg. 1992;2(4):177–185. doi: 10.1055/s-2008-1057131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shotton J, Kuhwoede R, Fisch U. Mesenchymal tumors of the skull base with particular reference to surgical management and outcome. Skull Base Surg. 1992;2(2):112–117. doi: 10.1055/s-2008-1057120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kondziolka D, Lunsford LD, Flickinger JC. The role of radiosurgery in the management of chordoma and chondrosarcoma of the cranial base. Neurosurgery. 1991;29(1):38–45. doi: 10.1097/00006123-199107000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Miyamori T, Mizukoshi H, Yamano K, Takayanagi N, Sugino M, Hayase H, Ito H. Intracranial chondrosarcoma - case report. Neurol Med Chir. 1990;30(4):263–267. doi: 10.2176/nmc.30.263. [DOI] [PubMed] [Google Scholar]
- 35.Charabi S, Engel P, Bonding P. Myxoid tumours in the temporal bone. J Laryngol Otol. 1989;103(12):1206–1209. doi: 10.1017/s0022215100111351. [DOI] [PubMed] [Google Scholar]
- 36.Sen C, Sekhar LN, Schramm VL, Janecka IP. Chordoma and chondrosarcoma of the cranial base: an 8-year experience. Neurosurgery. 1989;25(6):931–940. doi: 10.1097/00006123-198912000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Oguro K, Nakahara N, Yamaguchi Y, Shimabukuro H, Masuzawa T. Chondrosarcoma of the posterior fossa - case report. Neurol Med Chir. 1989;29(11):1030–1038. doi: 10.2176/nmc.29.1030. [DOI] [PubMed] [Google Scholar]
- 38.Seidman M, Nichols RD, Raju UB, Mehta B, Levy HG. Extracranial skull base chondrosarcoma. Ear Nose Throat J. 1989;68(8):626–632. [PubMed] [Google Scholar]
- 39.Coltrera M, Googe PB, Harrist TJ, Hyams VJ, Schiller AL, Goodman ML. Chondrosarcoma of the temporal bone. Diagnosis and treatment of 13 cases and review of the literature. Cancer. 1986;58(12):2689–2696. doi: 10.1002/1097-0142(19861215)58:12<2689::aid-cncr2820581224>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 40.Kveton J, Brackmann DE, Glasscock ME, 3rd, House WF, Hitselberger WE. Chondrosarcoma of the skull base. Otolaryngol Head Neck Surg. 1986;94(1):23–32. doi: 10.1177/019459988609400104. [DOI] [PubMed] [Google Scholar]
- 41.Adegbite A, McQueen JD, Paine KW, Rozdilsky B. Primary intracranial chondrosarcoma: a report of two cases. Neurosurgery. 1985;17(3):490–494. doi: 10.1227/00006123-198509000-00017. [DOI] [PubMed] [Google Scholar]
- 42.Kubota T, Yamamoto S, Hirano A, Murata H. Chondrosarcoma in the optic canal - a case report with ultrastructural study. Neurol Med Chir. 1985;25(1):36–41. doi: 10.2176/nmc.25.36. [DOI] [PubMed] [Google Scholar]
- 43.Chandler J, Yashar P, Laskin WB, Russell EJ. Intracranial chondrosarcoma: a case report and review of the literature. J Neurooncol. 2004;68(1):33–39. doi: 10.1023/b:neon.0000024728.72998.7d. [DOI] [PubMed] [Google Scholar]
- 44.Mashman L, Gunasekera L, Rose PE, Olney JS. Primary intracerebral mesenchymal chondrosarcoma with rhabdomyosarcomatous differentiation: case report and literature review. Br J Neurosurg. 2001;15(5):419–424. doi: 10.1080/02688690120082431. [DOI] [PubMed] [Google Scholar]
