Abstract
We analyzed the 2009 Medicare inpatient claims data and other databases to estimate Medicare payments for primary or revision total knee arthroplasty (TKA). The average Medicare hospital payment per procedure was $13464 for primary TKA (n=227587) and $17331 for revision TKA (n=18677). For both primary and revision TKA Medicare payments varied substantially across patients, hospitals and healthcare markets. Less than one percent of primary TKA cases but seven percent of revision TKA cases triggered Medicare “outlier” payments, which were $10000 or higher per case beyond regular diagnosis-related-group payments. Urban and major teaching hospitals were more likely to treat these unusually expensive cases. Hospitals in the Northeast and West regions tended to receive higher Medicare payments than hospitals in the Midwest.
Keywords: total knee arthroplasty, Medicare, payment, outlier payment, revision TKA
INTRODUCTION
Total knee arthroplasty (TKA) is a common and safe surgery performed to relieve pain, restore function, and improve quality of life for patients with end-stage arthritis.1–6 The annual number of primary TKA procedures in the United States (US) is now close to 500,000 in recent years, of which sixty percent were performed in adults 65 years and older.7 During 1991–2010, the per-capita utilization among Medicare beneficiaries increased by 100 percent for primary TKA (60 operations per 10,000 Medicare population in 2010), and by over 50 percent for revision TKA (5.0 operations per 10,000 population in 2010).5 Total expenditures for TKA in the US were approximately $8 billion in 2006, making it one of the most expensive surgical procedures to individuals, insurers, and the government.8–10
Medicare, the single largest payer for inpatient care, reimburses hospitals for joint arthroplasties according to predetermined rates based on diagnosis-related groups (DRGs). Recognizing the substantially increased resource use imposed upon hospitals performing revision procedures and caring for medically complex patients, the Centers for Medicare and Medicaid Services (CMS) uses several DRG categories to reimburse separately primary and revision joint procedures that may be accompanied with major complications and comorbidities.11–16 In addition to the DRG-based prospective payments, the CMS makes extra payments (called outlier payments) for replacement procedures whose costs are extraordinarily high and exceed the DRG-based rate by a specified stop-loss amount.17
Although Medicare’s inpatient prospective payment system is designed to standardize payment for equivalent procedures performed among homogeneous patient subgroups, analyses have reported large variations in payment across hospitals, suggesting that the prospective payment system may not work precisely as intended. Of the limited number of studies evaluating such variations, most have focused on major cardiac and non-cardiac surgeries and few have evaluated Medicare payments for joint arthroplasty.18–21
Consequently, our objective was to estimate Medicare payments (both overall and outlier payments) for beneficiaries receiving total knee arthroplasty in 2009, with particular focus on payment variations over patients, major hospital types, and geographic regions. Our more general goal was to provide clinicians and policy makers with an improved understanding of how Medicare payments for TKA are calculated and how payments vary across the U.S.
METHODS
Data sources
The primary data source was the 2009 Medicare Provider Analysis and Review (MedPAR) 100% inpatient file obtained from the Centers for Medicare and Medicaid Services. The MedPAR contains uniformly abstracted administrative and clinical information about the acute care hospital stays of all fee-for-service beneficiaries. Patient-level records include age, gender, race/ethnicity, admission source (e.g. emergency department or transfer from other hospitals), principal and up to 9 secondary diagnoses classified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, principal and up to 5 secondary ICD-9-CM procedure codes, Medicare payments for inpatient stay, an encrypted patient identifier and a Medicare hospital identifier. Medicare payments in the MedPAR data are the actual payment made to the hospital by CMS for a given inpatient hospital stay. Several payment types are recorded for each patient including the regular payment for a given DRG, amount of outlier payment above and beyond the DRG-payment, and (depending on hospital types) extra payments related to a hospital’s disproportionate share of low income patients or graduate medical education. The precise formulas governing Medicare hospital payments are complex and have been published previously.17
The MedPAR was merged with several supplemental data bases including (1) the 2009 American Hospital Association (AHA) annual hospital survey file to obtain variables for hospital characteristics; (2) the University of Washington rural urban commuting area (RUCA) file to define rural vs. urban location of the hospital;22 (3) the Dartmouth Atlas of Healthcare file to define hospital care markets; and (4) the 2009 annual wage index file published by CMS to adjust for regional price differences.
Sample
We used the MedPAR to identify beneficiaries who underwent primary or revision TKA during 2009 (ICD-9-CM procedure codes 81.54 for primary and 80.06, 81.55, 00.80–00.84 for revision TKA).4,5,11 We applied several inclusion and exclusion criteria to the primary and revision groups. First, for both groups we excluded patients who were younger than sixty-five years of age since they were seriously disabled beneficiaries who differed from the general Medicare population. Second, we limited our cohort to the first primary (or revision) TKA performed on a given patient during any 30-day period of the year. We also excluded bilateral or second “staged” procedures that occurred within the 30-day window. This exclusion is necessary because Medicare data historically has not included “sidedness” for a specific procedure; thus, for a patient who underwent two primary TKA procedures in close temporal proximity, it is impossible to know if this represented an initial primary followed by an early complication requiring a second procedure or a planned bilateral (aka, staged) procedure. Third, as primary TKA is most often an elective procedure while revision TKA can be either an elective or more urgent procedure, we applied separate exclusion criteria to the primary and revision TKA populations in accordance with prior studies.5 For primary TKA we sequentially excluded patients admitted through the emergency department and patients admitted after transfer from another acute-care hospital, in order to focus on patients undergoing elective primary TKA. Our revision TKA group did not exclude these types of patients and thus included emergent or unscheduled cases for revision TKA because revision TKA is commonly a non-elective procedure.
