Abstract
Background & Aims
The aim of this study was to assess factors associated with healthcare utilization in patients with chronic liver disease with a focus on pain, opioid use, and psychiatric symptoms.
Methods
We retrospectively assessed a consecutive sample of 1286 visitors to a hepatology clinic with chronic liver disease. Baseline psychiatric symptoms, pain, and opioid prescriptions were collected. Liver-related clinic visits, total clinic visits, phone calls, and hospitalizations were assessed over a subsequent 6-month period. Multivariable logistic and negative binomial regression models were used to determine the medical and psychosocial factors associated with increased healthcare utilization.
Results
Over a 6-month period, hospitalization was more common among patients with pain (13% vs. 7%, p<0.0001) and opioid usage (18% vs. 6% p<0.0001). Pain and opioid usage were independently and significantly associated with an increased hospitalizations and median number of clinic visits and phone calls (p<0.0001). In multivariable modeling, hospitalization was significantly associated with opioid use (OR=2.72, CI=1.72,4.29), Child’s Class B (OR=2.24, CI=1.19,4.14) and C (OR=8.51, CI=4.18,17.27) cirrhosis, and cardiopulmonary disease (OR=2.11, CI=1.28,3.41). Pain and opioid usage were independently and significantly associated with numbers of phone calls and total outpatient visits, as were medical comorbidities and Child’s Class. The significant predictors of increased outpatient liver-related visits were pain (IRR=1.13, CI=1.02,1.26), interferon usage (IRR=1.75,CI=1.54,1.98), and more advanced liver disease (IRR=1.58,CI=1.32,1.88).
Conclusions
Pain and prescription opioid usage were significantly linked to increased healthcare utilization, suggesting the need to evaluate and incorporate evidence-based pain management strategies into routine care of patients with chronic liver disease.
Keywords: Healthcare costs, pain management, cirrhosis
Introduction
Chronic liver disease carries a significant burden for affected individuals and society. In addition to progressive disability, patients with cirrhosis require greater inpatient and outpatient care (1). In general, chronic liver disease is costly in terms of healthcare expenditures, though the factors associated with increased costs have yet to be fully elucidated. Patients with hepatitis C virus (HCV) were found to have a four-fold increase in 1-year costs compared to age and sex-matched controls (2). Similarly, recent studies demonstrated high healthcare utilization among patients with advanced liver disease. Patients with cirrhosis have been found to have a 1-month readmission rate of 20-37% (3, 4). Factors associated with higher hospitalization rates have included both disease-specific variables, such as the Model for End-Stage Liver Disease (MELD) score, being listed for liver transplant, or having hyponatremia, and liver-independent factors such as the number of medications, male gender, and diabetes (3). Beyond being simply a financial burden, repeat admissions also correlated with increased 90-day mortality.
Whereas these studies clearly highlight the importance of type and stage of liver disease and medical comorbidities, potentially relevant and modifiable psychosocial factors have yet to be addressed in the existing models. These factors have been shown to be important in other disease processes. For example, anxiety was associated with readmission for patients with chronic obstructive pulmonary disease (5) and depression has been associated with 10% of all hospital admissions and longer inpatient stays (6). In addition to psychiatric illness, pain is a frequent reason for physician visits, emergency room encounters and hospitalizations (7). Chronic opioid use has been correlated with far higher healthcare utilization costs, even when patients are adherent to their prescription regimen (8). Pain is common among patients with liver disease (9, 10). Despite their potential impact, no study has previously explored the impact of psychosocial factors, pain, and opioid-driven pain management on healthcare utilization in a consecutive cohort of ambulatory patients seeking care for their chronic liver disease. We hypothesized that these factors would be important predictors of hospitalizations, clinic phone calls, and outpatient clinic visits in this population.
Patients and Methods
Population
This protocol was approved by the Institutional Review Board of the University of Pittsburgh. We reviewed the charts of all consecutive visitors to the Center for Liver Diseases at the University of Pittsburgh Medical Center (UPMC) from December 1, 2010 to January 31, 2011. To be included in the study, patients had to visit a hepatologist or physician extender and have a chronic liver disease, defined as expected to last or lasting ≥6 months. Pregnant or previously transplanted patients were excluded. Baseline variables were defined at the time of the first visit, and patients were then followed for 6 months from the index visit.
Demographics and medical comorbidities
Age at the index visit was recorded. Gender, race, and marital status were self-reported and abstracted from the chart. Cardiopulmonary disease was defined as having any of the following diagnoses in the chart: hypertension, congestive heart failure (CHF), coronary artery disease (CAD), or chronic obstructive pulmonary disease (COPD)/asthma. A diagnosis of diabetes was based on a diagnosis in the chart.
