Abstract
Purpose
To present nationally representative estimates of the impact of cancer survivorship on medical expenditures and lost productivity among adults in the United States.
Methods
Using the 2008 to 2010 Medical Expenditure Panel Survey, we identified 4,960 cancer survivors and 64,431 individuals without a history of cancer age ≥ 18 years. Direct medical costs were measured using annual health care expenditures and examined by source of payment and service type. Indirect morbidity costs were estimated from lost productivity as a result of employment disability, missed work days, and lost household productivity. We evaluated the economic burden of cancer survivorship by estimating excess costs among cancer survivors, stratified by time since diagnosis (recently diagnosed [≤ 1 year] and previously diagnosed [> 1 year]), compared with individuals without a history of cancer using multivariable regression models stratified by age (18 to 64 and ≥ 65 years), controlling for age, sex, race/ethnicity, education, and comorbidities.
Results
In 2008 to 2010, the annual excess economic burden of cancer survivorship among recently diagnosed cancer survivors was $16,213 per survivor age 18 to 64 years and $16,441 per survivor age ≥ 65 years. Among previously diagnosed cancer survivors, the annual excess burden was $4,427 per survivor age 18 to 64 years and $4,519 per survivor age ≥ 65 years. Excess medical expenditures composed the largest share of the economic burden among cancer survivors, particularly among those recently diagnosed.
Conclusion
The economic impact of cancer survivorship is considerable and is also high years after a cancer diagnosis. Efforts to reduce the economic burden caused by cancer will be increasingly important given the growing population of cancer survivors.
INTRODUCTION
An estimated 13.7 million Americans with a history of cancer were alive in 2012.1 Cancer survivorship prevalence has increased substantially over time and is anticipated to increase further given advances in treatment, early detection, increased life expectancy, and an aging population.2 As the number of cancer survivors increases, the importance of understanding the unique needs of this population also grows. Cancer treatment is associated with such long-term health effects as cardiotoxicity, lymphedema, sexual dysfunction, incontinence, pain and fatigue, cognitive dysfunction, and psychological distress.3 Cancer survivors also have an increased risk of secondary cancers.4,5
Cancer survivorship is associated with substantial medical expenditures and lost productivity, including employment disability, fewer hours worked, and more missed work days.6–11 Previous studies of medical expenditures have used cancer registry data linked to administrative claims or encounter data in the Medicare population12 or among individuals with managed care coverage in specific geographic regions.13,14 Studies assessing expenditures nationally have only included cancer survivors receiving cancer-related health care.15 The few studies that have assessed multiple components of the economic burden of survivorship were conducted in a single state.16–18 To our knowledge, no study quantifies both medical expenditures and indirect morbidity cost of lost productivity among adult cancer survivors of all ages at the national level.
In this study, we used nationally representative data to estimate direct medical costs and indirect morbidity costs among adult cancer survivors compared with individuals without a history of cancer. We examine direct medical costs by examining annual health care expenditures and indirect morbidity costs by examining lost productivity associated with employment disability, missed work days, and lost household productivity.
METHODS
Data
We used data from the 2008 to 2010 Medical Expenditure Panel Survey (MEPS) Household Component, a nationally representative sample of the US civilian noninstitutionalized population. Each year, a MEPS panel is selected from a sample of households that participated in the National Health Interview Survey the previous year. The panel is followed for 2 years through five rounds of in-person interviews, in which an individual typically responds for all family members in the household. Overlapping panels were combined from the 2008 to 2010 MEPS, with the final response rate ranging from 53.5% to 59.3%. MEPS collects detailed information on sociodemographic characteristics, health care expenditures, and employment characteristics. More detailed information on the MEPS survey design and content is available elsewhere.19,20
Analytic Sample
We defined a cancer survivor as any person who has ever been diagnosed with cancer. We identified 4,960 adult cancer survivors from a question asking whether a doctor or other health professional had ever told them they had cancer or a malignancy of any kind. The remaining 64,431 adults with no reported history of cancer were used as the comparison group. Individuals with missing data on cancer history were excluded (n = 121). Individuals diagnosed solely with nonmelanoma skin cancer were not classified as cancer survivors and were included in the comparison group.10
Sample characteristics of cancer survivors at the time of the survey included age, sex, race/ethnicity, educational attainment, marital status, number of MEPS priority conditions, health status, body mass index, and health insurance status. All analyses were stratified by age (18 to 64 and ≥ 65 years). Cancer survivors were stratified by time since diagnosis, which was calculated by subtracting age at diagnosis from age at the time of the survey. Because previous studies of medical expenditures have reported different treatment patterns in the first 6 to 12 months after diagnosis and later periods,6,21 we stratified cancer survivors as either recently diagnosed (≤ 1 year) or previously diagnosed (> 1 year).8,10 Cancer survivors reporting an implausible age of diagnosis were assumed to have misinterpreted the question and were excluded.10 The economic burden of cancer survivorship was measured by comparing direct medical costs and indirect morbidity costs between cancer survivors and individuals without a history of cancer. Data were analyzed using Stata version 12.0 (Stata, College Station, TX) to account for the complex survey design.
Annual Direct Medical Costs
Direct medical costs were estimated using total annual medical expenditures, by source of payment (out-of-pocket, private insurance, Medicare, Medicaid, and other sources) and service type (ambulatory care, inpatient care, prescription medications, and other services). Medical expenditures were adjusted to 2010 dollars using the Personal Health Care Expenditure Price Index.22 The overall price index was applied to total expenditures while individual components were applied to each service type.
We controlled for age, sex, race/ethnicity, and number of comorbid conditions in adjusted analyses of medical expenditures. To account for skewness in the distribution of medical expenditures, we used generalized linear models with a gamma distribution and a log link. Adjusted mean expenditures are presented as predictive margins, which standardize expenditures to the covariate distribution of the overall population.23
Annual Indirect Morbidity Costs
We measured indirect morbidity costs by assessing the lost productivity associated with individuals who are unable to work because of their health, days of work missed by workers because of their health, and days spent in bed by all individuals because of their health (in addition to days off work). Predictive margins from logistic regression modeling were used to estimate the percentage of individuals reporting employment disability controlling for age, sex, race/ethnicity, number of comorbid conditions, and education. Productivity loss from employment disability was calculated by multiplying the adjusted percentage unable to work as a result of illness or injury by the median annual wage ($33,721) from the Bureau of Labor Statistics.24 We used median wage instead of actual wages because actual wages would result in a lower value for vulnerable subpopulations, raising equity concerns.25
Employed individuals were asked how many days (half-day or more) of work they missed as a result of illness, injury, or mental or emotional problems. All individuals, regardless of work status, were also asked about additional missed days, other than work or school, in which they spent at least a half-day in bed as a result of illness or injury. Negative binomial regression models were used to estimate the impact of cancer survivorship on the number of missed work days and additional bed days controlling for age, sex, race/ethnicity, number of comorbid conditions, and education. Because the MEPS does not differentiate between missed full and partial days, we assumed each missed work day to be 6 hours.25,26 Lost productivity from missed work days was calculated as the product of the adjusted average number of missed days and cost per day using the median hourly wage ($16.21) from the Bureau of Labor Statistics.24 Lost household productivity was calculated by multiplying the average number of additional bed days by the value of daily household productivity ($40.61).27 All productivity costs were adjusted to 2010 dollars using the Consumer Price Index.28
National-Level Aggregate Economic Burden Estimates
Cancer prevalence estimates derived from national surveys differ from those derived from cancer registries.29–31 To address this variation, we created a plausible range of national-level aggregate net medical expenditures and indirect costs, using prevalence estimates from the MEPS sample weights and age-specific estimates from cancer registries.1 Per capita excess expenditures and indirect costs were multiplied by the number of cancer survivors per age group.
