Abstract
OBJECTIVE
To estimate the effect of increasing severity of obesity on post-cesarean wound complications and surgical characteristics.
STUDY DESIGN
We performed a retrospective cohort study of consecutive cesarean deliveries at a tertiary care facility from 2004-2008. Four comparison groups were defined by body mass index (BMI kg/cm2) <30 (n=728), 30-39.9 (n=1087), 40-49.9 (n=428), or ≥50 (n=201). The primary outcome was wound complication, defined as wound disruption or infection within 6 weeks post-operative. Surgical characteristics were compared between groups including: administration of pre-operative antibiotics, type of skin incision, estimated blood loss (EBL), operative time, and type of skin closure.
RESULTS
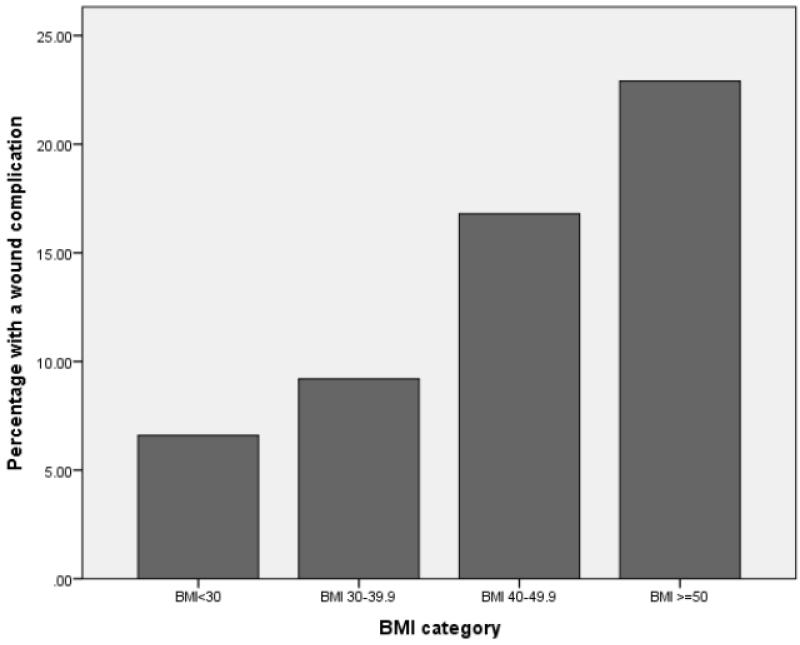
Of the 2444 women with complete follow up data, 266 (10.9%) developed a wound complication. Compared to non-obese women (6.6%), increasing BMI was associated with an increased risk of wound complications: BMI 30.0-39.9, 9.2%, aOR 1.4 [95% CI 0.99-2.0]; BMI 40.0-49.9, 16.8%, aOR 2.6 [95% CI 1.7-3.8]; BMI ≥50, 22.9%, aOR 3.0 [95% CI 1.9-4.9]. Increasing BMI was also associated with increased rates of midline vertical incision, longer operative time, higher EBL, and lower rates of subcuticular skin closure.
CONCLUSION
A dose response relationship exists between increasing BMI and risk of postcesarean wound complications. Increasing obesity also significantly influences operative outcomes.
Keywords: Obese, Cesarean, Wound, Surgical
Introduction
There are over 1.4 million cesarean deliveries performed each year in the United States, and the number is expected to increase.1 Simultaneously, the prevalence of obesity has increased markedly over the past two decades, with over one-third of reproductive age women being classified as obese.2 Obese women are more likely to be delivered by cesarean than women of normal weight, and are at increased risk for operative morbidity including wound complications.3-5 Given the paralleled increasing rates of obesity and cesarean deliveries, it is prudent to consider the societal cost of treating these complications and to determine ways in which the wound complication risk can be decreased.
