Abstract
Patient: Male, 38
Final Diagnosis: Cavernous hemangioma
Symptoms: Headache • parietal mass
Medication: —
Clinical Procedure: —
Specialty: Neurosurgery
Objective:
A rare disease
Background:
Bone hemangioma is a vascular hemartoma of bone structures. In general, this pathology is detected on incidentally investigated patients’ films. Bone hemangioma is most commonly seen in 4th decade of life and the male/female ratio is 1/1.5. The locations of these lesions are commonly long bones of the vertebral column and the skull.
Primary bone hemangiomas constitute less than 1% of all bone tumors, and they are seen at 0.2% in the calvarial region.
Case Report:
Cases with this pathology are seen on incidental radiological evaluations. We report the case of a 38-year-old man with localized headache and a palpable mass in the left parietal region, admitted and operated on after cranial CT and MRI. Pathology investigation revealed a cavernous hemangioma.
Conclusions:
We suspected that in our case head trauma may have been the cause of cavernous hemangioma in the calvarial region, because cavernous hemangiomas are rarely located there. Localized headache and minor discomfort can be seen with this pathology. The best treatment for cavernous hemangiomas is the removal of the mass within the limits of safe surgery.
Keywords: headache, trauma, cavernous hemangioma
Background
Bone hemangioma is a vascular hemartoma of bone structures. In general, this pathology is detected on incidentally investigated patients’ films. Bone hemangioma is most commonly seen in the 4th decade of life and the male/female ratio is 1/1.5 [1]. The locations of these lesions are commonly long bones of the vertebral column and the skull [1].
Primary bone hemangiomas are less than 1% of all bone tumors, and they are seen at 0.2% in the calvarial region [1,2]. However, these tumors usually located in the parietal and frontal regions [3,4]. Traumatic types are rarer than congenital hemangiomas.
They cause swelling in involved skull bones and, rarely, headache due to their bone-expansive features [5]. The granular calcifications (“sunlight view”) may be seen on the skull x-ray. Also, these calcifications may be multicentric. Macroscopically, hemangiomas are soft, easily broken, red-blooded tissues. Cavernous, vascular, endothelial cells forming the epithelial lining and blood elements are observed microscopically.
Case Report
A 38-year-old man with a left parietal mass and intermittent localized pain was admitted to our clinic. The patient had a history of a motor vehicle injury to the left parietal region 2 years ago. The patient was evaluated with CT, which showed an increase in the left parietal diploë space (Figure 1). After CT, the patient was screened MRI, which showed an expansive lesion in the bone structure (Figure 2). Dural connection and parenchymal compression were not seen on MRI.
Figure 1.
Pre op. cranial CT.
Figure 2.
Pre op. cranial MRG.
The mass was 2×2×2 cm in size and was excised (Figures 3 and 4). Histopathology of the mass showed fibroconnective tissue containing osseous areas in some places and large blood vessels in the stroma. The histopathology result was reported as cavernous hemangioma (Figures 5 and 6).
Figure 3.

Parietal bone with hemangioma.
Figure 4.

Parital bone craniotomy material.
Figure 5.
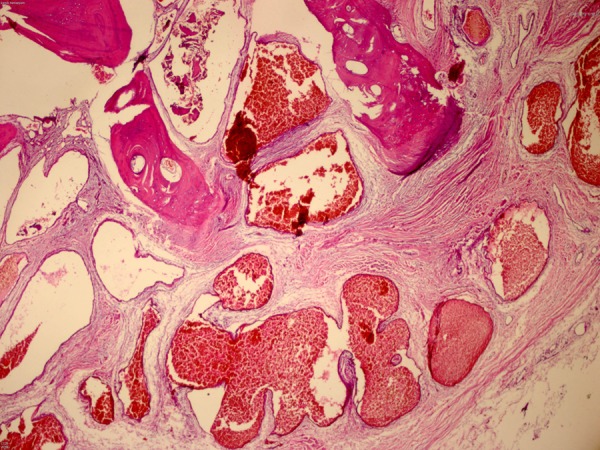
Pathological specimen (hematoxylin and eosin; 200×).
Figure 6.
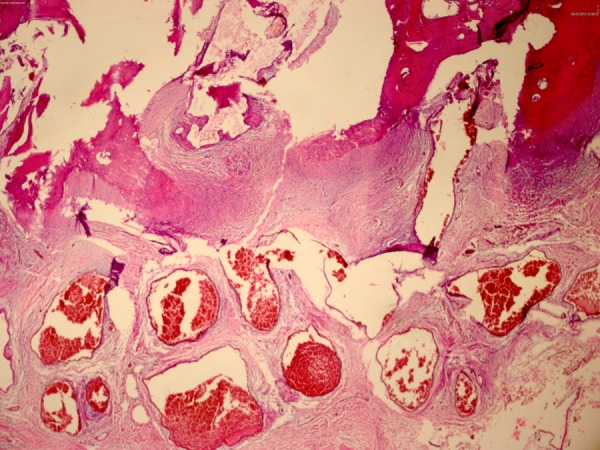
Pathological specimen (hematoxylin and eosin; 200×).
