Abstract
Importance
Clear guidelines on the health effects of dairy food are important given the high prevalence of obesity, cardiovascular disease and diabetes, and increasing global consumption of dairy food.
Objective
To evaluate the effects of increased dairy food on cardio metabolic risk factors.
Data Sources
Searches were performed until April 2013 using MEDLINE, Science Direct, Google,Embase, the Cochrane Central Register of Controlled Trials, reference lists of articles, and proceedings of major meetings.
Study Selection
Randomized controlled studies with healthy adults randomized to increased dairy food for more than one month without additional interventions.
Data Extraction and Synthesis
A standard list was used to extract descriptive, methodological and key variables from all eligible studies. If data was not included in the published report corresponding authors were contacted.
Results
20 studies with 1677 participants with a median duration of dietary change of 26 (IQR 10-39) weeks and mean increase in dairy food intake of 3.6 (SD 0.92) serves/day were included.
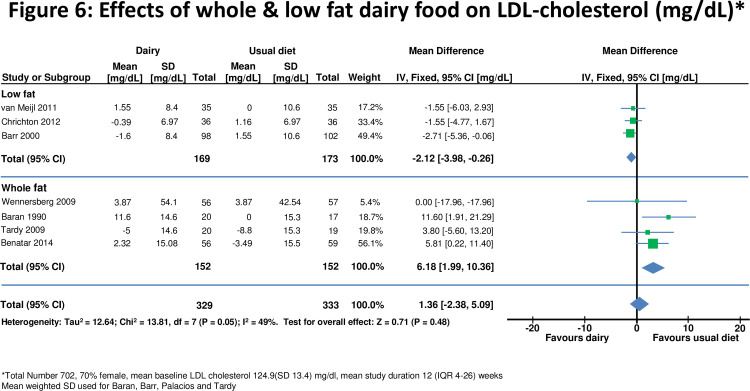
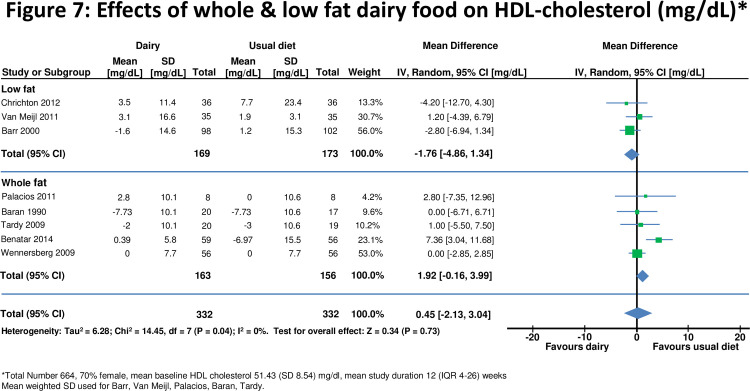
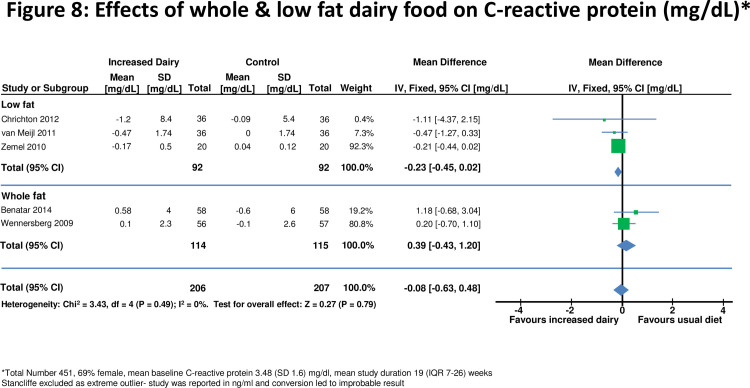
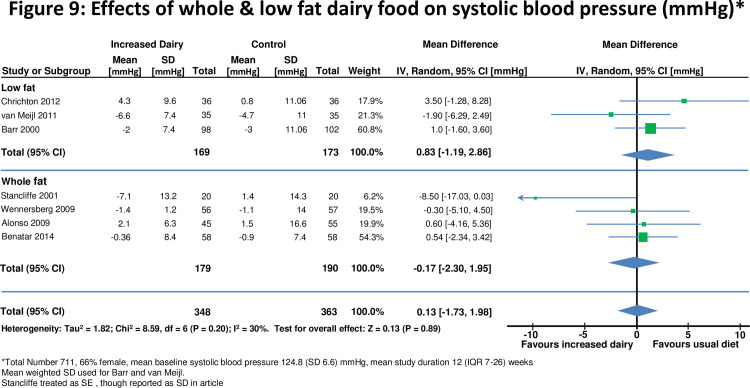
Increased dairy food intake was associated with a modest weight gain (+0.59, 95% confidence interval 0.34 to 0.84kg, p<0.0001) but no significant change in waist circumference (0.35 , -0.75 to 1.45 cm); insulin resistance (HOMA –IR -0.94 , -1.93 to 0.05 units); fasting glucose (0.87, -0.27 to 2.01 mg/dl); LDL-cholesterol (1.36 ,-2.38 to 5.09 mg/dl); HDL-cholesterol (0.45, -2.13 to 3.04 mg/dl); systolic (-0.13, -1.73 to 1.98 mmHg) and diastolic blood pressure (0.13, -1.73 to 1.98 mmHg) or C-reactive protein (-0.08, -0.63 to 0.48 mg/L). Results were similar for studies with low-fat and whole-fat dairy interventions.
Limitations
Most clinical trials were small and of modest quality. .
Conclusion
Increasing whole fat and low fat dairy food consumption increases weight but has minor effects on other cardio-metabolic risk factors.
Trial Registration ACTRN
Australian New Zealand Clinical Trials Registry ACTRN12613000401752, http://www.anzctr.org.au
Ethics Approval Number
NTX/10/11/115
Introduction
Clear guidelines on the health effects of dairy food are important given the high and increasing prevalence of obesity[1], cardiovascular disease [2] and diabetes[3] in most countries, and the increasing global consumption of dairy food[4]. Many current dietary guidelines promote low fat dairy as a healthy food[5,6]. This advice is supported by observational studies which report that increased dairy consumption is associated with lower blood pressure[7-11], weight reduction [12], improved insulin sensitivity[7,11,13,14], less inflammation [15,16] and a lower ratio of total to HDL cholesterol[17]. A modest inverse association between dairy consumption and cardiovascular disease has also been reported[18-20].
In contrast, whole fat dairy is not recommended in most food guidelines [21-23] because of the concern that saturated fat in dairy food may have an adverse effect on serum lipids which could increase the risk of cardiovascular disease. Despite these guidelines the effects of high fat dairy food on the risk of obesity, diabetes and cardiovascular disease are uncertain. A recent meta-analysis found no association of dietary saturated fat intake and the risk of cardiovascular disease[24]. Whole fat dairy foods contain many fatty acids, which may have favorable as well as unfavorable effects on lipids and other cardio-metabolic risk factors[25]. Also, effects of reducing saturated fat from one food are determined by other dietary changes, including carbohydrates, and mono-unsaturated and poly-unsaturated fatty acids[17].