Liver disease variables
Patients were classified based on the designation by a hepatologist into the following categories of liver disease: HCV±alcohol, alcohol-related, non-alcoholic fatty liver disease (NAFLD) including patients with “cryptogenic” cirrhosis thought to be most likely related to NAFLD, and other. Classification of cirrhosis was defined based on the note at the index visit into none and Child-Pugh classification. A history of hepatic encephalopathy or ascites was based on the clinical notes and review of the medications. Ascites was further classified into present on the day of the index visit or not.
Psychiatric Symptoms and Substance Abuse
Mood and sleep symptoms were classified based on the self-report review of systems form at the index visit. Mood symptoms were defined as responding yes to any of the following symptoms of anxiety or depression: “feeling overwhelmed”, “anxious/nervous”, “lonely/depressed”, or “thoughts of hurting yourself in the past month”. Emotional distress was defined as responding yes to the following: “During the past 4 weeks have you experienced any emotional difficulties that have affected your ability to complete your activities of daily living?” Substance abuse variables including history of nicotine use, illicit drug use, and alcohol use were all collected from the best available data in the electronic medical record (EMR). Because very few patients admitted to active alcohol and drug use, past and present use were grouped together. Nicotine use combined all tobacco products. Alcohol use was categorized as affirmative if classified as more than “social” by the physician.
Pain and medication use
Patients were asked by a triage nurse if they had pain as a part of routine care. If they said they had pain or gave a score >0 on a 0 to 10 Likert pain scale, they were considered to have pain at the index visit. The data were then reanalyzed using a pain level >5 at the index visit to define pain, excluding those without pain scores from the analyses. Medications at the time of the index visit were abstracted from the EMR. Psychiatric medications were classified into selective serotonin reuptake inhibitor/serotonin norepinephrine reuptake inhibitors (SSRI/SNRI), tricyclic antidepressants (TCA), trazodone, benzodiazepines, and other sleep medications.
Healthcare utilization
Given that patients tend to stay within the UPMC system and its affiliates for their healthcare and that the electronic medical record (EMR) captures all visits, phone calls, and inpatient stays within a large network of hospitals and clinics, the EMR was used to abstract for each patients the number of outpatient visits, phone calls to a physician’s office, and hospitalizations over a 6 month period for each patient.
Statistical Analysis
All data were analyzed in the R statistical package, version 2.15.2 (11). Baseline characteristics for patients with and without hospitalization were compared using chi-square for categorical variables and t-tests for continuous variables in univariate testing. Those variables with p<0.20 in univariate testing were included in the pool of potential predictors for the final logistic regression model, which assessed factors associated with hospitalization over a 6-month period. One model was made using Child-Pugh Classification of cirrhosis vs. no cirrhosis and a second model was made substituting signs of decompensated cirrhosis including ascites and encephalopathy. Outpatient healthcare utilization was not used as a predictor of hospitalization because outpatient visits could be concurrent with or after hospitalization.
For univariate testing the median number of phone calls and clinic visits were compared between levels of categorical variables using Wilcoxon Rank-Sum or Kruskal-Wallis tests. The number of clinic visits and phone calls were compared for continuous variables using Spearman’s correlation coefficients. Those variables significantly related to the outcomes of interest in univariate testing were included in the full negative binomial regression models. Substance abuse factors were highly correlated with etiology of liver disease and so were excluded, and analgesics were collapsed into one variable. Because of the high correlation between emotional distress and mood symptoms and the stronger relationship of mood symptoms to outcomes on univariate testing, emotional distress was eliminated from the models. Two models were made: one with Child Classification and the other with symptoms of decompensated cirrhosis. Models were made looking specifically at primary care and liver-related visits. A secondary analysis assessed the effect of including only patients who rated their pain as moderate (>5 on a scale of 1-10).
Logistic regression was used to model the outcome of hospitalization, while negative binomial regression was used to model the three outcomes of number of clinic visits, number of primary care visits, and number of phone calls, all of which best matched a distribution of overdispersed count data. The model for hospitalizations and the model for liver clinic visits had too few outcomes and too little dispersion respectively to allow for the inclusion of all covariates that were included in the other models. For these models the StepAIC function in R which uses automated forward and backwards elimination to optimize Akaike information criterion (AIC) was used to find a final parsimonious model (12). Multi-level variables were reported with an overall p-value from a Wald test and with pairwise p-values for each level that were adjusted for multiple comparisons using a Holm-Bonferroni correction. Continuous variables including age and BMI were standardized before entry into the regression models. Ninety-five percent confidence intervals (CI) were calculated. Two-way interactions between pain and opioid use were considered for all models. Additionally, the absence of significant multicollinearity was confirmed for each model using a pre-specified variance inflation factor of 5.