Variables
Our primary outcome of interest was Medicare payments for each case; analyses were conducted separately for the primary and revision TKA cohort. Overall payments for each case were the sum of the outlier payment, if any, and the regular DRG-based payments.
We began by examining patient demographic characteristics including age in years, sex (female/male), and race (white, black, other) for the primary and revision TKA cohorts. We defined comorbid illnesses of the patient presented on the index admission using algorithms described by Elixhauser et al.23,24 which consider 30 specific conditions and exclude comorbid conditions that may represent complications of care or that are related to the primary reason for hospitalization.
We defined hospitals according to a number of key attributes including teaching status (major teaching hospital, minor teaching hospital, and non-teaching hospital), whether the hospital treated a disproportionate share (DSH) of low-income patients (high DSH [greater than the mean share of all hospitals], low DSH [less than the mean share of all hospitals], and non-DSH), and the geographic location of the hospital (rural versus urban). Finally, we mapped each hospital into one of 306 referral regions (HRRs) according to the Dartmouth Atlas of Health Care.25
Analyses
We first examined demographic characteristics, prevalence of key comorbid illnesses, and Medicare payments for primary and revision patients separately. Summary statistics including mean (standard deviation), median (interquartile range), and percentage as appropriate, were presented. Second, we examined mean Medicare payments for primary and revision TKA at both the patient and the hospital level. Payments were price-standardized where the regular DRG payment was calculated as the national DRG price multiplied by the specific DRG weight, and the outlier payment was standardized with a wage index factor using methods described before.17,26 The wage index for each metropolitan statistical area is updated annually by CMS to reflect regional price differences in labor inputs; the wage index was applied to the labor-related portion (estimated to be 75%) of outlier payments.
Third, we examined variation in hospital payments after stratifying hospitals according to teaching status, level of DSH payments, and urban/rural location; we examined how payments varied according to whether IME (indirect medical education) or DSH payments were or were not included. Fourth, we examined outlier payments; specifically we examined the proportion of hospitals that received and patients who qualified for outlier payments. We examined both the magnitude of the outlier payments and the proportion of cases within each hospital that qualified for outlier payments since, at least in theory, outlier payments offer hospitals an opportunity to obtain excess payments from Medicare. Again all analyses were conducted separately for primary and revision TKA.
Finally, we used graphical methods to examine variations of Medicare payments over hospital groups and over hospital referral regions. Price-adjusted payments (overall or outlier) were calculated for each type of hospitals or for each region, and for primary and revision TKA separately. All analyses were performed using SAS software version 9.2 (SAS Institute Inc, Cary, North Carolina). This project was approved by the Institutional Review Boards of University of Iowa and of University of Rochester Medical Center.
RESULTS
Our sample included 227587 Medicare patients receiving primary TKA and 18677 patients receiving revision TKA in 2009 (Table 1). Among those receiving primary TKA, the average age was 74 years; approximately sixty percent were female and ninety percent were White. In addition, twenty-two percent had comorbid diabetes and twelve percent were obese; the mean number of comorbidities was 2.1 per-patient. Similar demographic and diagnostic patterns were found for those receiving revision procedures.
Table 1.
Characteristics of Medicare beneficiaries receiving primary and revision TKA in 2009 (Patient Level)
| Primary TKA | Revision TKA | |
|---|---|---|
| Characteristics | ||
| No. of hospitalizations | 227587 | 18677 |
| Age, mean(SD), years | 74.1 (6.2) | 74.6 (6.5) |
| Sex, female, number (%) | 146520 (64.4) | 10824 (58.0) |
| Race | ||
| White, number (%) | 207119 (91.0) | 16786 (89.9) |
| Black, number (%) | 12001 (5.3) | 1314 (7.0) |
| Other, number (%) | 7848 (3.5) | 527 (2.8) |
| Missing, number (%) | 619 (0.3) | 50 (0.3) |
| Comorbidity | ||
| Diabetes, number (%) | 49703 (21.8) | 4540 (24.3) |
| CHF, number (%) | 8449 (3.7) | 1384 (7.4) |
| Obesity, number (%) | 27233 (12.0) | 1955 (10.5) |
| Renal failure, number (%) | 9719 (4.3) | 1274 (6.8) |
| Number of comorbid conditions, mean (SD) | 2.1 (1.4) | 2.3 (1.4) |
Table 2 shows that the total Medicare payment for primary TKA was $13464 on average (median=$12199) and varied substantially across patients even after adjustment for wage-differences across geographic regions (SD=$7415; interquartile rage [IQR] $11195-$14060). Medicare incurred outlier payments to hospitals for 1576 patients receiving primary TKA (<1% of all primary TKA patients), and the outlier payments added approximately $10000 to the regular DRG-based payment for these patients. The overall Medicare payment for revision TKA was $17331 on average (median=$15782) and varied substantially (SD=$10404; IQR $12484-$19656) across patients. Approximately 7% (n=1275) of all revision TKA cases triggered outlier payments which added approximately $12000 to the regular Medicare DRG-based payment (Table 2). For both primary and revision TKAs and compared to patients with only regular DRG payments, “outlier” patients tended to be male (41% vs 36% for primary TKA and 44% vs 42% for revision TKA) and to have higher rates of comorbid congestive heart failure (9.5% vs 3.7% and 11.4 vs 7.1%, respectively) and renal failure (6.5% vs 4.3% and 10.3% vs 6.6%, respectively).
