Abstract
Caring for young people with first-episode psychosis (FEP) is challenging and can adversely affect carer well-being, with limited evidence-based support materials available. We aimed to examine whether completion of a self-directed problem-solving bibliotherapy among carers of young people with FEP led to a better experience of caring, less distress and expressed emotion, and better general health than carers who only received treatment as usual (TAU). A randomized controlled trial was conducted across two early-intervention psychosis services in Melbourne, Australia. A total of 124 carers were randomized to problem-solving bibliotherapy intervention (PSBI) or TAU and assessed at baseline, 6-week and 16-week follow-up. Intent-to-treat analyses were carried out and indicated that recipients of PSBI had a more favorable experience of caring than those receiving TAU, and these effects were sustained at both follow-up time points. Across the other measures, both groups demonstrated improvements by week 16, although the PBSI group tended to improve earlier. The PSBI group experienced a greater reduction in negative emotional evaluations of the need to provide additional support to young people with FEP than the TAU group by week 6, while the level of psychological distress decreased at a greater rate from baseline to 6 weeks in the PSBI compared with the TAU group. These findings support the use of problem-solving bibliotherapy for first-time carers, particularly as a cost-effective adjunct to TAU.
Key words: burden, experience of caregiving, expressed emotion, problem-solving, self-help
Introduction
First-time caring for a young person with first-episode psychosis (FEP) is difficult, demanding, and frequently prolonged, and the carer can be confronted by varying levels of physical, emotional, and financial hardship.1,2 This in turn can adversely impact on carers’ experience of caring,2 psychological distress,3 general well-being,2 and expressed emotion,4–6 with the latter being associated with greater rates of relapse and nonrecovery1,7 in young people with FEP.
Numerous studies have reported on outcomes for families with schizophrenia.8–10 While several intervention studies in early psychosis have included family treatments as one component of a larger program of specialist care, it is not possible to ascertain their specific contribution to treatment outcomes.11 Nonetheless, many have been associated with positive effects (eg, Grawe, Falloon, Widen, and Skogvoll12). Gleeson et al.13 conducted the only published randomized controlled trial (RCT) that included a family intervention specifically developed for families receiving treatment in a specialist FEP service. The comprehensive, 7-month intervention arm included individual therapy for the young person in addition to separate cognitive behavior therapy (CBT) sessions for families. Perceived stress related to caregiving significantly improved in the intervention group compared with gold standard specialist treatment.13 While few other studies have been conducted, Addington et al.14 reported that a specialist FEP family program is highly acceptable to carers and is associated with a significant reduction in carer distress. Despite their promise, some approaches are costly and resource intensive, limiting their reach and penetration, while others are difficult to access.
An alternative, cost-effective, less therapist-intensive approach to helping carers is to use bibliotherapy (ie, self-help therapy in book form).15–17 Bibliotherapy can be carried out by carers more or less independent of health care professionals17,18 although the approach seems to work best when used in association with other therapeutic approaches.15 It is readily accessible and gives the reader the opportunity to re-read material at a later date and minimizes travel to attend therapy.18 Nevertheless, most bibliotherapy studies with a mental health focus have concentrated on people with depression and anxiety, and not on carers.
The cognitive model of caregiving predicts that negative “internal” attributions made by carers regarding the behavior of a relative diagnosed with psychosis lead to greater likelihood of criticism—one component of expressed emotion which has been shown to predict psychotic relapse.1 Psychoeducation is an important strategy for increasing the flexibility of carer attributions; therefore, bibliotherapy should reduce expressed emotion reported by carers.