Results
Patient Sample
The final cohort consisted of 1286 patients, after 151 were excluded. The most common reasons for exclusion were a lack of chronic liver disease (n=98), acute hepatitis (n=24), and prior liver transplantation (n=20). The group was 51% male and 84% Caucasian with a mean age of 54±13 years. Cirrhosis was present in 48% of patients and common etiologies of liver disease included HCV±alcohol (46%), NAFLD (19%), and alcohol alone (10%). Opioids were prescribed to 25%, and pain was endorsed by 19% at the index visit. Psychiatric symptoms were common in the sample; 22% reported mood symptoms and 33% reported sleep symptoms at the index visit.
Hospitalizations
Over the 6 months of follow-up, 9% of the patients in the cohort were hospitalized. In univariate analyses, patients who were hospitalized were older, had more alcohol-based liver disease, more advanced disease, increased ascites and encephalopathy, and more alcohol use and cardiopulmonary disease. Notably, those who were subsequently hospitalized were more likely to endorse symptoms fatigue as well as emotional distress. Pain was present in 33% of hospitalized and 18% of non-hospitalized patients in the study period. Opioid use at the time of the index visit was associated with subsequent hospitalization, and was present in 22% of non-hospitalized and 51% of hospitalized patients. Aspirin and acetaminophen were also more commonly used among those who were subsequently hospitalized. (Table 1)
Table 1.
Baseline Characteristics by Admission Status†
| Variable | No Admission (N=1171) | Admission (N=115) | P |
|---|---|---|---|
| Demographics | |||
| Age | 52.2±13.2 | 56.4±11.3 | 0.0002* |
| BMI | 28.9±6.4 | 29.6±6.1 | 0.24 |
| Female | 574 (49) | 62 (54) | 0.37 |
| Non-white race | 92 (8) | 21 (18) | 0.13 |
| Married | 601 (51) | 58 (50) | 0.93 |
|
| |||
| Liver Disease Variables | |||
| Etiology LD | 0.01* | ||
| HCV±alcohol | 539 (46) | 47 (41) | |
| ETOH | 108 (9) | 22 (19) | |
| NAFLD | 221 (19) | 19 (17) | |
| Other | 303 (26) | 27 (23) | |
| Cirrhosis | <0.0001* | ||
| None | 640 (55) | 34 (30) | |
| A | 314 (27) | 28 (24) | |
| B | 179 (15) | 28 (24) | |
| C | 38 (3) | 25 (22) | |
| Hepatic encephalopathy | 79 (7) | 36 (31) | <0.0001* |
| Ascites | <0.0001* | ||
| Past | 155 (13) | 31 (27) | |
| Current | 64 (5) | 23 (20) | |
|
| |||
| Comorbidities/Substance abuse history | |||
| Nicotine use | 697 (60) | 73 (63) | 0.50 |
| Illicit drug use | 82 (7) | 33 (29) | 0.43 |
| Alcohol use > social | 66 (6) | 49 (43) | 0.01* |
| Cardiopulmonary disease | 237 (20) | 37 (32) | 0.0004* |
| Diabetes | 137 (12) | 17 (15) | 0.41 |
|
| |||
| Pain and psychiatric symptoms | |||
| Mood symptoms | 251 (21) | 31 (27) | 0.14 |
| Trouble sleeping/nightmares | 225 (19) | 23 (20) | 0.75 |
| Fatigue | 342 (29) | 45 (39) | 0.01* |
| Emotional distress | 143 (12) | 23 (20) | 0.03* |
| Pain | 210 (18) | 38 (33) | 0.001* |
|
| |||
| Medications | |||
| Opioids | 262 (22) | 59 (51) | <0.0001* |
| SSRI/SNRI | 380 (32) | 40 (35) | 0.68 |
| TCA | 74 (6) | 5 (4) | 0.52 |
| Benzodiazepines | 211 (18) | 28 (24) | 0.12 |
| Trazodone | 80 (7) | 11 (10) | 0.37 |
| Other Sleeping Aids | 99 (8) | 16 (14) | 0.07 |
| Aspirin | 208 (18) | 32 (28) | 0.01* |
| NSAIDS | 235 (20) | 16 (14) | 0.14 |
| Acetaminophen | 198 (17) | 33 (29) | 0.003* |
| Any analgesic | 511 (44) | 59 (51) | 0.14 |
| Interferon | 122 (10) | 6 (5) | 0.11 |
numbers are presented as mean±sd for continuous and N(column %) for categorical variables,
p<0.05, statistically significant
After controlling for other factors, the final logistic regression model (Table 2) demonstrated that the strongest predictors of subsequent hospitalization among all patients were Child Class B/C cirrhosis, prescription opioid use, and cardiopulmonary disease. When ascites and encephalopathy were entered into the model rather than cirrhosis stage, it was ascites, particularly ongoing ascites, that was the strongest predictor of hospitalization (OR=5.31, CI=2.76,9.95), with opioid use (OR=2.87, CI=1.82,4.52) and cardiopulmonary disease (OR=2.23, CI=1.37,3.60) remaining significant in the final model.