- 45.Rapidis A, Archondakis G, Anteriotis D, Skouteris CA. Chondrosarcomas of the skull base: review of the literature and report of two cases. J Craniomaxillofac Surg. 1997;25(6):322–327. doi: 10.1016/s1010-5182(97)80034-0. [DOI] [PubMed] [Google Scholar]
- 46.Volpe N, Lessell S. Remitting sixth nerve palsy in skull base tumors. Arch Ophthalmol. 1993;111(10):1391–1395. doi: 10.1001/archopht.1993.01090100099035. [DOI] [PubMed] [Google Scholar]
- 47.Aksoy S, Abali H, Kilickap S, Guler N. Successful treatment of a chemoresistant tumor with temozolomide in an adult patient: report of a recurrent intracranial mesenchymal chondrosarcoma. J Neurooncol. 2005;71(3):333–334. doi: 10.1007/s11060-004-1725-z. [DOI] [PubMed] [Google Scholar]
- 48.Gonzales-Lois C, Cuevas C, Abdullah O, Ricoy JR. Intracranial extraskeletal myxoid chondrosarcoma: case report and review of the literature. Acta Neurochir (Wien) 2002;144(7):735–740. doi: 10.1007/s00701-002-0949-y. [DOI] [PubMed] [Google Scholar]
- 49.Oruckaptan H, Berker M, Soylemezoglu F, Ozcan OE. Parafalcine chondrosarcoma: an unusual localization for a classical variant. Case report and review of the literature. Surg Neurol. 2001;55(3):174–179. doi: 10.1016/s0090-3019(01)00329-9. [DOI] [PubMed] [Google Scholar]
- 50.Crosswell H, Buchino JJ, Sweetman R, Reisner A. Intracranial mesenchymal chondrosarcoma in an infant. Med Pediatr Oncol. 2000;34(5):370–374. doi: 10.1002/(sici)1096-911x(200005)34:5<370::aid-mpo14>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 51.Salcman M, Scholtz H, Kristt D, Numaguchi Y. Extraskeletal myxoid chondrosarcom of the falx. Neurosurgery. 1992;31(2):344–348. doi: 10.1227/00006123-199208000-00021. [DOI] [PubMed] [Google Scholar]
- 52.Pages A, Pages M, Ramos J, Benezech J. Radiation-induced intracranial fibrochondrosarcoma. J Neurol. 1986;233(5):309–310. doi: 10.1007/BF00314165. [DOI] [PubMed] [Google Scholar]
- 53.Cybulski G, Russell EJ, D’Angelo CM, Bailey OT. Falcine chondrosarcoma: case report and literature review. Neurosurgery. 1985;16(3):412–415. doi: 10.1227/00006123-198503000-00024. [DOI] [PubMed] [Google Scholar]
- 54.Rodda R, Franklin CI. Intracranial meningeal chondrosarcoma - probably mesenchymal type. Aust N Z J Surg. 1984;54(4):387–390. [PubMed] [Google Scholar]
- 55.Bernstein M, Perrin RG, Platts ME, Simpson WJ. Radiation-induced cerebellar chondrosarcoma. Case report. Journal of Neurosurgery. 1984;61(1):174–177. doi: 10.3171/jns.1984.61.1.0174. [DOI] [PubMed] [Google Scholar]
- 56.Kubota T, Hayashi M, Yamamoto S. Primary intracranial mesenchymal chondrosarcoma: case report with review of the literature. Neurosurgery. 1982;10(1):105–110. [PubMed] [Google Scholar]
- 57.Wu W, Lapi A. Primary non-skeletal intracranial cartilaginous neoplasms: report of a chondroma and a mesenchymal chondrosarcoma. J Neurol Neurosurg Psychiatry. 1970;33(4):469–475. doi: 10.1136/jnnp.33.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lotts S, Bordley JE. A radiosensitive chondrosarcoma of the sphenoid sinus and base of the skull. Report of a case. Laryngoscope. 1972;82(1):57–60. doi: 10.1002/lary.5540820109. [DOI] [PubMed] [Google Scholar]