Previous studies have identified obesity as a risk factor for wound complications, with rates ranging from 3.5% to 30%.6-10 These studies used varied definitions of wound complications, small sample sizes, and were conducted in populations in which obese patients were the minority. Thus far, the relationship between increasing wound complications with degree of obesity has not been established, despite the fact that the obese population represents the greatest burden of cesarean-related morbidity and health care costs.
The primary aim of our study was to evaluate the risk of wound complication after cesarean delivery in non-obese women with BMI <30 compared to obese women, stratified by BMI category. We hypothesized that there will be a dose-response relationship between increasing BMI and risk of wound complications. Secondarily, we aimed to characterize differences in surgical characteristics which may contribute to the increased postcesarean morbidity in obese women.
Materials and Methods
We conducted a retrospective cohort study of all consecutive cesarean deliveries occurring over a 4 year study period from 2004-2008 at Washington University in St. Louis Medical Center. Before initiation of the study, approval was obtained from the Washington University human research protection board. Inclusion criteria consisted of all women who underwent cesarean delivery at this tertiary care facility during the study period regardless of gestational age, indication for delivery, type of skin or uterine incision, and number of gestations. There were no cesarean deliveries that were excluded in this cohort. However analysis was limited to those who had complete follow up data, women with no record of follow-up in our hospital system within 6 weeks post-partum were excluded.
For all women in the cohort, detailed demographic information was extracted from the medical record including medical and surgical history, obstetrics and gynecology history, prenatal history, antepartum records, delivery records, and post-partum records by trained obstetric research nurses. Body Mass Index (BMI) was calculated from height and weight in the medical record from their Labor and Delivery admission. Obesity was defined as BMI ≥ 30 according to the WHO criteria.11 Four comparison groups were defined by BMI <30 (reference group), 30-39.9, 40-49.9, or ≥50.
The primary outcome was a wound complication, defined as the occurrence of a wound seroma, hematoma, separation, dehiscence or infection from time of delivery to 6 weeks post-operative. Women with wound cellulitis were included in those with a wound infection, and women with superficial wound separation not requiring intervention were not included as having a wound complication. Wound complication diagnoses were made in the inpatient setting prior to hospital discharge, in the emergency room, or in the outpatient clinic in follow up. The diagnosis of a wound complication was determined by the treating physician in the various hospital settings, including emergency physicians, obstetricians and gynecologists, and maternal fetal medicine specialists. Finally, women with more than one wound complication, for example, wound hematoma and resultant separation, were only counted once in the composite for wound complication.
Baseline characteristics were compared between each of the study groups and the reference group (BMI < 30). Categorical variables were compared using the Chi-square test. Incidence and 95% confidence intervals were calculated for wound complication by degree of obesity. Bivariate analyses were used to identify potentially confounding factors. Adjusted odds ratios were calculated using logistic regression. Backward step-wise selection was used to reduce the number of variables in the logistic regression model by assessing the magnitude of change in the effect size of wound complication and other risk covariates. Only variables that were statistically significant were included in the final models.
The following surgical characteristics were also compared between groups of increasing BMI: administration of pre-operative antibiotics, type of skin incision, estimated blood loss (EBL), total operative time, and type of skin closure. Women who received pre-operative antibiotics were given medications and dosages according to the American College of Obstetricians and Gynecologists (ACOG) guidelines, and were administered prior to skin incision.12 Estimated blood loss for cesarean delivery was determined by both the anesthesiologist and obstetrician in partnership at completion of the case. Total operative time was defined as time from skin incision to completion of skin closure. Skin closure method was determined by the operating physician, and sutures used for subcuticular closure were size 3-0 to 4-0 of either monocryl or vicryl. Statistical analysis for the secondary outcomes was performed using one-way ANOVA test for continuous variables and Chi-square test for categorical variables. All statistical analyses were completed using STATA software package, version 10, Special Edition (College Station, TX). Bar graphs were created using SPSS software package, version 20.
