Abstract
PURPOSE
This paper describes the systematic construction and psychometric analysis of a knowledge assessment instrument for phase II cardiac rehabilitation (CR) patients measuring risk modification disease management knowledge and behavioral outcomes derived from national standards relevant to secondary prevention and management of cardiovascular disease.
METHODS
First, using adult curriculum based on disease specific learning outcomes and competencies, a systematic test item development process was completed by clinical staff. Second, a panel of educational and clinical experts used an iterative process to identify test content domain and arrive at consensus in selecting items meeting criteria. Third, the resulting 31 question instrument the Cardiac Knowledge Assessment Tool (CKAT) was piloted in CR patients to insure utility of application. Validity and reliability analysis were performed on 3,638 adult pre test administrations with additional focused analyses on 1,999 individuals completing both pre and post treatment administrations within 6 months.
RESULTS
Evidence of CKAT content validity was substantiated with 85% agreement among content experts. Evidence of construct validity was demonstrated via factor analysis identifying key underlying factors. Estimates of internal consistency, e.g. Cronbach’s Alpha = .852 and a Spearman-Brown split-half reliability = .817 on pre testing, supports test reliability. Item analysis, using point biserial correlation, measured relationships between performance on single items and total score (p<.01). Analyses utilizing item difficulty and item discrimination indices further verified item stability and validity of the CKAT.
CONCLUSIONS
A knowledge instrument specifically designed for an adult CR population was systematically developed and tested in a large representative patient population, satisfying psychometric parameters including validity and reliability.
Keywords: Heart Disease, Prevention and Control, Health Care Evaluation Mechanisms, Educational Measurement, Cardiac Rehabilitation
Advances in the early recognition and aggressive medical treatment of cardiac disease have led to a sharp decrease in mortality in the predominately older adult population at risk1. As mortality figures have decreased an increased burden has been placed on the health care system to provide the necessary preventive tools to effect long-term disease self-management in this large patient cohort2. These same advances in the early recognition and aggressive medical treatment of cardiac events coupled with the dramatic decrease in time of hospital stay have limited in-hospital patient education. There is also evidence of a fundamental inability of the adult patient and family to comprehend the behaviors required of them to improve long-term health outcomes during an acute period of physical and psychological stress typical of post procedural inpatient hospital care3. During this shortened immediate post recovery period both patients’ and families’ perceived learning needs are directed at effecting survival of the serial event and not secondary preventive strategies4. The goal of outpatient cardiac rehabilitation (CR) from its initial inception has been to return the patient to optimal physical and psychosocial functional status post cardiac illness. Contemporary CR programs employ substantial resources teaching risk factor and disease management strategies. To this end education programs are formulated to help patients modify high-risk behaviors and assume personal responsibility for long-term disease management5. Results are encouraging; meta-analyses have revealed a 34% reduction in cardiac mortality and 29% reduction in recurrent myocardial infarction in CR settings where these focused psychoeducational programs have shown to be most effective6. Many CR programs have developed “home-grown” assessment tools to measure baseline disease and risk knowledge as well as quantify gains. Lacking is a test specifically developed and validated in the target population. Although instruments have been systematically developed to measure general knowledge in a variety of other cardiovascular settings they want for specificity of purpose and application in both pre and post testing CR use7,8,9. In a more focused CR cliental Smith et al designed a 40 item test with good reliability and validity results10. However, design flaws included: development in a small, non representative sample of male phase II & III CR participants with & without diagnosed CAD; inclusion of a pilot-group of 38 spouses; and a Flesh Kincaide reading grade level of 11.3 and reading ease of 41.6 (both well outside the recommend levels of 8th grade or lower and readability ease of 75, respectively)11–13. Also, test items included program specific knowledge including entry requirements, cardiopulmonary resuscitation technique and type A and B behavior analysis, further limiting general application. Missing were objective questions focused on specific, nationally established disease management goals including lipids, blood pressure, exercise, diabetes, diet and CHF management criteria14. More recently Bergman et al. developed a psychometrically sound test which claimed useful application in “adult populations” however, the test was developed using an urban undergraduate student cohort. A follow-up comparative study by the authors using an older adult cohort, mean age 57yrs., demonstrated a negative association between subject age and test score further calling into question the use of young adults in the original design, validation and interpretation of the instrument. Furthermore, a lack of specific focus on CAD risk modification and disease management knowledge limits utility of this instrument in CR adult clientele15.
Methods
Project overview
This work’s primary purpose was development and deployment of a valid clinical assessment tool for this specific adult patient population. The design strategy we describe was first validated as a clinical improvement project in a focused representative sample of 50 CR patients from 2000–2001. With local IRB approval, the results of this developmental project were expanded to include an additional 114 test applications which completed pilot analysis in 2002. During the ensuing years 2002–2011 this instrument fulfilled its primary goal of measuring clinically relevant knowledge in our patients thus enabling effective individual and group educational remediation. In January of 2011, with local IRB approval, we retrospectively conducted in-depth analysis to further validate its application and make any necessary psychometric adjustments to its construct.
Design approach
The formative stage of the project was initially influenced by the model developed by Gastafson and Branch (1997) which enumerates four major activities consistent of effective adult instructional development (AID). First, analysis (of the setting and learner needs); Second, design of a set of specifications for an effective, efficient, and relevant learner environment; Third, development of all learner and delivery materials and; Fourth, evaluation16. Richey (1986) also identified six core elements of AID that also influenced our design approach: (1) Determine learner needs; (2) Determine goals and objectives; (3) Construct assessment procedures; (4) Design/select delivery approaches; (5) Try-out instructional system; (6) Install and maintain system17.These models form the foundation of the World Wide Instructional Design System (WIDS) whose curriculum and evaluative models mandate a structured process with a primary focus on: Who the learners are (adults 40–85yrs.); What they need to know (heart disease risk and disease management knowledge and skills); When learning objectives are met (learning time lines); and How they’re going to get there (instructional strategies). The process then involves matching learning competencies to achievement criteria in an iterative item development format prior to piloting the test in the target population and performing reliability analyses18. Our work was purposed to follow this design utilizing a multidisciplinary team of experts including professionals representing nursing, medicine, exercise physiology, dietetics, pharmacy, psychology and adult education… then pilot, and rigorously investigate the designed psychometric constructs over time in our large CR patient population.