Table 2.
Final Logistic Regression Model for Hospitalization†
| Variable | OR | 95% CI | P | Variable | OR | 95% CI | P |
|---|---|---|---|---|---|---|---|
| Opioid use | 2.72 | 1.72,4.29 | <0.0001* | Opioid use | 2.87 | 1.82,4.52 | <0.001* |
| Fatigue | 1.47 | 0.92,2.33 | 0.10 | Sleep Medications | 1.75 | 0.88,3.29 | 0.09 |
| Cardiopulmonary disease | 2.11 | 1.28,3.41 | 0.003* | Cardiopulmonary disease |
2.23 | 1.37,3.60 | 0.001* |
| Child Class | <0.001* | Ascites | <0.001* | ||||
| Class A (vs. none) | 1.58 | 0.89,2.79 | 0.12 | Past | 2.90 | 1.68,4.90 | <0.001* |
| Class B (vs. none) | 2.24 | 1.19,4.14 | 0.02* | Present | 5.31 | 2.76,9.95 | <0.001* |
| Class C (vs. none) | 8.51 | 4.18,17.27 | <0.001* |
Statistically significant, p<0.05. The p-value for Child Class category was corrected with Holm-Bonferroni correction, p-value for the overall variable was based on the Wald test.
models were made with either Child's class or ascites/PSE and the complete final models after AIC optimization are shown.
Number of Clinic Visits and Phone Calls
The number of clinic visits varied broadly in the study, with 30 patients having ≥10 visits (Figure 1). Figure 2 demonstrates that as the number of visits increased, the number of liver-related visits decreased. By definition, those patients with one visit had a liver-related visit (i.e., the index visit), whereas only 27% of visits among patients with ≥10 visits were liver-related. The number of phone calls also varied widely; 24% had none, 22% had one call, and 9% had ≥10 in a 6-month period (Figure 1).
Fig. 1.
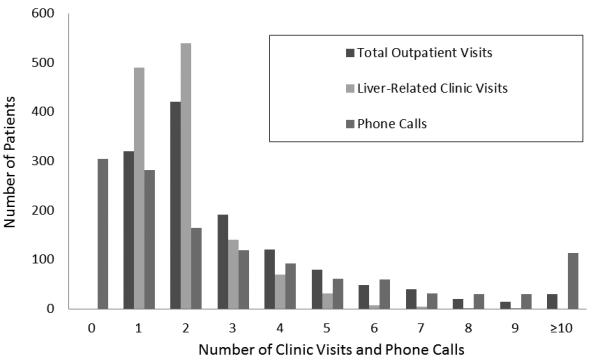
Histogram of Number of Visits and Phone Calls Over 6 Months
Fig. 2.
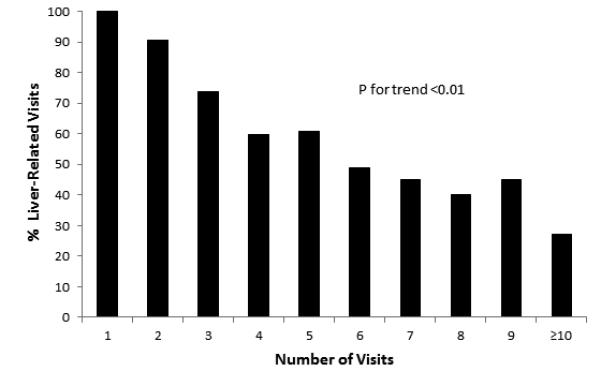
Percentage of Liver-Related Visits by Total Number of Visits
In univariate testing, the median number of clinic visits was significantly associated with race, comorbidities, etiology and stage of liver disease (both Child’s class and ascites/PSE), drug and nicotine use, pain, sleep problems, and psychiatric symptoms. Accordingly, the use of analgesics and opioids, interferon, antidepressants, and benzodiazepines were also related. Differentiating between visits to hepatology or transplant surgery clinics and those to primary care revealed only subtle differences. Comorbid factors, non-opioid analgesics, and emotional distress were not associated with liver-related encounters, while age was additionally correlated with the number of primary care visits. The factors associated with number of phone calls on univariate testing were similar to the number of clinical visits except that race, analgesics, nicotine use, and Child’s class were not but emotional distress, older age, and female gender were associated.
