Abstract
PURPOSE
Social integration predicts morbidity and mortality, but relationships with specific health behaviors that could explain this relationship, such as physical activity, have not been established. Additionally, studies associating social integration with health have not distinguished between sources of social contact (family vs. friends), which could be differentially related to health. The purpose of this study was to examine the association between social integration and physical activity, and to explore differences in family and friend social integration.
METHODS
Data came from the 2001 wave of the National Health Interview Survey (NHIS). Adult participants (N=33,326) indicated levels of social integration by reporting whether they had seen and/or called friends and/or family in the past two weeks and also reported their weekly minutes of physical activity. Logistic regression was used to determine odds of meeting PA guidelines (≥150 minutes/week) and odds of inactivity (0 min/week) based on levels of social integration.
RESULTS
Greater integration predicted higher odds of meeting PA guidelines and lower odds of inactivity after controlling for sociodemographic variables. This association was stronger and dose-dependent for integration with friends, whereas moderate family contact predicted greater activity than high levels of family contact.
CONCLUSIONS
Those who are more socially integrated, particularly with friends rather than family, are also more physically active, which could partially explain the link between social integration and morbidity and mortality. Future studies examining this association should distinguish between sources of integration, and explore why and how contact with friends vs. family is differentially associated with health behaviors.
Keywords: physical activity, social integration, NHIS, social support
Introduction
Physical activity (PA) is a well-established preventive health behavior, with evidence demonstrating its ability to protect against a wide array of health conditions, including cardiovascular disease [1, 2], diabetes [3], and depression [4]. Experts recommend that all adults participate in at least 30 minutes of moderate to vigorous PA (defined as any activities that produce at least mild sweating and moderate increase in heart rate) most days of the week in order to fully reap its benefits [5], yet estimates suggest that less than one-third of Americans achieve this goal [6]. Given the profound benefits of PA, gaining a better understanding of the factors that could increase PA among adults is essential.
Among the strong predictors of PA are psychosocial variables, such as social network characteristics. Quality of social interaction (social support), for example, strongly predicts PA. Across races, those with more social support are more likely to engage in regular PA than those without social support [7-12]. A multi-national study found that, across countries, those who reported high social support were twice as likely to be physically active than those who reported low social support [13]. The connection between social support and PA has been found for both general social support [14] and social support specifically for engaging in PA [8, 15].
Social support, however, should not be confused with social integration, a variable referring to the quantity of network members and interactions rather than their actual quality or content[16]. Although these terms are often used interchangeably, the two are qualitatively different and may have very different effects on health and health behavior [16, 17]. Social support is one aspect of social integration and has been identified as one of several pathways through which social integration can be related to health [18]. Other identified pathways may not be as consistently positive in their influence on PA. Social influence, for example, is an important aspect of social integration that establishes social norms, and it could influence health for better or worse depending on the habits and values of others [18]. If peers or family members were not physically active themselves then social influence could be a barrier to PA. Social engagement may define and reinforce social roles, which foster a sense of belonging and connectedness [18]. This, in turn, could motivate individuals to take better care of their health [19]; alternatively, if social roles do not emphasize PA (e.g. role of a caregiver), social engagement may not facilitate PA.
Relatively few studies to date have examined the effects of social integration or quantity of social contact on PA. Those that have do not always show a consistent effect [14] or do not separate it from social support [20]. Although social integration is strongly and negatively associated with all-cause mortality and cardiovascular disease [21-24], the mechanisms of this relationship are not clear. Furthermore, whether this association is related to the adoption of specific health behaviors, such as PA, is relatively unexplored. Thus, how simple contact with family and friends (i.e., social integration) influences frequency of PA is currently unknown.
One weakness of social integration studies is that many examine contact quantity without distinguishing the source. In fact, the vast majority of studies examining the effects of social integration on health combine contact with family and friends into a single index [14, 20, 23, 25-29]. This method supposes that family and friends exert equivalent influences on health, an assumption that may not be accurate. Health-related social norms among friends, for example, may be very different from those among family members. Therefore, contact with family and friends may be differentially related to PA, particularly because contact within each of these networks likely includes a wide range of supportive or unsupportive interactions.
Finally, the effects of family and friend contact may also be moderated by gender, but this question has received limited attention in the literature. Women may face unique social barriers to PA that could lead to greater discouragement from family and peers, such as an emphasis on caregiving[30]. One recent study demonstrated a negative association between social integration and inactivity for both men and women [14], but it was limited to only phone contact and again combined contact with friends and family into a single index. A more thorough investigation of gender and family vs. friend social integration is thus warranted.
