Abstract
Extant research has demonstrated that compared to adults with insecure attachment styles, more securely attached parents tend to be more responsive, sensitive, and involved parents resulting in improved outcomes for their children. Less studied is the influence of a mother's attachment style on her attachment to her unborn child during pregnancy and the consequent developmental outcomes of the child during early childhood. Thus, the aim of this prospective longitudinal study was to examine the relationship between maternal-fetal attachment (MFA) during pregnancy and infant and toddler outcomes and the role of mothers’ attachment style on early childhood developmental outcomes in an economically disadvantaged sample of women and their children. Gamma regression modeling demonstrated an avoidant maternal attachment style (b = .98, 95% CI [.97, .98], p < 0.001) and post-partum depressive symptomatology (b = .97, 95% CI [.96-.99], p = .03) were significant predictors of early childhood development. Women demonstrating higher avoidant attachment styles and greater depressive symptomatology were more likely to have children demonstrating early childhood developmental delays than those women with less avoidant attachment styles and less depressive symptomatology. Furthermore, women reporting higher MFA during pregnancy had more secure attachment styles and their children had more optimal early childhood development than those women reporting lower MFA and less secure attachment styles. Findings have implications for enhancing early intervention programs aimed at improving maternal and childhood outcomes. An earlier identification of disruptions in attachment may be beneficial in tailoring interventions focused on the mother-child dyad.
Keywords: Maternal-fetal Attachment (MFA), Maternal attachment style, Postpartum depression, Early childhood development
Introduction
Maternal attachment is a biologically-driven construct, inherent within humans and other primates, designed to preserve the species through nurturing and protective behaviors (Bowlby 1982/1969; Bowlby 1978). When attachment figures do not exhibit these nurturing and protective behaviors towards their young, children's social, emotional, and cognitive development may be impaired (Ainsworth 1979; Belsky and Cassidy 1994; Bowlby 1982/1969). Moreover, attachment bonds developed in early childhood may constitute the foundation of an individual's attachment style well into adulthood, potentially affecting one's social and parenting relationships across generations (Antonucci et al. 2004; Waters et al. 2000). For these reasons, maternal attachment style, beginning as early as pregnancy, has become an area of clinical and empirical interest (McFarland et al. 2011; Siddiqui and Hagglof 2000).
In a previous study of healthy low-income women, we found that poorer maternal attachment quality to the fetus during pregnancy (e.g. maternal-fetal attachment) to be associated with a greater likelihood of giving birth to an infant with adverse neonatal outcomes (Alhusen et al. 2012). This relationship was mediated by the quality of the woman's health practices during pregnancy, with mothers reporting poorer quality of maternal-fetal attachment engaging in fewer healthy behaviors during pregnancy. Qualitative interviews with the mothers during pregnancy uncovered themes of sadness, loss, and concern for their children's futures, suggesting that maternal attachment quality during pregnancy might have long-term implications for their parenting once the child is born (Alhusen et al. 2012). The purpose of the current study is to follow a subsample of these mothers 1-2 years later to examine maternal attachment quality over time and its association with their young children's development. Our goal is to add to the emerging literature on the importance of maternal attachment style in contributing to early childhood outcomes in vulnerable women and children. An enhanced understanding of these relationships, particularly in samples of children at high risk for poor developmental outcomes is critical in informing how best to direct intervention efforts.
Classifications of adult attachment styles have been described and can be classified in adults by administering specific instruments or semi-structured interviews (see Mkiulincer and Shaver, 2007 for an overview). A secure attachment style is attributed to the availability and responsiveness of an attachment figure that provides a “secure base”, particularly in times of stress (Green et al. 2007). In contrast, an insecure attachment style will develop if attachment figures are unresponsive or inconsistently responsive, particularly in times of need (Green et al. 2007). Two major patterns of insecure maternal attachment styles have been distinguished in the literature: avoidant and anxious attachment styles (Mikulincer and Shaver 2007).
Individuals with avoidant attachment styles are considerably less comfortable in intimate relationships, and may refrain from establishing and maintaining close relationships (Simpson 1990). They may view establishing close relationships as futile, perhaps even dangerous because of the anticipated distress from failing to achieve closeness with an attachment figure (Vrticka and Vuilleumier 2012). In contrast, anxious attachment styles are noted in individuals who desire intimacy in relationships, but are fearful of rejection and thus do not trust their ability to cultivate close relationships (Green et al. 2007; Simpson et al. 1996).
Attachment research conducted among vulnerable samples has demonstrated that poverty and its accompanying stressors may increase an individual's risk of developing an insecure attachment style (Allen et al. 2004; Cozzarelli et al. 2003; Davila et al. 1997; Diener et al. 2003). Bowlby (1973, 1980) described the attachment system as relatively stable, but when confronted with significant stressors, individuals may display less stable and secure working models of relationships over time. For example, urban poverty and its related stressors (i.e., exposure to neighborhood crime and violence, housing instability, transient and untrustworthy neighbors, unresponsive landlords, lack of employment opportunities) can breed fear and mistrust and undermine one's ability to develop and maintain secure attachments (Candelaria et al. 2011; Stansfeld et al. 2008). Over multiple generations, persistent exposures to these environmental threats could lead to chronic hypervigilance, parental depression, and the expectation that self-sufficiency is the key to survival, qualities that could dampen parents’ abilities to nurture and support their young children's development (Caughy et al. 2003; Gershoff et al. 2007; Vernon-Feagans et al. 2012).