In this study, we aimed to evaluate if carers of young people with FEP who completed a problem-solving bibliotherapy intervention (PSBI) reported a better experience of caring, less distress and expressed emotion, and better general health compared with carers who only receivedgold standard specialist treatment (defined here as treatment as usual [TAU]). Problem-solving involves specific identifiable steps in addressing problems, including problem orientation, definition of problems, “brainstorming of solutions,” evaluation of options, and implementation. It has been used widely in individual therapies (eg, depression) and in family therapy for schizophrenia.19–21
Our primary hypotheses were that the PSBI group would have a better experience of caring and a lower level of psychological distress compared with the TAU group, as assessed at 6-week and 16-week follow-up. Secondary hypotheses were that levels of expressed emotion would be lower and general health would be better in the PSBI group compared with the TAU group, as assessed at 6-week and 16-week follow-up.
Methods
The study was a RCT of a problem-solving bibliotherapy, which was used as an adjunct to gold standard support from specialist early intervention FEP services in Melbourne, Australia.
Participants
Participants were first-time carers who were recruited through case managers of two specialist FEP centers, Orygen Youth Health (OYH) and the Recovery and Prevention of Psychosis Service (RAPPS). The centers cater to young people aged 15–25 years, diagnosed with FEP (eg, schizophrenia, schizophreniform disorder, psychosis not otherwise specified, delusional disorder, brief reactive psychosis), with a duration of 2–3 years of treatment.
A carer was defined as the key person (aside from health, social, or voluntary care provider) responsible for assisting with activities of daily living and supporting and advocating on behalf of the young person with FEP.2 The study inclusion criteria were the following: (a) first-time carer (had never previously been in a caregiver role with any other individual), (b) in the carer role for less than three years, and (c) able to communicate in conversational English. Exclusion criteria were the following: (a) had been a recipient of specialist family interventions for FEP and (b) had recent personal history of serious and enduring mental illness.
Randomization
Carers were randomized to the PSBI or TAU control group. A computer-generated randomization list was drawn up by the statistician (SC), with randomization in blocks of 10 and given to the research officer (LC) who was responsible for recruitment. The researcher allocated the next available number on entry into the trial, and the code was not revealed until the completion of the baseline assessment to avoid selection bias and secure allocation concealment.
Treatments
Problem-Solving Bibliotherapy Intervention.
The PSBI group completed the self-help manual Reaching Out: Supporting a Family Member or Friend With First-Episode Psychosis (as well as receiving TAU), which was based on problem-solving therapy. Problem-solving based bibliotherapy,21 in this instance, involved helping carers to (a) develop a positive attitude to caregiving; (b) identify caregiving related problems by ascertaining the facts, identifying obstacles that inhibited goal achievement, and setting realistic goals; (c) consider a range of alternatives to circumvent the obstacles and achieve the stated goal; (d) predict positive and negative implications of each alternative in order to choose the one most likely to achieve the problem-solving goal; and (e) try out the solution and monitor if it worked and to what extent.
The manual contained 5 modules, written in plain language, that promoted a carer’s well-being and supported them in their caregiving role: (a) strengthening the carer’s well-being (physical and mental) and coping skills; (b) how to get the best out of support services (how to access services, and a framework for asking questions from treatment providers); (c) promoting the well-being of the person with FEP (how to prevent relapse and understand treatment options); (d) dealing with the effects of the illness Part A (communication, amotivation, social withdrawal, risky and unrestrained behavior, disturbed sleep, hallucinations and delusions); and (e) dealing with the effects of the illness Part B (weight gain, reluctance to take medication, substance misuse, aggression, and suicidal behavior).
Carers worked independently through the modules over 5 weeks. While they could do this at their own pace and at a time and place convenient to them, they were requested not to finish more than 1 module per week. The content of each module took up to 2h to complete and contained reading materials and exercises. Treatment adherence was assessed through weekly telephone calls from a research officer who asked the carer a set of standardized questions about the content of specific modules. Participants were also able to seek clarification about material covered in the readings.
Treatment as Usual.
TAU consisted of specialist support, coordinated by a case manager and psychiatrist, within an enriched assertive case management framework. This comprised the family being engaged and integrated within the patient’s individual treatment plan, with printed basic information about psychosis and additional support offered depending on assessment of need and phase of illness. At entry to the service, the family received at least one telephone call from a family peer support service for information and emotional support, with around 30% opting to have additional follow-up contact (telephone and face-to-face). Families were encouraged to participate in individual meetings with the case manager and doctor. They were also invited to take part in a 3-session psychoeducation group, run 3–4 times per year by case managers, though few accepted this invitation. For example, at OYH, of the 150 (approximate) admissions each year, about 25 families attended group sessions.