Results
There were 2543 women who underwent a cesarean during the study period and 2444 women who had complete follow up data and thus were included in the analysis. In the cohort, 728 (30%) women were non-obese, and 1716 (70%) women were obese (BMI ≥ 30). Among obese women, 1087 (44.5%) women had a BMI 30-39.9, 428 (17.5%) women had a BMI 40-49.9, and 201 (8.2%) women had a BMI ≥50. At baseline, increasing BMI was associated with African American race and multiparity. Obese women also had a higher rate of medical comorbidities, specifically gestational diabetes, pre-gestational diabetes, and chronic hypertension. Women with increasing BMI were found to have higher rates of previous cesarean deliveries. The groups were similar in rates of tobacco and drug use, and incidence of advanced maternal age. (Table 1)
Table 1.
Baseline characteristics for women in the cohort compared by BMI
| BMI<30 (n=728) |
BMI 30-39.9 (n=1087) |
BMI 40-49.9 (n=428) |
BMI ≥ 50 (n=201) |
P value | |
|---|---|---|---|---|---|
| Advanced Maternal Age (n=274) |
11.1% | 11.0% | 11.2% | 12.4% | 0.95 |
| Nulliparity (n=963) | 44.1% | 40.0% | 35.3% | 28.4% | <0.01 |
| African American race (n=1628) |
55.4% | 69.1% | 76.4% | 73.1% | <0.01 |
| Tobacco use (n=414) | 16.6% | 17.1% | 17.3% | 16.4% | 0.99 |
| Drug use (n=194) | 8.1% | 8.3% | 7.9% | 5.5% | 0.60 |
| Gestational Diabetes (n=173) |
3.2% | 6.7% | 11.9% | 12.9% | <0.01 |
| Pre-gestational Diabetes (n=104) |
0.8% | 3.4% | 8.2% | 12.9% | <0.01 |
| Chronic Hypertension (n=131) |
1.4% | 4.9% | 8.9% | 14.9% | <0.01 |
| Pre-Eclampsia (n=124) | 4.1% | 5.1% | 5.6% | 7.5% | 0.26 |
| Prior cesarean (n=1033) |
37.5% | 42.0% | 44.9% | 55.2% | <0.01 |
Of the 2444 women who underwent a cesarean, 266 (10.9%) developed a wound complication. When stratified by BMI, increasing BMI was associated with an increased incidence of wound complication. Non-obese women had a wound complication rate of 6.6%. There was a statistically significant relationship between rate of wound complication and increasing BMI: 9.2% in women with BMI 30-39.9 (aOR 1.4, 95% CI 0.99-2.0, p= 0.06), 16.8% in women with BMI 40-49.9 (aOR 2.6, 95% CI 1.7-3.8, p<0.01), and 22.9% in women with BMI ≥50 (aOR 3.0, 95% CI 1.9-4.9, p<0.01), with a p value for test of trend <0.01. Importantly, in stratified analyses, skin incision type and skin closure type were found to have an association with wound complication, and were therefore considered in the adjusted analysis. In the adjusted analysis, only pre-gestational diabetes, midline vertical skin incision, and prior cesarean delivery were found to be significant confounders in the final model; labor prior to cesarean, skin closure method, and gestational diabetes were not significant and thus did not remain in the final model. (Table 2 and Figure 1)
Table 2.
Effect of increasing BMI on risk for wound complications
| BMI<30 (n=728) |
BMI 30-39.9 (n=1087) |
BMI 40-49.9 (n=428) |
BMI ≥ 50 (n=201) |
P value | |
|---|---|---|---|---|---|
| Wound complication Rate (n=266) |
6.6% | 9.2% | 16.8% | 22.9% | <0.01 |
| Adjusted OR (95% CI)* | Reference | 1.4 (0.99-2.0) | 2.6 (1.7-3.8) | 3.0 (1.9-4.9) | - |
adjusted for pre-gestational diabetes, prior cesarean, and vertical skin incision
Figure 1.