The current study explores the associations among maternal-fetal attachment (MFA), maternal depression, maternal attachment style, and early childhood developmental outcomes in an urban sample of low-income mothers originally assessed during pregnancy. Our goal is to examine the extended impact of poor attachment quality during pregnancy on young children's development. Of particular importance is whether poor MFA is indicative of an overall attachment style that makes it difficult for mothers to engage in close, intimate relationships with others, including their child, beginning in pregnancy and through the child's earliest years.
We hypothesized that women with an insecure attachment style as assessed when their children are 1-2 years old would a) have had lower MFA during pregnancy, and b) higher depressive symptomatology in the post-partum period. Furthermore, we hypothesized that after controlling for adverse neonatal outcomes and perinatal depressive symptomatology, mothers classified as more anxious or avoidant in their attachment style would have children with greater developmental delays than those women with more secure attachment styles.
Methods
Participants
The current study was conducted among a convenience sample of English-speaking women who previously participated in a larger study examining the association between MFA and neonatal outcomes during their pregnancies between 2010 and 2011. Mailings were sent to all participants (n=166) regarding the current study and participants were given the option to optout of further contact. No participants opted out of further contact; however, we were unable to locate nineteen (11.4%) women. After describing the purpose of the follow-up study, eight women (4.6%) declined further study participation largely due to difficulty in scheduling around employment and school responsibilities. Recruitment for the current study occurred from December 2011 until August 2012. Mothers who consented to the current study were required to reside with the child that participated in the original study.
Procedures
The study protocol and informed consent received institutional review board approval from the Johns Hopkins Medical Institutions. After a complete description of the current study, informed consent was obtained. Women were interviewed in their homes with their child present. The women completed measures related to their attachment style, and post-partum depressive symptomatology, described below, that were read aloud by the first author. Immediately following completion of the questionnaires, a developmental assessment was conducted on the child. The interviews and developmental assessment lasted approximately 60 minutes and participants were compensated $25 for their participation. Upon completion of study measures, all women were given the opportunity to discuss any concerns regarding their child's development with the first author. Women were also provided with a list of resources to assist in obtaining additional information or referrals for their child.
Measures
Maternal variables of interest in this study include maternal depressive symptomatolgy, maternal-fetal attachment and maternal attachment style. Child variables of interest include neonatal outcomes and early childhood development. Table 1 outlines the study measures used, and the time points each measure was collected.
Table 1.
Study measures and time point of data collection
| Pregnancy (24-28 wks. gestation) | Neonatal period | Early childhood (14 months - 26 months) | |
|---|---|---|---|
| Maternal-Fetal Attachment Scale (MFAS) | x | ||
| Birthweight, gestational age | x | ||
| Edinburgh Postnatal Depression Scale (EPDS) | x | ||
| Attachment Style Questionnaire | x | ||
| Ages and Stages, Third Edition (ASQ-3) | x |
Maternal measures collected during pregnancy
The Maternal-Fetal Attachment Scale (MFAS) is a 24 item self-report measure intended to measure the extent to which pregnant women engage in behaviors indicative of an emotional connection and interaction with their unborn child. The response format is a five-point Likert-type items with options ranging from 1 (definitely no) to 5 (definitely yes). The total scale score ranges from 24-120 with higher scores indicative of more optimal MFA. Examples of statements included on the MFAS include “I talk to my unborn baby” and “I stroke my tummy to quiet the baby when there is too much kicking.” The MFAS is a widely used measure of MFA across diverse populations, including samples of young, low-income mothers (Ahern and Ruland 2003; Hart and McMahon 2006; Lindgren, 2001; Shieh and Kravitz 2006; Zachariah, 2004) with reliability for the overall instrument reported to be .85 (Cranley 1981) and noted to be .88 in the current study. The MFAS was administered during pregnancy when the woman was between 24-28 weeks gestation.
Neonatal measures
Neonatal birth weight and gestational age were extracted from the electronic chart within 48 hours of delivery to assess for the presence of an adverse outcome. A neonate was classified as having an adverse outcome in the presence of low birth weight (e.g. the neonate weighed <2500 grams), preterm birth (e.g. the neonate was born at <37 completed weeks of gestation) or small for gestational age (e.g. the neonate was classified as <10th percentile birthweight adjusted for gestational age). Intrauterine growth was then calculated by relating neonatal birthweight to the gestational age at birth against reference curves. We used comprehensive reference values of birth weight based on a national sample of over 6 million infants (Oken et al. 2003). Neonatal outcome received a binary rating of 1 (one or more adverse outcomes) or 0 (no adverse outcomes).