The purpose of the current study was to separately investigate the relationships between contact with family and contact with friends and at least moderate PA. Few studies have examined the relationship between social integration and PA, and, to our knowledge, none has looked at how contact with family and friends may differentially predict PA. We also sought to determine how family and friend contact is differentially related to PA among men vs. women. Because physical inactivity (i.e., reporting zero PA) may be predicted by different factors than PA [31] and has been independently associated with health consequences different from those of being insufficiently active [32, 33], we also assessed the relationship between social integration and physical inactivity.
Methods
Participants & Data
Data for the study were taken from the 2001 wave of the National Health Interview Survey (NHIS), a household survey conducted by the Centers for Disease Control and Prevention and the National Center for Health Statistics and is administered yearly by the US Census Bureau. A complex stratified, clustered design that oversamples Hispanics and non-Hispanic Blacks from the non-institutionalized civilian population is used. When weighted, it is representative of the US adult population. One adult per household was randomly chosen to answer a variety of questions on health, healthcare services, and behaviors. The 2001 wave of the survey (N = 33,326) also included several questions about the frequency and nature of contact participants had with family and friends in the past two weeks.
Measures
Physical Activity
The primary dependent variable of interest was whether or not participants met Centers for Disease Control (CDC)/American College of Sports Medicine (ACSM) guidelines for weekly minutes of moderate or vigorous physical activity (MVPA). The CDC/ACSM recommends 150 minutes per week of moderate PA, 75 minutes per week of vigorous PA, or an equivalent combination of the two [34].
MVPA in the current study was measured by self-report. Participants indicated the number of times per week they participated in activities lasting ≥10 minutes that resulted in 1) light sweating and a slight increase in heart rate (moderate activity) and/or 2) heavy sweating and a large increase in heart rate (vigorous activity), as well as the duration of each activity. The measure does not specify context of PA, and thus may include transportation and occupational PA in addition to leisure PA. Frequency and duration were used together to calculate total weekly minutes of MVPA. In accordance with the 2008 Physical Activity Guidelines[34], total MVPA was calculated for each participant by doubling minutes of vigorous activity and adding it to minutes of moderate activity. Participants were classified as sufficiently active if this total met or exceeded 150 minutes. Those who indicated that they never engaged in MVPA were classified as inactive.
Social Integration
The NHIS Survey does not include a standard measure of social integration; rather, it contains a variety of questions that relate to social networks and contact. Participants were asked to indicate whether in the last two weeks they had a) spoken to relatives on the phone, b) spoken to friends on the phone, c) seen relatives (not living in the home) in person, d) seen friends in person, e) participated in a group event, or f) gone to a worship service. Because the latter two do not specify the relationships with those they interacted with (family and/or friends), and could possibly double count the first four items, only the first four questions were used to assess social integration. Although these questions do not assess the number of times participants interacted with their networks, they assess whether or not participants are engaged with their networks and in what mode(s).
Indexes of social integration similar to those used in other studies analyzing the same data set were created [25, 26]. In this case, an index of overall social integration was created by adding the total number of types of contact participants reported during the past two weeks, ranging from 0 (no contact) to 4 (called relatives, called friends, saw relatives, and saw friends). A score of 1 to 3, therefore, indicates the number of types of contact the participant engaged in, but does not specify precisely which types of contact were used. These scores could reflect a number of combinations of calling and/or seeing family and/or friends. This approach of tallying types of contact has been used in previous studies utilizing the NHIS [26] and other large datasets [14, 35, 36]. In order to assess the effects of the social integration source, two additional indexes were created: contact with friends and contact with family. Each source of contact was assessed by adding the types of contact participants had with that source (friend or family) in the past two weeks, yielding either a 0 (neither called nor saw in person), a 1 (either called or saw in person), or a 2 (both called and saw in person).
Demographic Characteristics
We divided participant education into five categories based on the highest grade completed: none/elementary school, some high school, high school diploma or equivalent, some college, and college and/or graduate degree.
Race/ethnicity was determined first by asking participants whether they considered themselves Hispanic/Latino. All participants then selected the race that best described their racial background. If more than one race was chosen, participants were asked to indicate the one that best described them. For the current study, we divided participants in to four racial/ethnic categories: non-Latino White (White), non-Latino Black (Black), Latino, and non-Latino other (Other).