The effects of a high dairy food diet on diabetes and cardiovascular disease have not been evaluated in randomized clinical outcome trials. The large long term randomized dietary intervention studies which evaluated the ‘Dietary Approaches to Stop Hypertension’ (DASH) [26] and ‘Mediterranean’ [27] diets on clinical outcomes, while including increased low fat dairy food in the intervention, do not allow an evaluation of the independent effects of changes in dairy food intake. Health effects of whole and low fat dairy food would be more reliably evaluated in clinical trials than in observational studies, and by assessing a number, rather than just one cardio-metabolic risk factor. We therefore undertook a meta-analysis of randomized clinical studies that evaluated effects of changing whole and low fat dairy food intake in healthy adults on a broad range of cardio-metabolic risk factors including weight, insulin resistance, lipids, blood pressure and c- reactive protein (CRP).
Methods
We followed the PRISMA (http://www.prisma-statement.Org ) guidelines throughout the design, implementation, analysis, and reporting of this meta-analysis. See Checklist S1 and File S1 for the PRISMA checklist and flow chart, respectively. A protocol for the study was designed and is available as File S2. The study was registered with the Australian New Zealand Clinical Trials Registry, with trial registration number ACTRN12613000401752.
Search Strategy
We searched for all trials that randomized adults to increased dairy for at least one month without additional interventions (e.g. caloric restriction, multiple dietary interventions), had an appropriate control group, and sufficient data to calculate estimates of effect with standard deviations on at least one of the following: weight, waist circumference, blood pressure, HDL and LDL cholesterol, fasting glucose, insulin resistance and C-reactive protein. Studies were excluded if they were observational or otherwise non-randomized; were commentaries, reviews, or duplicate publications from the same study. We restricted to studies of healthy adults who did not have diabetes, hypertension or vascular disease. Both feeding and dietary advice trials and studies with a crossover or parallel group study design were included.
Searches were performed of literature published through March 2013 using Medline, Science Direct, Google, Embase, the Cochrane Central Register of Controlled Trials, reference lists of articles, and proceedings of major meetings for relevant literature. The search terms were ‘dairy’ and each of the following; ‘cardio metabolic risk’, ‘weight’, ‘waist circumference’, ‘glucose’, ‘insulin’, ‘insulin resistance’, ‘inflammation’, ‘inflammatory markers’, ‘blood pressure’, ‘cholesterol’ and ‘lipids’.
Assessment of study eligibility and data extraction
One reviewer screened all abstracts and titles and, upon retrieval of candidate studies, two team members (JB, KS) reviewed the full text to determine eligibility. If the study was eligible, data were abstracted by JB. Through an iterative process, a standard list was used to extract descriptive, methodological and key variables from all eligible studies. Data extracted included years the study was performed and reported, the primary aim of the study, population characteristics, funding source, control and intervention diets, duration of follow-up, estimates of effect and standard deviations. If data was not included in the published report corresponding authors were contacted [28,29]. The quality of each study was rated using the Jadad score[30]. Questions arising during data abstraction were resolved by discussion with all team members.
Definitions
Dairy food with less 1% fat, such as trim or low fat milk was categorized as a low fat dairy food. Dairy food that included full fat milk (3-4% fat), cheese, butter, cream and ice cream, was categorized as whole fat dairy food..
The method used to quantify insulin resistance was the homeostatic model assessment- Insulin resistance (HOMA-IR)[31]. This estimates steady state insulin sensitivity as units. The equation that is used is HOMA-IR = glucose (mmol/L) x insulin (munits/L) ÷22.5.
Statistical analysis
Each cardio-metabolic risk factor when on a higher and lower dairy diet was compared between cases and controls from the same study. For those studies with 3 treatment groups, comparison was made between the control and the high dairy food group. Effects were measured at least 4 weeks after randomization, with the final results used for studies with more than one measurement during follow up. A negative effect size means that dairy has a favorable effect on the cardio metabolic risk factor. Because increase in HDL-cholesterol is considered beneficial, positive and negative exponents were switched to maintain consistency in presentation. In one study the standard deviation was not reported [32] but calculated from the 95% confidence intervals.
For each cardio-metabolic risk factor the weighted mean change from baseline to follow up was calculated across all included studies within each randomized group. The inverse-variance method, whereby study differences are weighted according to the reciprocal of their variance, was used to pool all standardized mean differences to yield an overall effect size with corresponding 95% confidence intervals.
When SD were not available, the mean weighted standard deviation of the group was used. For studies that used standard error of the mean (SEM) , this was converted to SD.
Each meta-analysis was assessed for heterogeneity by a Chi square test and I2 statistic. A fixed effects model was used when heterogeneity was not present (I2=0) and a random effects model was used when statistical heterogeneity (I2≥1%) was present. A p-value of <0.05 was considered statistically significant. Studies are presented in Forrest plots in order of statistical power. Stratified analyses was studied by low fat and whole fat dairy, duration of dietary intervention (less than or greater than 6 months), body weight of study participants, and industry or public source of funding. Studies where the intervention was skim, trim or <1% dairy food are low fat dairy studies. Sensitivity analyses were also conducted to evaluate the impact of selected studies on overall pooled estimates and heterogeneity. The Statistical analyses were performed using RevMan software version 5·2 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen).
Results
Search Results
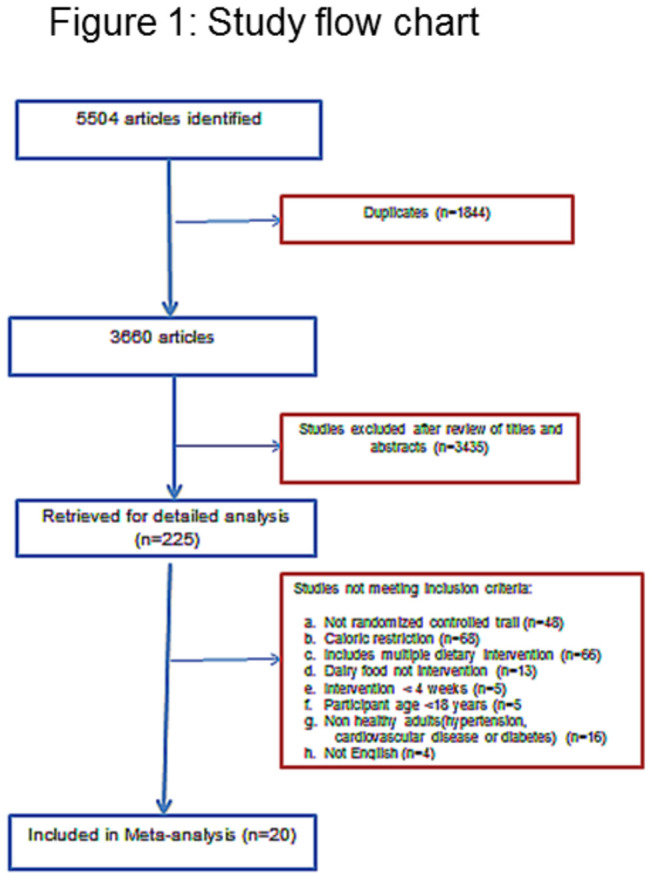
The literature search yielded 5504 citations (2495 on Pub Med and 2849 on Science Direct,160 on Google), of which included 1844 duplicates. After title and abstract screening, the full text of 225 articles were evaluated, with 205 excluded either because the intervention included caloric restriction or had multiple dietary changes, or the study was in a population with disease (Figure 1). Twenty studies were included in the meta-analysis.