Sensitivity Analysis
We conducted sensitivity analyses to examine the uncertainty of our estimates. All medical expenditure estimates included 95% CIs to demonstrate the lower and upper bounds of our estimates. Additionally, 95% CIs of the three indirect cost components were carried through to calculate lower and upper bounds of the indirect morbidity cost estimates. We also examined the sensitivity of our indirect morbidity cost estimates to the choice of wage and household productivity values by constructing lower and upper bounds using the 25th and 75th percentiles of national wage values and 50% and 150% of daily household productivity values.
RESULTS
Characteristics of Cancer Survivors and Individuals Without Cancer
Cancer survivors were more likely to be older than individuals without a history of cancer, particularly among those age 18 to 64 years (Table 1). Compared with individuals without cancer, a higher proportion of cancer survivors age 18 to 64 years were women. Cancer survivors in both age groups were more likely to be non-Hispanic white, have more comorbid conditions, and report being in fair or poor health compared with individuals without a history of cancer. Among those age 18 to 64 years, cancer survivors were less likely to be uninsured than individuals without a history of cancer.
Table 1.
Demographic and Clinical Characteristics of the Study Population: Cancer Survivors and Individuals With No History of Cancer: Medical Expenditure Panel Survey, 2008 to 2010
| Characteristic | Age 18-64 Years |
Age ≥ 65 Years |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cancer Survivor |
No History of Cancer (n = 55,972) % | Cancer Survivor |
No History of Cancer (n = 8,459) % | |||||||
| Recently Diagnosed (≤ 1 year; n = 348) |
Previously Diagnosed (> 1 year; n = 1,993) |
Recently Diagnosed (≤ 1 year; n = 214) |
Previously Diagnosed (> 1 year; n = 2,104) |
|||||||
| % | P* | % | P* | % | P* | % | P* | |||
| Age, years | ||||||||||
| 18-29 | 8.5 | < .001 | 4.9 | < .001 | 27.6 | |||||
| 30-34 | 4.5 | 3.2 | 10.5 | |||||||
| 35-39 | 6.4 | 5.2 | 10.6 | |||||||
| 40-44 | 6.0 | 8.9 | 11.0 | |||||||
| 45-49 | 12.1 | 11.6 | 11.2 | |||||||
| 50-54 | 12.4 | 16.9 | 11.5 | |||||||
| 55-59 | 22.0 | 21.5 | 9.6 | |||||||
| 60-64 | 28.1 | 27.8 | 7.9 | |||||||
| 65-69 | 33.7 | .1750 | 23.4 | < .001 | 32.4 | |||||
| 70-74 | 24.9 | 22.3 | 23.0 | |||||||
| 75-79 | 24.1 | 20.6 | 18.3 | |||||||
| 80+ | 17.4 | 33.7 | 26.3 | |||||||
| Sex | ||||||||||
| Men | 46.3 | .3062 | 32.8 | < .001 | 50.3 | 58.8 | .0015 | 46.9 | .0021 | 41.8 |
| Women | 53.7 | 67.2 | 49.7 | 41.2 | 53.1 | 58.2 | ||||
| Race/ethnicity | ||||||||||
| Non-Hispanic white | 82.4 | < .001 | 81.7 | < .001 | 64.8 | 86.0 | < .001 | 87.9 | < .001 | 76.5 |
| Non-Hispanic black | 8.8 | 7.7 | 12.3 | 8.4 | 5.8 | 9.4 | ||||
| Hispanic | 5.6 | 7.0 | 15.7 | 3.1 | 3.7 | 8.4 | ||||
| Non-Hispanic other | 3.2 | 3.5 | 7.2 | 2.6 | 2.5 | 5.7 | ||||
| Education | ||||||||||
| Less than high school graduate | 13.1 | .2634 | 11.4 | < .001 | 16.3 | 19.9 | .5138 | 18.4 | < .001 | 23.9 |
| High school graduate | 29.1 | 30.2 | 29.1 | 37.7 | 34.6 | 34.8 | ||||
| Some college or more | 57.6 | 58.4 | 54.2 | 42.3 | 46.7 | 40.8 | ||||
| Marital status | ||||||||||
| Married | 58.7 | .0753 | 62.1 | < .001 | 52.9 | 63.2 | .0361 | 54.9 | .7134 | 54.1 |
| Not married | 41.3 | 37.9 | 47.1 | 36.8 | 45.1 | 45.9 | ||||
| No. of priority conditions† | ||||||||||
| None | 25.7 | < .001 | 26.5 | < .001 | 52.8 | 4.5 | .0048 | 6.1 | < .001 | 8.3 |
| 1 | 20.2 | 25.8 | 23.8 | 10.8 | 13.7 | 16.1 | ||||
| 2 | 26.9 | 20.4 | 12.5 | 29.2 | 21.1 | 23.9 | ||||
| ≥ 3 | 27.1 | 27.4 | 10.8 | 55.4 | 59.1 | 51.7 | ||||
| Health status | ||||||||||
| Excellent/very good | 36.1 | < .001 | 42.1 | < .001 | 62.3 | 29.7 | < .001 | 39.6 | < .001 | 45.8 |
| Good | 29.7 | 31.6 | 27.3 | 37.3 | 32.5 | 32.7 | ||||
| Fair/poor | 34.2 | 26.2 | 10.5 | 33.0 | 27.7 | 21.2 | ||||
| BMI, kg/m2 | ||||||||||
| Not overweight/obese, < 25.0 | 27.2 | .0580 | 32.1 | .0529 | 35.3 | 27.7 | .5056 | 34.9 | .0120 | 31.3 |
| Overweight/obese, ≥ 25.0 | 66.5 | 64.0 | 61.8 | 64.5 | 58.2 | 63.3 | ||||
| Health insurance | ||||||||||
| Age < 65 years, any private | 74.7 | < .001 | 75.9 | < .001 | 70.8 | |||||
| Age < 65 years, public only | 18.0 | 13.4 | 10.1 | |||||||
| Age < 65 years, uninsured | 7.3 | 10.6 | 19.1 | |||||||
| Age ≥ 65 years, Medicare and private | 55.4 | .1970 | 54.5 | .0012 | 49.2 | |||||
| Age ≥ 65 years, Medicare and public | 8.0 | 8.4 | 10.8 | |||||||
| Age ≥ 65 years, Medicare only | 34.9 | 36.2 | 38.6 | |||||||
Abbreviation: BMI, body mass index.