Statistical Analysis
We used logistic regression models to evaluate relationships between indices of social integration with categorical indices of a) sufficient physical activity and b) inactivity. Models including terms for planned covariates (age, gender; Model 1) first evaluated primary relationships with social integration indices and then adjusted further for additional sociodemographic covariates (race/ethnicity, education, and marital status; Model 2), as these variables could be associated with PA and/or social integration. The two models were first run using the total social integration index and then the separate family and friend indexes. Finally, we also conducted an exploratory interaction analysis to test for a possible modifying effect of marital status on the association between social integration and PA. Analyses were conducted in R statistical software [37] using the survey package that allows for complex NHIS survey design when estimating model parameters [38]. Participants missing social integration data (<1% of the sample) were excluded from the analysis.
Results
Sample Characteristics
Weighted means and percentages for all sample characteristics entered into the model are shown in Table 1, both overall and across physical activity variables. The sample was comprised of only slightly more females than males (52%) and was relatively well educated, with more than half of the sample (53%) reporting at least some college education. Approximately one-quarter (26.5%) of the sample comprised ethnic minorities (i.e., non-White). The sample was also quite well integrated: roughly two-thirds of the sample (65.5%) reported all four types of social contact in the past two weeks. Frequency of contact with family and with friends was roughly equal, with 79.4% both seeing and calling friends and 77.1% both seeing and calling family. Participants were also generally inactive. More than one-third (37.7%) reported never getting any PA, and just 43.4% reported meeting PA guidelines.
Table 1.
Sample characteristics by physical activity classification
| Met Activity Requirements |
Inactive |
||||||
|---|---|---|---|---|---|---|---|
| Overall | Yes | No | p | Yes | No | p | |
| % | 43.4 | 56.6 | < .001 | 37.7 | 62.3 | < .001 | |
|
| |||||||
| Age (mean (SD)) | 45.1 (.14) | 41.6 | 47.1 | < .001 | 48.2. | 42.6 | < .001 |
|
| |||||||
| Female (%) | 52 | 46.3 | 56.7 | < .001 | 55.8 | 50.0 | < .001 |
|
| |||||||
| Race/Ethnicity (%) | < .001 | < .001 | |||||
| White | 73.5 | 78.6 | 68.7 | 64.7 | 78.0 | ||
| Black | 11.3 | 9.3 | 13.0 | 14.4 | 9.6 | ||
| Latino | 10.8 | 8.0 | 13.5 | 16.0 | 8.2 | ||
| Other | 4.4 | 4.0 | 4.8 | 4.9 | 4.2 | ||
|
| |||||||
| Education (%) | < .001 | < .001 | |||||
| No HS | 6.3 | 2.7 | 8.6 | 10.9 | 3.1 | ||
| Some HS | 9.1 | 5.9 | 11.1 | 13.0 | 6.4 | ||
| HS diploma | 31.7 | 26.1 | 35.4 | 37.1 | 27.9 | ||
| Some college | 29.2 | 33.1 | 26.2 | 24.9 | 31.8 | ||
| College diploma | 23.8 | 32.2 | 18.6 | 14.1 | 30.7 | ||
|
| |||||||
| Married (%) | 58.1 | 57.9 | 58.6 | 0.37 | 56.9 | 59.2 | .001 |
|
| |||||||
| Total Integration (%) | <.001 | <.001 | |||||
| 0 contacts | 1.9 | 1.0 | 3.1 | 4.1 | 1.0 | ||
| 1 contact | 3.3 | 2.0 | 4.1 | 4.6 | 2.3 | ||
| 2 contacts | 9.9 | 7.8 | 10.7 | 11.5 | 8.1 | ||
| 3 contacts | 19.4 | 20.4 | 18.5 | 17.3 | 20.5 | ||
| 4 contacts | 65.5 | 68.8 | 63.7 | 62.4 | 68.0 | ||
|
| |||||||
| Friend Integration (%) | <.001 | <.001 | |||||
| 0 contacts | 6.5 | 3.7 | 8.4 | 9.9 | 4.2 | ||
| 1 contact | 14.1 | 11.4 | 15.7 | 16.3 | 12.2 | ||
| 2 contacts | 79.4 | 84.9 | 76.0 | 73.8 | 83.5 | ||
|
| |||||||
| Family Integration (%) | <.001 | <.001 | |||||
| 0 contacts | 5.4 | 4.2 | 6.3 | 7.3 | 4.2 | ||
| 1 contact | 17.5 | 18.2 | 16.9 | 16.6 | 18.0 | ||
| 2 contacts | 77.1 | 77.6 | 76.8 | 76.1 | 77.7 | ||
Compared to those not meeting activity requirements, sufficiently active participants were more likely to be younger, male, White, and to have more education. They were also generally more socially integrated, across the general index and both the family and friend indexes. The reverse was true for inactive participants.