Figure 1. Study flow chart.
Characteristics of studies
Characteristics of the 20 included trials which included 1677 participants are summarized in Table 1. The average age was 51 (SD 16) years and 78% of participants were female. The median duration of follow up was 26 (IQR 10-39) weeks. The average difference in dairy intake between groups was 3.12 (SD 0.62) standard serving sizes /day. Within studies there was no imbalance between randomized groups. One crossover study [28] had a higher dropout rate for subjects initially randomized to low compared to high dairy intake (49% vs. 22%).
Table 1. Baseline characteristics of studies included in this meta-analysis.
| Trial Year published | Country | Population | Mean BMI (kg/M2) | Funding source | Number of subjects (% female) | Mean Age years (SD) | Design | Length of intervention (Weeks) | Primary outcome | Low dairy | High Dairy (+ serves /day) | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alonso[32] 2009 | Spain | Normotensive college students | 23.6 | Public | 45 (60%) | 19·9 (1·5) | Crossover | 8 | Blood pressure and weight | 1·5 serves/day | 3·5 whole-fat | 2 |
| Baran[46] 1990 | America | Healthy volunteers | 22.8 | Industry | 37 (100%) | 36.5 (3.4) | Parallel | 156 | Bone density | Usual diet | 2.5 whole-fat or low-fat dairy | 2 |
| Barr[29] 2000 | North America | Healthy volunteers | 25.8 | Industry | 198 (64%) | 65·2 (6·7) | Parallel | 12 | Weight, blood pressure, lipids | Usual diet | 3 low-fat dairy | 3 |
| Benatar[45] 2014 | New Zealand | Healthy volunteers | 24.6 | Public | 120 (75%) | 46·3 (12·0) | Parallel | 4 | Weight, blood pressure | Usual diet | 3·5 whole-fat or low-fat dairy | 3 |
| Chee[36] 2003 | Malaysia | Postmenopausal Chinese woman | 23.8 | Industry | 173 (100) | 59·0 (3·2) | Parallel | 104 | Bone loss | Usual diet | 2 low-fat dairy | 3 |
| Crichton[28] 2012 | Australia | Overweight and obese volunteers | 31.5 | Public | 36 (83) | 47·3 (15·1) | Crossover | 26 | Weight | ≤1 serves/day | 4 low-fat dairy | 2 |
| Eagan[37] 2006 | North America | Normal weight young women | 22.5 | Industry | 37 (100) | 20·0 (2·0) | Parallel | 26 | Fat mass | Usual diet | 3 whole-fat or low-fat dairy | 2 |
| Gardner[47] 2007 | North America | Healthy volunteers | 26.0 | Industry | 28 (79) | 52(9) | Crossover | 4 | Lipids | Usual diet | 2·5 low-fat dairy | 3 |
| Ghadirian [35] 1995 | Canada | Postmenopausal nuns | 23.0 | Industry | 158(100%) | 79 (9.5) | Parallel | 4 | Uric acid | 0 | 3.6 whole-fat or low-fat dairy | 2 |
| Gunther [38] 2005 | North America | Healthy woman | 22.2 | Industry | 99 (100) | 20·0 (2·1) | Parallel | 52 | Weight | Usual diet | 3 low-fat dairy | 2 |
| Kukuljan [34] 2009 | Australia | Older men (>50years) | 27.6 | Public | 89(0%) | 60.9 (7.5) | Parallel | 52 | Bone Density | Usual diet | 1.7 low-fat dairy | 2 |
| Lau[39] 2001 | China | Postmenopausal women | 22.2 | Industry | 185 (100) | 57·0 (1·8) | Parallel | 104 | Bone loss | Usual diet | 2 low-fat dairy | 3 |
| Manios[33] 2009 | Greece | Postmenopausal women | 30.4 | Industry | 62(100) | 61.2 (4.9) | Parallel | 52 | Weight | Usual diet | 3 low-fat dairy | 2 |
| Palacios[40] 2011 | Puerto Rico | Obese adults | 38.5 | Public | 16 (81) | 37·0 (2·2) | Parallel | 21 | Weight, lipids | Usual diet | 4 whole-fat or low-fat dairy | 1 |
| Stancliffe[41] 2011 | North America | Overweight and obese with metabolic syndrome | 30.7 | Industry | 40 (53) | 37·0 (9·9) | Parallel | 12 | Inflammatory markers | 0·5 serves /day | 3·5 whole-fat or low-fat dairy | 2 |
| Tardy[42] 2009 | France | Healthy women with abdominal obesity | 32.6 | Public | 39 (100) | 36·4 (7·7) | Parallel | 4 | HOMA | Usual diet + vegetable oils | 3 whole-fat | 2 |
| Van Meilj[49] 2010 | Holland | Overweight adults | 32.0 | Industry | 35 (71) | 49·5(13·2) | Crossover | 8 | Blood pressure, Lipids, inflammatory marker, glucose | Usual diet | 3 low-fat dairy | 2 |
| Wennersberg[43] 2009 | Scandinavia | Metabolic syndrome | 30.0 | Industry and Public | 105 (67) | 51·2 (8·0) | Parallel | 26 | Waist circumference | Usual diet | 3-5 whole-fat or low-fat dairy | 2 |
| Zemel[48] 2010 | North America | Obese and overweight adults | 30.0 | Industry | 20 (30) | 31·0 (10·3) | Crossover | 4 | Inflammatory markers | 0 | 3 low-fat dairy | 3 |
| Zemel (phase 1)[44] 2005 | North America | Obese adults | 34.9 | Industry | 34 (59) | 41·7 (2·8) | Parallel | 26 | Weight | Usual diet | 3 whole-fat or low-fat dairy | 1 |
Sixteen studies had a parallel group design and 4 were cross-over studies. In 10 studies increased dairy food included whole fat dairy, while 10 only low fat dairy food was advised. Fifteen of the studies were at least partly funded by the dairy or food industry.