The final negative binomial regression models (Table 3) demonstrate that pain and/or opioid use were important predictors of phone calls and clinic visits. Severity of liver disease was an important predictor of everything other than primary care visits. Psychiatric medications and interferon were also important drivers of healthcare utilization. Importantly, the only factors that predicted number of hepatology clinic visits were interferon use, severity of liver disease, and pain. There was no evidence of any collinearity in any models. Including both opioid use and pain simultaneously in the models did not change their effect sizes by more than 20%.
Table 3.
Final Negative Binomial Regression for Number of Clinic Visits and Number of Telephone Calls
| Total Clinic Visits | Primary Care Visits | Liver-Related Visits | Phone Calls | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | IRR | 95% CI | P | IRR | 95% CI | P | IRR | 95% CI | P | IRR | 95% CI | P |
|
| ||||||||||||
| Pain | 1.15 | 1.04,1.27 | <0.01* | 0.74 | 0.46,1.17 | 0.18 | 1.13 | 1.02,1.26 | 0.02* | 1.39 | 1.17,1.66 | <0.01* |
| Opioids | 1.16 | 1.05,1.28 | <0.01* | 1.80 | 1.22,2.68 | <0.01* | 1.42 | 1.21,1.68 | <0.01* | |||
| Age | 1.00 | 0.95,1.05 | 0.99 | 1.24 | 1.01,1.51 | 0.04* | 1.03 | 0.95,1.11 | 0.44 | |||
| Female | 1.09 | 1.002,1.19 | 0.04* | 1.61 | 1.12,2.33 | <0.01* | 1.27 | 1.10,1.47 | <0.01* | |||
| Non-white | 1.20 | 1.07,1.35 | <0.01* | 1.80 | 1.11,2.96 | 0.01* | 1.00 | 0.80,1.25 | 0.99 | |||
| Nicotine | 1.10 | 1.01,1.21 | 0.03* | 1.67 | 1.13,2.46 | <0.01* | 1.12 | 0.96,1.30 | 0.15 | |||
| CPD | 1.39 | 1.26,1.53 | <0.01* | 3.00 | 2.08,4.38 | <0.01* | 1.57 | 1.32,1.85 | <0.01* | |||
| Diabetes | 1.19 | 1.06,1.34 | <0.01* | 1.77 | 1.11,2.87 | 0.02* | 1.26 | 1.03,1.55 | 0.03* | |||
| Etiology (vs. HCV) | 0.69 | 0.41 | 0.06 | |||||||||
| Alcohol | 0.92 | 0.79,1.08 | 0.31 | 0.67 | 0.34,1.32 | 0.24 | 1.17 | 0.91,1.51 | 0.42 | |||
| NAFLD | 0.95 | 0.83,1.07 | 0.39 | 0.68 | 0.41,1.14 | 0.15 | 1.09 | 0.88,1.34 | 0.43 | |||
| Other | 0.98 | 0.87,1.10 | 0.73 | 0.85 | 0.53,1.38 | 0.50 | 1.28 | 1.06,1.55 | 0.03* | |||
| Cirrhosis Class (vs. none) | <0.001* | 0.52 | <0.01* | <0.01* | ||||||||
| Class A | 0.96 | 0.87,1.07 | 0.47 | 0.84 | 0.54,1.31 | 0.41 | 1.03 | 0.93,1.15 | 0.54 | 1.11 | 0.94,1.33 | 0.22 |
| Class B | 1.23 | 1.08,1.40 | <0.01* | 1.24 | 0.73,2.11 | 0.43 | 1.27 | 1.12,1.43 | <0.01* | 2.09 | 1.69,2.59 | <0.01* |
| Class C | 1.41 | 1.17,1.70 | <0.01* | 1.21 | 0.52,2.87 | 0.64 | 1.58 | 1.32,1.88 | <0.01* | 3.05 | 2.22,4.25 | <0.01* |
| Interferon | 1.57 | 1.38,1.79 | <0.01* | 1.46 | 0.84,2.56 | 0.37 | 1.75 | 1.54,1.98 | <0.01* | 0.89 | 0.69,1.15 | 0.39 |
| Analgesics | 1.02 | 0.94,1.11 | 0.60 | 1.18 | 0.83,1.68 | 0.37 | 0.90 | 0.78,1.05 | 0.17 | |||
| Benzo | 1.10 | 0.99,1.22 | 0.07 | 1.18 | 0.77,1.81 | 0.44 | 1.31 | 1.10,1.56 | <0.01* | |||
| SSRI/SNRI | 1.03 | 0.94,1.14 | 0.52 | 1.08 | 0.72,1.63 | 0.69 | 1.08 | 0.98,1.18 | 0.12 | 1.06 | 0.89,1.25 | 0.53 |
| Mood sxs | 1.04 | 0.93,1.15 | 0.51 | 1.74 | 1.12,2.70 | 0.01* | 1.08 | 0.90,1.29 | 0.41 | |||
| Sleep sxs | 1.04 | 0.94,1.14 | 0.47 | 0.89 | 0.60,1.30 | 0.54 | 0.99 | 0.85,1.16 | 0.90 | |||
CPD=cardiopulmonary disease, benzo=benzodiazepines, SSRI/SNRI=selective serotonin reuptake inhibitors/selective norepinephrine reuptake inhibitor, sxs=symptoms
statistically significant p<0.05. The p-values for Child Class and etiology were corrected with Holm-Bonferroni correction, p-values for the overall variables were based on the Wald test.