Test Construction
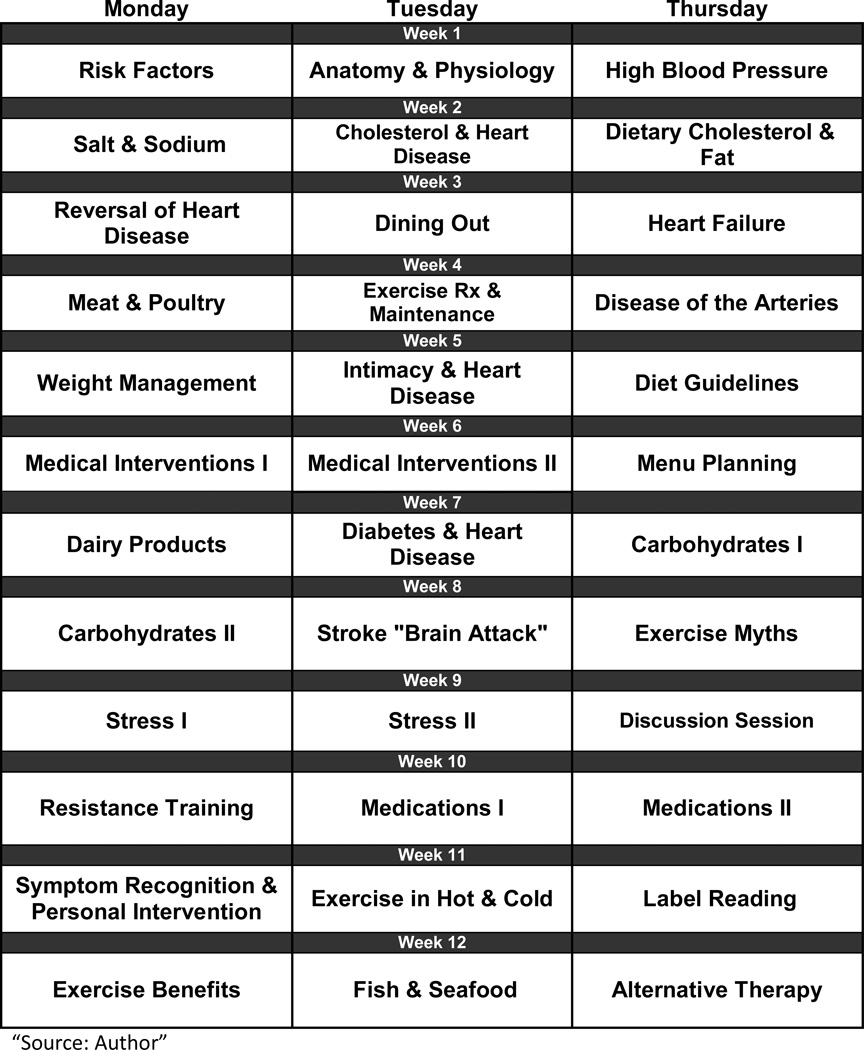
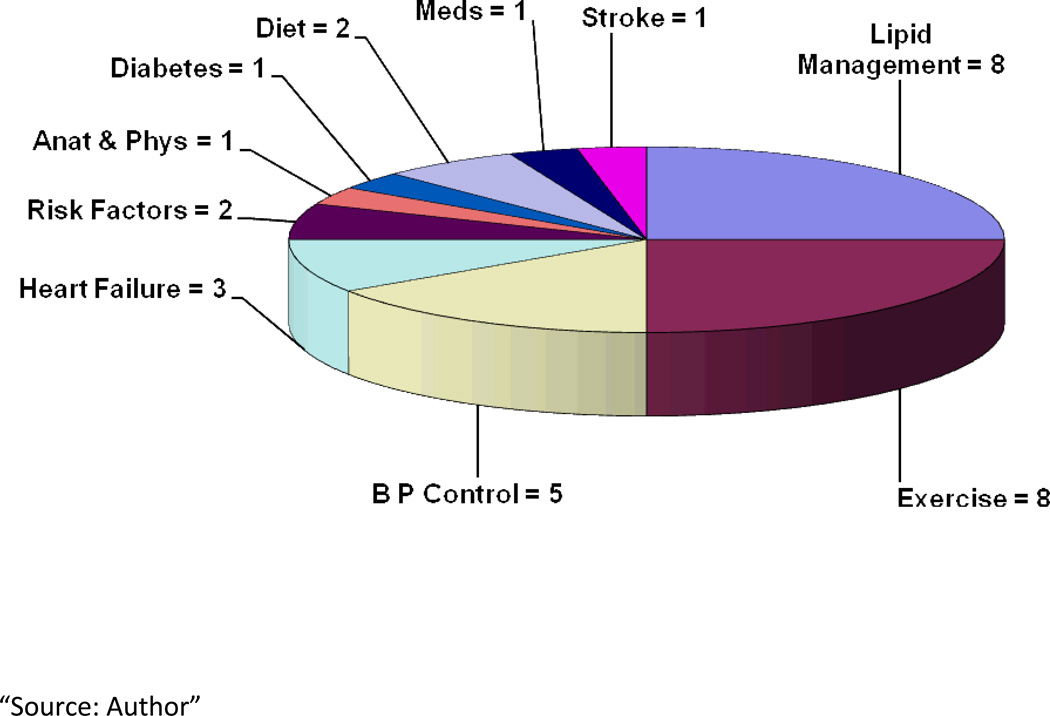
Instrument development was initiated in May of 2000 by multidisciplinary members of our program’s CR staff (SCR) using a systematic process suggested by Grant and Davis that involves step-wise content domain identification, item generation and instrument construction19–22. Developers adhered to a process, pioneered by Bloom (1956) and refined by (Anderson 2010), which recognizes a taxonomy of learning objectives within cognitive and affective learning domains20–22. Test item development focused on Bloom’s foundation learning objectives of knowledge, comprehension and application, all fundamental evaluative milestones in realizing the ultimate goal of behavioral change. The SCR program’s core curriculum consists of 36 instructional modules (Figure 1) developed according to guidelines established by the American Heart Association and American College of Cardiology for secondary prevention of heart disease and lifetime maintenance of heart healthy lifestyle practices23. We followed the process that Lynn, 1986 defines content validity as “the determination of the content representativeness or content relevance of the elements/items of an instrument”. The two stage process first involved a structured developmental stage followed by a quantification stage24. During the developmental stage SCR staff, utilizing their cumulative experience with the teaching plan objectives contained in each module were challenged to identify focused curriculum domains specific to desired learner based competencies and outcomes. Ten learning content domains evolved as a result of this process: 1) blood pressure control; 2) lipid management; 3) exercise; 4) heart failure; 5) cardiovascular disease risk; 6)medications; 7) anatomy & physiology; 8) diet; 9) diabetes and 10) stroke (Figure 2). Next, the SCR staff generated teaching plans with specific objectives and curriculum content for the individual teaching sessions contained within the ten identified learning domains. Test items were then systematically developed to measure desired competencies and objectives specific to each key learning domain. A pool of test items was constructed by working from a list of instructional objectives weighted to approximate and prioritize importance within each learning content domain. Care was taken to ensure that teaching content and learning objectives were tested in proportion to the relative importance they received during group instruction and individual remediation. Item relevance was then determined using a content validity index (CVI). Items were individually scored by the eight SCR developers on a 4-point scale of; 1= not relevant, 2=somewhat relevant, 3=quite relevant, 4=highly relevant. Scores above 1 connoted relevance. Item inclusion scores required .85 agreement among the CR raters24, 25. From this item pool developers then weighted learning domain complexity based on a five point Likert scale from easy to difficult. Difficult domains, which required multiple learning objectives and more complex behavioral mastery, were thereby systematically allotted sufficient items to satisfy these needs. (Figure 1) The test structure focused on criteria referenced learning objectives. The instrument item structure consisted of a short phrased question followed by 5 multiple choice responses; one correct response and three incorrect interspersed distractors followed by a 5th “I don’t know” response, also scored incorrect. The “I don’t know” option was chosen due to the criteria based design of the instrument and the importance of clinicians to clearly evaluate baseline and temporal improvements in knowledge by avoiding guessing and test-taking acumen26–29. Reading comprehension was kept at a basic 8th grade comprehension level via SMOG and Flesh readability analysis 30, 31. This reading level was well within our patient education demographic (mean 13.6 years, sd 2.69) and generally accepted in the adult health literacy literature 32, 33. Test developers avoided the use of jargon and obtuse medical terminology in item design. Test items were also screened for simplicity of sentence construct, redundancy and optimal clarity of interpretation. A panel of 7 expert judges was then recruited and using a table of specification format, these content experts evaluated the relevancy of the test item to the curriculum content and teaching objectives previously identified34 (Table 1). If expert mean agreement on an item was 80% or less, the item was examined for either rewording or deletion. Fourteen items met this criterion, 9 were deleted and 5 were reworded. Test items were selected for inclusion in the final instrument using a cut-off criterion of at least 85% inter-rater (six of the seven) agreement among the judges24 (Table 1). The 31 items chosen for inclusion were a result of this systematic process and compose the Cardiac Knowledge Assessment Tool (CKAT©) developed to evaluate achievement of the learning objectives contained within this core CR curriculum (Table 2.).