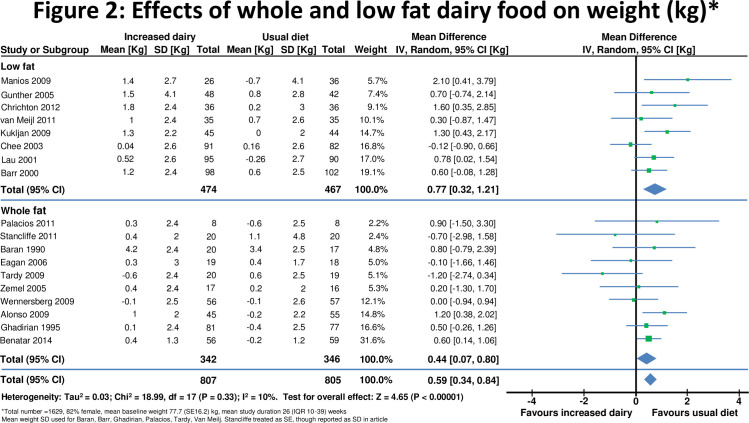
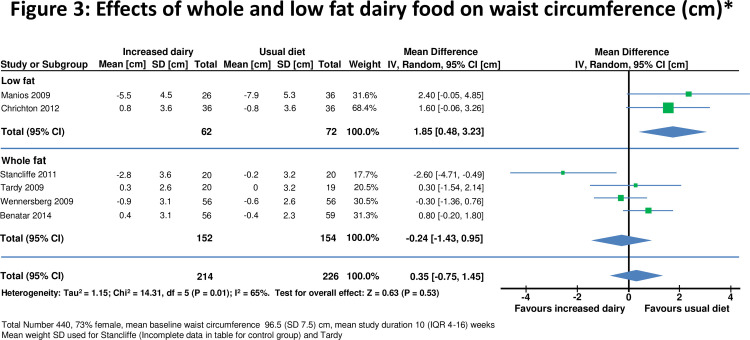
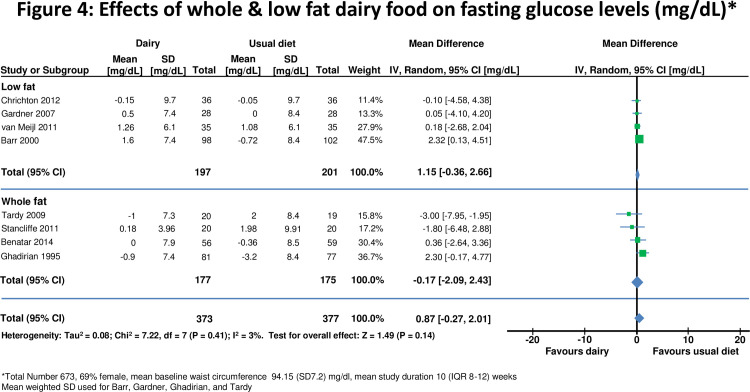
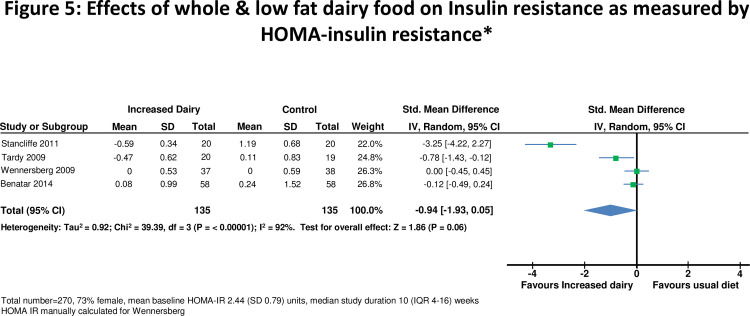
Change in risk factors on a high and a lower dairy diet in all studies combined are displayed in Figures 2-10. Results stratified by duration of intervention, participant body weight and by funding source are displayed in table 2.
Figure 2. Effects of whole & low fat dairy food on weight.
Table 2. Studies stratified by study duration, study population normal weight or overweight and source of funding on cardio-metabolic risk factors.
| Metabolic risk factors | Diet Change <6 months duration | Diet change ≥ 6 months duration | Normal weight (BMI <25 kg/m2) | Overweight or obese (BMI > 25kg/m2) | Industry funded studies | Public funded studies |
|---|---|---|---|---|---|---|
| Total number of studies | 10 | 10 | 8 | 12 | 14 | 6 |
| Total number of subjects | 738 | 982 | 854 | 823 | 1246 | 431 |
| Weight (kg) | +0.64* (0.35 to 0.92) | +0.58* (0.10 to 1.07) | +0.57* (0.29 to 0.85) | +0.67* (0.22 to 1.13) | +0.41* (0.09 to 0.72) | +0.79* (0.47 to 1.11) |
| N | 738 | 891 | 895 | 534 | 1198 | 431 |
| Waist circumference (cm) | -0.34 (-2.23 to 1.55) | +1.01 (-0.66 to 0.85) | +0.80 (-0.25 to 1.85) | -0.24 (-1.20 to 1.68) | -0.24 (-2.56 to 2.07) | +0.89 (-0.09 to 1.69) |
| N | 194 | 246 | 115 | 325 | 214 | 226 |
| HOMA- IR (units) | -1.32 (-2.84 to 0.20) | 0.00 (-0.45 to 0.45) | -0.12 (-0.4 to 0.24) | -1.29 (-2.90 to 0.32) | -1.59 (-4.77 to 1.59) | -0.39* (-1.02 to 0.24) |
| N | 195 | 75 | 116 | 154 | 115 | 155 |
| Fasting Glucose (mg/dl) | +0.05 (-0.01 to 0.12) | -0.01 (-0.18 to 0.17) | +0.09 (-0.01 to 0.19) | +0.02 (-0.06 to 1.10) | +0.07 (0.00 to 0.14) | +0.01 (-0.13 to 0.10) |
| N | 601 | 72 | 196 | 477 | 524 | 226 |
| LDL-cholesterol (mg/dl) | +0.94 (-2.97 to 4.85) | +2.67 (-8.49 to 13.83) | +7.3* (2.34 to 12.26) | 1.13 (-3.85 to 1.59) | -1.65 (-3.98 to 7.27) | +1.14 (-4.66 to 6.94) |
| N | 480 | 222 | 115 | 587 | 460 | 242 |
| HDL-cholesterol (mg/dl) | -1.33 (-3.52 to 6.19) | +0.64 (-2.71 to 1.43) | 4.63 (-2.34 to 11.60) | -0.95 (-2.72 to 0.81) | -0.86 (-3.01 to 1.29) | 2.37 (-3.19 to 7.94) |
| N | 443 | 221 | 155 | 509 | 419 | 245 |
| C- reactive protein (mg/L) | -0.55 (-1.26 to 0.16) | +0.11 (-0.77 to 0.98) | +1.18 (-0.68 to 3.04) | -0.43 (-1.01 to 0.14) | -0.41 (-1.00 to 0.17) | 0.62 (-0.99 to 2.23) |
| N | 268 | 183 | 116 | 335 | 265 | 186 |
| Systolic blood pressure (mmHg) | +0.48 (-1.39 to 2.36) | +1.76 (-1.95 to 5.47) | +0.57 (-1.37 to 2.51) | -1.05 (-2.62 to 0.52) | -1.44 (-3.15 to 0.28) | +0.64 (-1.10 to 2.37) |
| N | 526 | 185 | 216 | 495 | 423 | 288 |
| Diastolic blood pressure (mmHg) | +0.56 (-1.91 to 3.02) | +0.74 (-1.78 to 3.25) | +0.56 (-1.91 to 3.02) | +0.74 (-1.78 to 3.25) | -0.01 (-2.87 to 2.85) | +1.29 (-0.85 to 3.42) |
| N | 526 | 185 | 216 | 495 | 423 | 423 |
P <0.05, n = number of participants
Effects on body weight
Eighteen [10,28,29,32-46] studies reported effects on weight in 1629 individuals (Figure 2). The mean body mass index (BMI) at baseline was 25.6(SD 6.2) kg/m2 and weight 77.7(SD 16.2) kg. Increased dairy intake was associated with a modest weight gain (+0.59, 95% confidence interval 0.34 to 0.84kg, p<0.0001). In six studies[28,33,41-43,45] in 440 individuals waist circumference did not change significantly(0.35 , -0.75 to 1.45cm) (Figure 3).
Figure 3. Effects of whole & low fat dairy food on waist circumference.