Table 2.
Medicare hospital payments for primary and revision TKA at patient level
| Primary TKA | Revision TKA | |
|---|---|---|
| All Patients | (N=227587) | (N=18677) |
| Payment, Mean (Std) | 13463.8 (7414.6) | 17330.7 (10403.5) |
| Payment, Median (IQR) | 12199.0 (11195.0–14060.0) | 15782.0 (12484.0–19656.0) |
| Non-Outlier Patients | N=226011 (99.3%) | N=17402 (93.2%) |
| Payment, Mean (Std) | 13390.8 (7122.5) | 16486.3 (8289.3) |
| Payment, Median (IQR) | 12187.0 (11187.0–14014.0) | 15405.0 (12087.0–19067.0) |
| Outlier Patients | N=1576 (0.7%) | N=1275 (6.8%) |
| Payment, Mean (Std) | 23925.1 (23538.9) | 28856.3 (22481.6) |
| Payment, Median (IQR) | 16931.5 (13400.0–24393.5) | 22134.0 (17746.0–30811.0) |
Table 3 shows that overall Medicare payment for primary and revision TKA varied substantially across hospital subgroups and that medical education (IME) payments were substantial. For primary TKA, although the average total payment was $13723 for all hospitals (n=2924), the average payment was $17552 for major teaching hospitals (n=260; $15353 after excluding payment related to indirect medical education or IME), $14303 for minor teaching hospitals (n=473; $13763 after excluding IME payment), and $13146 for non-teaching hospitals (n=2137; $13089 after excluding IME payment). As would be expected, the average total payment for primary TKA was higher for hospitals treating the highest proportion of low-income patients (high DSH hospitals) than for other hospitals, but the difference largely disappeared after excluding the supplemental DSH payment. Note that the estimated payments for zero DSH hospitals tended to be slightly higher than those for low DSH hospitals which may be caused by differences in patient populations between the two types of hospitals, differences in other hospital or geographic factors, or simply chance variations. The average total payment for primary TKA was higher for urban hospitals (n=2056, $14185) than rural hospitals (n=779, $12738). The total Medicare payment for revision TKA varied in a similar pattern across these major hospital groups (Table 3).
Table 3.
Medicare hospital payments for primary and revision TKA (Hospital Level)
| Primary TKA | Revision TKA | |||
|---|---|---|---|---|
| All hospitals | N=2924 | N=2217 | ||
| Payment, Mean (Std) | 13722.8 (3307.6) | 17215.3 (7169.3) | ||
| Payment, Median (IQR) | 12911.7 (11720.1–14723.9) | 15797.3 (13492.8–19234.8) | ||
| Teaching Status | w/IME | w/o IME | w/IME | w/o IME |
| Major Teaching Hospitals | N=260 | N=235 | ||
| Payment, Mean (Std) | 17551.3 (4313.9) | 15352.4 (3785.2) | 22293.6 (6691.3) | 19595.0 (5906.4) |
| Payment, Median (IQR) | 16716.1 (14466.2–19566.2) | 14359.6 (12999.0–16715.4) | 20897.0 (18008.7–25688.0) | 18195.6 (15834.5–21917.8) |
| Minor Teaching Hospitals | N=473 | N=416 | ||
| Payment, Mean (Std) | 14302.3 (3791.3) | 13762.6 (3585.6) | 18058.3 (7924.8) | 17429.8 (7511.4) |
| Payment, Median (IQR) | 13507.0 (12399.3–15390.0) | 13023.3 (12030.8–14705.9) | 16654.8 (14126.3–19577.2) | 16002.7 (13796.4–18865.8) |
| Non Teaching Hospitals | N=2137 | N=1536 | ||
| Payment, Mean (Std) | 13145.8 (2625.5) | 13089.4 (2596.3) | 16190.7 (6346.5) | 16124.0 (6317.1) |
| Payment, Median (IQR) | 12538.9 (11523.4–13974.8) | 12478.4 (11507.9–13889.6) | 15087.7 (13054.3–17972.8) | 15044.9 (13008.4–17836.8) |
| DSH Status | w/DSH | w/o DSH | w/DSH | w/o DSH |