Discussion
Cavernous hemangiomas are often seen in the vertebral column, but are rarely seen in the skull. Intraosseous hemangiomas of the skull constitute 0.2% of all bone tumors, and are commonly seen in frontal and parietal bones [4–6]. However, occipital, sphenoid, and temporal bones may be involved [4]. The incidence of these tumors increases in females and in the 2nd and 4th decades of life. Cavernous hemangiomas consist of blood vessels separating fibrous tissues. Most types of calvarial hemangiomas are fed from branches of the external carotid artery, especially from branches of the middle meningeal artery, superficial temporal artery, and posterior occipital artery [7,8].
A lytic lesion affecting the outer layer of the skull, without the internal layer, may cause sclerotic margin. Bone spicules extending from center to periphery in the lytic lesion (sunburst pattern or honeycombing) are characteristic for the lesion. However, this finding may be seen in meningioma, osteogenic sarcoma, and osteoblastic metastases. The MRI signal of hemangioma is variable and the hyperintensity of hemangiomas at T1-weighted sequences is an important distinguishing feature for these tumors [1].
Calvarial hemangiomas are generally seen as congenital in the literature. The rates are low after head trauma when compared with congenital forms. The effect of trauma on the development of hemangiomas is unclear [3–7]. It is thought that some growth factors are released after trauma. Our case was a 38-year-old male and had a history of trauma to the pa rietal bone 2 years ago.
These tumors can be misdiagnosed as a dermoid cyst, a giant cell tumor of bone, multiple myeloma, and metastasis [2]. Pre-operative diagnosis of this tumor may be difficult because of its similarity to other bone pathologies. The most useful radiological tool is CT, clearly showing cortical and trabecular structures [9,10]. The diagnosis of cavernous hemangiomas is established by histopathology. Hemangiomas consist of 4 types: cavernous, sclerosing, cellular, and capillary. The most common is cavernous type [6].
Our patient was diagnosed histologically as having cavernous hemangioma.
Hemangiomas are usually symptomatic lesions. Clinical findings include headache, increased intracranial pressure by parenchymal compression, cranial nerve deficits, and cosmetic changes [4]. In our case, correction of cosmetic changes and localized pain were the purposes of the surgery. If possible, the aim of surgery should include normal neighboring bones for these tumors.
Conclusions
As a result, we suggest that head trauma may be the cause of cavernous hemangioma in the calvarial region, as in our case, because cavernous hemangiomas are rarely seen in the calvarial region. Localized headache and minor discomfort can be seen with this pathology. The best treatment for cavernous hemangiomas is the removal of the mass within the limits of safe surgery.
References:
- 1.Khanam H, Lipper MH, Wolff CL, Lopes MB. Calvarial hemangiomas: report of two cases and review of the literature. Surg Neurol. 2001;55:63–67. doi: 10.1016/s0090-3019(00)00268-8. [DOI] [PubMed] [Google Scholar]
- 2.Vernet O, Bernasconi A, Fankhauser H. Cavernous hemangioma of the frontal bone: a case report. Turkish Neurosurgery. 1993;3:118–21. [Google Scholar]
- 3.Dogan S, Kocaeli H, Sahin S, et al. Large cavernous hemangioma of the frontal bone: case report. Neurol Med Chir (Tokyo) 2005;45:264–67. doi: 10.2176/nmc.45.264. [DOI] [PubMed] [Google Scholar]
- 4.Heckl S, Aschoff A, Kunze S. Cavernomas of the skull: review of the literature 1975–2000. Neurosurg Rev. 2002;25:56–62. doi: 10.1007/s101430100180. [DOI] [PubMed] [Google Scholar]
- 5.Kang DW, Choi CH. A case of calvarial hemangioma in cranioplasty site. J Korean Neurosurg Soc. 2009;46:484–87. doi: 10.3340/jkns.2009.46.5.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valentini V, Nicolai G, Lore B, et al. Intraosseous hemangiomas. J Craniofac Surgery. 2008;19:1459–64. doi: 10.1097/SCS.0b013e318188a030. [DOI] [PubMed] [Google Scholar]
- 7.Pastore FS, De Caro GM, Faiola A, et al. Cavernous hemangioma of theparietal bone. Case report and review of the literature. Neuro Chirurgie. 1999;45:312–15. [PubMed] [Google Scholar]
- 8.Bastug D, Ortiz O, Schochet SS. Hemangiomas in thecalvaria: Imagingfindings. Am J Roentgenol. 1995;164:683–87. doi: 10.2214/ajr.164.3.7863894. [DOI] [PubMed] [Google Scholar]
- 9.Moore SL, Chun JK, Mitre SA, Som PM. Intraosseous hemangioma of the zygoma: CT and MR findings. Am J Neuroradiol. 2001;22:1383–85. [PMC free article] [PubMed] [Google Scholar]
- 10.Liu JK, Burger PC, Harnsberger HR, et al. Primary intraosseous skull base cavernous hemangioma: case report. Skull Base. 2003;13:219–28. doi: 10.1055/s-2004-817698. [DOI] [PMC free article] [PubMed] [Google Scholar]