Maternal measures collected in the post-partum period
The Edinburgh Postnatal Depression Scale (EPDS) is a widely used self-report measure to assess for depressive symptoms, particularly during the perinatal period (Cox et al. 1987). The scale consists of 10 items and asks women to respond to each statement based on their mood over the previous 7 days. Each item is scored from 0 to 3 with a maximum score of 30. A higher EPDS score represents an increased risk of depressive symptomatology, and this study used the widely recommended cut-off score of >12 as indicative of clinically significant depressive symptoms. A sensitivity rate of 82% with a specificity of 95% has been previously demonstrated with this chosen cut-off in a similar participant population (Tandon et al. 2012). Examples of items from the EPDS include “I have looked forward with enjoyment to things” and “I have blamed myself unnecessarily when things went wrong”. The Cronbach's α for the current study was .91.
Attachment style was measured using the Attachment Style Questionnaire, a 40-item self-report measure rated on a scale of 1 (totally disagree) to 6 (totally agree) (Feeney et al. 1994). Items include, “I find it hard to trust people” and “I worry that others won't care about me as much as I care about them.” Scores from the Attachment Style Questionnaire have been linked in theoretically predicted ways to maternal depression, and stress (Feeney and Collins 2003; Meredith et al. 2006; Shurman and Rodriguez, 2006). In this study, the Attachment Style Questionnaire was selected as it was designed to tap general (as opposed to romantic) attachment security and because it has good psychometric properties, including internal consistency (α coefficients ranging from .76 to .80) and test re-test reliability over a 10 week period ranging from .67 to .74(Feeney et al. 1994). The Cronbach's α for the current study was .85.
Early childhood development
The Ages and Stages Questionnaire, Third Edition (ASQ-3), is composed of a series of 21 age-specific questionnaires starting at one month and ending at five and one half years of age (Squires et al. 1997). Five developmental domains are evaluated (i.e., communication, gross motor, fine motor, problem solving, and personal-social), and each domain is comprised of six items to evaluate developmental milestones in each area. In this study, mothers evaluated whether the child had achieved a milestone (yes), had partly achieved the milestone (sometimes), or had not yet achieved the milestone (no). The ASQ-3 is one of the most extensively evaluated parent-completed tools, and has good psychometric properties with an overall specificity of 86 percent, and an average sensitivity of 85 percent (Mackrides and Ryherd, 2011). In this study, the ASQ-3 was administered in the child's home when the child was between 14 months and 26 months of age.
Data analysis
Data were analyzed using IBM SPSS Version 19 and SAS. Data analysis began with descriptive and exploratory statistical analyses. Study variables were examined to assess distributions, identify outlying or extreme observations, and determine the need for transformation. . The early childhood development outcome, measured by the ASQ-3, was highly skewed and modeled using a generalized linear model with a gamma distribution and log link, also known as gamma regression. This method was chosen because it provides robust estimators in the absence of normality. Model selection was based on statistical significance and use of Akaike's Information Criterion (AIC). There were no missing data.
Results
Based on the size of the association between MFA and neonatal outcomes obtained in the original study (r = -0.52), with 80% power and a level of significance of 0.05, a sample size of at least 34 would be needed. Of the 147 mothers located from the original study, 81 (55%) participated in the current study. The demographic characteristics of the original study sample (n=166) and current study sample (n=81) are outlined in Table 2. Overall, the study sample consisted of low-income, predominantly African American younger women. Women participating in the current study did not differ significantly on key demographic variables (e.g. age, race, income, MFAS scores, adverse neonatal outcomes, depressive symptomatology) from those women who participated in the original study including those women who we were unable to locate or those who declined further participation.
Table 2.
Socio-demographic characteristics of original and current study sample
| Demographic | Original Sample (n=166) n (%) | Follow-up Sample (n=81) n (%) | p-value |
|---|---|---|---|
| Age (mean/SD) | 23.30 (5.7) | 23.04 (5.1) | 0.12* |
| Race | |||
| African American | 155 (93) | 75 (93) | 0.44+ |
| White non-Hispanic | 9 (5) | 6 (7) | |
| Other | 2 (2) | ||
| Education | |||
| Less than High School | 110 (67) | 55 (68) | 0.12+ |
| High School Graduate/GED | 45 (27) | 21 (26) | |
| Some College/Trade School | 5 (3) | 3 (4) | |
| College/Trade School Graduate | 6 (3) | 2 (2) | |
| Marital Status | |||
| Single | 90 (54) | 47 (58) | 0.13+ |
| Partnered/Married | 73(44) | 31 (38) | |
| Other | 3 (2) | 3 (4) | |
| Employment Status | |||
| Unemployed | 127(77) | 60 (74) | 0.68+ |
| Employed Full Time | 25 (15) | 12 (15) | |
| Employed Part Time | 14 (8) | 9 (11) | |
| Total Annual Household Income | |||
| Under $10,000 | 76 (46) | 38 (47) | 0.95+ |
| $10,001-$20,000 | 66 (40) | 32 (40) | |
| >$20,001 | 24 (14) | 11 (13) |
T-test
Fisher's exact test
Bivariate and point biserial correlations among the main study variables are presented in Table 3. As hypothesized, an avoidant maternal attachment style was highly correlated with lower MFA (ES = -.62) and higher post-partum depressive symptomatology (ES = .85). Similarly, an anxious maternal attachment style was highly correlated with lower MFA (ES = -.53) and higher post-partum depressive symptomatology (ES = .54).