| High DSH | N=1131 | N=847 | ||
| Payment, Mean (Std) | 15231.9 (3743.9) | 12968.4 (2971.8) | 19582.9 (8431.9) | 16871.1 (7683.5) |
| Payment, Median (IQR) | 14231.3 (12853.9–16757.6) | 12412.5 (11159.7–14026.0) | 17902.1 (15109.5–22263.0) | 15529.9 (13139.0–18883.7) |
| Low DSH | N=1134 | N=854 | ||
| Payment, Mean (Std) | 12685.0 (1999.1) | 12065.0 (2011.2) | 15389.8 (4831.6) | 14710.5 (4769.4) |
| Payment, Median (IQR) | 12346.0 (11498.9–13537.4) | 11743.5 (10874.3–12891.6) | 14794.0 (12869.0–17332.7) | 14082.3 (12238.0–16566.5) |
| Zero DSH | N=659 | N=516 | ||
| Payment, Mean (Std) | 12918.9 (3350.8) | 12918.9 (3350.8) | 16350.0 (7085.9) | 16350.0 (7085.9) |
| Payment, Median (IQR) | 12078.4 (11039.9–13697.9) | 12078.4 (11039.9–13697.9) | 14719.1 (12560.1–17692.2) | 14719.1 (12560.1–17692.2) |
| Rural/Urban | ||||
| Urban | N=2056 | N=1684 | ||
| Patient Payment, Mean (Std) | 14184.7 (3443.7) | 17610.3 (6806.2) | ||
| Patient Payment, Median (IQR) | 13287.3 (12039.7–15316.2) | 16105.7 (13843.4–19696.5) | ||
| Rural | N=779 | N=488 | ||
| Patient Payment, Mean (Std) | 12737.9 (2153.2) | 15908.2 (7340.1) | ||
| Patient Payment, Median (IQR) | 12241.0 (11405.0–13437.0) | 14810.5 (12864.4–17317.2) | ||
IME: Indirect Medical Education;
DSH: Disproportionate share;
High DSH hospitals were defined as hospitals with DSH payments higher than the average for all hospitals, low DSH hospitals were defined as hospitals with DSH payments lower than the average for all hospitals, and hospitals of zero DSH were hospitals did not receive any DSH payment.
Table 4 shows outlier payments for both primary and revision TKA. For primary TKA, twenty-four percent of hospitals (n=707) received outlier payment for one or more patients at an average of $8326; the median rate of patients triggering outlier payment in these hospitals was 1.6% (IQR 0.9–4.0%). These figures varied considerably across hospital groups. For example, the average outlier payment was $14749 for major teaching hospitals, $8690 for minor-teaching hospitals, and $7384 for non-teaching hospitals. Similarly, the average outlier payment was $11062 for high-DSH hospitals, $7541 for low-DSH hospitals, and $6126 for non-DSH hospitals.
Table 4.
Medicare hospital Outlier payments for primary and revision TKA (Hospital Level)
| Primary TKA (N=2924 hospitals) | Revision TKA (N=2217 hospitals) | |
|---|---|---|
| Hospital receiving Outlier Payment, No (% of total) | 707 (24.2) | 644 (29.0) |
| % of hospitalizations receiving outlier payments (among all hospitals), Median (IQR) | 0 (0–0) | 0 (0–6.1) |
| % of hospitalizations receiving outlier payments (among hospitals receiving outlier payments only), Median (IQR) | 1.6 (0.9–4.0) | 17.0 (10.0–33.3) |
| Outlier Payment, Mean (95% CI) | 8326.1 (7410.8, 9241.4) | 8020.4 (7172.5, 8868.3) |
| Teaching Status | ||
| Major Teaching Hospitals | N=260 | N=235 |
| Hospital receiving Outlier Payment, No (%) | 74 (28.5) | 89 (37.9) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0.4) | 0 (0–7.1) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.0 (0.6–1.5) | 10.0 (5.3–15.4) |
| Outlier Payment, Mean (95% CI) | 14748.6 (10142.8, 19354.5) | 11931.7 (9067.5, 14795.9) |
| Minor Teaching Hospitals | N=472 | N=416 |
| Hospital receiving Outlier Payment, No (%) | 119 (25.2) | 149 (35.8) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0.2) | 0 (0–8.6) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.1 (0.6–1.9) | 14.3 (7.7–24.2) |