- 59.Arlen M, Tollefsen HR, Huvos AG, Marcove RC. Chondrosarcoma of the head and neck. Am J Surg. 1970;120(4):456–460. doi: 10.1016/s0002-9610(70)80006-x. [DOI] [PubMed] [Google Scholar]
- 60.Minagi H, Newton TH. Cartilaginous tumors of the base of skull. Am J Roentgenol Radium Ther Nucl Med. 1969;105(2):308–313. doi: 10.2214/ajr.105.2.308. [DOI] [PubMed] [Google Scholar]
- 61.George B, Ferrario CA, Blanquet A, Kolb F. Cavernous sinus exenteration for invasive cranial base tumors. Neurosurgery. 2003;52(4):772–780. doi: 10.1227/01.neu.0000053364.33375.c2. [DOI] [PubMed] [Google Scholar]
- 62.Lalwani A, Kaplan MJ, Gutin PH. The transsphenoethmoid approach to the sphenoid sinus and clivus. Neurosurgery. 1992;31(6):1008–1014. doi: 10.1227/00006123-199212000-00004. [DOI] [PubMed] [Google Scholar]
- 63.Leedham P, Swash M. Chondrosarcoma with subarachnoid dissemination. J Pathol. 1972;107(1):59–61. doi: 10.1002/path.1711070111. [DOI] [PubMed] [Google Scholar]
- 64.Debus J, Schulz-Ertner D, Schad L, Essig M, Rhein B, Thillmann CO, Wannenmacher M. Sterotactic fractionated radiotherapy for chordomas and chondrosarcomas of the skull base. Int J Radiat Oncol Biol Phys. 2000;47(3):591–596. doi: 10.1016/s0360-3016(00)00464-8. [DOI] [PubMed] [Google Scholar]
- 65.Hug E, Loredo LN, Slater JD, DeVries A, Grove RI, Schaefer RA, Rosenberg AE, Slater JM. Proton radiation therapy for chordomas and chondrosarcomas of the skull base. Journal of Neurosurgery. 1999;91(3):432–439. doi: 10.3171/jns.1999.91.3.0432. [DOI] [PubMed] [Google Scholar]
- 66.Austin J, Urie MM, Cardenosa G, Munzenrider JE. Probably causes of recurrence in patients with chordoma and chondrosarcoma of the base of skull and cervical spine. Int J Radiat Oncol Biol Phys. 1993;25(3):439–444. doi: 10.1016/0360-3016(93)90065-4. [DOI] [PubMed] [Google Scholar]
- 67.Suit H, Goitein M, Munzenrider J, Verhey L, Davis KR, Koehler A, Linggood R, Ojemann RG. Definitive radiation therapy for chordoma and chondrosarcoma of base of skull and cervical spine. Journal of Neurosurgery. 1982;56(3):377–385. doi: 10.3171/jns.1982.56.3.0377. [DOI] [PubMed] [Google Scholar]
- 68.Lustig L, Sciubba J, Holliday MJ. Chondrosarcomas of the skull base and temporal bone. J Laryngol Otol. 2007;121(8):725–735. doi: 10.1017/S0022215107006081. [DOI] [PubMed] [Google Scholar]
- 69.Brackmann D, Teufert KB. Chondrosarcoma of the skull base: long-term follow-up. Otol Neurotol. 2006;27(7):981–991. doi: 10.1097/01.mao.0000233812.48800.b4. [DOI] [PubMed] [Google Scholar]
- 70.Raghu M, Moumoulidis I, De R, Moffat D. Chondrosarcomas of the temporal bone: presentation and management. J Laryngol Otol. 2004;118(7):551–555. doi: 10.1258/0022215041615272. [DOI] [PubMed] [Google Scholar]
- 71.Satyarthee G, Mahapatra AK. Unusual presentation of petro-clival chondrosarcoma: short report. J Clin Neurosci. 2004;11(5):539–542. doi: 10.1016/j.jocn.2003.07.009. [DOI] [PubMed] [Google Scholar]