Weight gain was observed both in studies which increased low fat (+0.77, 0.32 to 1.21 kg, p<0.001) and whole fat dairy food (+0.44, 0.07 to 0.80kg, p=0.04). Modest weight gain was also observed in 10 studies (n= 692) which included overweight and obese subjects (+0.66, 0.04 to 1.29kg, p=0.04) and in 8 studies (n= 937) of normal weight participants (+0.60, 0.35 to 0.85kg, p<0.001).
Effects on insulin resistance
In 8 studies [10,28,29,35,41,42,45,47], there was no significant change in fasting glucose on higher compared to lower dairy diet (Figure 4). Four studies [41-43,45] assessed effects on HOMA-IR in 270 subjects (Figure 5). One [42] did not report standard deviation so a weighted mean standard deviation from the other studies was used. HOMA-IR was recalculated in one study which used incorrect units [43]. For all studies combined HOMA-IR was slightly improved on the high dairy diet (-0.94, -1.93 to 0.05 units, p=0.06). However there was heterogeneity between studies (I2 =92%), accounted for by the two smallest studies [41,42] which reported reduced insulin resistance on the high dairy diet (-1.37, -1.64 to -1.10 units). HOMA-IR was similar on high and low dairy diets in the two larger studies[43,45] (-0.05, -0.26 to 0.17 units). HOMA-IR did not change significantly for studies stratified by body weight, duration of intervention or high versus low fat dairy (Table 2).
Figure 4. Effects of whole & low fat dairy food on fasting glucose levels.
Figure 5. Effects of whole & low fat dairy food on Insulin resistance as measured by HOMA-insulin resistance.
Effects on LDL and HDL cholesterol
Eight studies [10,28,29,40, 42, 43,45,46] assessed effects on LDL- and/or HDL-cholesterol (n=664 for HDL, n=662 for LDL). For all studies combined there was no significant change in either LDL or HDL-cholesterol after increasing dairy food (Figures 6 and 7). Effects of HDL-cholesterol were consistent (I2=0%) across studies, but there was heterogeneity for LDL-cholesterol (I2=49%). There was no change in LDL cholesterol when whole fat dairy (+6.18, 1.99 to 10.36 mg/dl) or low fat dairy (-2.12, -3.98 to -0.26 mg/dl) food was increased (Figure 6). Results were similar for shorter and longer periods of dietary intervention and for studies which included normal and overweight or obese participants.
Figure 6. Effects of whole & low fat dairy food on LDL-cholesterol.
Figure 7. Effects of whole & low fat dairy food on HDL-cholesterol.
Effects on C-reactive protein
Five studies[28,43,45,48,49] assessed effects on C-reactive protein in 400 individuals (Figure 8). For all studies combined there was no significant change in C-reactive protein on a high dairy diet (-0.08, -0.63 to 0.48 mg/dL). However two smaller studies [41,48] reported significant reductions in C-reactive protein with increased dairy intake. There was no evidence for effects on C-reactive protein when studies were stratified by duration of dietary intervention, high and low fat dairy, or normal or overweight subjects (Table 2).
Figure 8. Effects of whole & low fat dairy food on C-reactive protein.
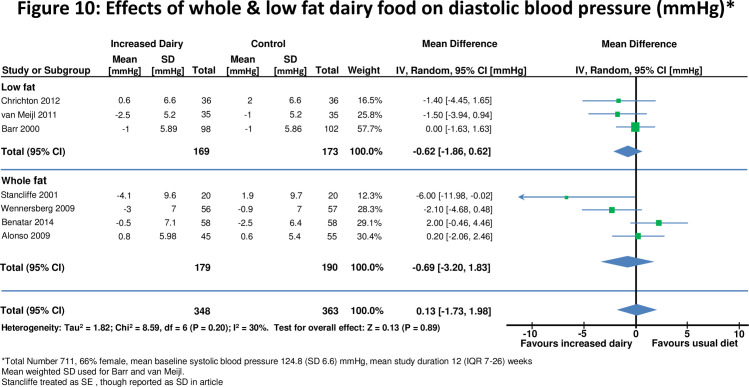
Effects on blood pressure
Seven studies [10,28,29,32,41,43,45,49] assessed effects on blood pressure in 711 participants (Figures 9 and 10). For all studies there was no significant change in either systolic blood pressure or diastolic blood pressure. There was also no evidence for effects on blood pressure when studies were stratified by duration of dietary intervention, high and low fat dairy or normal or overweight subjects.
Figure 9. Effects of whole & low fat dairy food on systolic blood pressure.
Figure 10. Effects of whole & low fat dairy food on diastolic blood pressure.
Evaluation of heterogeneity and sensitivity analysis
Industry sponsored studies were more likely to report favorable effects on risk factors than non-industry sponsor studies (Table 2). Results were also similar when analysis was repeated excluding the 4 cross-over studies. Funnel plots identified that the study by Stancliffe [41] reported decreases in LDL cholesterol, HOMA-IR, C-reactive protein and waist circumference on the increased dairy diet beyond the 95% confidence range for all studies combined (see S2 File in the accompanying notice [67]). This study also reported the greatest decrease in blood pressure and weight of all studies. Excluding this study in a sensitivity analysis substantially decreased heterogeneity, but overall effects were similar, and there was no other consistent difference between smaller and larger studies. The study by Manios[33] was the only study that fell outside the 95% confidence interval for weight, though excluding the study had no overall effect on results. This study had an imbalance in randomization with fewer people randomized to high dairy food (n=30) compared to the control group (n=40). The study by Ghadirian[35] was outside the 95% confidence interval for fasting plasma glucose. In this study, the control group had a statistically significant reduction in fasting plasma glucose, with little change for the high dairy group. Analysis repeated excluding this study showed no overall effect (+0.02,-0.05 to 0.09mmol/L, p=0.56) and a reduction in heterogeneity (25→0%).
On the basis of a funnel plot and Begg’s test, no significant publication bias was shown in the meta-analysis of body weight, waist circumference, insulin resistance, blood pressure, lipids and C-reactive protein.
Discussion
This systematic analysis of randomized dietary intervention trials suggests that a moderate increase in dairy food consumption has no or small effects on the major cardiovascular and metabolic risk factors [50]. This conclusion contrasts with results from several large epidemiological studies, which concluded that dairy food may have favorable effects on insulin resistance and decrease the risk of type 2 diabetes[7,51]. However, in these observational studies[32,52-54] dairy food intake was associated with an overall healthier eating pattern, healthier lifestyle, higher socio economic status and educational attainment, which are each associated with more favorable cardio metabolic profiles[55]. Evaluating effects of dairy in randomized intervention trials is likely to be more reliable than from observational studies, where associations may not be causal.
Several observational studies have suggested that dairy food may facilitate weight loss, particularly in obese and overweight individuals [12]. Also in randomized trials where the intervention included both increased dairy food and caloric restriction, weight loss has been reported [56]. However, in the current meta-analysis, which included studies which gave no advice on calorie restriction, increasing dairy food resulted in a modest weight gain. Results were similar in studies which included overweight and obese participants. Whilst no direct comparison is possible, mean weight gain on low fat dairy food is double that of whole fat dairy food. This is counterintuitive but is in keeping with a recent viewpoint in JAMA pediatrics[57] which suggest that trim milk is associated with increased weight in children. It is likely the weight gain was the result of increased total calories in studies which encouraged greater dairy intake without other changes in diet. It is uncertain whether weight gain also occurs when dairy food is taken as part of, rather than in addition to a balanced diet.