When pain was defined as a pain score of >5 on a 10 point scale and compared to no pain, there were not any substantial changes to the models. In addition to all of the variables in the aforementioned model pain was also in the final model of hospitalization (OR=1.75, CI=0.92,3.19, p=0.07). When ascites and encephalopathy were substituted for Child’s Class, the models also did not change substantially, but it appeared that ascites was more significantly related to healthcare utilization than encephalopathy, which was non-significant in all models.
Discussion
This is the first study to assess the predictors of clinic visits, phone calls, and hospitalizations in outpatients with chronic liver disease. We have found that pain and/or opioid-based pain regimens are significant predictors of all measures of healthcare utilization in this population. These have not been previously assessed as potential drivers of the increasingly recognized high healthcare utilization among patients with chronic liver disease. Previously, it has been found that more advanced disease is a driver of healthcare utilization among patients with HCV and cirrhosis (3, 4, 13, 14). While disease factors as well as medical comorbidities account for a large amount of the variation in readmission rates and costs, they do not fully explain the picture. Interestingly, one recent attempt to standardize and optimize chronic disease management failed to decrease readmissions or improve quality of life among patients with chronic liver disease (15), suggesting that factors other than etiology, treatment, and complications of the underlying liver disease influence utilization in this population. Our results thus provide important and new insight, demonstrating that pain, opioid use, and psychiatric variables are associated with increased healthcare utilization.
Using a large sample of outpatients with chronic liver diseases of all stages and etiologies, we confirmed the burden of liver disease on patients and the healthcare system. Over a 6-month period, 9% of patients required hospitalization, most patients were seen as outpatients at least twice, and nearly 10% were seen at least monthly. This is also the first study to address predictors of telephone encounters among patients with liver disease. Consistent with prior findings (3, 4), etiology and stage of the underlying liver disease and comorbid conditions were important predictors of healthcare resource utilization. Our work extends these findings by identifying pain and prescription opioid use as strongly associated with healthcare utilization in this population.
Pain has not been well-characterized in patients with liver disease. We have previously reported that the majority of patients with liver disease describing pain referred to the abdominal area as a pain location (16). While ascites was a likely contributor to discomfort and pain, this complication of advanced liver disease was not sufficient to explain the high pain prevalence, given that only 32% of those with pain had ever had ascites. The retrospective design of our study does not enable us to determine whether the pain was a presenting motivation for clinic visits and phone calls. However, the model suggests an interpretation that includes pain as an important contributor, with the abdominal location likely motivating affected individuals to seek explanation and/or relief by interacting with specialists dealing with their known disease of an abdominal organ. This highlights the importance of addressing pain and pain management as a means of decreasing healthcare utilization among patients with chronic liver diseases. While often not considered by providers to be the primary motivation for hepatology visits, pain is the most common cause for consultative visits in general gastroenterology practices (17). Others have similarly demonstrated that the presence of pain is associated with increased hospitalizations and diagnostic testing (18, 19). However, this is the first demonstration that pain is one of the major drivers of hepatology clinic visits. This is important because behaviorally-based pain management interventions have been shown to not only improve pain (20) but also reduce opioid use and clinic visits and improve quality of life in other disease models (21, 22).
Opioid use in our study and others was also independently associated with increased healthcare resource utilization (8). Consistent with a recent case-control study, we did not find an association between the use of over-the-counter analgesics in chronic liver disease and hospitalizations (23). The impact of opioid use in liver disease could be caused by several potential mechanisms. Considering the potential sedating and cognitive effects, opioids may lead to exacerbations of hepatic encephalopathy, which may drive healthcare utilization. Primary care providers, who are the typical prescribers of opioids may require frequent check-ins for patients on opioids, but this does not explain increased overall utilization or hospitalization. Additionally it may be the severity of underlying pain or associated psychopathology that drives this relationship.