Figure 1. Cardiac Rehab Instructional Modules.
36 instructional modules developed according to guidelines established by the American Heart Association and American College of Cardiology for secondary prevention of heart disease and lifetime maintenance of heart healthy lifestyle practices16.
Figure 2. Learning Content Domains and Corresponding Number of Test Items.
Ten focused curriculum domains, developed by multidisciplinary staff, and specific to the desired learner based competencies and outcomes suggested by the American Heart Association and American College of Cardiology guidelines16.
Table 1.
Table of Specification
| Reviewer #1 | Reviewer #2 | Reviewer #3 | Reviewer #4 | Reviewer #5 | Reviewer #6 | Reviewer #7 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Discipline | BSN-EP/15yrs | MA-EP/15yrs | BSN/25yrs | MS-EP/10 yrs 10yrrs | BS-RD/16 yrs 16yrs | BSN/15yrs | MD/12yrs | ||||||||
| Q# | Status | Domain | Ob/Met | Domain | Ob/Met | Domain | Ob/Met | Domain | Ob/Met | Domain | Ob/Met | Domain | Ob/Met | Domain | Ob/Met |
| #1 | ✓ | BP | 80%√ | BP | 80% | BP | 90% | BP | 90% | BP | 100% | BP | 100% | BP | 50% |
| #2 | ✓ | Chol. | 95% | Chol. | 80% | Chol. | 90% | Chol. | 95% | Chol. | 85% | Chol. | 98% | Chol. | 100% |
| #3 | ✓ | Ex. | 95% | Ex. | 80% | Ex. | 100% | Ex. | 95% | Ex. | 100% | Ex. | 98% | Ex. | 100% |
| #4 | X | BP | 85% | BP | 50% | BP | 90% | BP | 50% | BP | 100% | BP | 30% | BP | 20% |
| #5 | ✓ | Chol. | 80% | CAD | 50% | Chol. | 100% | Chol. | 90% | Chol. | 80% | Chol. | 80% | Chol. | 100% |
| #6 | ✓ | Ex. | 95% | Ex. | 80% | Ex. | 100% | Ex. | 90% | Ex. | 60% | Ex. | 95% | Ex. | 100% |
| #7 | ✓ | Ex./Sfty | 80% | Ex./Sfty | 80% | Ex./Sfty | 95% | Ex./Sfty | 100% | Ex./Sfty | 100% | Ex./Sfty | 85% | Ex./Sfty | 100% |
| #8 | ✓ | BP/Diet | 90% | BP | 88% | BP | 90% | BP | 85% | BP | 80% | BP/Diet | 58% | BP | 80% |
| #9 | ✓ | Chol. | 90% | Chol. | 50% | Chol. | 100% | Chol. | 95% | Chol. | 80% | Chol. | 93% | Chol. | 100% |
| #10 | ✓* | Chol. | 90% | Chol. | 70% | Chol. | 90% | Chol. | 80% | Chol. | 90% | Chol. | 99% | Chol. | 90% |
| #11 | X | BP | 80% | BP | 80% | BP | 90% | BP | 70% | BP | 50% | BP | 69% | BP | 20% |
| #12 | ✓ | BP/Diet | 85% | BP/Diet | 80% | BP/Diet | 90% | BP/Diet | 90% | BP/Diet | 10% | BP/Diet | 93% | BP/Diet | 100% |
| #13 | ✓ | Ex. | 95% | Ex. | 80% | Ex. | 90% | Ex. | 90% | Ex. | 80% | Ex. | 99% | Ex. | 100% |
| #14 | ✓ | Chol. | 85% | Chol. | 80% | Chol. | 90% | Chol. | 90% | Chol. | 100% | Chol. | 89% | Chol. | 100% |
| #15 | X | Diet | 70% | Diet | 80% | Diet | 90% | Diet | 80% | Diet | 100% | Diet | 50% | Diet | 50% |
| #16 | ✓ | Ex. | 85% | Ex. | 80% | Ex. | 90% | Ex. | 85% | Ex. | 80% | Ex. | 85% | Ex. | 50% |
| #17 | ✓ | Chol. | 85% | Chol. | 80% | Chol. | 85% | Chol. | 80% | Chol. | 80% | Chol. | 62% | Chol. | 100% |
| #18 | ✓ | BP | 80% | BP | 70% | BP | 80% | BP | 85% | BP | 80% | BP | 90% | BP | 100% |
| #19 | ✓ | Chol. | 95% | Chol. | 80% | Chol. | 90% | Chol. | 100% | Chol. | 100% | Chol. | 100% | Chol. | 50% |
| #20 | X | Ex. | 60% | Ex. | 50% | Ex. | 80% | Ex. | 80% | Ex. | 100% | Ex. | 83% | Ex. | 100% |
| #21 | ✓ | BP | 80% | BP | 70% | BP | 90% | BP | 80% | BP | 100% | BP | 88% | BP | 100% |
| #22 | X | BP | 65% | BP | 70% | BP | 80% | BP | 90% | BP | 10% | BP | 63% | BP | 50% |
| #23 | ✓* | Chol. | 95% | Chol. | 80% | Chol. | 100% | Chol. | 85% | Chol. | 40% | Chol. | 90% | Chol. | 100% |
| #24 | ✓* | Meds | 85% | Meds | 80% | Meds | 100% | Meds | 100% | Meds | 100% | Meds | 99% | Meds | 50% |
| #25 | ✓* | Ex. | 85% | Ex. | 90% | Ex. | 90% | Ex. | 90% | Ex. | 40% | Ex. | 82% | Ex. | 100% |
| #26 | ✓ | Chol. | 80% | Chol. | 80% | Chol. | 100% | Chol. | 85% | Chol. | 80% | Chol. | 93% | Chol. | 100% |
| #27 | ✓ | Ex. | 90% | Ex. | 80% | Ex. | 100% | Ex. | 75% | Ex. | 100% | Ex. | 100% | Ex. | 100% |
| #28 | X | Ex. | 85% | Ex. | 50% | Ex. | 90% | Ex. | 70% | Ex. | 100% | Ex. | 67% | Ex. | 50% |
| #29 | ✓ | Stroke | 90% | Stroke | 80% | Stroke | 90% | Stroke | 75% | Stroke | 100% | Stroke | 100% | Stroke | 100% |
| #30 | X | Stress | 80% | Stress | 80% | Stress | 100% | Stress | 55% | Stress | 100% | Stress | 79% | Stress | 50% |
| #31 | ✓ | Rsk/Rec | 80% | Rsk/Rec | 80% | Rsk/Rec | 90% | Rsk/Rec | 85% | Rsk/Rec | 95% | Rsk/Rec | 75% | Rsk/Rec | 100% |
| #32 | ✓ | CHF | 80% | CHF | 70% | CHF | 80% | CHF | 80% | CHF | 100% | CHF | 97% | CHF | 100% |
| #33 | ✓ | Ex. | 90% | Ex. | 80% | Ex. | 100% | Ex. | 85% | Ex. | 100% | Ex. | 90% | Ex. | 100% |
| #34 | X | Ex/Risk | 60% | Ex/Risk | 50% | Ex/Risk | 90% | Ex/Risk | 85% | Ex/Risk | 100% | Ex/Risk | 85% | Ex/Risk | 20% |
| #35 | ✓* | Rsk/Rec | 90% | Rsk/Rec | 80% | Rsk/Rec | 80% | Rsk/Rec | 80% | Rsk/Rec | 100% | Rsk/Rec | 100% | Rsk/Rec | 100% |
| #36 | ✓ | A&P | 85% | A&P | 70% | A&P | 100% | A&P | 100% | A&P | 90% | A&P | 90% | A&P | 100% |
| #37 | ✓ | Diabetes | 95% | Diabetes | 90% | Diabetes | 90% | Diabetes | 80% | Diabetes | 100% | Diabetes | 85% | Diabetes | 20% |
| #38 | ✓ | CHF | 85% | CHF | 80% | CHF | 100% | CHF | 90% | CHF | 80% | CHF | 75% | CHF | 100% |
| #39 | ✓ | CHF | 80% | CHF | 80% | CHF | 100% | CHF | 90% | CHF | 100% | CHF | 100% | CHF | 100% |
| #40 | X | CHF | 65% | CHF | 40% | CHF | 100% | CHF | 100% | CHF | 50% | CHF | 50% | CHF | 90% |
= Item Revised & Accepted
= Item Accepted
= Item Rejected
Table 2.