Table 3.
Correlations among the main study variables (n = 81)
| Variable | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|
| 1. MFA | -.62* | -.53* | -.61* | -.54* | .59* |
| 2. Avoidant Attachment Style | - | .71* | .85* | .35* | -.84* |
| 3. Anxious Attachment Style | - | .54* | .37* | -.64* | |
| 4. PPD Symptomatology | - | .39* | -.82* | ||
| 5. Adverse Neonatal Outcomea | - | -.51* | |||
| 6. Early Childhood Development | - |
p < .05
Referent group was no adverse outcome
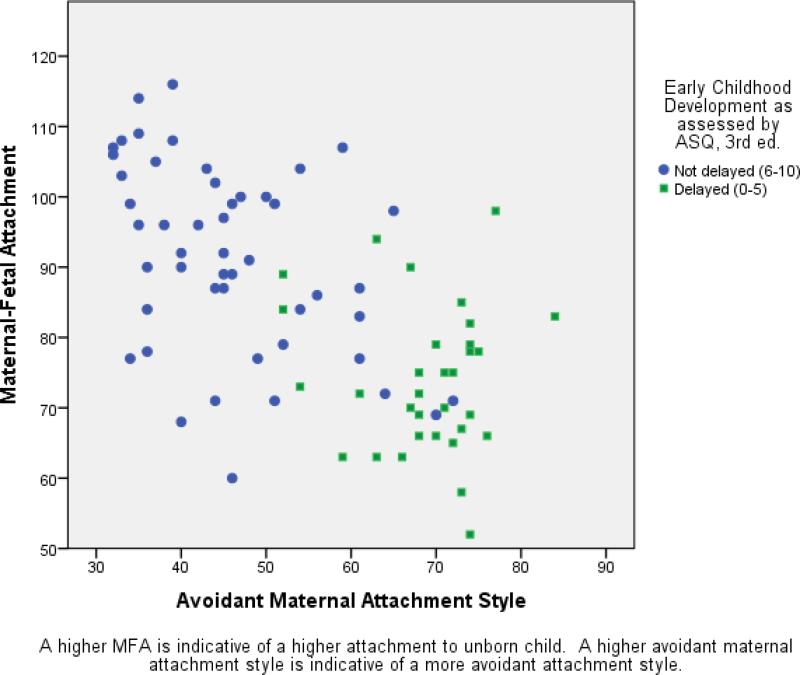
A series of regression analyses were conducted to examine predictors of early childhood development. In univariate analyses, after controlling for an adverse neonatal outcome, MFA was a significant predictor of early childhood development (b = .59, 95% CI [0.08, 0.16], p < 0.001). Specifically, women reporting lower MFA were more likely to have children demonstrating early childhood developmental delays than those women reporting higher MFA. Similarly, the individual predictors of an avoidant attachment style (b = -0.84, 95% CI [-0.20, -0.15], p < 0.001), an anxious attachment style (b = -0.64, 95% CI [-0.23, -0.13], p < 0.001), and the presence of post-partum depressive symptomatology (b = -0.82, 95% CI [-0.49, -0.29], p < 0.001) were all significant predictors of early childhood development . Women reporting increased attachment avoidance, increased attachment anxiety or post-partum depressive symptomatology were more likely to have children demonstrating early childhood developmental delays than women with more secure attachment styles and less depressive symptomatology. However, after accounting for an avoidant attachment style and post-partum depressive symptoms, MFA and an anxious maternal attachment style were no longer significant predictors of early childhood development. Figure 1 depicts the relationship between MFA and an avoidant maternal attachment style, by levels of overall early childhood development dichotomized at the mean score of the study sample. Those children not meeting the age-appropriate milestones in one or more of the developmental domains were classified as delayed (ASQ scores 0-5) and those children demonstrating milestone attainment, at least sometimes in the five developmental domains assessed, were classified as passing (ASQ scores 6-10). As shown in Figure 1, higher MFA was associated with less avoidant attachment style as well as more optimal early childhood development.
Figure 1.
Scatterplot of early childhood developmental classification for maternal avoidant attachment style by maternal-fetal attachment
The results of the gamma regression modeling for predicting early childhood development are demonstrated in Table 4. In the final model, after controlling for marital status, education, income, and an adverse neonatal outcome, an avoidant attachment style (b = .98, 95% CI [.97, .98], p < 0.001) and post-partum depressive symptomatology (b = .97, 95% CI [.96-.99], p = .03) were significant predictors of early childhood development. Women demonstrating higher avoidant attachment styles and greater depressive symptomatology were more likely to have children demonstrating early childhood developmental delays than those women with less avoidant attachment styles and less depressive symptomatology.