Logistic regression – Sufficient physical activity
Table 2 presents the odds ratios from the logistic regression model predicting meeting recommended PA levels. In Model 1 (adjusted only for age and sex), total social integration was significantly predictive of sufficient PA (OR = 1.24, 95% CI: 1.20 – 1.29), indicating that higher levels of social integration were associated with greater odds of sufficient activity.
Table 2.
Odds of meeting physical activity guidelines
| Model 1 | Model 2 | Model 1 | Model 2 | |
|---|---|---|---|---|
| Total Integration Index | 1.24*** | 1.19*** | ||
| Friend Integration | ||||
| No contact (reference) | 1.0 | 1.0 | ||
| Saw or called | 1.59*** | 1.48*** | ||
| Saw and called | 2.33*** | 1.93*** | ||
| Family Integration | ||||
| No contact (reference) | 1.0 | 1.0 | ||
| Saw or called | 1.47*** | 1.33*** | ||
| Saw and called | 1.28** | 1.21** |
Model 1: age, gender
Model 2: Model 1 + education, race/ethnicity, marital status
p ≤ .05
p ≤ .01
p ≤ .001
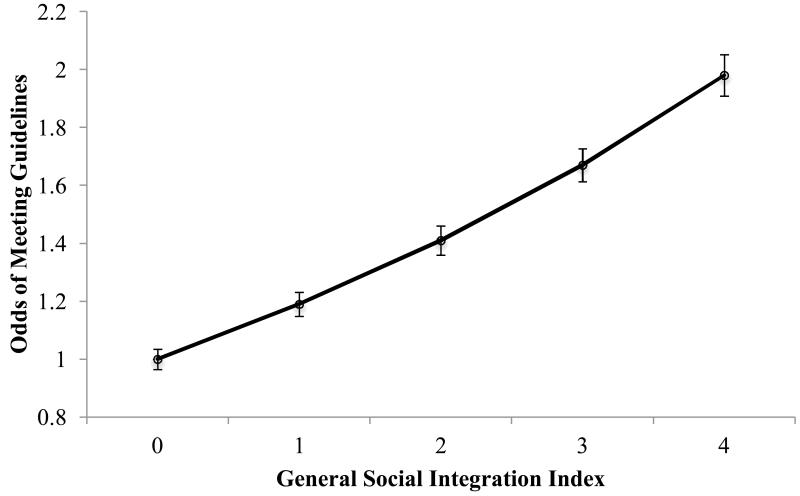
Further adjusting for race/ethnicity, education, and marital status in Model 2 did not appreciably attenuate the predictive value of any of these variables, and social integration remained a significant predictor of activity (OR = 1.19, 95% CI: 1.14 – 1.23). This relationship was dose-dependent, with greater social integration associated with greater odds of activity at every level of social integration (Figure 1).
Figure 1. Integration and Physical Activity.
Odds of being sufficiently active (≥150 minutes/week) from fully adjusted model based on number of types of social contact (calling and/or seeing family, calling and/or seeing friends). Error bars show 95% confidence interval.
Similar results were found when examining friends and family separately (see Table 2). Adjusting only for age and sex (Model 1), both social integration indexes significantly predicted sufficient PA. However, friend integration showed a stronger relationship with PA than family integration, and its relationship was dose-dependent. Specifically, those either seeing or calling friends had 59% higher odds of meeting guidelines than those who had neither seen nor called friends in the past two weeks (OR = 1.59, 95% CI: 1.28-1.70), and participants who both called and saw friends in the past two weeks had more than twice the odds of being sufficiently active than those who reported no contact with friends (OR = 2.33, 95% CI: 1.68 – 2.21).
For family integration, those either seeing or calling family had 47% higher odds of meeting activity requirements (OR = 1.47, 95% CI: 1.27 – 1.71), similar to those who either saw or called friends. However, at the highest level of social integration (both calling and seeing), a large difference emerged between family and friend integration. While friend integration predicted markedly greater odds of activity compared to a moderate level of social integration (either seeing or calling), greater family integration actually showed a decrease in predicting activity compared to moderate social integration (OR = 1.28, 95% CI: 1.11 – 1.47). In the fully adjusted model (Model 2), these relationships were slightly attenuated but still significant.