| # | Test Item |
Expert Mean Agreement |
|---|---|---|
| 1 | A term that is used to describe blood pressure higher than normal is: | 84.3 |
| a. Hyperactive b. Hypertension c. Vasoconstriction d. Hypotension e. I don’t know | ||
| 2 | A bad form of cholesterol is: | 91.8 |
| a. HDL (High Density Lipoprotein) b. Hbg (Hemoglobin) c. LDL (Low Density Lipoprotein) d. CPK (Phosphokinase) e. I don’t know | ||
| 3 | The best way to measure if you are working hard enough during exercise is to: | 95.4 |
| a. Count the minutes of each exercise session b. Count your pulse rate during exercise c. Count the settings on the exercise equipment d. Count your breathing rate during exercise e. I don’t know | ||
| 4 | High amounts of Bad Cholesterol may lead to heart problems by blocking: | 82.9 |
| a. Heart valves b. Heart arteries c. Heart electricity d. Heart chambers e. I don’t know | ||
| 5 | Each heart healthy exercise conditioning session should be not less than | 88.6 |
| a. 15 minutes b. 30 minutes c. 60 minutes d. 90 minutes e. I don’t know | ||
| 6 | If you feel lightheaded during or after exercise, the best thing to do is: | 91.4 |
| a. Continue to exercise b. Monitor your pulse c. Breath rapidly & deeply d. Sit or lie down e. I don’t know | ||
| 7 | The food item we eat or drink that most directly effects blood pressure is: | 81.6 |
| a. Fat b. Salt c. Water d. Sweets e. I don’t know | ||
| 8 | The two best ways to decrease bad cholesterol is by: | 86.9 |
| a. Exercise & medication b. Cardiac cath & medication c. Diet & medication d. Chelation & angiograms e. I don’t know | ||
| 9 | People who have had heart problems due to blocked arteries should keep their triglyceride levels less than | 87.0 |
| a. 150 mg/dL b. 200 mg/dL c. 250 mg/dL d. 200 mg/dL e. I don’t know | ||
| 10 | The amount of sodium (salt) in the daily diet should be less than: | 91.1 |
| a. 3,400 mg. b. 1,500 mg. c. 400 mg d. 3,000 mg e. I don’t know | ||
| 11 | To gain the most benefit from a heart healthy exercise program you should exercise at least: | 90.6 |
| a. Once each week b. Twice per week c. Three times per week d. Seven times per week e. I don’t know | ||
| 12 | The type of cholesterol that is good and acts to remove harmful cholesterol from the body is: | 90.6 |
| a. HDL (High Density Lipoprotein) b. Hbg (Hemoglobin) c. LDL (Low Density Lipoprotien) d. VLDL e. I don’t know | ||
| 13 | The best exercise for loosing body fat around the waist is: | 82.1 |
| a. Leg lifts b. Sit-ups c. Crunches d. Walking e. I don’t know | ||
| 14 | Choose the food below this is most likely to increase triglyceride levels: | 81.7 |
| a. Fried Foods b. Sweets c. Red Meat d. Eggs e. I don’t know | ||
| 15 | All of the below may help reduce high blood pressure except | 83.6 |
| a. Weight lifting & resistance exercises b. Body weight reduction c. Aerobic “cardio” exercises d. Stop smoking e. I don’t know | ||
| 16 | The ideal goal for people who have had heart problems due to blocked arteries is to keep their LDL cholesterol less than: | 87.9 |
| a. 50 mg/dL b. 70 mg/dL c. 150 mg/dL d. 200mg/dL e. I don’t know | ||
| 17 | High resting blood pressure levels increase the risk of all the below except: | 86.9 |
| a. Stroke b. High cholesterol c. Heart attack d. Diseased arteries e. I don’t know | ||
| 18 | The type of food that is most likely to increase LDL cholesterol is: | 88.6 |
| a. Fried Foods b. Sweets c. Pasta d. Eggs e. I don’t know | ||
| 19 | If you feel you are having side effects from your blood pressure medication you should: | 87.7 |
| a. Decrease the dose b. Call your physician c. Ignore the symptoms d. Stop taking the medication e. I don’t know | ||
| 20 | All of the below choices are types of heart healthy exercises except | 83.9 |
| a. Walking b. Weight lifting c. Swimming d. Cycling e. I don’t know | ||
| 21 | The health practice that is most effective in increasing (HDL) cholesterol is: | 88.3 |
| a. Low fat diet b. Exercise c. Stress reduction d. Weight reduction diet e. I don’t know | ||
| 22 | When should you plan and begin a home or community based exercise program. | 92.1 |
| a. During the Cardiac Rehab program b. During the last session of Cardiac Rehab c. Immediately after the Cardiac Rehab program d. Two weeks after completing Cardiac Rehab e. I don’t know | ||
| 23 | People who have had heart problems due to blocked blood vessels in the heart also are at a higher risk for stroke because: | 90.7 |
| a. Most strokes are caused by weakened blood vessels b. Most strokes are caused by blood thinners c. Most strokes are caused by blocked vessels in the brain d. Most stroke are caused by heart attacks e. I don’t know | ||
| 24 | If you have chest pain that is caused by movement of or pressing on the painful area it is likely that the pain is: | 86.4 |
| a. Heart related b. Muscle or bone related c. Breathing related d. Stomach related e. I don’t know | ||
| 25 | If you become short of breath when lying down or during rest it is most likely due to fluid build-up in the lungs caused by: | 86.7 |
| a. Bronchial congestion b. Emphysema c. Exertion d. Heart failure e. I don’t know | ||
| 26 | The best drink to replace fluid lost when exercising in warm conditions is: | 92.1 |
| a. Water b. Sports drinks c. Fruit Juice d. Diet soda e. I don’t know | ||
| 27 | The following are all controllable (modifiable) risk factors for heart disease except | 90.0 |
| a. High cholesterol b. High blood pressure c. Family History d. Smoking e. I don’t know | ||
| 28 | The job of the coronary arteries is to: | 90.7 |
| a. Supply the lungs with blood b. Take blood away from the heart c. Supply the heart muscle with blood d. Deliver blood to the brain e. I don’t know | ||
| 29 | It is possible to prevent Type II (adult onset) diabetes. | 85.7 |
| a. True b. False c. I don’t know | ||
| 30 | The most effective method for you to evaluate heart failure is: | 87.1 |
| a. Periodic checks with your doctor b. Weighing yourself at the same time each day c. Measure the amount of salt you eat each week. D. Measure the amount of water you drink each day e. I don’t know | ||
| 31 | A person may be having the signs and symptoms of heart failure if: | 92.9 |
| a. They wake up from sleep with sever air hunger b. They notice that they become short of breath when doing their normal daily activities c. They notice, the first thing in the morning, that they have ½ inch pitted swelling around both ankles d. All of the above may be signs of heart failure. e. I don’t know |
During the time period 2002–2011, two alterations have occurred to reflect changes in national guidelines. Item #10, correct response: Sodium 2400mg –changed to- 1500mg/day; and item #16, correct response: LDL cholesterol <100mg/dL- changed to- <70mg/dL. These changes did not affect response sequence or alter the substantive context of the correct answer or item distracters.]