Incidence of wound complication related to increasing BMI
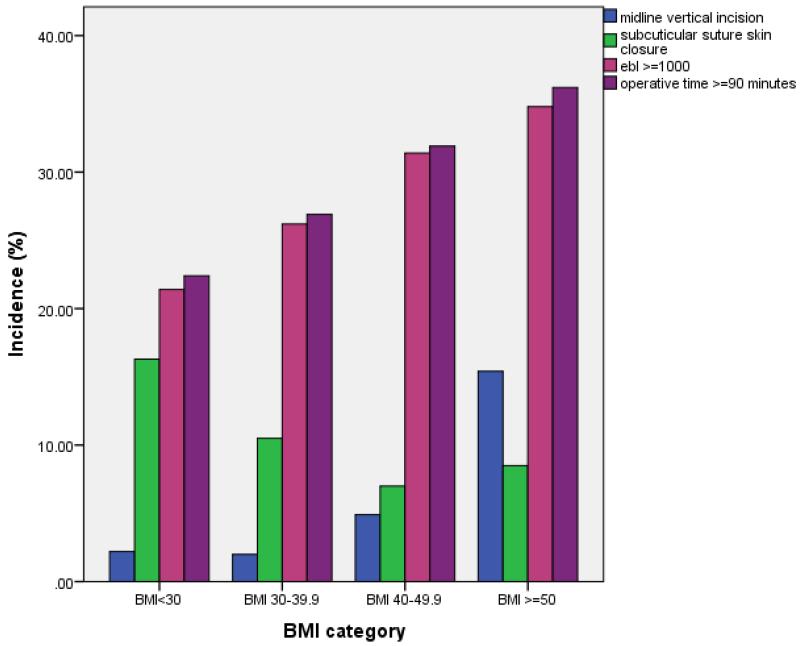
Operative characteristics of each group were compared in Table 3. Increasing BMI was associated with increased rates of midline vertical incision vs. Pfannensteil incision, longer operative time, and higher blood loss. As BMI increased, lower rates of subcuticular skin closure were observed. No difference was seen in administration of preoperative antibiotics. (Table 3 and Figure 2)
Table 3.
Operative characteristics for the four study groups, compared by BMI
| BMI<30 (n=728) |
BMI 30-39.9 (n=1087) |
BMI 40-49.9 (n=428) |
BMI ≥ 50 (n=201) |
P value | |
|---|---|---|---|---|---|
| Pre op Antibiotics (n=1943) |
77.7% | 80.9% | 80.8% | 76.6% | 0.24 |
| Midline vertical incision (n=89) |
2.2% | 2.0% | 4.9% | 15.4% | <0.01 |
| Estimated Blood Loss (mL) |
734 ± 274 | 784 ± 294 | 836 ± 333 | 861 ± 373 | <0.01 |
| Operative time (minutes) |
50 ± 22.7 | 54 ± 18.9 | 63 ± 25 | 71 ± 28 | <0.01 |
| Subcuticular Skin Closure (n=281) |
16.4% | 10.5% | 7.0% | 9.0% | <0.01 |
Figure 2.
Operative characteristics relating to increasing BMI
Discussion
We found that wound complications increase as severity of obesity increases. The most marked difference in wound complications was found in women with BMI ≥ 50 compared to non-obese women (22.9% vs. 6.6%, aOR 3.0). Women with BMI 40-49.9 were also at significantly increased risk for wound complications compared to their non-obese counterparts (16.8% vs 6.6%, aOR 2.6). There was also a higher risk of wound complications in obese women with BMI 30-39.9 compared to non-obese women, although the difference was not a statistically significant. These findings demonstrate a dose response relationship in a predominantly obese population with respect to increasing BMI and wound complications. In addition, we found significant differences is surgical characteristics related to increasing degree of obesity, specifically, higher EBL and operative time, more vertical skin incisions, and less subcuticular suture skin closure. This delineates an at risk population with some potentially modifiable factors to decrease postoperative morbidity.