Logistic Regression – Inactivity
Odds ratios from the logistic regression model predicting inactivity are shown in Table 3. Overall results show an inverse pattern to those predicting sufficient activity. Controlling only for age and sex (Model 1), social integration was significantly and negatively associated with inactivity (OR = 0.78, 95% CI: 0.76 – 0.81), such that those experiencing higher social integration were less likely to report inactivity.
Table 3.
Odds ratios from logistic regression: Inactivity
| Model 1 | Model 2 | Model 1 | Model 2 | |
|---|---|---|---|---|
|
| ||||
| Total Integration Index | 0.78*** | 0.83*** | ||
| Friend Integration | ||||
| No contact (reference) | 1.0 | 1.0 | ||
| Saw or called | 0.60*** | 0.64*** | ||
| Saw and called | 0.42*** | 0.52*** | ||
| Family Integration | ||||
| No contact (reference) | 1.0 | 1.0 | ||
| Saw or called | 0.61*** | 0.69*** | ||
| Saw and called | 0.71*** | 0.76*** | ||
Model 1: age, gender
Model 2: Model 1 + education, race/ethnicity, marital status
p ≤ .05
p ≤ .01
p ≤ .001
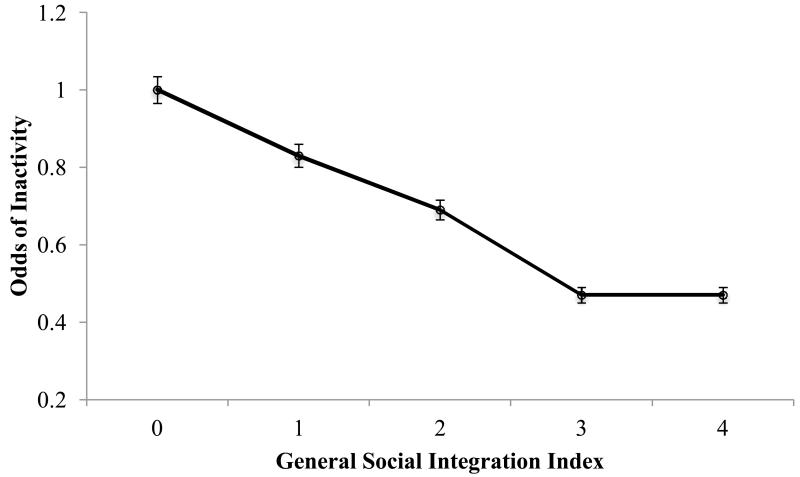
Further adjusting for sociodemographic variables (Model 2) again produced only small changes in odds ratios, and total social integration remained a significant negative predictor of inactivity (OR = 0.83, 95% CI: 0.80 – 0.86). Higher levels of social integration were generally associated with lower odds of inactivity, though the difference among those with three or four social contacts was not substantial (Figure 2).
Figure 2. Integration and Inactivity.
Odds of being inactive (0 minutes/week of activity) from fully adjusted model based on number of types of social contact (calling and/or seeing family, calling and/or seeing friends). Error bars show 95% confidence interval.
Dividing social integration into family and friend indexes showed that family and friend integration were both negatively associated with inactivity. At the moderate level of social integration (i.e., either seeing or calling), family and friends were again very similar in predicting less inactivity (OR = 0.60, 95% CI: 0.53 – 0.68 and OR = 0.61, 95% CI: 0.53 – 0.70, respectively). At the highest level of social integration, however, a greater divergence again emerged. Those who both saw and called friends had 58% lower odds of being inactive (OR = 0.42, 95% CI: 0.38 – 0.47), whereas those who both saw and called family had only 29% lower odds of being inactive (OR = 0.71, 95% CI: 0.62 – 0.81).
The fully adjusted model (Model 2) showed minimal changes in these values. Family and friend integration remained significant negative predictors of inactivity, with the lowest odds of inactivity seen in those who both called and saw friends (OR = 0.52, 95% CI: 0.46 – 0.58).
Gender & Social Integration
To test for differential predictive values of social integration based on gender, an interaction of gender and total social integration was entered into a logistic regression along with age, sex, and total social integration. The analysis showed no significant interaction of social integration and gender on PA (β = .022, SE= .033, p = 0.49) or inactivity (β = .021, SE= .032, p = 0.52). There was also no interaction effect for PA or inactivity in the fully adjusted model (β = .028, SE = .034, p =0.40 and β = .018, SE = .034, p = 0.59, respectively).