Sample Characteristics
A convenience sample of 3,638 adults tested from 2002–2011 in our urban Midwestern phase II CR program was chosen for the study (Table 3).
Table 3.
Demographic Characteristics for Patients n = 3638
| Entry Age M/(SD) |
Yrs Educ. M/(SD) |
Race | ||||
|---|---|---|---|---|---|---|
| Caucasian | AA | Asian | Other | |||
| Male | 64.58 (11.28) n=2416 |
13.81 (2.9) n = 2268 |
n = 2220 % = 94.9 |
n = 99 % = 4.2 |
n = 2 % = .1 |
n = 1 % = 0 |
| Female | 65.99 (11.28) n=1222 |
12.94 (2.27) n = 1149 |
n = 1060 % = 89.5 |
n = 109 % = 9.2 |
n = 2 % = .2 |
n = 2 % =.2 |
| Total | 65.05 (11.53) n=3638 |
13.52 (2.72) n =3417 334171928 |
% = 93.1 n = 3280 |
% = 5.9 n = 208 |
% = .1 n = 4 |
% = .1 n = 3 |
Abbreviations: AA, African American; M, mean; SD, standard deviation.
n size variability in sub-groups due to missing data.
Test Administration
Subject testing was conducted in a controlled environment during intake and discharge sessions at our facility. Each subject was instructed regarding the importance of candid responses and use of the “I don’t know” answer option to provide an accurate assessment of their knowledge levels. Test design allowed subjects to self-select either paper-and-pencil or computer mouse-click application. Visual test instructions were the same for both formats. IRB approval was obtained for the pilot project in 2001. The test was piloted then in a group of 50 consecutive CR patients who, through the use of a formatted questionnaire, rated the test to be understandable, ‘quick and easy to take’ (mean administration time 13.5 minutes) and unambiguous in reading interpretation.
Data Collection
Data was prospectively collected in our CR clinical database then retrospectively deidentified and entered in a separate database created in SPSS version 16 which was used to perform descriptive, validity and reliability analyses35.
Measures
Validity
While there are several types of validity the three most important in the educational literature are, content, construct and criteria-related36, 37. There is agreement in the methodologic literature that content validity is largely a matter of judgment, involving two distinct phases; First, a-priori efforts by the test developer to enhance content validity through careful conceptualization and domain analysis prior to item generation, and Second a-posteriori efforts to evaluate the relevance of the test’s content through expert assessment24, 25, 38. CKAT content validity was established by SCR developmental staff and clinical content experts, using this approach by use of a ‘table of specification’ described by Anastasi as ‘the systematic examination of test items to insure coverage of a representative sample of the content to be measured’39. Construct validity was evaluated through the use of factor analysis, a statistical methodology employed to identify underlying constructs of the test. Predictive validation was analyzed using a hierarchical linear regression holding baseline knowledge scores and functional work capacity constant while predicting post CR program values40. Also, correlation analysis was performed to evaluate concurrent performance with other recognized health care evaluative outcome measures, including the Medical Outcomes Study Short Form-36 (SF-36), Duke Activity Status Index (DASI),Mini-Mental State Exam (MMSE) and Beck Depression Inventory (BDI)41–45.
Reliability
Cronbach’s Alpha is a widely used estimate to support internal consistency of items in a scale. It is a measure of the level of mean intercorrelation of items. Alpha increases as the inter-correlation among test items increase and is considered to be a robust internal consistency estimate of reliability of test scores. An Alpha of .70 is generally recognized in the literature as acceptable46. We further measured internal consistency through use of the Spearman-Brown split half reliability coefficient, a method in which the items comprising a test are systematically split into two groups and scored independently the results of which are compared to compute a correlation coefficient37.
Item Analyses
A point biserial correlation (rpb) was used to measure the relationship between performance on an item (dichotomous variable) and the total score (continuous variable) and was calculated to determine the relative importance of test items47. Individual items were further analyzed using an Item Difficulty Index which ranges from 0 to 1 and is the proportion of subjects who answered the test item accurately. The greater the difficulty of an item, the lower its index will be. If the item difficulty is more than .75 it is considered an easy item and if the difficulty is below .25, it is a difficult item. The Discrimination Index which ranges from +1 to −1 and is a comparison of how subjects obtaining high total scores on an instrument performed on individual items as compared to those with low total scores further analyzed individual items (Table 4)48.
Table 4.