Several diabetes guidelines [5,58,59] recommend regular intake of low fat dairy because of its low glycemic index[60]. In observational studies[51,61] persons in the highest quartile of dairy consumption have less insulin resistance, and this association is strongest in those who are overweight or obese. In this analysis insulin sensitivity improved in two small studies[41,42] with no effect in the larger trials[43,45]. In stratified analyses there was no effect in overweight and obese participants, or with whole or low fat dairy interventions. Based on these observations, it is uncertain whether increasing dairy food improves insulin sensitivity, and further well designed studies are needed to resolve this question. A recent review by the American Diabetes Association[62] concluded that ‘none of the components of dairy appear to have an effect on glycemic control or cardiovascular disease risk reduction’, consistent with this analysis.
Many food guidelines encourage low fat dairy food, but advise avoiding whole fat dairy [22,63]. In the current analysis LDL cholesterol did not change significantly when whole fat dairy consumption was increased. Whilst the risk of cardiovascular disease is reduced when saturated fats are replaced by unsaturated fats [64], the reasons for this may be multifactorial. This study suggests that effects on LDL-cholesterol may not the primary reason.
Dairy intake was associated with lower blood pressure in observational studies [8,13] and in the large randomized DASH study [26]. In the DASH study the intervention included increased low fat dairy food, reduced total and saturated fat, and increased fruit and vegetables. In a secondary analysis it was estimated that low fat dairy could account for about half of the observed 5.5mmHg decrease in systolic blood pressure. However it is not possible to reliably estimate the effects of each dietary component when the intervention includes multiple dietary changes. For this reason the DASH study and studies of the Mediterranean diet [27] were not included in this meta-analysis. In this meta-analysis, the confidence intervals exclude significant effects (>1.6mmHg) of increasing dairy food on systolic and diastolic blood pressure.
Limitations of meta-analysis
The majority of subjects included in the meta-analysis were women, but there is currently no evidence for different effects of diet by gender. The diverse population and age range of subjects included makes the results relevant to improving lifestyle risk factors for diabetes and cardiovascular disease in the general population. Studying healthy populations also avoids possible treatment and disease effects on the outcomes of interest. Further research is needed to confirm similar neutral effects of dairy in patients with established diabetes and cardiovascular disease.
It is possible the duration of the dietary intervention was not long enough to identify effects on risk factors, but stratified analyses suggest similar results for longer and shorter periods of dietary intervention. The increase of 3.6 servings each day is a substantial dietary change, and previous studies suggest dietary interventions influence risk factors within one month[26,65].
Most studies included were relatively small. It is difficult to blind diet studies and the level of compliance with the dietary interventions was often uncertain. Several studies reported significant adverse or favorable effects of increasing dairy food on one or more risk factors, but sensitivity analyses suggested these studies had only a small effect on overall estimates. It is also possible that smaller studies which found no effects have not been published. Three quarters of the studies were funded by the dairy or food industry, and results were more favorable for industry compared to non-industry funded studies. This meta-analysis stratified studies by ‘low fat’ and ‘whole fat’ interventions, but a direct comparison of these studies may not be reliable, and no trials which directly compare ‘low’ with ‘whole’ fat dairy diets have been reported. Because studies were small, and some may be unreliable, the analysis can not exclude a small increase in LDL cholesterol with increase in whole fat dairy consumption. Studies are also needed to evaluate effects of other components of dairy food.
To provide a better estimate of health effects the meta-analysis evaluated associations with multiple rather than just one or two risk factors. However dairy food could influence the risk of cardiovascular disease or diabetes by pathways other than the risk factors measured[66]. The influence of dairy food on clinical outcomes rather than risk factors is most important for dietary guidelines. However, currently, no completed randomized trials allow independent assessment of the effects of changing dairy food on diabetic complications or cardiovascular events.
Conclusion
Increase in both whole and low fat dairy food, without other dietary interventions, is associated with a modest weight gain, with no or minor effects on other cardio-metabolic risk factors. These observations suggest that for most healthy individuals it is reasonable to include both low and whole fat dairy food as part of a healthy diet.
Supporting Information
Prisma checklist.
(DOC)
Prisma flow chart.
(PDF)
Protocol.
(DOCX)
Funding Statement
The authors have no support or funding to report.
References
- 1.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT et al. (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet 378: 804-814. doi: 10.1016/S0140-6736(11)60813-1. PubMed: 21872749. [DOI] [PubMed] [Google Scholar]
- 2.Mackay J, Mensah G, Mendis S, Greenland K. (2004) The atlas of heart disease and stroke / J Greenland. World Health Organization. U. S. Centers for Disease Control and Prevention. p 112. https://apps.who.int/iris/handle/10665/43007. [Google Scholar]
- 3.International Diabetes Federation (2011) IDF Diabetes Atlas [Internt]. 5th edition. https://diabetesatlas.org/atlas/fifth-edition/. [Google Scholar]
- 4.OECD-FAO Agricultural Outlook 2011-2020. Organisation for Economic Co-operation and Development. 2011. https://stats.oecd.org/Index.aspx?DataSetCode=HIGH_AGLINK_2011.
- 5.Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, Mooradian AD, Wheeler ML.(2008) Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 31 Suppl 1: S61-S78. [DOI] [PubMed] [Google Scholar]
- 6.U. S. Department of Agriculture. (2012) US Choosemyplate 2012. https://www.myplate.gov/.