Compared with those without a history of cancer.
In addition to cancer, Medical Expenditure Panel Survey priority conditions include arthritis, asthma, diabetes, emphysema, coronary heart disease, hypertension, stroke, high cholesterol, angina, and heart attack.
Annual Direct Medical Costs
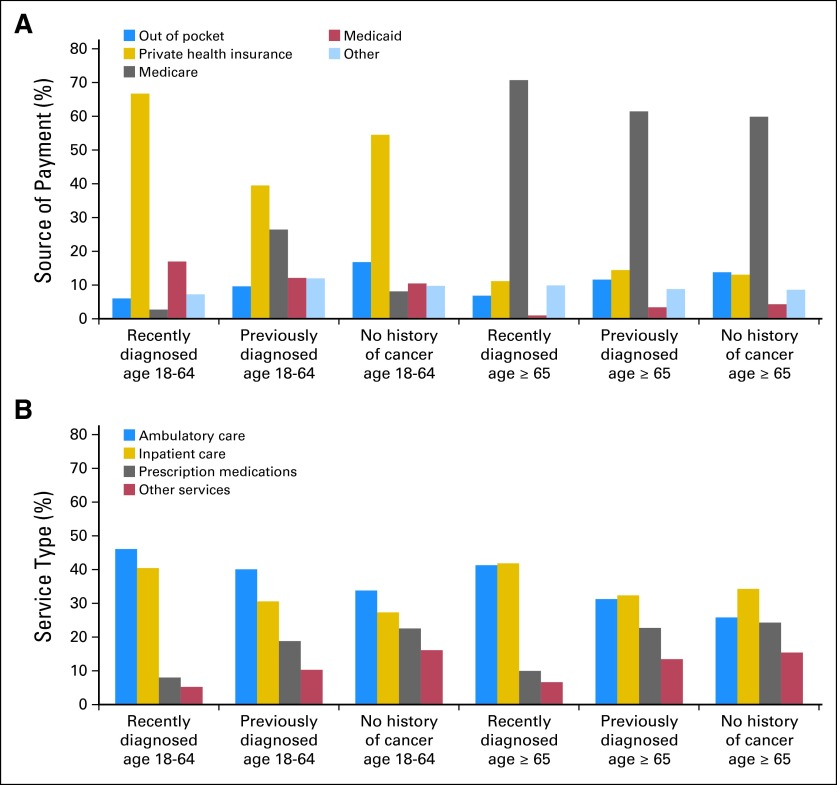
Cancer survivors had higher mean annual medical expenditures than individuals without a history of cancer. Recently diagnosed cancer survivors age 18 to 64 years had average annual total medical expenditures of $17,170, compared with $6,485 among previously diagnosed survivors and $3,611 among those without a history of cancer. Among those age ≥ 65 years, mean annual total medical expenditures were $23,441 among recently diagnosed cancer survivors, $12,357 among previously diagnosed survivors, and $8,724 for those without a history of cancer (Table 2). The largest source of payment for cancer survivors age 18 to 64 years was private health insurance, whereas the largest share among survivors age ≥ 65 years was Medicare (Fig 1A). Among cancer survivors age 18 to 64 years, ambulatory care accounted for the largest share of medical expenditures, whereas inpatient care accounted for the largest share among those age ≥ 65 years (Fig 1B).
Table 2.
Mean Annual Medical Expenditures Among Cancer Survivors and Individuals With No History of Cancer: Medical Expenditure Panel Survey, 2008 to 2010
| Source of Payment and Service Type | Cancer Survivors |
No History of Cancer |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recently Diagnosed (≤ 1 year) |
Previously Diagnosed (> 1 year) |
|||||||||||||
| Unadjusted Expenditure ($) |
Adjusted Expenditure* ($) |
P† | Unadjusted Expenditure ($) |
Adjusted Expenditure* ($) |
P† | Unadjusted Expenditure ($) |
Adjusted Expenditure* ($) |
|||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |||
| Adults age 18-64 years | ||||||||||||||
| All sources of payment | 21,222 | 17,688 to 24,755 | 17,170 | 13,433 to 20,907 | < .001 | 9,369 | 8,268 to 10,471 | 6,485 | 5,496 to 7,474 | < .001 | 3,450 | 3,319 to 3,580 | 3,611 | 3,486 to 3,736 |
| Source of payment | ||||||||||||||
| Out of pocket | 1,463 | 1,230 to 1,696 | 1,107 | 882 to 1,333 | < .001 | 1,182 | 1,033 to 1,331 | 747 | 673 to 820 | < .001 | 590 | 571 to 609 | 617 | 598 to 636 |
| Private health insurance | 13,974 | 10,533 to 17,414 | 12,091 | 8,513 to 15,669 | < .001 | 4,686 | 3,879 to 5,492 | 3,053 | 2,501 to 3,605 | < .001 | 1,867 | 1,769 to 1,965 | 1,995 | 1,891 to 2,098 |
| Medicare | 1,314 | 362 to 2,266 | 505 | 67 to 942 | .262 | 1,172 | 703 to 1,641 | 2,045 | 313 to 3,776 | < .001 | 270 | 233 to 306 | 299 | 229 to 369 |
| Medicaid | 2,535 | 1,207 to 3,864 | 3,091 | 351 to 5,830 | < .001 | 1,121 | 653 to 1,589 | 942 | 477 to 1,407 | .001 | 368 | 328 to 407 | 386 | 340 to 432 |
| Other | 1,936 | 918 to 2,954 | 1,331 | 772 to 1,890 | < .001 | 1,209 | 821 to 1,596 | 931 | 570 to 1,292 | < .001 | 355 | 323 to 387 | 360 | 327 to 394 |
| Service type | ||||||||||||||
| Ambulatory care | 9,560 | 7,474 to 11,645 | 8,316 | 6,158 to 10,474 | < .001 | 3,837 | 3,265 to 4,408 | 2,692 | 2,239 to 3,145 | < .001 | 1,169 | 1,120 to 1,218 | 1,225 | 1,176 to 1,274 |
| Inpatient care | 8,362 | 5,820 to 10,904 | 7,298 | 4,557 to 10,038 | < .001 | 2,463 | 1,792 to 3,134 | 2,054 | 1,081 to 3,027 | .005 | 943 | 852 to 1,034 | 990 | 893 to 1,087 |
| Prescription medications | 1,959 | 1,516 to 2,402 | 1,451 | 961 to 1,942 | .001 | 2,078 | 1,812 to 2,345 | 1,264 | 1,065 to 1,464 | < .001 | 775 | 740 to 810 | 818 | 781 to 854 |
| Other services | 1,329 | 911 to 1,748 | 947 | 642 to 1,251 | .004 | 996 | 862 to 1,130 | 694 | 598 to 789 | .026 | 567 | 535 to 598 | 584 | 550 to 617 |
| Adults age ≥ 65 years | ||||||||||||||