Item Analysis
| Item # | Point Biserial | Item Difficulty Index | Discrimination Index | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | |
| 1 | .446** | .357** | .83 | .93 | .32 | .15 |
| 2 | .590** | .534** | .49 | .90 | .75 | .25 |
| 3 | .505** | .298** | .81 | .97 | .38 | .07 |
| 4 | .439** | .305** | .92 | .98 | .18 | .05 |
| 5 | .411** | .451** | .45 | .84 | .46 | .33 |
| 6 | .350** | .243** | .80 | .94 | .24 | .11 |
| 7 | .384** | .315** | .81 | .90 | .27 | .22 |
| 8 | .229** | .386** | .54 | .63 | .19 | .51 |
| 9 | .469** | .477** | .39 | .83 | .54 | .35 |
| 10 | .434** | .501** | .32 | .86 | .48 | .32 |
| 11 | .414** | .183 | .85 | .95 | .24 | .07 |
| 12 | .604** | .530** | .50 | .91 | .76 | .23 |
| 13 | .323** | .450** | .37 | .83 | .35 | .35 |
| 14 | .311** | .603** | .13 | .53 | .22 | .77 |
| 15 | .508** | .555** | .52 | .85 | .60 | .37 |
| 16 | .436** | .523** | .27 | .76 | .46 | .48 |
| 17 | .559** | .616** | .54 | .81 | .67 | .46 |
| 18 | .417** | .318** | .61 | .87 | .43 | .18 |
| 19 | .424** | .282** | .93 | .98 | .14 | .04 |
| 20 | .475** | .415** | .83 | .96 | .32 | .11 |
| 21 | .420** | .597** | .24 | .68 | .42 | .66 |
| 22 | .300** | .505** | .32 | .76 | .30 | .48 |
| 23 | .491** | .446** | .58 | .85 | .56 | .30 |
| 24 | .479** | .592** | .46 | .75 | .56 | .57 |
| 25 | .447** | .542** | .49 | .79 | .50 | .47 |
| 26 | .320** | .237** | .87 | .97 | .16 | .07 |
| 27 | .526** | .499** | .76 | .91 | .47 | .22 |
| 28 | .477** | .450** | .58 | .78 | .54 | .41 |
| 29 | .428** | .430** | .54 | .81 | .49 | .38 |
| 30 | .319** | .593** | .13 | .53 | .23 | .77 |
| 31 | .417** | .372** | .66 | .86 | .39 | .26 |
p <.01
Results
As previously described, content validity was systematically established by SCR developers through use of item CVI relevance analysis, domain assignment and strict adherence to a ‘table of specification’ by a seven member multidisciplinary team of content experts. Construct validity was determined via a principle component factor analysis with varimax rotation performed on 3,638 pre test scores49. Simple structure was approached but not obtained. Seven underlying factors explaining 42% of the total variance were identified. Rotated factor loadings, were interpreted as the Pearson correlation between the test item and the factor (Only coefficients of .40 and above were retained for interpretation). Using these criteria, six items did not load significantly on any factor but were retained due to the underlying curriculum based content defining their inclusion in the instrument (Table 5). Test reliability was further supported via ‘Cronbach’s Alpha’ analysis, an estimate of internal consistency. Cronbach’s Alpha of .852 and .865 was obtained on the pilot and total test data set respectively (An Alpha of .70 is generally recognized in the literature as acceptable). Internal consistency was evaluated by use of the Spearman-Brown split half reliability coefficient. The results .817 pilot data, and .840 total data further confirmed the internal consistency of the instrument. Pre and post test, point biserial correlations measuring performance between each item (dichotomous variable) and the total score (continuous variable), determine the relative importance of test items. Values >.25, required for a “good” item, were significantly correlated with the total score at p<.01 for both the pre and post test with the exception of post test item #11. The Item Difficulty Index, which ranges from 0 to 1, reports the proportion of people answering a test item accurately (Table 4). The greater the difficulty of an item, the lower its index will be. If the item difficulty is more than .75 it is considered an easy item and if the difficulty is below .25, it is a difficult item. By this criteria 3 items would be considered difficult and 10 easy on the pretest. The remaining 18 items made up 58% of the test with an average difficulty score of 47.9 (50 being optimal). Post test difficulty scores ranged from .53 to .98, a trend that illustrates an overall expected decrease in item difficulty as a product of learning effect, described in educational psychology as the expected result of affective educational intervention50–52. The Discrimination Index which ranges from +1 to −1 is a comparison of how subjects obtaining high total scores on an instrument performed on individual items as compared to those with low total scores (Table 4). All values pre and post were positive, which indicates good validity since the formula for this calculation is such that the value will be positive if more subjects in the high scoring group chose the correct answer than did subjects in the low scoring group. Analyses between paper and pencil, and computer modes of administration in 1,999 subjects completing both pre and post tests were not significantly different (pre-test, p<.064: post-test, p<.774), confirming uniform interpretation of results across application modes. Also this group of completer’s test scores positively correlated with attendance at group education sessions p<.035, further validating the curriculum based design of the instrument. CKAT pre testing correlates with the (SF-36) Physical and Mental Composite Scales (n =3298), MMSE (n=1164), BDI (n =1654), and the DASI (n =1875) of p≤ .01 demonstrated CKAT’s strong levels of concurrent validity with established health outcomes instruments. Concurrent validity was further demonstrated in a convenience sample of subjects completing two established adult health literacy tests; The Test of Functional Health Literacy in Adults (TOFHLA) and the Medical Term Recognition Test (METER), which were found to correlate significantly with CKAT; r = .299, p <.01 (n = 152) and r = .330, p<.01 (n = 152) respectively 53, 54. Using hierarchical linear regression in a sample of 1,783 subjects completing both pre and post-testing, CKAT post-test scores were significant p<.001 in predicting CR program estimated mean FWC at program completion while controlling for pre-program CKAT scores and FWC results. The positive direction of this relationship strongly indicates higher scores on the CKAT predictive of FWC gain.
Table 5.
| Factor Analysis | Factor Description | Baseline % Correct |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Question# | Component | ||||||||
| #1 | #2 | #3 | #4 | #5 | #6 | #7 | |||
| 5 | .614 |
Factor #1 Self-Management Principles |
51.8 | ||||||
| 24 | .604 | 46.0 | |||||||
| 27 | .563 | 75.6 | |||||||
| 17 | .554 | 53.5 | |||||||
| 20 | .525 | 83.1 | |||||||
| 23 | .494 | 57.9 | |||||||
| 28* | |||||||||
| 12 | .814 |
Factor #2 Risk Identification |
49.4 | ||||||
| 2 | .808 | 48.6 | |||||||
| 16 | .519 | 26.8 | |||||||
| 18 | .487 | 60.7 | |||||||
| 9 | .486 | 39.7 | |||||||
| 4 | .649 |
Factor #3 Health Improvement Issues |
91.8 | ||||||
| 1 | .599 | 82.5 | |||||||
| 3 | .578 | 81.0 | |||||||
| 5* | |||||||||
| 11* | |||||||||
| 25 | .686 |
Factor #4 Symptom Recognition |
39.4 | ||||||
| 30 | .685 | 12.6 | |||||||
| 31 | .421 | 66.1 | |||||||
| 29* | |||||||||
| 10* | |||||||||
| 13 | .580 |
Factor #5 Reasoning Ability |
37.1 | ||||||
| 14 | .452 | 13.0 | |||||||
| 21 | .450 | 87.1 | |||||||
| 22* | |||||||||
| 26 | .637 |
Factor #6 Self-Care Strategies |
86.5 | ||||||
| 19 | .617 | 92.7 | |||||||
| 8 | .739 |
Factor #7 Intervention Identification |
54.3 | ||||||
| 6 | .457 | 80.2 | |||||||
| 7 | .407 | 80.9 | |||||||
Table metric shows Pearson correlation between each test item and the corresponding factor.