| Outlier Payment, Mean (95% CI) | 8690.2 (6773.4, 10607.0) | 8684.7 (6968.1, 10401.3) |
| Non Teaching Hospitals | N=2135 | N=1539 |
| Hospital receiving Outlier Payment, No (%) | 506 (23.7) | 397 (25.8) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0) | 0 (0–4.2) |
| % of outlier patients (outlier hospitals), Median (IQR) | 2.0 (1.0–5.9) | 22.2 (13.0–35.7) |
| Outlier Payment, Mean (95% CI) | 7383.5 (6410.6, 8356.4) | 6613.4 (5789.8, 7437.1) |
| DSH Status | ||
| High DSH | N=1130 | N=848 |
| Hospital receiving Outlier Payment, No (%) | 234 (20.7) | 223 (26.3) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0) | 0 (0–3.6) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.5 (0.9–3.0) | 16.7 (9.1–26.5) |
| Outlier Payment, Mean (95% CI) | 11062.0 (8972.1, 13151.8) | 10194.6 (8262.4, 12126.8) |
| Low DSH | N=1132 | N=854 |
| Hospital receiving Outlier Payment, No (%) | 283 (25.0) | 257 (30.1) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0) | 0 (0–7.7) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.7 (0.9–4.2) | 18.2 (10.0–33.3) |
| Outlier Payment, Mean (95% CI) | 7541.4 (6276.1, 8806.7) | 7231.9 (6162.7, 8301.1) |
| Zero DSH | N=660 | N=516 |
| Hospital receiving Outlier Payment, No (%) | 190 (28.8) | 164 (31.8) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0.5) | 0 (0–8.3) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.7 (0.7–6.5) | 20.0 (10.0–40.0) |
| Outlier Payment, Mean (95% CI) | 6125.6 (5018.5, 7232.7) | 6299.6 (5184.7, 7414.5) |
| Rural/Urban | ||
| Urban | N=2053 | N=1686 |
| Hospital receiving Outlier Payment, No (%) | 544 (26.5) | 511 (30.3) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0.3) | 0 (0–6.4) |
| % of outlier patients (outlier hospitals), Median (IQR) | 1.4 (0.7–3.0) | 16.7 (8.3–28.6) |
| Outlier Payment, Mean (95% CI) | 9318.1 (8205.4, 10430.8) | 8272.3 (7394.8, 9149.8) |
| Rural | N=781 | N=488 |
| Hospital receiving Outlier Payment, No (%) | 153 (19.6) | 120 (24.6) |
| % of outlier patients (all hospitals), Median (IQR) | 0 (0–0) | 0 (0–0) |
| % of outlier patients (outlier hospitals), Median (IQR) | 3.1 (1.5–7.7) | 33.3 (16.7–50.0) |
| Outlier Payment, Mean (95% CI) | 5137.8 (3762.6, 6512.9) | 6068.2 (4406.6, 7729.7) |
A larger percentage of urban hospitals received outlier payments from Medicare than rural hospitals (26.5% versus 19.6%). Among urban hospitals receiving outlier payments, the median percentage of patients in the hospital triggering the outlier payment was 1.4% (IQR 0.7–3.0%), resulting in an average of $9318 extra payment per case; while among rural hospitals receiving outlier payments, the median percentage of patients in the hospital triggering the outlier payment was 3.1% (IQR 1.5–7.7%), and was 3.1% for rural hospitals, resulting in an average of $5138 outlier payment per case.
For revision TKA, twenty-nine percent of hospitals (n=644) received outlier payment at an average payment of $8020, and the median rate of patients triggering outlier payment in these hospitals was 17% (IQR 10.0–33.3%). In a similar pattern to that of primary TKA, the outlier payment for revision TKA varied dramatically across hospital groups defined by teaching status, DSH-status, or rural/urban location (Table 4).
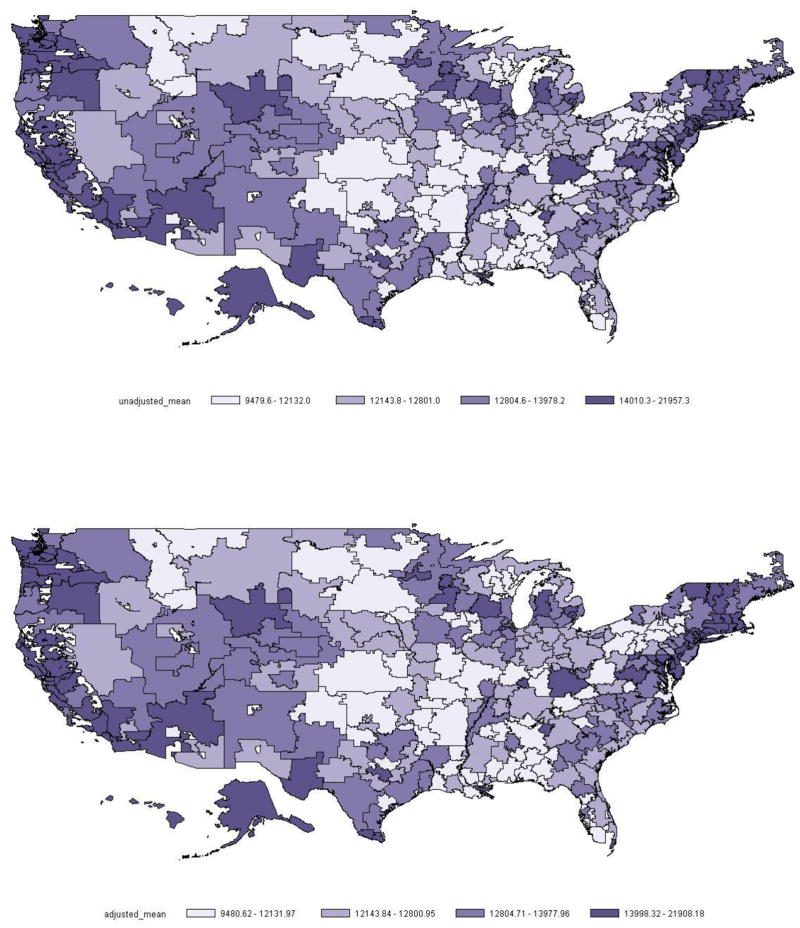
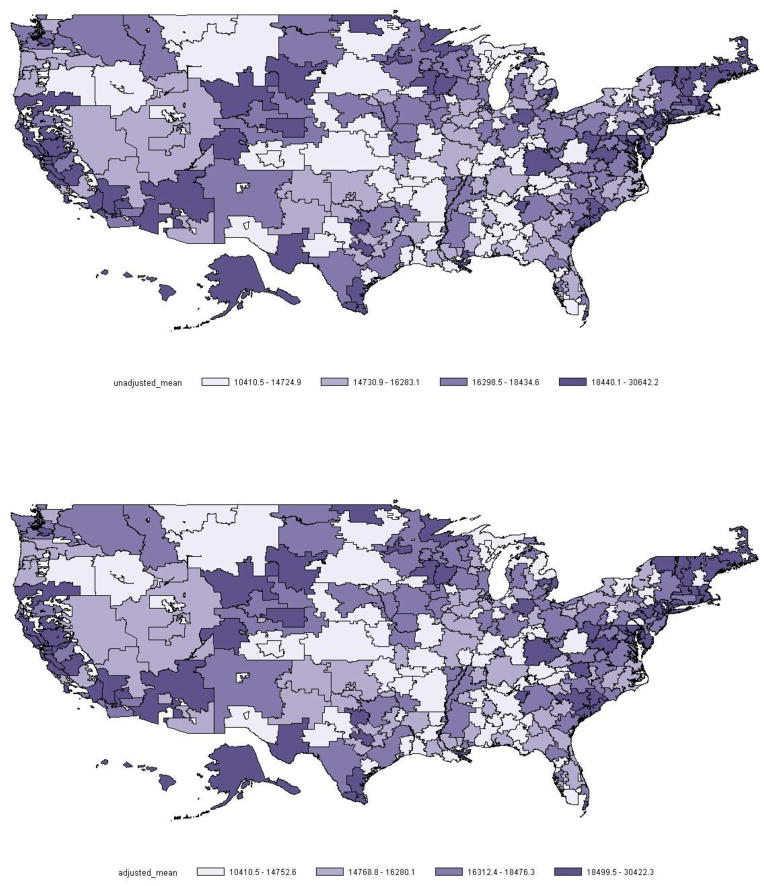