| All sources of payment | 21,731 | 17,349 to 26,112 | 23,441 | 18,367 to 28,514 | < .001 | 12,866 | 11,827 to 13,905 | 12,357 | 11,354 to 13,360 | < .001 | 8,591 | 8,162 to 9,020 | 8,724 | 8,302 to 9,147 |
| Source of payment | ||||||||||||||
| Out of pocket | 1,678 | 1,292 to 2,064 | 1,711 | 1,282 to 2,141 | .012 | 1,529 | 1,382 to 1,676 | 1,451 | 1,319 to 1,583 | .002 | 1,198 | 1,136 to 1,260 | 1,220 | 1,156 to 1,284 |
| Private health insurance | 2,385 | 1,561 to 3,210 | 2,771 | 1,400 to 4,143 | .001 | 1,908 | 1,476 to 2,340 | 1,799 | 1,479 to 2,119 | < .001 | 1,124 | 1,010 to 1,237 | 1,154 | 1,036 to 1,271 |
| Medicare | 15,292 | 11,306 to 19,279 | 17,409 | 12,727 to 22,091 | < .001 | 7,746 | 6,989 to 8,502 | 7,634 | 6,824 to 8,443 | < .001 | 5,222 | 4,870 to 5,575 | 5,269 | 4,933 to 5,605 |
| Medicaid | 120 | 0 to 267 | 273 | 0 to 572 | .528 | 395 | 160 to 629 | 433 | 214 to 652 | .602 | 312 | 224 to 399 | 388 | 244 to 532 |
| Other | 2,254 | 1,285 to 3,224 | 2,456 | 1,024 to 3,888 | < .001 | 1,288 | 928 to 1,648 | 1,101 | 889 to 1,313 | .001 | 735 | 646 to 824 | 767 | 673 to 861 |
| Service type | ||||||||||||||
| Ambulatory care | 9,435 | 6,736 to 12,134 | 9,914 | 6,839 to 12,989 | < .001 | 3,965 | 3,438 to 4,493 | 3,898 | 3,418 to 4,377 | < .001 | 2,256 | 2,092 to 2,419 | 2,271 | 2,114 to 2,429 |
| Inpatient care | 8,319 | 5,630 to 11,009 | 10,048 | 6,316 to 13,780 | < .001 | 4,307 | 3,680 to 4,934 | 4,036 | 3,374 to 4,698 | .005 | 2,884 | 2,613 to 3,155 | 3,012 | 2,714 to 3,309 |
| Prescription medications | 2,529 | 1,963 to 3,095 | 2,406 | 1,830 to 2,981 | .340 | 2,816 | 2,500 to 3,131 | 2,836 | 2,456 to 3,215 | < .001 | 2,131 | 2,023 to 2,239 | 2,134 | 2,032 to 2,236 |
| Other services | 1,439 | 1,001 to 1,877 | 1,596 | 1,070 to 2,121 | .351 | 1,789 | 1,405 to 2,173 | 1,681 | 1,391 to 1,970 | .012 | 1,329 | 1,192 to 1,467 | 1,356 | 1,206 to 1,505 |
NOTE. Calculations were made using the Medical Expenditure Panel Survey–Household Component, 2008 to 2010. All monetary amounts are converted to 2010 dollars using the Personal Health Care Expenditure Price Index. Ambulatory care includes office-based provider visits and outpatient visits. Other services include emergency room visits, home health visits, dental visits, vision expenses, and other medical expenditures.
Predicted margins from a generalized linear regression model with a gamma distribution and a log link controlling for age, sex, race/ethnicity, and number of comorbid conditions.
Reflects the difference in adjusted mean expenditures compared with individuals with no history of cancer.
Fig 1.
Percentage of medical expenditures by (A) source of payment and (B) service type. Recently diagnosed was defined as being diagnosed ≤ 1 year from the time of survey, previously diagnosed was defined as being diagnosed more than 1 year from the time of survey. Adjusted percentages are from predicted marginals from a generalized linear model with a gamma distribution and a log link controlling for age, sex, race/ethnicity, and number of comorbid conditions. Other payment sources included Veterans Affairs, TRICARE, other federal sources, other state and local sources, worker's compensation, other unclassified sources, other private sources, and other public sources. Ambulatory care includes office-based provider visits and outpatient visits. Other services include emergency room visits, home health visits, dental visits, vision expenses, and other medical expenditures.
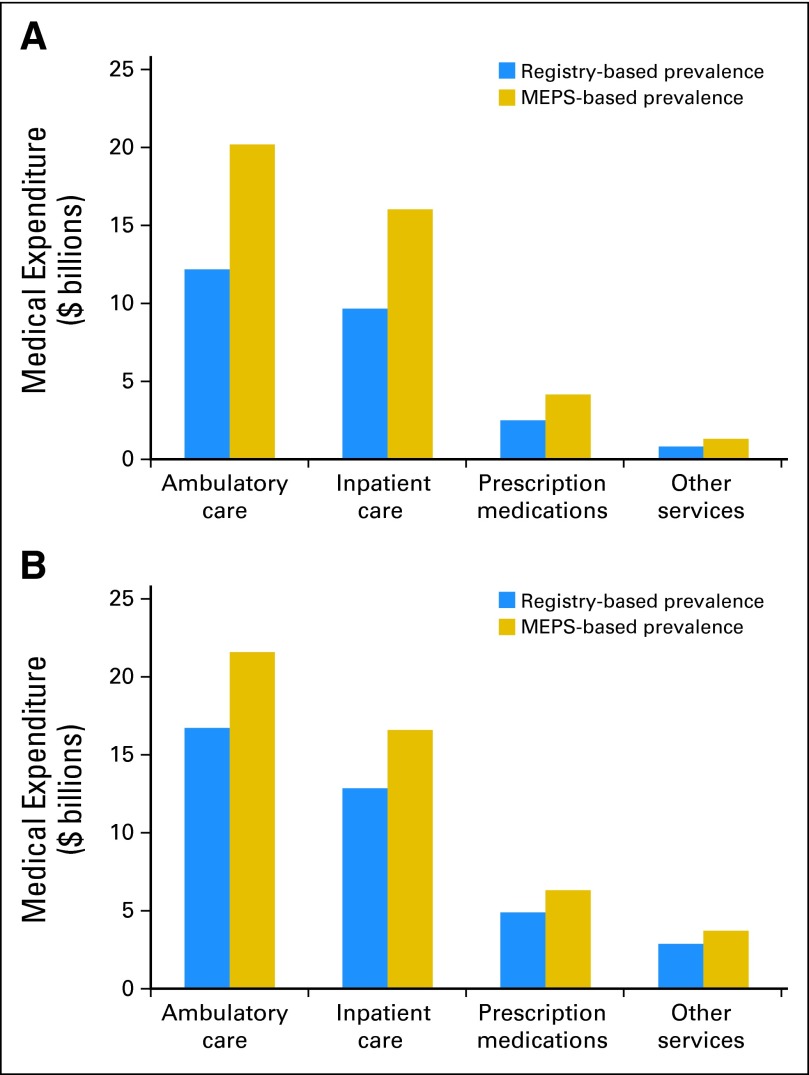
The plausible range of aggregate net annual medical expenditures was $25.2 to $41.7 billion among cancer survivors age 18 to 64 years and $37.3 to $48.1 billion among survivors age ≥ 65 years. The largest share of aggregate net expenditures came from ambulatory care, followed by inpatient care, prescription medications, and other services (Fig 2).