Previous investigations have shown consistently that obese women are at increased risk for wound complications after cesarean, however, the risk based on degree of obesity was not quantified. 5-8 Myles et al demonstrated that obesity is an independent risk factor for infectious morbidity.6 The Myles study was a retrospective cohort study of 574 women who underwent cesarean. The primary outcome investigated was infectious morbidity, defined as endometritis, wound infection, or urinary tract infection. They found a 3.5% rate of wound infection overall. In addition to the small sample size, they did not compare obese to non-obese women at baseline, and therefore did not adequately adjust for confounding factors.
In 2010, Alanis et al focused on the massively obese patient with BMI ≥ 50, investigating risks for wound complications after cesarean.7 The cohort consisted of 195 women and demonstrated a 30% rate of wound complication. While this study was novel and included a large population of women with BMI ≥ 50, there was no control group for comparison.
Our study offers several strengths over previous studies on this subject. The cohort consisted of a predominantly obese, high risk, population with a large proportion of patients with BMI > 40 and BMI >50. Another strength of our study is the 96% follow up rate. Only 99 (4%) out of 2543 patients did not have any follow up data regarding wound complications. This is important because the majority of wound complications occur after patients have been discharged from the hospital. The detailed information available on patients in our cohort, including demographics, history, and pregnancy outcomes allowed us to adjust for potential confounders. For example, we were able to adjust for known risk factors for wound complications such as vertical incision, diabetes, and prior cesarean.9,10,13 We were also able to explore variation in surgical characteristics across BMI, which might serve as potential targets for intervention or explanation for our findings.
Despite the strengths of our study, the potential limitations must be considered as well. In our cohort, the retrospective nature did not always allow us to extract information on the type of wound complication, but rather that a wound complication occurred. Also, due to the retrospective design, information was not available on subcutaneous tissue closure in our cohort. However, the cohort consisted of patients in a single tertiary care center where the general practice is to close the subcutaneous layer with 3-0 chromic catgut if it measured 2cm or greater.14 In addition, because patients were seen in multiple different settings for follow up, standardization of the diagnostic criteria for wound complications was not performed. However, variation among diagnostic criteria between practitioners more accurately reflects daily practice, further improving our generalizability. In follow up, we were only able to obtain records for women treated in our hospital system. Therefore, women who may have been treated at other institutions for a wound complication were excluded and assumed not to have experienced a wound complication and may have been misclassified. This assumption was made in order assure this potential source of bias to be toward the null. Another consideration is that the number of women treated with pre-operative antibiotics was lower than would be anticipated in current practice, ranging from 76.6% to 80.9%. The remainder of the women in the cohort received antibiotics after cord clamp. However, administration of pre-operative antibiotics did not differ between BMI strata and therefore does not act as a confounder in our dataset. Lastly, maternal BMI at delivery was used rather than pre-pregnancy BMI, because maternal BMI at the time of delivery is most relevant to patient counseling and decision-making regarding delivery.
We found that there is a dose response with respect to increasing BMI and risk for wound complications, with the most severely obese women at greatest risk. We also found that as degree of obesity increases, differences in operative characteristics change as well. Our findings are important given the increasing rate of obesity and extreme obesity in obstetrics. Additionally, wound complications cause significant emotional and financial stress on patients and on the healthcare system as a whole. These complications can lead to increased recovery time and even re-hospitalization. Given the higher wound complications with increasing BMI, it is imperative that patients are counseled appropriately. Importantly, studies are urgently needed to identify interventions and modifications in surgical techniques to decrease the overall cesarean morbidity in this prevalent demographic in the United States.
Acknowledgements
Dr. Cahill is a Robert Wood Johnson Physician Faculty Scholar, which partially supports this work. Dr. Conner is also supported by the NICHD T32 grant (#22-3125-77026E) and the Washington University Institute of Clinical and Translational Sciences grant (#UL1TR000448).