- 72.Im S, Kim DG, Park IA, Chi JG. Primary intracranial myxoid chondrosarcoma: report of a case and review of the literature. J Korean Med Sci. 2003;18(2):301–307. doi: 10.3346/jkms.2003.18.2.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allan C, Kaltsas G, Evanson J, Geddes J, Lowe DG, Plowman PN, Grossman AB. Pituitary chondrosarcoma: an unusual cause of a sellar mass presenting as a pituitary adenoma. J Clin Endocrinol Metab. 2001;86(1):386–391. doi: 10.1210/jcem.86.1.7111. [DOI] [PubMed] [Google Scholar]
- 74.Oikawa H, Satoh T, Masuda T, Arai H, Ehara S, Muro-Oka G. Intracranial low-grade chondrosarcoma with hyperostosis of the skull: a case report. J Neurooncol. 2000;49(3):249–254. doi: 10.1023/a:1006498209279. [DOI] [PubMed] [Google Scholar]
- 75.La Rocca R, Morgan KW, Paris K, Baeker TR. Recurrent chondrosarcoma of the cranial base: a durable response to ifosfamide-doxorubicin chemotherapy. J Neurooncol. 1999;41(3):281–283. doi: 10.1023/a:1006154904014. [DOI] [PubMed] [Google Scholar]
- 76.Megerian C, Chiocca EA, McKenna MJ, Harsh GF, 4th, Ojemann RG. The subtemporaltranspetrous appraoch for excision of petroclival tumors. Am J Otol. 1996;17(5):773–779. [PubMed] [Google Scholar]
- 77.Kletzker G, Smith PG, McIntire LD, Leonetti JP. Presentation and management of uncommon lesions of the middle ear. Am J Otol. 1995;16(5):634–642. [PubMed] [Google Scholar]
- 78.Sepehrnia A, Samii M, Tatagiba M. Management of intracavernous tumours: an 11-year experience. Acta Neurochir Suppl (Wien) 1991;53:122–126. doi: 10.1007/978-3-7091-9183-5_21. [DOI] [PubMed] [Google Scholar]
- 79.Sekhar L, Schramm VL, Jr, Jones NF. Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. Journal of Neurosurgery. 1987;67(4):488–499. doi: 10.3171/jns.1987.67.4.0488. [DOI] [PubMed] [Google Scholar]
- 80.Sekhar L, Moller AR. Operative management of tumors involving the cavernous sinus. Journal of Neurosurgery. 1986;64(6):879–889. doi: 10.3171/jns.1986.64.6.0879. [DOI] [PubMed] [Google Scholar]
- 81.Schulz-Ertner D, Nikoghosyan A, Hof H, Didinger B, Combs SE, Jakel O, Karger CP, Edler L, Debus J. Carbon ion radiotherapy of skull base chondrosarcomas. Int J Radiat Oncol Biol Phys. 2007;67(1):171–177. doi: 10.1016/j.ijrobp.2006.08.027. [DOI] [PubMed] [Google Scholar]
- 82.Rosenberg A, Nielsen GP, Keel SB, Renard LG, Fitzek MM, Munzenrider JE, Liebsch NJ. Chondrosarcoma of the base of the skull: a clinicopathologic study of 200 cases with emphasis on its distinction from chordoma. Am J Surg Pathol. 1999;23(11):1370–1378. doi: 10.1097/00000478-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 83.Gerszeten P, Pollack IF, Hamilton RL. Primary parafalcine chondrosarcoma in a child. Acta Neuropathol. 1998;95(1):111–114. doi: 10.1007/s004010050773. [DOI] [PubMed] [Google Scholar]
- 84.Harvey S, Wiet RJ, Kazan R. Chondrosarcoma of the jugular foramen. Am J Otol. 1994;15(2):257–263. [PubMed] [Google Scholar]
- 85.Stenstam B, Pellettieri L, Sorteberg W, Rezaei A, Skold K. BNCT for recurrent intracranial meningeal tumours - case reports. Acta Neurol Scand. 2007;115(4):243–247. doi: 10.1111/j.1600-0404.2006.00776.x. [DOI] [PubMed] [Google Scholar]