- 7.Pereira MA, Jacobs DR Jr., Van Horn L, Slattery ML, Kartashov AI et al. (2002) Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA 287: 2081-2089. doi: 10.1001/jama.287.16.2081. PubMed: 11966382. [DOI] [PubMed] [Google Scholar]
- 8.Toledo E, Delgado-Rodríguez M, Estruch R, Salas-Salvadó J, Corella D et al. (2009) Low-fat dairy products and blood pressure: follow-up of 2290 older persons at high cardiovascular risk participating in the PREDIMED study. Br J Nutr 101: 59-67. doi: 10.1017/S0007114508981496. PubMed: 18492300. [DOI] [PubMed] [Google Scholar]
- 9.Engberink MF, Geleijnse JM, de Jong N, Smit HA, Kok FJ et al. (2009) Dairy intake, blood pressure, and incident hypertension in a general Dutch population. J Nutr 139: 582-587. doi: 10.3945/jn.108.093088. PubMed: 19158223. [DOI] [PubMed] [Google Scholar]
- 10.van Meijl LE, Mensink RP (2011) Low-fat dairy consumption reduces systolic blood pressure, but does not improve other metabolic risk parameters in overweight and obese subjects. Nutr Metab Cardiovasc Dis 21: 355-361. doi: 10.1016/j.numecd.2009.10.008. PubMed: 20153619. [DOI] [PubMed] [Google Scholar]
- 11.Lutsey PL, Steffen LM, Stevens J (2008) Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation 117: 754-761. doi: 10.1161/CIRCULATIONAHA.107.716159. PubMed: 18212291. [DOI] [PubMed] [Google Scholar]
- 12.Abargouei AS, Janghorbani M, Salehi-Marzijarani M, Esmaillzadeh A (2012) Effect of dairy consumption on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Obes (Lond), 36: 1485–93. PubMed: 22249225. [DOI] [PubMed] [Google Scholar]
- 13.Liu S, Song Y, Ford ES, Manson JE, Buring JE et al. (2005) Dietary calcium, vitamin D, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes Care 28: 2926-2932. doi: 10.2337/diacare.28.12.2926. PubMed: 16306556. [DOI] [PubMed] [Google Scholar]
- 14.Snijder MB, van der Heijden AA, van Dam RM, Stehouwer CD, Hiddink GJ et al. (2007) Is higher dairy consumption associated with lower body weight and fewer metabolic disturbances? The Hoorn Study. Am J Clin Nutr 85: 989-995. PubMed: 17413097. [DOI] [PubMed] [Google Scholar]
- 15.Panagiotakos DB, Pitsavos CH, Zampelas AD, Chrysohoou CA, Stefanadis CI (2010) Dairy products consumption is associated with decreased levels of inflammatory markers related to cardiovascular disease in apparently healthy adults: the ATTICA study. J Am Coll Nutr 29: 357-364. doi: 10.1080/07315724.2010.10719852. PubMed: 21041810. [DOI] [PubMed] [Google Scholar]
- 16.Esmaillzadeh A, Azadbakht L (2010) Dairy consumption and circulating levels of inflammatory markers among Iranian women. Public Health Nutr 13: 1395-1402. doi: 10.1017/S1368980009992126. PubMed: 20003635. [DOI] [PubMed] [Google Scholar]
- 17.Mensink RP, Zock PL, Kester AD, Katan MB (2003) Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 77: 1146-1155. PubMed: 12716665. [DOI] [PubMed] [Google Scholar]
- 18.Hu FB, Stampfer MJ, Manson JE, Ascherio A, Colditz GA et al. (1999) Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr 70: 1001-1008. PubMed: 10584044. [DOI] [PubMed] [Google Scholar]
- 19.Kelemen LE, Kushi LH, Jacobs DR Jr., Cerhan JR (2005) Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol 161: 239-249. doi: 10.1093/aje/kwi038. PubMed: 15671256. [DOI] [PubMed] [Google Scholar]
- 20.Elwood PC, Strain JJ, Robson PJ, Fehily AM, Hughes J et al. (2005) Milk consumption, stroke, and heart attack risk: evidence from the Caerphilly cohort of older men. J Epidemiol Community Health 59: 502-505. doi: 10.1136/jech.2004.027904. PubMed: 15911647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.EUFIC. (2012) European Dietary Guidelines.https://www.eufic.org/en/.
- 22.American Heart Association Nutrition Committee, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, et al (2006) Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 114: 82-96. doi: 10.1161/CIRCULATIONAHA.106.617829. PubMed: 16785338. [DOI] [PubMed] [Google Scholar]
- 23.Australian Government National Health & Medical Research Council. (2012). Australian Guidelines to Healthy Eating. https://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating.
- 24.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM (2010) Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 91: 535-546. doi: 10.3945/ajcn.2009.27725. PubMed: 20071648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iggman D and Risérus U (2017) Role of Different Dietary Saturated Fatty Acids for Cardiometabolic Risk. J Clin Lipidol 6: 209-223. doi: 10.2217/clp.11.7. [DOI] [Google Scholar]
- 26.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336: 1117-1124. doi: 10.1056/NEJM199704173361601. PubMed: 9099655. [DOI] [PubMed] [Google Scholar]
- 27.Estruch R, Ros E, Salas-Salvado J, Covas MI et al. (2013) Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med 368: 1279-1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 28.Crichton GE, Howe PRC, Buckley JD, Coates AM, Murphy KJ (2012) Dairy consumption and cardiometabolic health: outcomes of a 12-month crossover trial. Nutr Metab (Lond) 9: 19. doi: 10.1186/1743-7075-9-19. PubMed: 22433747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barr SI, McCarron DA, Heaney RP, Dawson-Hughes B, Berga SL et al. (2000) Effects of increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. J Am Diet Assoc 100: 810-817. doi: 10.1016/S0002-8223(00)00236-4. PubMed: 10916520. [DOI] [PubMed] [Google Scholar]
- 30.Jadad AR, Caroll D (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1-12. doi: 10.1016/S0197-2456(96)90740-0. PubMed: 8721797. [DOI] [PubMed] [Google Scholar]
- 31.Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21: 2191-2192. doi: 10.2337/diacare.21.12.2191. PubMed: 9839117. [DOI] [PubMed] [Google Scholar]
- 32.Alonso A, Zozaya C, Vázquez Z, Alfredo Martínez J, Martínez-González MA (2009) The effect of low-fat versus whole-fat dairy product intake on blood pressure and weight in young normotensive adults. J Hum Nutr Diet 22: 336-342. doi: 10.1111/j.1365-277X.2009.00967.x. PubMed: 19486260. [DOI] [PubMed] [Google Scholar]
- 33.Manios Y, Moschonis G, Koutsikas K, Papoutsou S, Petraki I et al. (2009) Changes in body composition following a dietary and lifestyle intervention trial: The postmenopausal health study. Maturitas 62: 58-65. doi: 10.1016/j.maturitas.2008.11.005. PubMed: 19118956. [DOI] [PubMed] [Google Scholar]
- 34.Kukuljan S, Nowson CA, Bass SL, Sanders K, Nicholson GC et al. (2009) Effects of a multi-component exercise program and calcium-vitamin-D3-fortified milk on bone mineral density in older men: a randomised controlled trial. Osteoporos Int 20: 1241-1251. doi: 10.1007/s00198-008-0776-y. PubMed: 18958384. [DOI] [PubMed] [Google Scholar]
- 35.Ghadirian P, Shatenstein B, Verdy M, Hamet P (1995) The influence of dairy products on plasma uric acid in women. Eur J Epidemiol 11: 275-281. doi: 10.1007/BF01719431. PubMed: 7493659. [DOI] [PubMed] [Google Scholar]
- 36.Chee WS, Suriah AR, Chan SP, Zaitun Y, Chan YM (2003) The effect of milk supplementation on bone mineral density in postmenopausal Chinese women in Malaysia. Osteoporos Int 14: 828-834. doi: 10.1007/s00198-003-1448-6. PubMed: 12915959. [DOI] [PubMed] [Google Scholar]
- 37.Eagan MS, Lyle RM, Gunther CW, Peacock M, Teegarden D (2006) Effect of 1-year dairy product intervention on fat mass in young women: 6-month follow-up. Obesity (Silver Spring) 14: 2242-2248. doi: 10.1038/oby.2006.263. PubMed: 17189552. [DOI] [PubMed] [Google Scholar]