Discussion
As with social support, these data show a strong positive relationship between social integration and PA. Those who had any contact with either family or friends were significantly more likely to be sufficiently active than poorly integrated individuals, and this relationship generally increased with greater levels of social integration. Similarly, those who were more integrated generally had lower odds of being inactive than less integrated individuals. These data build on previous studies showing a negative relationship between social integration and mortality [23] by identifying specific health behaviors associated with social integration that could possibly act as mediators of the social integration-mortality connection.
Given the current data, it is unclear what mechanisms may be driving this association. Social integration may encourage greater PA directly if social interaction involves being physically active, or indirectly by enhancing feelings of belonging, connectedness, or general improved mental health, all of which could increase motivation to be healthy and engage in healthy behaviors. Alternatively, it could be that greater PA actually leads to greater social integration through similar direct or indirect mechanisms, or that both PA and social integration are increased by other variables such as mental health.
While the data showed an overall positive effect of social integration, it also revealed important differences between sources of social integration. Specifically, integration with friends was more strongly related to PA than integration with family, to the extent that any level of friend integration more strongly predicted sufficient activity than any level of family integration. This differential pattern was similar for inactivity, in that friend integration generally predicted lower rates of inactivity than family integration. Notably, PA increased with each level of friend integration, such that those who were most active were those who both saw and called friends in the past two weeks. Family integration, however, showed diminishing returns at higher levels of integration. Although those who had both seen and called family members in the past two weeks were still more active than those with no contact, the highest activity was seen in those who reported only one form of contact with family. Friend contact, then, was more strongly and reliably related to activity than family contact. Similar but inverse patterns were seen for inactivity levels, with lower levels of inactivity among those who reported only one form of contact with family compared to both types.
Again, it is unclear what mechanisms may be driving this association. Family and friends may differentially impact an individual’s desire or motivation to be physically active. Studies show that families may not be naturally supportive of exercise and may need to learn how to support other family members’ PA goals [39]. Inconsistent support from social contacts has been cited as a potential reason that social integration is only sometimes associated with better health [17]. Alternatively, this difference between family and friend integration could be due to the way participants actually spend time with family and friends; that is, time spent with friends may be more likely to be active than time spent with family. Of those who only had one type of contact with family, 78% did so over the phone. The highest level of social integration, therefore, appears to be achieved by adding face-to-face time with family, which, as suggested by lower odds of PA at this level of social integration, could compete with spending time being physically active. Friends may be more likely than family members to have similar ages and/or interests, which may better facilitate PA.
These results emphasize a need to distinguish between family and friends when examining effects of social integration. Whereas other studies examining global social integration and PA have generally found a positive relationship[14, 20], our results suggest that by combining family and friends into a single index these studies may actually be underestimating the effect of friend integration. For example, data from Reed et al. [14] generally showed the lowest rates of inactivity in those with moderate levels of social integration, compared to those with none or very high rates of contact. This effect could be partially due to higher levels of global social integration capturing greater family integration, which in our results was associated with slightly less activity than moderate family integration. Because the majority of studies relating social integration and physical health have combined family and friend contact in to one measure, exploring how these indexes are separately related to a wide range of health behaviors and outcomes is worthwhile.
Surprisingly, no interaction was observed between gender and social integration in predicting PA. This finding was unexpected given that social support appears to influence health behavior differently for men and women [40], and it further emphasizes that social integration is not synonymous with support. Future research should investigate the content of social interactions among men and women and how it may influence PA.
Adding sociodemographic variables to the multivariate model did not attenuate the effects of social integration, suggesting minimal mediating or confounding effects of race/ethnicity, education, and marital status. This finding is consistent with a recent study showing that various indicators of social integration were related to overall health status but did not mediate the relationship between SES and health [26]. The sample in the current study was unusually highly educated, with nearly 85% of participants having at least a high school diploma. Because education was the demographic variable most closely related to PA, the sample’s relatively high level of education could also explain why this group was also more physically active (43.5%) than the general population (30-33%)[6].
Limitations
The current data are limited in that they do not enable full exploration of the depth of participant social integration; that is, participants indicated whether or not they had seen or called friends and family over the past two weeks, but did not indicate how often. In this respect the data are better suited to show differences between those who are isolated and those who are at least minimally socially integrated. Daily phone calls to friends surely represent a different level of social integration than biweekly calls, and ideally these levels of social integration should not be treated homogenously. However, the majority of benefits may be apparent among those making any contact compared to those experiencing total isolation, rendering additional contact subject to diminishing returns [14]. Nevertheless, comparing participants at different levels of social integration would be useful, as the low threshold for social integration in this study (a phone call within the past two weeks) resulted in a relatively small comparison group of non-integrated individuals. The high levels of integration in the sample could also be indicative of a bias towards more socially integrated individuals participating in the NHIS survey, while more socially isolated individuals may decline participation or be less accessible.