Indicates items that did not load significantly (.4 or greater) on any factor
Discussion
Cardiac disease-knowledge assessment instruments that have been developed in a variety of inpatient and outpatient settings, lack population specificity, systematic construct and rigorous reliability/validity analysis8, 9, 15. We have described a comprehensive and systematic test development approach targeted for adults with cardiac disease learning needs which adheres to nationally recognized patient centered outcomes5. The design purposefully avoided parochial and non-evidenced based content, prevalent in previous instrument design10. The test development focused on fundamental adult cognitive learning objectives of knowledge, understanding, and application enumerated in Bloom’s and Anderson’s seminal work22. Test item development reflected systematic identification of CR specific learning content domains of blood pressure control, lipid management, exercise, heart failure, cardiovascular disease risk, medications, anatomy & physiology, diet, diabetes, and stroke14(Figure 1). Self-Management Principles, Risk Identification, Health Improvement Issues, Symptom Recognition, Reasoning Ability, Self-Care Strategies and Personal Intervention, a subset of highly desirable underlying personal care constructs immerged via factor analysis (Table 5). Validity and reliability analyses were robust. The test itself is unique in its use of a “don’t know” response set in multiple-choice format. Previous formats employed dichotomous (true/false) responses which increase the error effect of random guessing and test-taking acumen28. The “don’t know” feature further adds to the instrument’s utility as a clinical barometer of baseline learning needs pretreatment and remediation post treatment, by reducing error of interpretation. Attention was specifically directed at readability and ease and speed of administration. Administration and scoring uniformity in either paper & pencil or computer formats add to its utility as a clinical tool in diverse settings. The instrument has been used as an effective clinical tool by staff during initial and pre-discharge administrations coupled with follow-up one-on-one goal setting and outcome assessment reviews. As a result clinicians are better prepared to analyze the learning specific content needs and focus individual educational remediation.
Limitations
The current findings were limited in several ways. First, our findings are based on a study population representative of a large Midwestern, hospital based CR program. Second, we included six items that did not significantly load on one of the underlying seven psychometric factors identified in factor analysis. The choice to include these six items was based on their strong content relevancy based on program learning objectives. Third, a memorization effect may have occurred although mitigated by a mean time of 90.4 days between pre and post-testing applications. Also, subgroup analysis and, application and validity analysis in educational settings devoted to effective management of heart disease risk in populations other than CR needs to be explored.
Implications
Accurate assessment and interpretation of clinically relevant data enhances intervention at every level. It is particularly important for clinicians to accurately assess knowledge in their adult cliental who are often facing the need to understand a myriad of baffling terms and concepts then make significant adjustments to personal behavior, all during times of high psychological stress. We have described development and testing of such an instrument specifically focused at the cardiovascular disease management needs of this older-adult population. Although designed and validated in this large CR cohort, the utility of this instrument in other settings directed at integrated management of cardiovascular disease risk is reasonable. However, further research confirming test validity is needed in these and CR settings representing a broader range of demographic diversity.
Conclusions
Instruments, designed to measure achievement of cardiovascular disease management knowledge and behavioral change concepts in patients post cardiac event, indicate a variety of psychometric design flaws7–10, 15. Realizing this need we have systematically developed and tested an instrument specifically designed for this adult population that satisfies psychometric parameters and reliability/validity analysis in a large representative cardiac disease patient population.
What’s New and Important.
Comprehensive and systematic development of an adult outpatient heart disease knowledge and health management assessment tool.
Unique multiple choice format including correct response, three distracters and “Don’t Know” responses enhancing accuracy of measurement and clinical utility.
Rapid test administration.
Valid paper-and-pencil or computer application and scoring.
Rigorous validity and reliability analyses in over 3500 patient applications.
Acknowledgements
Project was supported by Nursing Research / Nursing Clinical Ladder programs and The Center for Cardiovascular Research, Summa Health System, Akron, OH
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
James S Rosneck, Manager: Cardiovascular & Pulmonary Rehabilitation, Administrative Director: Center for Cardiovascular Research, Summa Health System, Akron, OH, Associate Professor: Department of Sports Science & Wellness Education, The, University of Akron, Akron OH.
Joel Hughes, Director: Applied Psychology Center, Associate Professor Psychology Department, Kent State University, Kent, OH, Scientific Director: Center for Cardiovascular Research Summa Health System, Akron, OH Adjunct Assistant Professor: Francis Payne Bolton School of Nursing Case Western Reserve University, Cleveland, OH, Adjunct Assistant Professor: Department of Medicine Case Western Reserve University, Cleveland, OH.
John Gunstad, Associate Professor: Psychology Department, Kent State University, Kent, OH, Research Associate: Center for Cardiovascular Research, Summa Health System, Adjunct Assistant Professor: Department of Medicine, Case Western Reserve University Cleveland, OH.
Richard Josephson, Professor of Medicine: Case Western Reserve University School of Medicine, Cleveland, OH, Director Cardiac Intensive Care Unit / Director Cardiovascular & Pulmonary, Rehabilitation: Harrington Heart & Vascular Institute, University Hospitals Health System, Cleveland, OH.
Donald A Noe, Research Associate: Department of Research Administration, Summa Health System, Akron, OH.
Donna Waechter, Coordinator: Center for Cardiovascular Research, Summa Health System, Akron, OH Adjunct Professor: Psychology Department, Kent State University, Kent, OH.
REFERENCES
- 1.National Institutes of Health, editor. Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases. 2009th ed. Washington, DC: U S Department of Health and Human Services; National Institutes of Health: National Heart Lung and Blood Institute; 2009. [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The american heart association's strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Scott JT, Thompson DR. Assessing the information needs of post-myocardial infarction patients: A systematic review. Patient Educ Couns. 2003;50(2):167–177. doi: 10.1016/s0738-3991(02)00126-x. [DOI] [PubMed] [Google Scholar]
- 4.Czar ML, Engler MM. Perceived learning needs of patients with coronary artery disease using a questionnaire assessment tool. Heart Lung. 1997;26(2):109–117. doi: 10.1016/s0147-9563(97)90070-4. [DOI] [PubMed] [Google Scholar]
- 5.Williams MA. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 4th ed. Champaign, IL: American Association of Cardiovascular and Pulmonary Rehabilitation; 2003. [Google Scholar]
- 6.Dusseldorp E, van Elderen T, Maes S, Meulman J, Kraaij V. A meta-analysis of psychoeduational programs for coronary heart disease patients. Health Psychol. 1999;18(5):506–519. doi: 10.1037//0278-6133.18.5.506. [DOI] [PubMed] [Google Scholar]
- 7.Gwadry-Sridhar F, Guyatt GH, Arnold JM, et al. Instruments to measure acceptability of information and acquisition of knowledge in patients with heart failure. Eur J Heart Fail. 2003;5(6):783–791. doi: 10.1016/s1388-9842(03)00158-2. [DOI] [PubMed] [Google Scholar]