- 38.Gunther CW, Legowski PA, Lyle RM, McCabe GP, Eagan MS et al. (2005) Dairy products do not lead to alterations in body weight or fat mass in young women in a 1-y intervention. Am J Clin Nutr 81: 751-756. PubMed: 15817848. [DOI] [PubMed] [Google Scholar]
- 39.Lau EM, Woo J, Lam V, Hong A (2001) Milk supplementation of the diet of postmenopausal Chinese women on a low calcium intake retards bone loss. J Bone Miner Res 16: 1704-1709. doi: 10.1359/jbmr.2001.16.9.1704. PubMed: 11547841. [DOI] [PubMed] [Google Scholar]
- 40.Palacios C, Bertrán JJ, Ríos RE, Soltero S (2011) No effects of low and high consumption of dairy products and calcium supplements on body composition and serum lipids in Puerto Rican obese adults. Nutrition 27: 520-525. doi: 10.1016/j.nut.2010.02.011. PubMed: 20579848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stancliffe RA, Thorpe T, Zemel MB (2011) Dairy attentuates oxidative and inflammatory stress in metabolic syndrome. Am J Clin Nutr 94: 422-430. doi: 10.3945/ajcn.111.013342. PubMed: 21715516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tardy AL, Lambert-Porcheron S, Malpuech-Brugère C, Giraudet C, Rigaudière JP et al. (2009) Dairy and industrial sources of trans fat do not impair peripheral insulin sensitivity in overweight women. Am J Clin Nutr 90: 88-94. doi: 10.3945/ajcn.2009.27515. PubMed: 19474135. [DOI] [PubMed] [Google Scholar]
- 43.Wennersberg MH, Smedman A, Turpeinen AM, Retterstøl K, Tengblad S et al. (2009) Dairy products and metabolic effects in overweight men and women: results from a 6-mo intervention study. Am J Clin Nutr 90: 960-968. doi: 10.3945/ajcn.2009.27664. PubMed: 19710195. [DOI] [PubMed] [Google Scholar]
- 44.Zemel MB, Richards J, Milstead A, Campbell P (2005) Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes Res 13: 1218-1225. doi: 10.1038/oby.2005.144. PubMed: 16076991. [DOI] [PubMed] [Google Scholar]
- 45.Benatar JR, Jones E, White H, Stewart RAH (2014) A randomized trial evaluating the effects of change in dairy food consumption on cardio-metabolic risk factors. Euro. J. Preventive Cardiology. 21 (11): 1376-1386. doi: 10.1177/2047487313493567. [DOI] [PubMed] [Google Scholar]
- 46.Baran D, Sorensen A, Grimes J, Lew R, Karellas A et al. (1990) Dietary modification with dairy products for preventing vertebral bone loss in premenopausal women: a three-year prospective study. J Clin Endocrinol Metab 70: 264-270. doi: 10.1210/jcem-70-1-264. PubMed: 2294135. [DOI] [PubMed] [Google Scholar]
- 47.Gardner CD, Messina M, Kiazand A, Morris JL, Franke AA (2007) Effect of two types of soy milk and dairy milk on plasma lipids in hypercholesterolemic adults: a randomized trial. J Am Coll Nutr 26: 669-677. doi: 10.1080/07315724.2007.10719646. PubMed: 18187432. [DOI] [PubMed] [Google Scholar]
- 48.Zemel MB, Sun X, Sobhani T, Wilson B (2010) Effects of dairy compared with soy on oxidative and inflammatory stress in overweight and obese subjects. Am J Clin Nutr 91: 16-22. doi: 10.3945/ajcn.2009.28468. PubMed: 19889829. [DOI] [PubMed] [Google Scholar]
- 49.van Meijl LE, Mensink RP (2010) Effects of low-fat dairy consumption on markers of low-grade systemic inflammation and endothelial function in overweight and obese subjects: an intervention study. Br J Nutr 104: 1523-1527. doi: 10.1017/S0007114510002515. PubMed: 20579405. [DOI] [PubMed] [Google Scholar]
- 50.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A et al. (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364: 937-952. doi: 10.1016/S0140-6736(04)17018-9. PubMed: 15364185. [DOI] [PubMed] [Google Scholar]
- 51.Elwood PC, Pickering JE, Fehily AM (2007) Milk and dairy consumption, diabetes and the metabolic syndrome: the Caerphilly prospective study. J Epidemiol Community Health 61: 695-698. doi: 10.1136/jech.2006.053157. PubMed: 17630368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ et al. (2008) Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr 87: 1914-1925. PubMed: 18541585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O'Neil CE, Nicklas TA, Liu Y, Franklin FA (2009) The impact of dairy product consumption on nutrient adequacy and weight of Head Start mothers. Public Health Nutr 12: 1693-1701. doi: 10.1017/S1368980008003911. PubMed: 19000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Poddar KH, Hosig KW, Nickols-Richardson SM, Anderson ES, Herbert WG et al. (2009) Low-Fat Dairy Intake and Body Weight and Composition Changes in College Students. J Am Diet Assoc 109: 1433-1438. doi: 10.1016/j.jada.2009.05.005. PubMed: 19631052. [DOI] [PubMed] [Google Scholar]
- 55.Winkleby MA, Kraemer HC, Ahn DK, Varady AN (1998) Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988-1994. JAMA 280: 356-362. doi: 10.1001/jama.280.4.356. PubMed: 9686553. [DOI] [PubMed] [Google Scholar]
- 56.Chen M, Pan A, Malik VS, Hu FB (2012) Effects of dairy intake on body weight and fat: a meta-analysis of randomized controlled trials. Am J Clin Nutr 96: 735-747. doi: 10.3945/ajcn.112.037119. PubMed: 22932282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ludwig DS, Willett WC (2013) Three Daily Servings of Reduced-Fat Milk: An Evidence-Based Recommendation? JAMA Pediatr 167(9): 788-789 doi: 10.1001/jamapediatrics.2013.2408. [DOI] [PubMed] [Google Scholar]
- 58.National Institute for Health and Care Excellence. Type 2 diabetes: The management of type 2 diabetes. Published by: Royal College of Physicians. London. [Originally published 2009, last updated 2014]. https://www.nice.org.uk/guidance/cg87.
- 59.American Diabetes Association.(2013) Standards of Medical Care in Diabetes—2013. Diabetes Care 36 Suppl 1: S11-S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Atkinson FS, Foster-Powell K, Brand-Miller JC (2008) International tables of glycemic index and glycemic load values: 2008. Diabetes Care 31: 2281-2283. doi: 10.2337/dc08-1239. PubMed: 18835944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB (2005) Dairy consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med 165: 997-1003. doi: 10.1001/archinte.165.9.997. PubMed: 15883237. [DOI] [PubMed] [Google Scholar]
- 62.Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ et al. (2012) Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care 35: 434-445. doi: 10.2337/dc11-2216. PubMed: 22275443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.U.S. Department of Health and Human Services. (2010) Dietary guidelines for Americans. Office of Disease Prevention and Health Promotion. https://health.gov/sites/default/files/2020-01/DietaryGuidelines2010.pdf.
- 64.Mozaffarian D, Micha R, Wallace S (2010) Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLOS Med 7: e1000252. PubMed: 20351774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Truby H, Baic S, deLooy A, Fox KR, Livingstone MBE et al. (2006) Randomised controlled trial of four commercial weight loss programmes in the UK: initial findings from the BBC “diet trials”. BMJ 332: 1309-1314. doi: 10.1136/bmj.38833.411204.80. PubMed: 16720619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS et al. (2010) Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 341: c3691. doi: 10.1136/bmj.c3691. PubMed: 20671013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.The PLOS ONE Editors.(2023) Expression of Concern: Effects of High and Low Fat Dairy Food on Cardio-Metabolic Risk Factors: A Meta-Analysis of Randomized Studies. PLOS ONE [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prisma checklist.
(DOC)
Prisma flow chart.
(PDF)
Protocol.
(DOCX)