Fig 2.
Aggregate annual net medical expenditure ranges by service type among adult cancer survivors (A) age 18 to 64 years and (B) age ≥ 65 years. National level aggregate net medical expenditures were calculated by multiplying the number of cancer survivors in each age group by the per-person excess expenditure. Prevalence estimates from the Medical Expenditure Panel Survey (MEPS) sample weights and age-specific estimates calculated from cancer registries1 were used to estimate a plausible range. Ambulatory care includes office-based provider visits and outpatient visits. Other services include emergency room visits, home health visits, dental visits, vision expenses, and other medical expenditures.
Annual Indirect Morbidity Costs
Cancer survivors age 18 to 64 years were more likely to report employment disability, an increased number of missed work days as a result of health, and an increased number of additional days spent in bed as a result of health than individuals without a history of cancer. Among individuals age 18 to 64 years, total annual per capita lost productivity was $4,694 among recently diagnosed cancer survivors, $3,593 among previously diagnosed survivors, and $2,040 among individuals without a history of cancer.
Among cancer survivors age ≥ 65 years, those recently diagnosed reported significantly more lost household productivity compared with individuals without a history of cancer, whereas no significant difference was observed among those previously diagnosed. Although cancer survivors in this age group had an increased likelihood of employment disability and an increased number of missed work days as a result of health than individuals without a history of cancer, the differences were not statistically significant. Among individuals age ≥ 65 years, total annual per capita lost productivity was $6,133 among recently diagnosed cancer survivors, $5,295 among previously diagnosed survivors, and $4,409 among individuals without a history of cancer (Table 3).
Table 3.
Annual Lost Productivity Among Cancer Survivors and Individuals With No History of Cancer: Medical Expenditure Panel Survey, 2008 to 2010
| Productivity Measure | Cancer Survivors |
No History of Cancer |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recently Diagnosed (≤ 1 year) |
Previously Diagnosed (> 1 year) |
|||||||||||||
| Unadjusted |
Adjusted |
P* | Unadjusted |
Adjusted |
P* | Unadjusted |
Adjusted |
|||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |||
| Adults age 18-64 years | ||||||||||||||
| Total per capita productivity loss, $ | 7,335 | 5,323 to 9,715 | 4,694 | 3,038 to 6,353 | 6,205 | 5,272 to 7,277 | 3,593 | 3,005 to 4,180 | 1,954 | 1,803 to 2,088 | 2,040 | 1,908 to 2,163 | ||
| Employment disability | ||||||||||||||
| Unable to work as a result of illness/injury, %† | 15.3 | 11.1 to 20.6 | 7.9 | 5.1 to 10.7 | .006 | 15.4 | 13.3 to 17.9 | 8.4 | 7.2 to 9.6 | < .001 | 4.5 | 4.1 to 4.8 | 4.7 | 4.4 to 5.0 |
| Per capita productivity loss, $‡ | 5,159 | 3,743 to 6,947 | 2,664 | 1,720 to 3,608 | 5,193 | 4,485 to 6,036 | 2,833 | 2,428 to 3,237 | 1,517 | 1,383 to 1,619 | 1,585 | 1,484 to 1,686 | ||
| Missed work days among employed individuals | ||||||||||||||
| Per capita productivity loss, No. of days§ | 16.4 | 12.4 to 20.4 | 16.9 | 10.8 to 23.0 | < .001 | 5.6 | 4.5 to 6.7 | 4.6 | 3.6 to 5.6 | .003 | 3.2 | 3.1 to 3.4 | 3.3 | 3.1 to 3.4 |
| Per capita productivity loss, $‖ | 1,595 | 1,206 to 1,984 | 1,644 | 1,050 to 2,237 | 545 | 438 to 652 | 447 | 350 to 545 | 311 | 302 to 331 | 321 | 302 to 331 | ||
| Lost household productivity | ||||||||||||||
| Per capita productivity loss, No. of days§ | 14.3 | 9.2 to 19.3 | 9.5 | 6.6 to 12.5 | < .001 | 11.5 | 8.6 to 14.5 | 7.7 | 5.6 to 9.8 | < .001 | 3.1 | 2.9 to 3.4 | 3.3 | 3.0 to 3.6 |
| Per capita productivity loss, $¶ | 581 | 374 to 784 | 386 | 268 to 508 | 467 | 349 to 589 | 313 | 227 to 398 | 126 | 118 to 138 | 134 | 122 to 146 | ||
| Adults age ≥ 65 years | ||||||||||||||
| Total per capita productivity loss, $ | 6,989 | 3,517 to 11,907 | 6,133 | 3,090 to 9,843 | 5,231 | 4,292 to 6,301 | 5,295 | 4,328 to 6,237 | 4,346 | 3,901 to 4,870 | 4,409 | 3,943 to 4,867 | ||
| Employment disability | ||||||||||||||
| Unable to work as a result of illness/injury, %† | 14.4 | 9.6 to 20.9 | 12.9 | 8.2 to 17.6 | .455 | 13.1 | 11.1 to 15.5 | 13.3 | 11.2 to 15.3 | .050 | 11.1 | 10.1 to 12.3 | 11.2 | 10.2 to 12.2 |
| Per capita productivity loss, $‡ | 4,856 | 3,237 to 7,048 | 4,350 | 2,765 to 5,935 | 4,417 | 3,743 to 5,227 | 4,485 | 3,777 to 5,159 | 3,743 | 3,406 to 4,148 | 3,777 | 3,440 to 4,114 | ||
| Missed work days among employed individuals | ||||||||||||||
| Per capita productivity loss, No. of days§ | 15.7 | 0.0 to 42.4 | 11.4 | 0.0 to 29.7 | .148 | 4.4 | 2.6 to 6.2 | 4.4 | 2.7 to 6.2 | .230 | 3.2 | 2.5 to 4.0 | 3.4 | 2.5 to 4.2 |
| Per capita productivity loss, $‖ | 1,527 | 0 to 4,124 | 1,109 | 0 to 2,889 | 428 | 253 to 603 | 428 | 263 to 603 | 311 | 243 to 389 | 331 | 243 to 408 | ||
| Lost household productivity | ||||||||||||||
| Per capita productivity loss, No. of days§ | 12.5 | 6.9 to 18.1 | 16.6 | 8.0 to 25.1 | .005 | 9.5 | 7.3 to 11.6 | 9.4 | 7.1 to 11.7 | .111 | 7.2 | 6.2 to 8.2 | 7.4 | 6.4 to 8.5 |
| Per capita productivity loss, $¶ | 508 | 280 to 735 | 674 | 325 to 1,019 | 386 | 296 to 471 | 382 | 288 to 475 | 292 | 252 to 333 | 301 | 260 to 345 | ||
NOTE. Calculations were made using the Medical Expenditure Panel Survey–Household Component, 2008 to 2010. All monetary amounts are in 2010 US dollars.