We noted a significant association between increased healthcare utilization and use of psychiatric medications, which likely are a proxy underlying psychopathology. Depression and anxiety common in patients with chronic liver disease (24, 25) and have been associated with increased healthcare utilization and costs in general cohorts (26). Psychopathology also may affect the interpretation of pain (27). Substance abuse and other preexisting psychiatric disorders often lead to long-term opioid use independent of pain (28), emphasizing the importance of further exploring psychopathology when assessing healthcare utilization in chronic liver disease.
The study demonstrated associations between disease-related variables, pain, psychiatric medications and resource utilization, however there were several limitations. Because of the small number of hospitalizations and the dispersion of the liver clinic visits, only a limited number of potential confounders could be included in the models, necessitating the use of step-wise regression. However, sensitivity testing revealed stability of the results. Given the retrospective nature of our study design, we were unable to control for such potential unmeasured confounders such as marijuana use or other psychiatric disorders that can influence pain perception. Furthermore, data collection was limited to encounters within the network of a single, although dominant regional healthcare system, leaving a potential for external referrals or uncaptured visits, calls, and hospitalizations. Care provision for some of the comorbid conditions and opioid prescription may thus be underestimated; however, disease-related encounters as a focus of this study will largely be limited to the specialty clinic and thus represent a nearly-closed system. Additionally, the UPMC system is a broad-reaching network of local hospitals and clinics with a comprehensive EMR. Despite these caveats, the large and diverse population enabled us to identify important predictors of utilization.
In conclusion, this study highlights the importance of assessing pain and psychiatric disease among patients with chronic liver disease when trying to address high healthcare utilization. Pain and opioid use play an important role in this context, as they are common, confounded by psychiatric comorbidity, significantly affect quality of life, and can be targeted by therapeutic interventions. Opioid-sparing pain management strategies should likely be a part of the comprehensive patient care of patients with chronic liver disease. Given our findings, routine and systematic assessment for and treatment of pain and depression should be addressed in clinical trials as a possible mechanism for improving quality of life and resource utilization among patients with chronic liver disease.
Acknowledgements
We would like to thank Dr. David Benhayon. Shari Rogal was supported by NIH-T32 grant number DK063922. Eva Szigethy has funding from the NIMH. The project described was supported by the National Institutes of Health through Grant Numbers UL1 RR024153 and UL1TR000005. Dr. Szigethy received an honorarium and travel costs from Merck for an international symposium on pediatric IBD.
References
- 1.Rakoski MO, Mccammon RJ, Piette JD, et al. Burden of cirrhosis on older Americans and their families: analysis of the health and retirement study. Hepatology. 2012;55(1):184–91. doi: 10.1002/hep.24616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis KL, Mitra D, Medjedovic J, Beam C, Rustgi V. Direct economic burden of chronic hepatitis C virus in a United States managed care population. J Clin Gastroenterol. 2011;45(2):e17–24. doi: 10.1097/MCG.0b013e3181e12c09. [DOI] [PubMed] [Google Scholar]
- 3.Berman K, Tandra S, Forssell K, et al. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol. 2011;9(3):254–9. doi: 10.1016/j.cgh.2010.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital Readmissions Among Patients With Decompensated Cirrhosis. Am J Gastroenterol. 2011 doi: 10.1038/ajg.2011.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gudmundsson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: role of health status, anxiety and depression. Eur Respir J. 2005;26(3):414–9. doi: 10.1183/09031936.05.00078504. [DOI] [PubMed] [Google Scholar]
- 6.Russo CA, Hambrick MM, Owens PL. Hospital Stays Related to Depression, 2005: Statistical Brief #40. 2006. [PubMed] [Google Scholar]
- 7.Langley P, Muller-Schwefe G, Nicolaou A, Liedgens H, Pergolizzi J, Varrassi G. The societal impact of pain in the European Union: health-related quality of life and healthcare resource utilization. Journal of medical economics. 2010;13(3):571–81. doi: 10.3111/13696998.2010.516709. [DOI] [PubMed] [Google Scholar]