- 86.Bingaman K, Alleyne CH, Jr, Olson JJ. Intracranial extraskeletal mesenchymal chondrosarcoma: case report. Neurosurgery. 2000;46(1):207–211. [PubMed] [Google Scholar]
- 87.el-Gindi S, Abd-el-Hafeez M, Salama M. Extracranial skeletal metastases from an intracranial meningeal chondrosarcoma. Case report. Journal of Neurosurgery. 1974;40(5):651–653. doi: 10.3171/jns.1974.40.5.0651. [DOI] [PubMed] [Google Scholar]
- 88.Waga S, Matsushima M, Ando K, Morii S. Intracranial chondrosarcoma with extracranial metastases. Case report. Journal of Neurosurgery. 1972;36(6):790–794. doi: 10.3171/jns.1972.36.6.0790. [DOI] [PubMed] [Google Scholar]
- 89.Kretzschmar H, Eggert HR. Mesenchymal chondrosarcoma of the craniocervical junction. Clin Neurol Neurosurg. 1990;92(4):343–347. doi: 10.1016/0303-8467(90)90062-a. [DOI] [PubMed] [Google Scholar]
- 90.La Spina M, Dollo C, Giangaspero F, Bertolini P, Russo G. Intracranial mesenchymal chondrosarcoma with osteoid formation: report of a pediatric case. Childs Nerv Syst. 2003;19(9):680–682. doi: 10.1007/s00381-003-0727-z. [DOI] [PubMed] [Google Scholar]
- 91.Ruark D, Schlehaider UK, Shah JP. Chondrosarcoma of the head and neck. World J Surg. 1992;16(5):1010–1015. doi: 10.1007/BF02067021. [DOI] [PubMed] [Google Scholar]
- 92.Feiz-Erfan I, Han PP, Spetzler RF, Porter RW, Klopfenstein JD, Ferreira MA, Beals SP, Joganic EF. Exposure to midline cranial base without a facial incision through a combined craniofacial-transfacial procedure. Neurosurgery. 2005;56(1 Suppl):28–35. doi: 10.1227/01.neu.0000144209.03703.c6. [DOI] [PubMed] [Google Scholar]
- 93.Finn D, Goepfert H, Batsakis JG. Chondrosarcoma of the head and neck. Laryngoscope. 1984;94(12 Pt 1):1529–1544. [PubMed] [Google Scholar]
- 94.Jereczek-Fossa B, Krengli M, Orecchia R. Particle beam therapy for head and neck tumors: radiographical basis and clinical experience. Head Neck. 2006;28(8):750–760. doi: 10.1002/hed.20448. [DOI] [PubMed] [Google Scholar]
- 95.Castelnuovo P, Pagella F, Semino L, De Bernardi F, Delu G. Endoscopic treatment of the isolated sphenoid sinus lesions. Eur Arch Otorhinolaryngol. 2005;262(2):142–147. doi: 10.1007/s00405-004-0764-6. [DOI] [PubMed] [Google Scholar]
- 96.Gadwal S, Fanburg-Smith JC, Gannon FH, Thompson LD. Primary chondrosarcoma of the head and neck in pediatric patients: a clinicopathologic study of 14 cases with a review of the literature. Cancer. 2000;88(9):2181–2188. [PubMed] [Google Scholar]
- 97.Berkmen Y, Blatt ES. Cranial and intracranial cartilaginous tumours. Clin Radiol. 1968;19(3):327–333. doi: 10.1016/s0009-9260(68)80019-4. [DOI] [PubMed] [Google Scholar]
- 98.Herskowitz A, el-Gammal T. Supratentorial cartilaginous tumors. (A report of 2 cases) Dis Nerv Syst. 1973;34(7):384–388. [PubMed] [Google Scholar]
- 99.Lau D, Wharton SB, Antoun NM, Bottrill ID, Moffat DA. Chondrosarcoma of the petrous apex. Dilemmas in diagnosis and treatment. J Laryngol Otol. 1997;111(4):368–371. doi: 10.1017/s002221510013734x. [DOI] [PubMed] [Google Scholar]