Reflects the difference in adjusted productivity loss compared with individuals with no history of cancer.
Adjusted mean estimated using predicted margins from a logistic regression model controlling for age, sex, race/ethnicity, number of comorbid conditions, and education.
Annual productivity loss is the product of the median annual wage ($33,721)23 and the adjusted percentage unable to work as a result of illness/injury.
Adjusted mean estimated using predicted margins from a negative binomial regression model controlling for age, sex, race/ethnicity, number of comorbid conditions, and education.
Annual productivity loss is the product of the median national daily wage23 ($16.21/hour × 6 hours = $97.26/day) and adjusted number of days lost from work.
Annual productivity loss is the product of the value of daily home productivity in 2010 dollars ($40.61)26 and adjusted number of additional bed days.
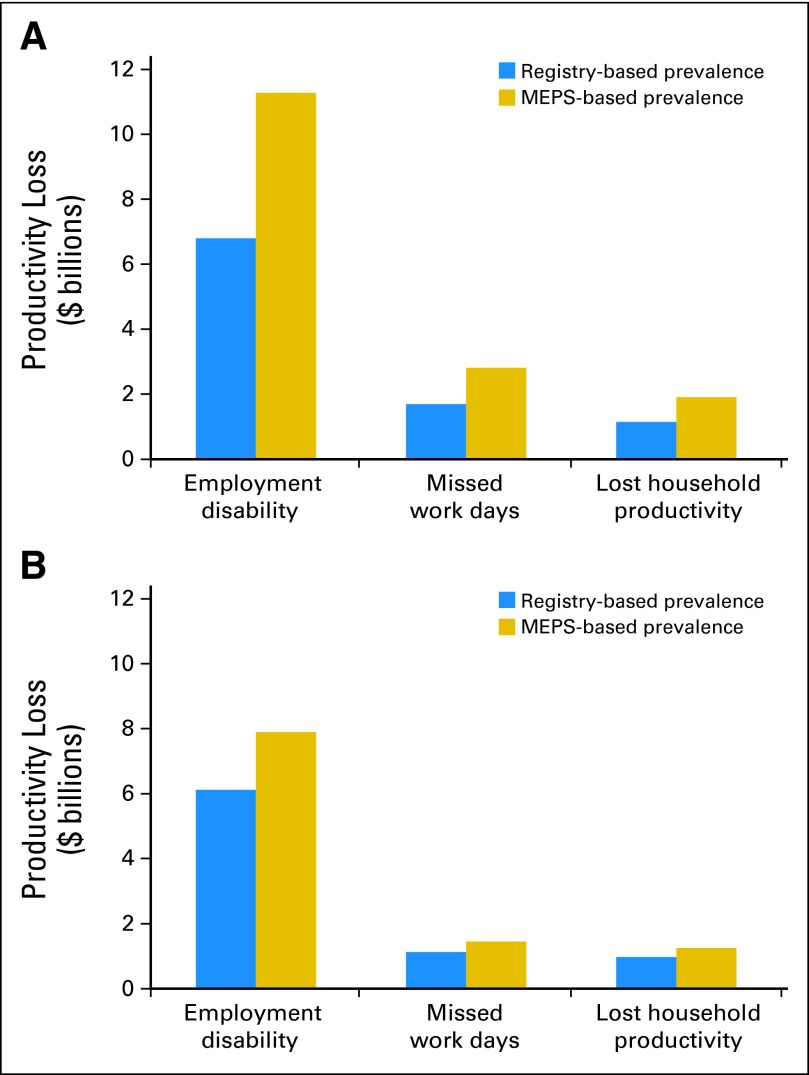
The plausible range of aggregate annual net productivity loss among cancer survivors was $9.6 to $16.0 billion among those age 18 to 64 years and $8.2 to $10.6 billion among those age ≥ 65 years. The largest share of aggregate lost productivity across both age groups came from employment disability, followed by missed work days and lost household productivity (Fig 3).
Fig 3.
Aggregate annual net productivity loss ranges among adult cancer survivors (A) age 18 to 64 years and (B) age ≥ 65 years. National-level aggregate net productivity loss was calculated by multiplying the number of cancer survivors in each age group by the per-person excess cost. Prevalence estimates from the Medical Expenditure Panel Survey (MEPS) sample weights and age-specific estimates calculated from cancer registries1 were used to estimate a plausible range.
Sensitivity Analysis
Among cancer survivors age 18 to 64 years, per capita excess annual medical expenditures ranged from $9,947 to $17,171 (base case: $13,559) among those recently diagnosed and from $2,010 to $3,738 (base case: $2,874) among those previously diagnosed. Excess annual indirect morbidity costs ranged from $1,704 to $4,208 (base case: $2,654) per recently diagnosed cancer survivor and from $992 to $2,459 (base case: $1,553) per previously diagnosed survivor. Among cancer survivors age ≥ 65 years, per capita excess annual medical expenditures ranged from $10,065 to $19,367 (base case: $14,717) among those recently diagnosed and from $3,052 to $4,213 (base case: $3,633) among those previously diagnosed. Meanwhile, excess annual indirect morbidity costs ranged from $1,075 to $2,715 (base case: $1,724) per recently diagnosed cancer survivor and from $570 to $1,406 (base case: $886) per previously diagnosed survivor.
DISCUSSION
This study demonstrates that cancer survivorship is associated with a considerable economic impact on society. In 2008 to 2010, the annual excess economic burden of cancer survivorship among those recently diagnosed was $16,213 per cancer survivor age 18 to 64 years and $16,441 per survivor age ≥ 65 years. The annual excess economic burden among those previously diagnosed was $4,427 per cancer survivor age 18 to 64 years and $4,519 per survivor age ≥ 65 years. Excess medical expenditures composed the largest share, accounting for 83.6% and 89.5% of the total excess burden among recently diagnosed cancer survivors and 64.9% and 80.4% among previously diagnosed survivors age 18 to 64 years and ≥ 65 years, respectively. To our knowledge, this is the first study to quantify both medical expenditures and lost productivity as a result of cancer survivorship in adults of all ages at the national level, using the same data source, allowing for important comparisons of the economic burden between groups and by type of burden.