- 8.Leider HL, Dhaliwal J, Davis EJ, Kulakodlu M, Buikema AR. Healthcare costs and nonadherence among chronic opioid users. The American journal of managed care. 2011;17(1):32–40. [PubMed] [Google Scholar]
- 9.Marchesini G, Bianchi G, Amodio P, et al. Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology. 2001;120(1):170–8. doi: 10.1053/gast.2001.21193. [DOI] [PubMed] [Google Scholar]
- 10.Whitehead AJ, Dobscha SK, Morasco BJ, Ruimy S, Bussell C, Hauser P. Pain, substance use disorders and opioid analgesic prescription patterns in veterans with hepatitis C. J Pain Symptom Manage. 2008;36(1):39–45. doi: 10.1016/j.jpainsymman.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 11.R_Core_Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2012. [Google Scholar]
- 12.Venables WN, Ripley BD. Modern Applied Statistics with S. Fourth Edition Springer; New York: 2002. [Google Scholar]
- 13.Gordon SC, Pockros PJ, Terrault NA, et al. Impact of disease severity on healthcare costs in patients with chronic hepatitis C (CHC) virus infection. Hepatology. 2012;56(5):1651–60. doi: 10.1002/hep.25842. [DOI] [PubMed] [Google Scholar]
- 14.Ganesh S, Rogal SS, Yadav D, Humar A, Behari J. Risk factors for frequent readmissions and barriers to transplantation in patients with cirrhosis. PLoS One. 2013;8(1):e55140. doi: 10.1371/journal.pone.0055140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wigg AJ, Mccormick R, Wundke R, Woodman R. Efficacy of a Chronic Disease Management Model for Patients with Chronic Liver Failure. Clin Gastroenterol Hepatol. 2013 doi: 10.1016/j.cgh.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Rogal S, Winger D, Bielefeldt K, Szigethy E. Pain and Opioid Use in Chronic Liver Disease. Dig Dis Sci. doi: 10.1007/s10620-013-2638-5. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179–87. e3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA. Health-related quality of life and healthcare utilization in multimorbidity: results of a cross-sectional survey. Qual Life Res. 2012 doi: 10.1007/s11136-012-0214-7. [DOI] [PubMed] [Google Scholar]
- 19.Dudekula A, O’connell M, Bielefeldt K. Hospitalizations and testing in gastroparesis. J Gastroenterol Hepatol. 2011;26(8):1275–82. doi: 10.1111/j.1440-1746.2011.06735.x. [DOI] [PubMed] [Google Scholar]
- 20.Van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine. 2001;26(3):270–81. doi: 10.1097/00007632-200102010-00012. [DOI] [PubMed] [Google Scholar]
- 21.Ryan S, Packham JC,PTD, Jordan KP. The impact of a nurse-led chronic musculoskeletal pain clinic on healthcare utilization. Musculoskeletal care. 2012;10(4):196–201. doi: 10.1002/msc.1018. [DOI] [PubMed] [Google Scholar]
- 22.Van Hooff ML, Ter Avest W, Horsting PP, et al. A short, intensive cognitive behavioral pain management program reduces health-care use in patients with chronic low back pain: two-year follow-up results of a prospective cohort. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21(7):1257–64. doi: 10.1007/s00586-011-2091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fenkel JM, Coron RN, Daskalakis C, et al. Over-the-counter analgesics in cirrhotic patients: a case-control study examining the risk of hospitalization for liver-associated events. Scand J Gastroenterol. 2010;45(9):1101–9. doi: 10.3109/00365521003663704. [DOI] [PubMed] [Google Scholar]
- 24.Elwing JE, Lustman PJ, Wang HL, Clouse RE. Depression, anxiety, and nonalcoholic steatohepatitis. Psychosom Med. 2006;68(4):563–9. doi: 10.1097/01.psy.0000221276.17823.df. [DOI] [PubMed] [Google Scholar]
- 25.Ewusi-Mensah I, Saunders JB, Wodak AD, Murray RM, Williams R. Psychiatric morbidity in patients with alcoholic liver disease. Br Med J (Clin Res Ed) 1983;287(6403):1417–9. doi: 10.1136/bmj.287.6403.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simon G, Ormel J, Vonkorff M, Barlow W. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152(3):352–7. doi: 10.1176/ajp.152.3.352. [DOI] [PubMed] [Google Scholar]
- 27.Hosoi M, Molton IR, Jensen MP, et al. Relationships among alexithymia and pain intensity, pain interference, and vitality in persons with neuromuscular disease: Considering the effect of negative affectivity. Pain. 2010;149(2):273–7. doi: 10.1016/j.pain.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breckenridge J, Clark JD. Patient characteristics associated with opioid versus nonsteroidal anti-inflammatory drug management of chronic low back pain. J Pain. 2003;4(6):344–50. doi: 10.1016/s1526-5900(03)00638-2. [DOI] [PubMed] [Google Scholar]