- 100.Gay I, Elidan J, Kopolovic J. Chondrosarcoma at the skull base. Ann Otol Rhinol Laryngol. 1981;90(1):53–55. doi: 10.1177/000348948109000113. [DOI] [PubMed] [Google Scholar]
- 101.Miller R, Foote RL, Coffey RJ, Gorman DA, Earle JD, Schomberg PJ, Kline RW. The role of stereotactic radiosurgery in the treatment of malignant skull base tumors. Int J Radiat Oncol Biol Phys. 1997;39(5):977–981. doi: 10.1016/s0360-3016(97)00377-5. [DOI] [PubMed] [Google Scholar]
- 102.Boorstein J, Spizarny DL. Case report 476: Chondrosarcoma of base of skull (CBS) Skeletal Radiol. 1988;17(3):208–211. doi: 10.1007/BF00351012. [DOI] [PubMed] [Google Scholar]
- 103.Nokes S, Dauito R, Murtagh FR, Love LC, Arrington JA. Intracranial mesenchymal chondrosarcoma. Am J Neuroradiol. 1987;8(6):1137–1138. [PMC free article] [PubMed] [Google Scholar]
- 104.Labram E, Pobereskin LH, Siraj MU. Intracranial chondrosarcoma. Acta Neurochir. 1997;139(2):156–157. doi: 10.1007/BF02747198. [DOI] [PubMed] [Google Scholar]
- 105.Gentry L, Thompson B, Godersky JC. Trauma to the corpus callosum: MR features. Am J Neuroradiol. 1988;9(6):1129–1138. [PMC free article] [PubMed] [Google Scholar]
- 106.Al-Mefty O, Fox JL, Rifai A, Smith RR. A combined infratemporal and posterior fossa approach for the removal of giant glomus tumors and chondrosarcoma. Surg Neurol. 1987;28(6):423–431. doi: 10.1016/0090-3019(87)90224-2. [DOI] [PubMed] [Google Scholar]
- 107.Shuangshoti S, Kasantikul V. View from beneath - pathology in focus. Primary intracranial mesenchymal chondrosarcoma. J Laryngol Otol. 1989;103(5):545–549. doi: 10.1017/s0022215100156853. [DOI] [PubMed] [Google Scholar]
- 108.Kothary N, Law M, Cha S, Zagzag D. Conventional and perfusion MR imaging of parafalcine chondrosarcoma. Am J Neuroradiol. 2003;24(2):245–248. [PMC free article] [PubMed] [Google Scholar]
- 109.Oghalai JS, Buxbaum JL, Jackler RK, McDermott MW. Skull base chondrosarcoma originating from the petroclival junction. Otol Neurotol. 2005;26(5):1052–1060. doi: 10.1097/01.mao.0000185076.65822.f7. [DOI] [PubMed] [Google Scholar]
- 110.Colli BO, Al-Mefty O. Chordomas of the skull base: follow-up review and prognostic factors. Neurosurg Focus. 2001;10(3):E1. doi: 10.3171/foc.2001.10.3.2. [DOI] [PubMed] [Google Scholar]
- 111.McLoughlin GS, Sciubba DM, Wolinsky JP. Chondroma/Chondrosarcoma of the spine. Neurosurg Clin N Am. 2008;19(1):57–63. doi: 10.1016/j.nec.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 112.Boriani S, De Iure F, Bandiera S, et al. Chondrosarcoma of the mobile spine: report on 22 cases. Spine. 2000;25(7):804–812. doi: 10.1097/00007632-200004010-00008. [DOI] [PubMed] [Google Scholar]