Figures 1 and 2 present the distributions of overall Medicare payment across HRRs for primary and revision TKA respectively (panel A for unadjusted payment and panel B for adjusted payment). Estimates suggested large geographic variations in Medicare payment for both procedures. For example, the average payments were $9481–12132 for HRRs in the lowest quartile and $13998–21908 for HRRs in the highest quartile for primary TKA, while the average payments were $10411–14753 and $18500–30423, respectively, for revision TKA. For both primary and revision procedures, Medicare seemed to pay higher rates to hospitals in the Northeast and West regions than most hospitals in the Midwest, even after adjustment for regional price differences.
Figure 1.
HRR Level of unadjusted (top) and adjusted (bottom) mean payment for primary TKA
Figure 2.
HRR Level of unadjusted (top) and adjusted (bottom) mean payment for revision TKA
DISCUSISON
In this study of older Medicare patients receiving total knee arthroplasty in 2009, we found that the average Medicare payment for primary TKA was $13464 and $17331 for revision TKA. However, for both primary and revision TKA Medicare payments varied substantially across patients, hospitals and healthcare markets in both anticipated and unexpected ways. Less than one percent of primary TKA cases but nearly seven percent of revision TKA cases triggered Medicare “outlier” payments and these payments averaged approximately $8000 per-case. Urban and major teaching hospitals were more likely to treat these unusually expensive cases, and Medicare spending (both overall and outlier reimbursement) to these hospitals tended to be higher than other hospitals. Finally, hospitals in the Northeast and West regions tended to receive higher Medicare payments than hospitals in the Midwest even after adjustment for differences in the prevailing wage-index.
Our estimate that Medicare reimbursement for revision TKA was-on average–approximately $4000 higher than primary TKA is consistent with the evidence showing higher hospital resource use for revision TKA, and with recent changes of Medicare payment policies to better cover hospital costs associated with revision procedures.11–14,16 Medicare historically paid all lower extremity arthroplasty cases under a single DRG weight regardless of primary or revision procedures. However, a large body of literature has documented relatively higher resource consumption for revision arthroplasty due to increased intensity and complexity of the procedure (e.g. multi-component revisions), higher implant costs, prolonged operative time and hospital stay, and increased risk for infections or other major perioperative complications. In response to these data, Medicare revised its payment scheme and started using separate DRGs to reimburse primary and revision joint arthroplasty in 2005,11 assigning a higher price weight to revision than primary procedures. In addition, the current version of DRGs (Medicare severity DRGs or MS-DRGs) adjusts per discharge payment for severity of disease (comorbidities and/or complications) in order to ensure that patients within each MS-DRG group are clinically similar and require comparable level of inpatient resources.17 We would argue that it remains an open issue whether the incremental payment for revision TKA is enough given the substantial difference in complexity and resource use for revision cases when compared to primary procedures.