Table 4.
| Adjusted Coefficientc | 95% Confidence Interval | p-value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Avoidant Attachment | 0.9800 | 0.9705 | 0.9897 | <0.0001 |
| Post-partum Depression | 0.9798 | 0.9611 | 0.9988 | 0.0375 |
Generalized linear model with gamma distribution and log link function
AIC=352.1
Adjusted for marital status, education, income, adverse neonatal outcome
Discussion
To our knowledge, this study is the first to examine the relationships among MFA, maternal attachment style, and early childhood development. Our findings suggest that an insecure maternal attachment style, particularly an avoidant attachment style, is related to significantly lower levels of MFA during pregnancy. There is some discussion in the literature on whether MFA accurately reflects an “attachment” as opposed to a “relationship” (Van den Bergh and Simons 2009) or the foundation of a “caregiving system” (Walsh 2010). In our sample, the high correlations between MFA and maternal attachment style suggest that MFA may in fact be part of a larger attachment construct. MFA captures the nature of a mother's connection to her unborn child, and the subsequent behavioral manifestations of this connection (McFarland et al. 2011) that are largely indicative of a desire to protect the unborn child.
Several studies have found an association between depressive symptoms during pregnancy and lower MFA (Alhusen et al. 2012; Brandon et al. 2008; McFarland et al. 2011). Depression during pregnancy may lead to lower MFA by compromising a woman's ability to feel confident in her new role as an expectant mother. A hallmark symptom of depression is disturbances in seeking or maintaining social relationships across a variety of relationships (Overbeek et al. 2006); thus, the negative sequelae may very well impact the maternal-fetal bond. In our study, the presence of post-partum depressive symptomatology was related to lower MFA during pregnancy. This is not surprising given that depression during pregnancy is the strongest predictor of post-partum depression (Toohey, 2012), underscoring the importance of assessing a woman's mental health during pregnancy (National Research Council, 2009).
An insecure maternal attachment style was significantly associated with post-partum depressive symptomatology. Previous research supports a relationship between insecure attachment styles and depression, though few studies have examined maternal attachment style during the post-partum period (Bifulco et al. 2002; Gerlsma and Luteijn 2000). This time point is critical as extant research largely supports the adverse effects of maternal depressive symptoms on sensitive parenting and subsequent quality of attachments formed between mothers and children (Diener et al. 2003; Goodman and Gotlib, 2002; Lyons-Ryth et al. 2002; Mills-Koonce et al. 2008). Furthermore, recent research supports the influence of maternal attachment style, and maternal depressive symptoms on the ability to benefit from early intervention programs aimed at improving parent-child interaction (Berlin et al. 2011; Duggan et al. 2009; Heinicke et al. 2006). Mothers whose attachment styles make it difficult to connect with their unborn child may also have difficulty connecting with an interventionist charged with engaging the mother in a working alliance (Duggan et al. 2009). That is, mothers with avoidant attachments may be more resistant to forming trusting relationships with health care providers, and may be less receptive to provider efforts to educate and promote optimal childhood development (Berlin et al. 2011). Low-income mothers, similar to those who participated in this study, are particularly likely to be targeted in support-based interventions and yet maternal attachment style remains understudied in terms of how these attachment processes may influence intervention outcomes (Crittenden and Claussen, 2000; Green et al. 2007). Thus, further research on how attachment processes may influence targeted parent and child outcomes in vulnerable families is vital, particularly to inform program approach.
This study provides compelling evidence of the important relationships among MFA, maternal attachment style, post-partum depressive symptomatology, and early childhood developmental outcomes in a sample of low-income, predominantly African-American women and children. Historically, much of the focus on maternal mental health and poor childhood outcomes has centered on postpartum depression. Our results suggest that an earlier assessment of maternal psychological well-being during pregnancy, including an assessment of maternal attachment style, may be more cost-effective for identifying high risk mothers and initiating interventions to prevent adverse neonatal and developmental outcomes. Home visiting programs initiated prenatally, such as the Nurse-Family Partnership, have demonstrated enduring effects on reducing poverty, and improving children's health and development (Kitzman et al. 1997; Olds et al. 2002; Olds et al. 2010). Other programs that center on building secure mother-baby attachments beginning in pregnancy, such as the “Minding the Baby” program, also hold promise for improving maternal-child outcomes. In both interventions, significant focus is given to establishing a relationship between home visitors and the mother as well as other family members (Sadler et al. 2006). The development of a trusting relationship between the home visiting nurse and the first-time mother is fundamental to building mothers’ self-efficacy to support and protect their children. Addressing maternal psychological well-being may constitute one of the most amendable and feasible prevention strategies for decreasing risk factors for early childhood developmental delays (Kingston et al. 2012).
There are two important limitations of this study. First, the results are based on a convenience sample which limits generalizability to other populations. Second, this longitudinal study used a cross-sectional design, limiting inferences of causality.