- 113.Isaacson B, Kutz JW, Roland PS. Lesions of the petrous apex: diagnosis and management. Otolaryngol Clin North Am. 2007;40(3):479–519. viii. doi: 10.1016/j.otc.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 114.Neff B, Sataloff RT, Storey L, Hawkshaw M, Spiegel JR. Chondrosarcoma of the skull base. Laryngoscope. 2002;112(1):134–139. doi: 10.1097/00005537-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 115.Rosenberg AE, Nielsen GP, Keel SB, et al. Chondrosarcoma of the base of the skull: a clinicopathologic study of 200 cases with emphasis on its distinction from chordoma. Am J Surg Pathol. 1999;23(11):1370–1378. doi: 10.1097/00000478-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 116.Tzortzidis F, Elahi F, Wright DC, et al. Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chondrosarcomas. Neurosurgery. 2006;58(6):1090–1098. doi: 10.1227/01.NEU.0000215892.65663.54. discussion 1090-1098. [DOI] [PubMed] [Google Scholar]
- 117.Oikawa H, Satoh T, Masuda T, et al. Intracranial low-grade chondrosarcoma with hyperostosis of the skull: a case report. J Neurooncol. 2000;49(3):249–254. doi: 10.1023/a:1006498209279. [DOI] [PubMed] [Google Scholar]
- 118.Koch BB, Karnell LH, Hoffman HT, et al. National cancer database report on chondrosarcoma of the head and neck. Head Neck. 2000;22(4):408–425. doi: 10.1002/1097-0347(200007)22:4<408::aid-hed15>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 119.Evans HL, Ayala AG, Romsdahl MM. Prognostic factors in chondrosarcoma of bone: a clinicopathologic analysis with emphasis on histologic grading. Cancer. 1977;40(2):818–831. doi: 10.1002/1097-0142(197708)40:2<818::aid-cncr2820400234>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 120.Borba LA, Al-Mefty O, Mrak RE, Suen J. Cranial chordomas in children and adolescents. J Neurosurg. 1996;84(4):584–591. doi: 10.3171/jns.1996.84.4.0584. [DOI] [PubMed] [Google Scholar]
- 121.Coffin CM, Swanson PE, Wick MR, Dehner LP. Chordoma in childhood and adolescence. A clinicopathologic analysis of 12 cases. Arch Pathol Lab Med. 1993;117(9):927–933. [PubMed] [Google Scholar]
- 122.Menezes AH, Gantz BJ, Traynelis VC, McCulloch TM. Cranial base chordomas. Clin Neurosurg. 1997;44:491–509. [PubMed] [Google Scholar]
- 123.Forsyth PA, Cascino TL, Shaw EG, et al. Intracranial chordomas: a clinicopathological and prognostic study of 51 cases. J Neurosurg. 1993;78(5):741–747. doi: 10.3171/jns.1993.78.5.0741. [DOI] [PubMed] [Google Scholar]
- 124.Mitchell A, Scheithauer BW, Unni KK, et al. Chordoma and chondroid neoplasms of the spheno-occiput. An immunohistochemical study of 41 cases with prognostic and nosologic implications. Cancer. 1993;72(10):2943–2949. doi: 10.1002/1097-0142(19931115)72:10<2943::aid-cncr2820721014>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 125.Linskey ME. Hearing preservation in vestibular schwannoma stereotactic radiosurgery: what really matters? J Neurosurg. 2008 Dec;109(Supplement):129–136. doi: 10.3171/JNS/2008/109/12/S20. [DOI] [PubMed] [Google Scholar]
- 126.Lyman GH, Kuderer NM. The strengths and limitations of meta-analyses based on aggregate data. BMC Med Res Methodol. 2005;5(1):14. doi: 10.1186/1471-2288-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Barker FG, 2nd, Carter BS. Synthesizing medical evidence: systematic reviews and metaanalyses. Neurosurg Focus. 2005;19(4):E5. doi: 10.3171/foc.2005.19.4.6. [DOI] [PubMed] [Google Scholar]