An important study strength is our ability to examine medical expenditures by care setting and source of payment, including out-of-pocket expenditures, because many previous studies examined expenditures in a single setting (eg, hospital)32 or for a single insurer.12–14 Overall, the largest source of payment among cancer survivors age 18 to 64 was private insurance, whereas Medicare was the largest source among those age ≥ 65 years. The relative contribution of medical expenditures by source of payment differed between groups; for example, Medicare accounted for a larger proportion and private insurance accounted for a smaller proportion of expenditures among previously diagnosed cancer survivors compared with those recently diagnosed and those without a history of cancer among individuals age 18 to 64 years. This may be a result of several factors including shifts in employment and disability-related Medicare eligibility.33 Out-of-pocket expenditures were higher among cancer survivors than individuals without a cancer history, particularly among those recently diagnosed, with annual excess expenditures averaging $490 and $491 among those age 18 to 64 years and ≥ 65 years, respectively. Given changes in insurance related to the Patient Protection and Affordable Care Act, it is important to monitor medical expenditures by source of payment.
Cancer survivors are more likely to incur higher indirect morbidity costs than individuals without a cancer history. An important strength of this study is the ability to examine costs separately among working-age adults and those age ≥ 65 years. Our results indicate that excess lost productivity was greater among working-age adults and those recently diagnosed with cancer. Lost productivity differed substantially across groups; for example, recently diagnosed cancer survivors had significantly more lost work days than those previously diagnosed and those without a history of cancer.
Aggregate national estimates of excess medical expenditures and morbidity costs among cancer survivors ranged from $80.4 to $116.5 billion, depending on whether the estimates were derived from registries or household reports. There are several possible reasons for the difference in estimated prevalence. Compared with registry-based methods, household-reported cancer history under-identifies rare and short-survival, high-cost cancers.29,30 Additionally, because the cancer history question included malignancy of any type, household report likely over-identifies individuals with preinvasive disease. Thus, our per capita estimates are likely understated.
Our national estimates of medical expenditures are lower than most previous estimates,34 reflecting differences in the samples of cancer survivors identified. Previous studies in cohorts of newly diagnosed incident patients with cancer have shown expenditures to be the highest after diagnosis and at the end of life and lowest in the intermediate phase.6,7,12,34 However, because the majority of cancer survivors in a specific year are longer term cancer survivors, with approximately two thirds ≥ 5 years since diagnosis,35 prevalent cancer survivors in the MEPS will primarily be those in the intermediate, low-cost period. Additionally, previous studies examining cancer care costs among individuals age 18 to 64 years using earlier years of the MEPS15,36,37 only captured cancer survivors with cancer-related health care during the survey year, resulting in an overestimation of per-person medical expenditures.8 Only recently has the MEPS allowed for the identification of all adults ever diagnosed with cancer. Our estimates are consistent with the only other study using a prevalence-based definition of cancer survivors and MEPS data to examine medical expenditures among adults age less than 65 years.8 Our study builds on this analysis, also assessing medical expenditures among adults age ≥ 65 years and examining productivity losses among both age groups.
Although MEPS is one of the most detailed nationally representative data sources available to estimate the economic burden of cancer survivorship, there are a number of limitations in this study. First, this study relied on household-reported data, including the identification of cancer survivors, which introduces potential reporting biases. However, such bias may be limited, given the general agreement between household reports and physician-reported conditions.38,39 Second, the use of population-based survey data may lead to an underestimation of rare cancers and cancers with short survival. Third, we were unable to examine costs associated with terminal care, which are among the most costly on a per capita basis.12 Lastly, we were unable to examine the burden by cancer site given inadequate sample size.
We likely underestimate the burden of cancer survivorship among adults, as we did not include caregivers' productivity losses, intangible costs associated with pain and suffering, presenteeism costs, and patient transportation costs. Future analyses should examine these additional costs. Although the focus of this study was on cancer survivors, our estimates can be combined with mortality costs to give a more complete picture of the burden of cancer in the United States. Previous studies have shown lost productivity from premature mortality to be between $115.8 and $173.1 billion annually.40,41
The 2005 Institute of Medicine report, From Cancer Patient to Cancer Survivor: Lost in Translation, highlighted key gaps in cancer survivorship research, including the need for national estimates of the burden of cancer, examining the financial impact of cancer on survivors and their families, and studies on employment patterns.3 Through a new collaborative effort, the MEPS Experiences With Cancer Survivorship Supplement promises to address these key gaps in cancer survivorship research by providing important information to help improve the quality of the cancer survivorship experience and reduce the burden of cancer in the United States.42
In summary, the economic burden of cancer survivorship is substantial, resulting in excess health care expenditures and lost productivity costs among survivors compared with individuals without a history of cancer. The economic impact of cancer is considerable and long lasting. Although the economic burden is greatest shortly after diagnosis, the burden is also high years after a cancer diagnosis. With the number of cancer survivors projected to increase to nearly 18 million by 2022,1 the economic burden of cancer is also likely to increase. Multifaceted prevention strategies including research, education, policy change, and sustained intervention programs may help reduce the economic impact of cancer. Information in this article characterizing the major sources of economic burden may be helpful in guiding the development of comprehensive intervention programs to improve the quality of the cancer survivorship experience and decrease the burden of cancer in the United States.
Footnotes
Processed as a Rapid Communication manuscript.