Future research is needed to strengthen and extend the current findings by examining additional sources of environment risk (e.g. home and neighborhood characteristics) to strengthen our understanding of how context influences maternal attachment and experimental studies to evaluate the impact of preventive interventions initiated in pregnancy on multiple indicators of attachment quality and child outcomes.
Acknowledgments
Funding sources:
This research was supported by the National Institute of Nursing Research (F31 NR010957), and the National Center for Research Resources (5KL2RR025006), a component of the NIH Roadmap for Medical Research.
Footnotes
Conflicts of Interest:
The authors declare no conflicts of interest.
References
- Ahern NR, Ruland JP. Maternal-fetal attachment in African-American and Hispanic-American women. The Journal of Perinatal Education. 2003;12:27–35. doi: 10.1624/105812403X107044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth MD. Infant--mother attachment. The American Psychologist. 1979;34:932–937. doi: 10.1037//0003-066x.34.10.932. [DOI] [PubMed] [Google Scholar]
- Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN / NAACOG. 2012;41:E71–81. doi: 10.1111/j.1552-6909.2012.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhusen JL, Gross D, Hayat MJ, Woods AB, Sharps PW. The influence of maternal-fetal attachment and health practices on neonatal outcomes in low-income, urban women. Research in Nursing & Health. 2012;35:112–120. doi: 10.1002/nur.21464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP, McElhaney KB, Kuperminc GP, Jodl KM. Stability and change in attachment security across adolescence. Child Development. 2004;75:1792–1805. doi: 10.1111/j.1467-8624.2004.00817.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonucci TC, Akiyama H, Takahashi K. Attachment and close relationships across the life span. Attachment & Human Development. 2004;6:353–370. doi: 10.1080/1461673042000303136. [DOI] [PubMed] [Google Scholar]
- Belsky J, Cassidy J. Attachment: Theory and evidence. In: Rutter M, Hay D, editors. Development through life: A handbook for clinicians. Blackwell; Oxford: 1994. pp. 373–402. [Google Scholar]
- Berlin LJ, Whiteside-Mansell L, Roggman LA, Green BL, Robinson J, Spieker S. Testing maternal depression and attachment style as moderators of early head start's effects on parenting. Attachment & Human Development. 2011;13:49–67. doi: 10.1080/14616734.2010.488122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bifulco A, Moran PM, Ball C, Bernazzani O. Adult attachment style. I: Its relationship to clinical depression. Social Psychiatry and Psychiatric Epidemiology. 2002;37:50–59. doi: 10.1007/s127-002-8215-0. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Volume 1. Attachment. 2nd ed. Basic Books; New York: 1982/1969. [Google Scholar]
- Bowlby J. Attachment theory and its therapeutic implications. Adolescent Psychiatry. 1978;6:5–33. [PubMed] [Google Scholar]
- Brandon AR, Trivedi MH, Hynan LS, Miltenberger PD, Labat DB, Rifkin JB, Stringer CA. Prenatal depression in women hospitalized for obstetric risk. The Journal of Clinical Psychiatry. 2008;69:635–643. doi: 10.4088/jcp.v69n0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candelaria M, Teti DM, Black MM. Multi-risk infants: Predicting attachment security from sociodemographic, psychosocial, and health risk among African-American preterm infants. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2011;52:870–877. doi: 10.1111/j.1469-7610.2011.02361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caughy MO, O'Campo PJ, Muntaner C. When being alone might be better: Neighborhood poverty, social capital, and child mental health. Social Science & Medicine. 2003;57:227–237. doi: 10.1016/s0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- Cox J, Holden J, Sagovsky R. Detection of postnatal depression- development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry. 1987;150:82–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Cozzarelli C, Karafa JA, Collins NL, Tagler MJ. Stability and change in adult attachment styles: Associations with personal vulnerabilities, life events, and global constructs of self and others. Journal of Social and Clinical Psychology. 2003;22:315–346. [Google Scholar]
- Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nursing Research. 1981;30:281–284. [PubMed] [Google Scholar]
- Crittenden PM, Claussen A. The organization of attachment relationships: Maturation, culture, and context. Cambridge University Press; New York: 2000. [Google Scholar]
- Davila J, Burge D, Hammen C. Why does attachment style change? Journal of Personality and Social Psychology. 1997;73:826–838. doi: 10.1037//0022-3514.73.4.826. [DOI] [PubMed] [Google Scholar]
- Diener ML, Nievar MA, Wright C. Attachment security among mothers and their young children living in poverty: Associations with maternal, child, and contextual characteristics. Merrill-Palmer Quarterly. 2003;49:154–182. [Google Scholar]