- 8.Thanavaro JL, Thanavaro S, Delicath T. Coronary heart disease knowledge tool for women. J Am Acad Nurse Pract. 2010;22(2):62–69. doi: 10.1111/j.1745-7599.2009.00476.x. [DOI] [PubMed] [Google Scholar]
- 9.Wagner J, Lacey K, Chyun D, Abbott G. Development of a questionnaire to measure heart disease risk knowledge in people with diabetes: The heart disease fact questionnaire. Patient Educ Couns. 2005;58(1):82–87. doi: 10.1016/j.pec.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Smith MM, Hicks VL, Heyward VH. Coronary heart disease knowledge test: Developing a valid and reliable tool. Nurse Pract. 1991;16(4):28, 31, 35–38. [PubMed] [Google Scholar]
- 11.Dollahite J, Thompson C, McNew R. Readability of printed sources of diet and health information. Patient Educ Couns. 1996;27(2):123–134. doi: 10.1016/0738-3991(95)00829-2. [DOI] [PubMed] [Google Scholar]
- 12.Aldridge MD. Writing and designing readable patient education materials. Nephrol Nurs J. 2004;31(4):373–377. [PubMed] [Google Scholar]
- 13.Friedman DB, Hoffman-Goetz l. A systematic review of readability and comprehension instruments used for print and web based cancer information. Health Educ Behav. 2006;33:352–373. doi: 10.1177/1090198105277329. [DOI] [PubMed] [Google Scholar]
- 14.Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services endorsed by the american college of chest physicians, american college of sports medicine, american physical therapy association, canadian association of cardiac rehabilitation, european association for cardiovascular prevention and rehabilitation, inter-american heart foundation, national association of clinical nurse specialists, preventive cardiovascular nurses association, and the society of thoracic surgeons. J Am Coll Cardiol. 2007;50(14):1400–1433. doi: 10.1016/j.jacc.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 15.Bergman HE, Reeve BB, Moser RP, Scholl S, Klein WM. Development of a comprehensive heart disease knowledge questionnaire. Am J Health Educ. 2011;42(2):74–87. doi: 10.1080/19325037.2011.10599175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gustafson KL, Branch RM. Survey of Instructional Models. 3rd ed. Syracuse, New York: ERIC Clearinghouse on Information & Technology; 1997. [Google Scholar]
- 17.Richey RC. The Theoretical and Conceptual Bases of Instructional Design. 120 Pentonville Road, London, UK: Kogan Page Ltd; 1986. [Google Scholar]
- 18.Nickel R, Osborn L. WIDS and performance based learning. 2009;1:1–12. [Google Scholar]
- 19.Grant JS, Davis LL. Selection and use of content experts for instrument development. Research in Nursing & Health. 1997;20(3):269–274. doi: 10.1002/(sici)1098-240x(199706)20:3<269::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 20.Bloom BS. Taxonomy of Educational Objectives: Book1 Cognitive Domain. London: Longman Group Limited; 1979. [Google Scholar]
- 21.Bloom BS. Human Characteristics and School Learning. New York: McGraw-Hill; 1976. [Google Scholar]
- 22.Anderson LW, Krathwohl DR, Bloom BS. A Taxonomy for Learning, Teaching, and Assessing : A Revision of Bloom's Taxonomy of Educational Objectives. New York: Longman; 2001. [Google Scholar]
- 23.Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: Endorsed by the national heart, lung, and blood institute. Circulation. 2006;113(19):2363–2372. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 24.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–385. [PubMed] [Google Scholar]
- 25.Beck CT, Gable RK. Ensuring content validity: An illustration of the process. J Nurs Meas. 2001;9(2):201–215. [PubMed] [Google Scholar]
- 26.Muijtjens AM, Mameren HV, Hoogenboom RJ, Evers JL, van der Vleuten CP. The effect of a 'don't know' option on test scores: Number-right and formula scoring compared. Med Educ. 1999;33(4):267–275. doi: 10.1046/j.1365-2923.1999.00292.x. [DOI] [PubMed] [Google Scholar]
- 27.SANDERSON PH. The ?don't know? option in MCQ examinations. Med Educ. 1973;7(1):25–29. [PubMed] [Google Scholar]
- 28.Burton RF. Misinformation, partial knowledge and guessing in true/false tests. Med Educ. 2002;36(9):805–811. doi: 10.1046/j.1365-2923.2002.01299.x. [DOI] [PubMed] [Google Scholar]
- 29.White R, Walker P, Roberts S, Kalisky S, White P. Bristol COPD knowledge questionnaire (BCKQ): Testing what we teach patients about COPD. Chron Respir Dis. 2006;3(3):123–131. doi: 10.1191/1479972306cd117oa. [DOI] [PubMed] [Google Scholar]
- 30.Contreras A, Garcia-Alonso R, Echenique M, Daye-Contreras F. The SOL formulas for converting SMOG readability scores between health education materials written in spanish, english, and french. J Health Commun. 1999;4(1):21–29. doi: 10.1080/108107399127066. [DOI] [PubMed] [Google Scholar]
- 31.Gillen B, Kendall PC, Finch AJ., Jr Reading ease and human interest scores: A comparison of flesch scores with subjective ratings. Teaching of Psychology. 1977;4(1):39. [Google Scholar]
- 32.Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy. 2006 NCES 2006483. [Google Scholar]
- 33.Miller B, McCardle P, Hernandez R. Advances and remaining challenges in adult literacy research. J Learn Disabil. 2010;43(2):101–107. doi: 10.1177/0022219409359341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Notar CE, Zuelke DC, Wilson JD, Yunker BD. The table of specifications: Insuring accountability in teacher made tests. Journal of Instructional Psychology. 2004;31(2):115–129. [Google Scholar]
- 35.SPSS I. SPSS 16.0 for windows. 2008. [Google Scholar]
- 36.Kerlinger FN. Foundations of Behavioral Research. 3rd ed. New York: CBS Publishing; 1986. [Google Scholar]
- 37.Polit D, Hungler B. Nursing Research Principles and Methods. 4th ed. Philadelphia: Lippincott Company; 1991. [Google Scholar]
- 38.Mastaglia B, Toye C, Kristjanson LJ. Ensuring content validity in instrument development: Challenges and innovative approaches. Contemp Nurse. 2003;14(3):281–291. doi: 10.5172/conu.14.3.281. [DOI] [PubMed] [Google Scholar]
- 39.Anastasi A. Psychological Testing. 6th ed. New York: Macmillan; 1988. [Google Scholar]
- 40.Mertler CA, Vannatta RA. Advanced and Multivariate Statistical Methods : Practical Application and Interpretation. 3rd ed. Glendale, CA: Pyrczak; 2005. [Google Scholar]
- 41.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. vol 30(6)1992 p.473-483. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 42.Brown K. A review to examine the use of SF-36 in cardiac rehabilitation. British Journal of Nursing. 2003;12(15):904–910. doi: 10.12968/bjon.2003.12.15.11422. [DOI] [PubMed] [Google Scholar]
- 43.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the duke activity status index) Am J Cardiol. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 44.Folstein M, Folstien S, McHugh P. "MINI-MENTAL STATE" A practicle method for grading the cognitive state of patients for the clinician. J psychiat Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 45.Beck AT, Steer RA, Brown GK. Beck Depression Inventory. 2nd ed. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 46.Cronbach LJ. Essentials of Psychological Testing. 4th ed. New York NY: Harper & Row; 1984. [Google Scholar]
- 47.Raudenbush SW, Byrk AS. Hierarchial Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- 48.Hopkins KD. Educational and Psychological Measurement and Evaluation. 8Th Ed. Needham Heights, MA: Allyn & Bacon; 1998. [Google Scholar]
- 49.Rummel RJ. Applied Factor Analysis. Evanston: Northwestern University Press; 1970. [Google Scholar]
- 50.Merriam SB, Caffarella RS, Baumgartner L. Learning in Adulthood : A Comprehensive Guide. 3rd ed. San Francisco: Jossey-Bass; 2007. [Google Scholar]
- 51.Ormrod J. Human Learning. 6th ed. Boston: Pearson; 2012. [Google Scholar]
- 52.Truluck JE, Courtenay BC. Learning style preferences among older adults. Educational Gerontology. 1999;25:221–236. 25, 221-236. [Google Scholar]
- 53.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 54.Rawson KA, Gunstad J, Hughes J, et al. The METER: A brief, self-administered measure of health literacy. J Gen Intern Med. 2010;25(1):67–71. doi: 10.1007/s11606-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]