Despite the relatively standard Medicare payment scheme, our analyses over all patients revealed a large variation of the severity- and price-adjusted payment for primary TKA (e.g. interquartile range from roughly $11k to $14k), and an even larger variation for revision TKA (e.g. interquartile range $12k – $20k). Further analyses at the hospital and region levels suggested that part of these variations across individuals might have resulted from Medicare’s intentional differences in payments to different hospitals or hospitals in different regions. For example, Medicare pays direct and indirect supplements to teaching hospitals for their graduate medical education, and extra amounts to hospitals caring for disproportionate numbers of low-income patients. Our stratified analyses demonstrate that the typical teaching hospital would receive an incremental $2000 per-case and hospitals treating a high proportion of lower income patients (high DSH) would receive an incremental $2500 per-case). Moreover, our analyses of urban versus rural hospitals and analyses at the HRR level (showing lowest payments for most rural HRRs in the Midwest) are consistent with the fact that in general Medicare pays hospitals in rural areas at lower rates than to hospitals in metropolitan areas. It remains an open question whether these incremental payments are too much, too little, or just right.
Nonetheless, even after accounting for these intended differences, our estimates within each group of hospitals continued to show large variations in reimbursement amount. For example, for primary TKA, the interquartile ranges of payment were $13k-$17k within major teaching hospitals, $12k-15k within minor teaching hospitals, and $11.5k-$14k for non-teaching hospitals (all excluding payments for medical education); for revision TKA procedures, the corresponding ranges were $16k-$22k, $14k-$19k, and $13k-$18k respectively. These “unexplained” variations in spending are consistent with estimates from recent reports,18,19,21,26 and may be driven by differences in hospital billing and accounting practices. However, evidence suggests that such variations could also be driven, at least partially, by variations in potentially discretionary inpatient service use such as laboratory tests, supplies administered to the patient, and inpatient consultations by critical care physicians or other specialists.27,28 Thus, our findings of large variations in TKA spending for all hospital groups and across healthcare markets suggest considerable room for hospitals to improve their cost efficiency for total joint arthroplasty procedures.10,29
The finding that a much higher percentage of revision cases than primary TKA cases (7% versus <1%) triggered Medicare outlier payments is likely due to the fact that compared to patients undergoing primary TKA, those having revision knee procedures tend to be more complicated cases, with certain revision procedures such as those performed for deep infection, being exceptionally expensive.12–14 The more intense resource utilization for revision procedures in general and the extra hospital expenses incurred in highly-complicated revision cases in specific, have been reported to exert substantial economic burdens on centers performing many of these revision cases. Thus, the CMS’s outlier payment mechanism helps prevent huge financial losses for these hospitals and ensure appropriate access to revision procedures for these clinically complex cases. This is critical in that our estimates of the Medicare data showed that over one fourth of hospitals treated at least one “outlier” patient while among these hospitals, seventeen percent of their revision cases were extremely costly and triggered outlier payments (average amount $8020 per case). Further analyses showed that compared to non-teaching hospitals, major teaching hospitals were found to be more likely to have treated highly-complex revision cases (38% versus 26%) and on average received almost twice as high outlier payments per case ($11931 versus $6613). These findings are consistent with our anticipation that complex revision cases tend to be referred to tertiary care centers with teaching commitment and incur higher costs there. In contrast, our analyses on hospitals of different disproportionate groups or urban versus rural hospitals revealed less dramatic variations in outlier payment patterns.