- Duggan AK, Berlin LJ, Cassidy J, Burrell L, Tandon SD. Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at-risk mothers and infants. Journal of Consulting and Clinical Psychology. 2009;77:788–799. doi: 10.1037/a0015709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney JA, Noller P, Hanrahan M. Assessing adult attachment. In: Sperling MB, Berman WH, editors. Attachment in adults. Guilford; New York: 1994. pp. 128–151. [Google Scholar]
- Feeney BC, Collins NL. Motivations for caregiving in adult intimate relationships: Influences on caregiving behavior and relationship functioning. Personality & Social Psychology Bulletin. 2003;29:950–968. doi: 10.1177/0146167203252807. [DOI] [PubMed] [Google Scholar]
- Gerlsma C, Luteijn F. Attachment style in the context of clinical and health psychology: A proposal for the assessment of valence, incongruence, and accessibility of attachment representations in various working models. The British Journal of Medical Psychology. 2000;73:15–34. doi: 10.1348/000711200160273. [DOI] [PubMed] [Google Scholar]
- Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: Incorporating material hardship into models of income associations with parenting and child development. Child Development. 2007;78:70–95. doi: 10.1111/j.1467-8624.2007.00986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychological Association; Washington, DC: 2002. [Google Scholar]
- Green BL, Furrer C, McAllister C. How do relationships support parenting? Effects of attachment style and social support on parenting behavior in an at-risk population. American Journal of Community Psychology. 2007;40:96–108. doi: 10.1007/s10464-007-9127-y. [DOI] [PubMed] [Google Scholar]
- Hart R, McMahon CA. Mood state and psychological adjustment to pregnancy. Archives of Women's Mental Health. 2006;9:329–337. doi: 10.1007/s00737-006-0141-0. [DOI] [PubMed] [Google Scholar]
- Heinicke CM, Goorsky M, Levine M, Ponce VA, Ruth G, Silverman M, Sotelo C. Pre and postnatal antecedents of a home visiting intervention and family developmental outcome. Infant Mental Health Journal. 2006;27:91–119. doi: 10.1002/imhj.20082. [DOI] [PubMed] [Google Scholar]
- Kemp VH, Sibley DE, Pond EF. A comparison of adolescent and adult mothers on factors affecting maternal role attainment. Maternal-Child Nursing Journal. 1990;19:63–75. [PubMed] [Google Scholar]
- Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry and Human Development. 2012;43:683–714. doi: 10.1007/s10578-012-0291-4. [DOI] [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, McConnochie KM, Sidora K, Luckey DW, Shaver D, Engelhardt K, James D, Barnard K. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA : The Journal of the American Medical Association. 1997;278:644–652. [PubMed] [Google Scholar]
- Koniak-Griffin D. The relationship between social support, self-esteem, and maternal-fetal attachment in adolescents. Research in Nursing and Health. 1988;11:269–278. doi: 10.1002/nur.4770110408. [DOI] [PubMed] [Google Scholar]
- Lewis MW. Relationship of prior custody loss to maternal-fetal bonding in a subsequent pregnancy. Children and Youth Services Review. 2006;28:1169–1180. [Google Scholar]
- Lindgren K. Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Research in Nursing and Health. 2001;24:203–217. doi: 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- Lindgren K. A comparison of pregnancy health practices of women in inner-city and small urban communities. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2003;32:313–321. doi: 10.1177/0884217503253442. [DOI] [PubMed] [Google Scholar]
- Lyons-Ryth K, Lyubchik A, Wolfe R, Bronfman E. Parental depression and child attachment: Hostile and helpless profiles of parent and child behavior among families at risk. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychological Association; Washington, DC: 2002. pp. 89–120. [Google Scholar]
- Mackrides PS, Ryherd SJ. Screening for developmental delay. American Family Physician. 2011;84:544–549. [PubMed] [Google Scholar]
- McFarland J, Salisbury AL, Battle CL, Hawes K, Halloran K, Lester BM. Major depressive disorder during pregnancy and emotional attachment to the fetus. Archives of Women's Mental Health. 2011;14:425–434. doi: 10.1007/s00737-011-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith PJ, Strong J, Feeney JA. The relationship of adult attachment to emotion, catastrophizing, control, threshold and tolerance, in experimentally-induced pain. Pain. 2006;120:44–52. doi: 10.1016/j.pain.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. Attachment, group-related processes, and psychotherapy. International Journal of Group Psychotherapy. 2007;57:233–245. doi: 10.1521/ijgp.2007.57.2.233. [DOI] [PubMed] [Google Scholar]
- Mills-Koonce WR, Gariepy JL, Sutton K, Cox MJ. Changes in maternal sensitivity across the first three years: Are mothers from different attachment dyads differentially influenced by depressive symptomatology? Attachment & Human Development. 2008;10:299–317. doi: 10.1080/14616730802113612. [DOI] [PubMed] [Google Scholar]