Presented in part at the 18th Annual International Meeting of the International Society for Pharmacoeconomics and Outcomes Research, New Orleans, LA, May 18-22, 2013.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the National Institutes of Health, Massachusetts General Hospital, or Emory University.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: Gery P. Guy Jr
Data analysis and interpretation: Gery P. Guy Jr, Donatus U. Ekwueme, K. Robin Yabroff, Emily C. Dowling, Janet S. de Moor
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Cancer survivors–United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60:269–272. [PubMed] [Google Scholar]
- 3.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 4.Ng AK, Travis LB. Second primary cancers: An overview. Hematol Oncol Clin North Am. 2008;22:271–289. doi: 10.1016/j.hoc.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Oeffinger KC, Bhatia S. Second primary cancers in survivors of childhood cancer. Lancet. 2009;374:1484–1485. doi: 10.1016/S0140-6736(09)61885-7. [DOI] [PubMed] [Google Scholar]
- 6.Brown ML, Riley GF, Schussler N, et al. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care. 2002;40(suppl):IV-107–117. doi: 10.1097/00005650-200208001-00014. [DOI] [PubMed] [Google Scholar]
- 7.Yabroff KR, Warren JL, Banthin J, et al. Comparison of approaches for estimating prevalence costs of care for cancer patients: What is the impact of data source? Med Care. 2009;47(suppl):S64–S69. doi: 10.1097/MLR.0b013e3181a23e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Short PF, Moran JR, Punekar R. Medical expenditures of adult cancer survivors aged < 65 years in the United States. Cancer. 2011;117:2791–2800. doi: 10.1002/cncr.25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Tangka FK, Trogdon JG, et al. The personal financial burden of cancer for the working-aged population. Am J Manag Care. 2009;15:801–806. [PubMed] [Google Scholar]
- 10.Yabroff KR, Lawrence WF, Clauser S, et al. Burden of illness in cancer survivors: Findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–1330. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 11.Moran JR, Short PF, Hollenbeak CS. Long-term employment effects of surviving cancer. J Health Econ. 2011;30:505–514. doi: 10.1016/j.jhealeco.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yabroff KR, Lamont EB, Mariotto A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100:630–641. doi: 10.1093/jnci/djn103. [DOI] [PubMed] [Google Scholar]
- 13.Fireman BH, Quesenberry CP, Somkin CP, et al. Cost of care for cancer in a health maintenance organization. Health Care Financ Rev. 1997;18:51–76. [PMC free article] [PubMed] [Google Scholar]
- 14.Taplin SH, Barlow W, Urban N, et al. Stage, age, comorbidity, and direct costs of colon, prostate, and breast cancer care. J Natl Cancer Inst. 1995;87:417–426. doi: 10.1093/jnci/87.6.417. [DOI] [PubMed] [Google Scholar]
- 15.Tangka FK, Trogdon JG, Richardson LC, et al. Cancer treatment cost in the United States: Has the burden shifted over time? Cancer. 2010;116:3477–3484. doi: 10.1002/cncr.25150. [DOI] [PubMed] [Google Scholar]
- 16.Max W, Rice DP, Sung HY, et al. The economic burden of prostate cancer, California, 1998. Cancer. 2002;94:2906–2913. doi: 10.1002/cncr.10532. [DOI] [PubMed] [Google Scholar]
- 17.Max W, Rice DP, Sung HY, et al. The economic burden of gynecologic cancers in California, 1998. Gynecol Oncol. 2003;88:96–103. doi: 10.1016/s0090-8258(02)00101-4. [DOI] [PubMed] [Google Scholar]
- 18.Max W, Sung HY, Stark B. The economic burden of breast cancer in California. Breast Cancer Res Treat. 2009;116:201–207. doi: 10.1007/s10549-008-0149-4. [DOI] [PubMed] [Google Scholar]
- 19.Cohen JW, Monheit AC, Beauregard KM, et al. The Medical Expenditure Panel Survey: A national health information resource. Inquiry. 1996;33:373–389. [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. MEPS survey background. http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. [DOI] [PubMed]
- 21.Warren JL, Brown ML, Fay MP, et al. Costs of treatment for elderly women with early-stage breast cancer in fee-for-service settings. J Clin Oncol. 2002;20:307–316. doi: 10.1200/JCO.2002.20.1.307. [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality. Using the appropriate price indices for analyses of health care expenditures or income across multiple years. http://meps.ahrq.gov/about_meps/Price_Index.shtml.
- 23.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 2004;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 24.US Bureau of Labor Statistics. May 2011 national occupational employment and wage estimates, United States. http://www.bls.gov/oes/current/oes_nat.htm#00-0000.
- 25.Sullivan PW, Ghushchyan V, Wyatt HR, et al. Productivity costs associated with cardiometabolic risk factor clusters in the United States. Value Health. 2007;10:443–450. doi: 10.1111/j.1524-4733.2007.00199.x. [DOI] [PubMed] [Google Scholar]
- 26.Fu AZ, Qiu Y, Radican L, et al. Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions. Diabetes Care. 2009;32:2187–2192. doi: 10.2337/dc09-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grosse SD, Krueger KV, Mvundura M. Economic productivity by age and sex: 2007 estimates for the United States. Med Care. 2009;47(suppl):S94–S103. doi: 10.1097/MLR.0b013e31819c9571. [DOI] [PubMed] [Google Scholar]
- 28.US Bureau of Labor Statistics. Consumer Price Index. http://www.bls.gov/cpi/data.htm.
- 29.Byrne J, Kessler LG, Devesa SS. The prevalence of cancer among adults in the United States: 1987. Cancer. 1992;69:2154–2159. doi: 10.1002/1097-0142(19920415)69:8<2154::aid-cncr2820690823>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 30.Hewitt M, Breen N, Devesa S. Cancer prevalence and survivorship issues: Analyses of the 1992 National Health Interview Survey. J Natl Cancer Inst. 1999;91:1480–1486. doi: 10.1093/jnci/91.17.1480. [DOI] [PubMed] [Google Scholar]
- 31.Cockburn M, Swetter SM, Peng D, et al. Melanoma under-reporting: Why does it happen, how big is the problem, and how do we fix it? J Am Acad Dermatol. 2008;59:1081–1085. doi: 10.1016/j.jaad.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seifeldin R, Hantsch JJ. The economic burden associated with colon cancer in the United States. Clin Ther. 1999;21:1370–1379. doi: 10.1016/s0149-2918(99)80037-x. [DOI] [PubMed] [Google Scholar]
- 33.Sabatino SA, Coates RJ, Uhler RJ, et al. Health insurance coverage and cost barriers to needed medical care among U.S. adult cancer survivors age < 65 years. Cancer. 2006;106:2466–2475. doi: 10.1002/cncr.21879. [DOI] [PubMed] [Google Scholar]
- 34.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trogdon JG, Tangka FK, Ekwueme DU, et al. State-level projections of cancer-related medical care costs: 2010 to 2020. Am J Manag Care. 2012;18:525–532. [PMC free article] [PubMed] [Google Scholar]
- 37.Thorpe KE, Howard D. Health insurance and spending among cancer patients. Health Aff (Millwood) 2003;W3(suppl):189–198. doi: 10.1377/hlthaff.w3.189. [DOI] [PubMed] [Google Scholar]
- 38.Bush TL, Miller SR, Golden AL, et al. Self-report and medical record report agreement of selected medical conditions in the elderly. Am J Public Health. 1989;79:1554–1556. doi: 10.2105/ajph.79.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harlow SD, Linet MS. Agreement between questionnaire data and medical records: The evidence for accuracy of recall. Am J Epidemiol. 1989;129:233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- 40.Ekwueme DU, Guy GP, Jr, Li C, et al. The health burden and economic costs of cutaneous melanoma mortality by race/ethnicity–United States, 2000 to 2006. J Am Acad Dermatol. 2011;65(suppl):S133–S143. doi: 10.1016/j.jaad.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 41.Bradley CJ, Yabroff KR, Dahman B, et al. Productivity costs of cancer mortality in the United States: 2000-2020. J Natl Cancer Inst. 2008;100:1763–1770. doi: 10.1093/jnci/djn384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yabroff KR, Dowling E, Rodriguez J, et al. The Medical Expenditure Panel Survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv. 2012;6:407–419. doi: 10.1007/s11764-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]