Conclusions
Social isolation has been identified as a major risk factor for heart disease [22] and is linked to all cause morbidity and mortality [21]. Results from the current study suggest that more socially isolated individuals are also less physically active, which could potentially offer a partial explanation for the association between social isolation and chronic disease. Clearly, more research is needed to determine whether this is a causal relationship, and, if so, the mechanisms through which social integration would motivate PA. Such findings could inform the design of interventions to promote physical activity, determining the type and frequency of social contact most likely to promote PA. These data do suggest, however, that the source of social contact is important and that this variable should not be overlooked when discussing social contact and health.
Acknowledgment
This research was supported in part by a grant from the National Heart, Lung, and Blood Institute (T32HL079891).
References
- 1.Wessel T, Arant C, Olson M, et al. Relationship of Physical Fitness vs Body Mass Index With Coronary Artery Disease and Cardiovascular Events in Women. JAMA. 2004;292(10):1179–1187. doi: 10.1001/jama.292.10.1179. [DOI] [PubMed] [Google Scholar]
- 2.Thompson P, Buchner D, Pina I, Balady G, Williams M, Marcus BH. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Mebatolism (Subcommittee on Physical Activity) Circulation. 2003;107(24):3109–3116. doi: 10.1161/01.CIR.0000075572.40158.77. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein AR, Sesso HD, Lee IM, et al. Relationship of Physical Activity vs Body Mass Index With Type 2 Diabetes in Women. JAMA: The Journal of the American Medical Association. 2004;292(10):1188–1194. doi: 10.1001/jama.292.10.1188. [DOI] [PubMed] [Google Scholar]
- 4.Dunn A, Trivedi M, O’Neal H. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33(6):S587–S597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- 5.Haskell WL, Lee IM, Pate RR, et al. Physical Activity and Public Health: Updated Recommendation for Adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 6.Carlson S, Densmore D, Fulton J, Your M, Kore H.r. Differences in physical activity prevalence and trends from 3 US surveillance systems: NHIS, NHANES, and BRFSS. Journal of Physical Activity and Health. 2009;6(S1):S18–S27. doi: 10.1123/jpah.6.s1.s18. [DOI] [PubMed] [Google Scholar]
- 7.Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006;29(3):281–289. doi: 10.1007/s10865-006-9055-6. [DOI] [PubMed] [Google Scholar]
- 8.Eyler A, Brownson R, Donatelle R, King A, Brown D, Sallis J. Physical activity social support and middle- and older-aged minority women: Results from a U.S. survey. Soc Sci Med. 1999;49(7):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 9.Eyler A. Correlates of physical activity among women from diverse racial/ethnic groups. Journal of Women’s Health & Gender Based Medicine. 2002;11(3):239–253. doi: 10.1089/152460902753668448. [DOI] [PubMed] [Google Scholar]
- 10.Trost SG, Owen N, Bauman A, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34:1996–2000. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Courneya K, Plotnikoff R, Hotz S, Birkett N. Social support and the Theory of Planned Behavior in the exercise domain. American Journal of Health Behavior. 2000;24(4):300–308. [Google Scholar]
- 12.Amesty S. Barriers to physical activity in the Hispanic community. J Public Health Policy. 2003;24:41–58. [PubMed] [Google Scholar]
- 13.Stahl T, Rutten A, Nutbeam D, et al. The importance of the social environment for physical activity lifestyle: Results from an international study. Soc Sci Med. 2001;52:1–10. doi: 10.1016/s0277-9536(00)00116-7. [DOI] [PubMed] [Google Scholar]
- 14.Reed S, Crespo C, Harvey W, Anderson R. Social isolation and physical inactivity in older US adults: Results from the third National Health and Nutrition Examination Survey. European Journal of Sport Science. 2011;11(5):347–353. [Google Scholar]
- 15.Booth M, Owen N, Bauman A, Clavisi O, Leslie E. Social-cognitive and perceived environmental influences associated with physical activity in older Australians. Prev Med. 2000;31:15–22. doi: 10.1006/pmed.2000.0661. [DOI] [PubMed] [Google Scholar]
- 16.Berkman L, Glass T. Social integration, social networks, social support, and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. [Google Scholar]