- National Research Council . Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Kitzman HJ, Cole RE, Hanks CA, Arcoleo KJ, Anson EA, Luckey DW, Knudtson MD, Henerson CR, Jr, Bondy J, Stevenson AJ. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: Follow-up of a randomized trial among children at age 12 years. Archives of Pediatrics & Adolescent Medicine. 2010;164:419–424. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR, Jr, Ng RK, Sheff KL, Korfmacher J, Hiatt S, Talmi A. Home visiting by paraprofessionals and by nurses: A randomized, controlled trial. Pediatrics. 2002;110:486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Overbeek G, Vollebergh W, de Graaf R, Scholte R, de Kemp R, Engels R. Longitudinal associations of marital quality and marital dissolution with the incidence of DSM-III-R disorders. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2006;20:284–291. doi: 10.1037/0893-3200.20.2.284. [DOI] [PubMed] [Google Scholar]
- Sadler LS, Slade A, Mayes L. Minding the baby: A mentalization-based parenting program. In: Allen J, Fonagy P, editors. The handbook of mentalization-based treatment. Johns Wiley & Sons; Hoboken, NJ: 2006. pp. 271–288. [Google Scholar]
- Shieh C, Kravitz M. Maternal-fetal attachment in pregnant women who use illicit drugs. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2002;31:156–164. [PubMed] [Google Scholar]
- Shieh C, Kravitz M. Severity of drug use, initiation of prenatal care, and maternal-fetal attachment in pregnant marijuana and Cocaine/Heroine users. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2006;35:499–508. doi: 10.1111/j.1552-6909.2006.00063.x. [DOI] [PubMed] [Google Scholar]
- Shurman LA, Rodriguez CM. Cognitive-affective predictors of women's readiness to end domestic violence relationships. Journal of Interpersonal Violence. 2006;21:1417–1439. doi: 10.1177/0886260506292993. [DOI] [PubMed] [Google Scholar]
- Siddiqui A, Hagglof B. Does maternal prenatal attachment predict postnatal mother-infant interaction? Early Human Development. 2000;59:13–25. doi: 10.1016/s0378-3782(00)00076-1. [DOI] [PubMed] [Google Scholar]
- Simpson JA. The influence of attachment styles on romantic relationships. Journal of Personality and Social Psychology. 1990;59:273–280. [Google Scholar]
- Simpson JA, Rholes WS, Phillips D. Conflict in close relationships: An attachment perspective. Journal of Personality and Social Psychology. 1996;71:899–914. doi: 10.1037//0022-3514.71.5.899. [DOI] [PubMed] [Google Scholar]
- Squires J, Bricker D, Potter L. Revision of a parent-completed development screening tool: Ages and stages questionnaires. Pediatric Psychology. 1997;22:313–328. doi: 10.1093/jpepsy/22.3.313. [DOI] [PubMed] [Google Scholar]
- Stansfeld S, Head J, Bartley M, Fonagy P. Social position, early deprivation and the development of attachment. Social Psychiatry and Psychiatric Epidemiology. 2008;43:516–526. doi: 10.1007/s00127-008-0330-4. [DOI] [PubMed] [Google Scholar]
- Tandon SD, Cluxton-Keller F, Leis J, Le HN, Perry DF. A comparison of three screening tools to identify perinatal depression among low-income African American women. Journal of Affective Disorders. 2012;136:155–162. doi: 10.1016/j.jad.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toohey J. Depression during pregnancy and postpartum. Clinical Obstetrics and Gynecology. 2012;55:788–797. doi: 10.1097/GRF.0b013e318253b2b4. [DOI] [PubMed] [Google Scholar]
- Van den Bergh BRH, Simons A. A review of scales to measure the mother-foetus relationship. Journal of Reproductive and Infant Psychology. 2009;27:114–126. [Google Scholar]
- Vernon-Feagans L, Garrett-Peters P, Willoughby M, Mills-Koonce R, The Family Life Project Key Investigators Chaos, poverty, and parenting: Predictors of early language development. Early Childhood Research Quarterly. 2012;27:339–351. doi: 10.1016/j.ecresq.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrticka P, Vuilleumier P. Neuroscience of human social interactions and adult attachment style. Frontiers in Human Neuroscience. 2012;6:212. doi: 10.3389/fnhum.2012.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh J. Definitions matter: If maternal-fetal relationships are not attachment, what are they? Archives of Women's Mental Health. 2010;13:449–451. doi: 10.1007/s00737-010-0152-8. [DOI] [PubMed] [Google Scholar]
- Waters E, Merrick S, Treboux D, Crowell J, Albersheim L. Attachment security in infancy and early adulthood: A twenty-year longitudinal study. Child Development. 2000;71:684–689. doi: 10.1111/1467-8624.00176. [DOI] [PubMed] [Google Scholar]
- Wayland J, Tate S. Maternal-infant attachment and perceived relationships with important others in adolescents. Birth. 1993;20:198–203. doi: 10.1111/j.1523-536x.1993.tb00227.x. [DOI] [PubMed] [Google Scholar]
- Wilson ME, White MA, Cobb B, Curry R, Greene D, Popovich D. Family dynamics, parental-fetal attachment and infant temperament. Journal of Advanced Nursing. 2000;31:204–210. doi: 10.1046/j.1365-2648.2000.01245.x. [DOI] [PubMed] [Google Scholar]
- Zachariah R. Attachment, social support, life stress, and psychological well-being in pregnant low-income women: A pilot study. Clinical Excellence for Nurse Practitioners. 2004;8:60–67. [Google Scholar]