Although Medicare’s outlier payment policy is important to guarantee equitable reimbursement for knee arthroplasty, the CMS has recently tightened restrictions on and substantially reduced the amount of outlier payments over time, with concerns that some hospitals may use this mechanism to overbill the Medicare program and that outlier payments may be associated with potentially avoidable complications.20,30 Our data suggest that the more restricted payment policies would affect a large number of hospitals performing complex revision knee arthroplasty, and may create financial disincentives for hospitals to continue their high standard of care for revision TKA. These issues of appropriate access and quality for TKA revision surgery may become more salient with the projected increases in volume of orthopaedic patients requiring revision procedures in the future.2–4
We acknowledge several potential limitations of our study. First, this study focused on Medicare payments for TKA. These estimates are important since Medicare pays for approximately 60% of all total knee replacements in the US. Nonetheless, our analyses on the reimbursement amount, its variations, and policy implications, may or may not be generalized to other insurance programs. Second, our estimates were limited to Medicare payment to hospitals for TKA surgery, but did not include physician fees during hospitalization or rehabilitation and other post-acute care expenditures after discharge. However, it has been shown that inpatient care spending accounts for a large portion of the total acute and post-acute care expenditures for knee or hip replacement procedures.14,16,19 Finally, our study relied on large administrative data of the Medicare program and similar to other studies of this type, are subject to the potential issues of such data including issues related to the accuracy and completeness of diagnoses, coding of procedures, and recording of payment amounts and types.31
In sum, our study suggests that for older patients receiving total knee arthroplasty, Medicare payments to hospitals varied substantially over individuals, hospitals and healthcare markets. A portion of revision knee procedures were extremely costly to hospitals and the Medicare program. Changes in Medicare payment policies may have direct and indirect impacts on hospital finance and patient access to total knee arthroplasty.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005 Jul;87(7):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Jain NB, Higgins LD, Ozumba D, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005 Dec;52(12):3928–3933. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 4.Lu X, Hagen TP, Vaughan-Sarrazin MS, Cram P. The impact of new hospital orthopaedic surgery programs on total joint arthroplasty utilization. J Bone Joint Surg Am. 2010 Jun;92(6):1353–1361. doi: 10.2106/JBJS.I.00833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012 Sep 26;308(12):1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997 Dec;345:134–139. [PubMed] [Google Scholar]
- 7.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National health statistics reports number 29: National hospital discharge survey 2007 summary. Oct 26, 2010. [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Health, United States, 2009: With special feature on medical technology. Hyattsville: 2009. [PubMed] [Google Scholar]
- 9.Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009 Jun 22;169(12):1113–1121. doi: 10.1001/archinternmed.2009.136. discussion 1121–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson NA, Schneller ES, Montgomery K, Bozic KJ. Hip and knee implants: current trends and policy considerations. Health Aff (Millwood) 2008 Nov-Dec;27(6):1587–1598. doi: 10.1377/hlthaff.27.6.1587. [DOI] [PubMed] [Google Scholar]
- 11.Bozic KJ, Rubash HE, Sculco TP, Berry DJ. An analysis of medicare payment policy for total joint arthroplasty. J Arthroplasty. 2008 Sep;23(6 Suppl 1):133–138. doi: 10.1016/j.arth.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 12.Lavernia C, Lee DJ, Hernandez VH. The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res. 2006 May;446:221–226. doi: 10.1097/01.blo.0000214424.67453.9a. [DOI] [PubMed] [Google Scholar]
- 13.Bozic KJ, Durbhakula S, Berry DJ, et al. Differences in patient and procedure characteristics and hospital resource use in primary and revision total joint arthroplasty: a multicenter study. J Arthroplasty. 2005 Oct;20(7 Suppl 3):17–25. doi: 10.1016/j.arth.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 14.Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005 Aug;87(8):1746–1751. doi: 10.2106/JBJS.D.02937. [DOI] [PubMed] [Google Scholar]
- 15.Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005 Mar;87(3):570–576. doi: 10.2106/JBJS.D.02121. [DOI] [PubMed] [Google Scholar]
- 16.Lavernia CJ, Drakeford MK, Tsao AK, Gittelsohn A, Krackow KA, Hungerford DS. Revision and primary hip and knee arthroplasty. A cost analysis. Clin Orthop Relat Res. 1995 Feb;311:136–141. [PubMed] [Google Scholar]
- 17.MedPAC. Payment Basics: Hospital acute inpatient services payment system. The Medicare Payment Advisory Commission; Oct, 2011. [Google Scholar]
- 18.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012 Mar 22;366(12):1075–1077. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff (Millwood) 2011 Nov;30(11):2107–2115. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baser O, Fan Z, Dimick JB, Staiger DO, Birkmeyer JD. Outlier payments for cardiac surgery and hospital quality. Health Aff (Millwood) 2009 Jul-Aug;28(4):1154–1160. doi: 10.1377/hlthaff.28.4.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010 Dec;45(6 Pt 1):1783–1795. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rural health research center RUCA data version 2.0. 2005 http://depts.washington.edu/uwruca/ruca-data.php.
- 23.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 25.The Dartmouth Atlas for Health Care. http://www.dartmouthatlas.org.
- 26.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood) 2010 Mar-Apr;29(3):537–543. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen SI, Dharmarajan K, Kim N, et al. Procedure intensity and the cost of care. Circ Cardiovasc Qual Outcomes. 2012 May;5(3):308–313. doi: 10.1161/CIRCOUTCOMES.112.966069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pham HH, Devers KJ, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005 Feb;20(2):101–107. doi: 10.1111/j.1525-1497.2005.40184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bozic KJ, Smith AR, Mauerhan DR. Pay-for-performance in orthopedics: implications for clinical practice. J Arthroplasty. 2007 Sep;22(6 Suppl 2):8–12. doi: 10.1016/j.arth.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 30.The Centers for Medicare and Medicaid Services. [Accessed August 14, 2012];Outlier payments. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/outlier.html.
- 31.Bozic KJ, Chiu VW, Takemoto SK, et al. The validity of using administrative claims data in total joint arthroplasty outcomes research. J Arthroplasty. 2010 Sep;25(6 Suppl):58–61. doi: 10.1016/j.arth.2010.04.006. [DOI] [PubMed] [Google Scholar]