- 17.Seeman T. Social ties and health: The benefits of social integration. Ann Epidemiol. 1996;6(5):442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- 18.Berkman L, Glass T, Brisette I, Seeman T. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;5(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Syme S. Social Support and Health. Academic Press; San Francisco: 1985. [Google Scholar]
- 20.McAuley E, Jerome G, Marquez DX, Elavsky S, Blissmer B. Exercise self-efficacy in older adults: Social, affective, and behavioral influences. Ann Behav Med. 2003;25:1–7. doi: 10.1207/S15324796ABM2501_01. [DOI] [PubMed] [Google Scholar]
- 21.Uchino B, Cacioppo J, Kiecolt-Glaser J. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 22.House J, Landis K, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 23.Orth-Gomer K, Rosengren A, Wilhelmsen L. Lack of social support and incidence of coronary heart disease in middle-aged Swedish men. Psychosom Med. 1993;55:37–43. doi: 10.1097/00006842-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Berkman L, Syme S. Social networks, host resistance, and mortality: A nine-year follow-up of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 25.Barger S. Perceived emotional support and frequent social contacts are associated with greater knowledge of stroke warning signs: Evidence from two cross-sectional US population surveys. Journal of Health Psychology. 2012;17(2):169–178. doi: 10.1177/1359105311412837. [DOI] [PubMed] [Google Scholar]
- 26.Gorman B, Sivaganesan A. The role of social support and integration for understanding socioeconomic disparities in self-rated health and hypertension. Soc Sci Med. 2007;65:958–975. doi: 10.1016/j.socscimed.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Barger S, Donoho C, Wayment H. The relative contributions of race/ethnicity, socioeconomic status, health, and social relationships to life satisfaction in the United States. Qual Life Res. 2009;18:179–189. doi: 10.1007/s11136-008-9426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reed D, McGee D, Yano K. Social networks and coronary heart disease among Japanese men in Hawaii. Am J Epidemiol. 1983;117:384–396. doi: 10.1093/oxfordjournals.aje.a113557. e. al. [DOI] [PubMed] [Google Scholar]
- 29.Kaplan G, Salonen J, Cohen R, Brand R, Syme S, Puska P. Social connections and mortality from all cause and from cardiovascular disease: Prospective evidence from Eastern Finland. Am J Epidemiol. 1988;128(2):370–380. doi: 10.1093/oxfordjournals.aje.a114977. [DOI] [PubMed] [Google Scholar]
- 30.Yancey A, Ory M, Davis S. Dissemination of physical activity promotion interventions in underserved populations. Am J Prev Med. 2006;31(4):82–91. doi: 10.1016/j.amepre.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 31.Gordon-Larsen P, McMurray RG, Popkin BM. Adolescent physical activity and inactivity vary by ethnicity: The National Longitudinal Study of Adolescent Health. The Journal of Pediatrics. 1999;135(3):301–306. doi: 10.1016/s0022-3476(99)70124-1. [DOI] [PubMed] [Google Scholar]
- 32.Dietz WH. The role of lifestyle in health: the epidemiology and consequences of inactivity. Proc Nutr Soc. 1996;55(03):829–840. doi: 10.1079/pns19960082. [DOI] [PubMed] [Google Scholar]
- 33.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting Time and Mortality from All Causes, Cardiovascular Disease, and Cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 34.U.S.D.o.H.a.H. Services, editor. Physical activity guidelines for Americans. DHHS; Washington, DC: 2008. [Google Scholar]
- 35.Fothergill KE, Ensminger ME, Robertson J, Green KM, Thorpe RJ, Juon HS. Effects of social integration on health: A prospective study of community engagement among African American women. Soc Sci Med. 2011;72(2):291–8. doi: 10.1016/j.socscimed.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michael YL, Berkman LF, Colditz GA, Kawachi I. Living arrangements, social integration, and change in functional health status. Am J Epidemiol. 2001;153(2):123–31. doi: 10.1093/aje/153.2.123. [DOI] [PubMed] [Google Scholar]
- 37.Team RDC. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2011. [Google Scholar]
- 38.Lumley T. Survey: analysis of complex survey samples: R package version 3.26. 2011. [Google Scholar]
- 39.Baranowski T, Nader P, Dunn K, Vanderpool N. Family self-help: Promoting changes in behavior. J Commun. 1982;32(3):161–172. [Google Scholar]
- 40.Treiber FA, Baranowski T, Braden DS, Strong WB, Levy M, Knox W. Social support for exercise: relationship to physical activity in young adults. Prev Med. 1991;20:737–50. doi: 10.1016/0091-7435(91)90068-f. [DOI] [PubMed] [Google Scholar]