Abbreviations
- (BMI)
Body Mass Index
- (EBL)
Estimated Blood Loss
- (aOR)
Adjusted Odds Ratio
- (CI)
Confidence Interval
- (WHO)
World Health Organization
- (ACOG)
American College of Obstetricians and Gynecologists
Footnotes
Financial disclosures: none
References
- 1.Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. NCHS data brief. 2010 Mar;(35):1–8. [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS data brief. 2012 Jan;(82):1–8. [PubMed] [Google Scholar]
- 3.Kominiarek MA, Vanveldhuisen P, Hibbard J, Landy H, Haberman S, Learman L, et al. The maternal body mass index: a strong association with delivery route. American journal of obstetrics and gynecology. 2010 Sep;203(3):264, e1–7. doi: 10.1016/j.ajog.2010.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Usha Kiran TS, Hemmadi S, Bethel J, Evans J. Outcome of pregnancy in a woman with an increased body mass index. BJOG: an international journal of obstetrics and gynaecology. 2005 Jun;112(6):768–72. doi: 10.1111/j.1471-0528.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 5.Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstetrics and gynecology. 2005 Dec;106(6):1357–64. doi: 10.1097/01.AOG.0000188387.88032.41. [DOI] [PubMed] [Google Scholar]
- 6.Myles TD, Gooch J, Santolaya J. Obesity as an independent risk factor for infectious morbidity in patients who undergo cesarean delivery. Obstetrics and gynecology. 2002 Nov;100(5 Pt 1):959–64. doi: 10.1016/s0029-7844(02)02323-2. [DOI] [PubMed] [Google Scholar]
- 7.Alanis MC, Villers MS, Law TL, Steadman EM, Robinson CJ. Complications of cesarean delivery in the massively obese parturient. American journal of obstetrics and gynecology. 2010 Sep;203(3):271, e1–7. doi: 10.1016/j.ajog.2010.06.049. [DOI] [PubMed] [Google Scholar]
- 8.Tran TS, Jamulitrat S, Chongsuvivatwong V, Geater A. Risk factors for postcesarean surgical site infection. Obstetrics and gynecology. 2000 Mar;95(3):367–71. doi: 10.1016/s0029-7844(99)00540-2. [DOI] [PubMed] [Google Scholar]
- 9.Leth RA, Uldbjerg N, Norgaard M, Moller JK, Thomsen RW. Obesity, diabetes, and the risk of infections diagnosed in hospital and post-discharge infections after cesarean section: a prospective cohort study. Acta obstetricia et gynecologica Scandinavica. 2011;90:501–9. doi: 10.1111/j.1600-0412.2011.01090.x. [DOI] [PubMed] [Google Scholar]
- 10.Thornburg LL, Linder MA, Durie DE, Walker B, Pressman EK, Glantz JC. Risk factors for wound complications in morbidly obese women undergoing primary cesarean delivery. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2012 Sep;25(9):1544–8. doi: 10.3109/14767058.2011.653422. [DOI] [PubMed] [Google Scholar]
- 11.Obesity: preventing and managing the global epidemic . Report of a WHO consultation. Vol. 894. World Health Organization; 2000. pp. i–xii.pp. 1–253. technical report series. [PubMed] [Google Scholar]
- 12.Use of Prophylactic Antibiotics in Labor and Delivery . American College of Obstetricians and Gynecologists Practice Bulletins. 2011. p. 120. [Google Scholar]
- 13.Wall PD, Deucy EE, Glantz JC, Pressman EK. Vertical skin incisions and wound complications in the obese parturient. Obstetrics and gynecology. 2003 Nov;102(5 Pt 1):952–6. doi: 10.1016/s0029-7844(03)00861-5. [DOI] [PubMed] [Google Scholar]
- 14.Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstetrics and gynecology. 2004 May;103(5 Pt 1):974–80. doi: 10.1097/01.AOG.0000124807.76451.47. [DOI] [PubMed] [Google Scholar]