Primary Outcome Measures.
Primary outcome measures were the experience of caring and psychological distress, assessed using the Experience of Caregiving Inventory (ECI)22 and the Kessler Psychological Distress Scale (K10),23 respectively.
The ECI22 is a 66-item self-report questionnaire that assesses experience of caring for a relative with a serious mental illness within a stress-appraisal-coping framework.24 It is rated on a 5-point Likert scale, with responses ranging from 0 (never) to 4 (nearly always). The ECI has 10 subscales that measure negative (difficult behaviors, negative symptoms, stigma, problems with services, effects on family, need to backup, dependency, loss) and positive (positive personal experiences, good aspects of the relationship) aspects of caregiving. Higher scores on negative subscales and lower scores on positive subscales indicate negative appraisal.
The K1023 is a 10-item self-report questionnaire that assesses psychological distress in the general population.23 Items are rated on a 5-point Likert scale, with responses ranging from 0 (none of the time) to 4 (all of the time). Cut-off scores are below 20 (likely to be well), 20–24 (mild distress), 25–29 (moderate distress) and 30–50 (severe distress).25
Secondary Outcome Measures.
Secondary outcome measures were expressed emotion within the family and carers’ general health status, assessed using the Family Questionnaire (FQ)26 and the Short Form Health Survey (SF-12).27
The FQ26 is a 20-item self-report questionnaire that assesses Expressed Emotion (EE) directed at a client by family members. It has 2 subscales (critical comments, emotional over-involvement) rated on a 4-point Likert scale, ranging from 1 (never/very rarely) to 4 (very often). Critical comments are unfavorable statements about the personality or behavior of the client. Emotional over-involvement includes over intrusiveness, over protectiveness, and over identification with the client.28,29 Higher scores indicate greater levels of EE. The FQ has been validated against the Camberwell Family Interview, which is the gold standard measure of EE.26
The Short Form Health Survey (SF-12)27 is a 12-item self-report measure of perceived health status. It was scored according to Australian normative data.30 The instrument contains 2 subscales: physical health and emotional health, with scores normalized to a mean of 50 and a SD of 10. A higher score reflects better physical and emotional functioning.
Procedure
Ethical approval was obtained from university and health service research ethics committees. All participants provided written informed consent; the young person also provided verbal consent. Case managers were contacted when a client reached 9 weeks of treatment in the service to see if they were suitable for the study. This time frame allowed attempted engagement with the client and his/her family, as well as stabilization of their psychosis. Once consent was obtained, and if randomized to the PSBI group, the treatment manual was sent via post. In addition, baseline assessments were conducted with all participants via telephone. Research officers were blinded to group allocation to ensure unbiased assessments at both follow-up interviews (week 6 and week 16). Participants could choose to complete the questionnaire and mail/email their responses or provide them directly to research officers by telephone (most chose the latter option). Interrater reliability was maintained by training research officers to adhere to a written protocol for communicating with, and collecting data from, participants.
The PSBI group received a 10-min telephone call each week from a researcher to determine whether the module had been completed.
Data Analyses
Analyses were conducted using IBM® SPSS® Statistics Version 19. Data were screened prior to statistical analysis for accuracy of data entry, outliers, nonnormality, heterogeneity of variance, and heteroscedasticity. Differences between the PSBI and TAU groups at baseline were examined using independent sample t tests and chi-square (χ2) analyses. These statistical tests were also used to examine differences between completers and noncompleters. Intent-to-treat principles were used for the main data analyses; all cases were analyzed according to their assigned treatment group, and analysis was confined to those who had data for at least 1 follow-up time point.31 To contrast differences between the groups on the primary and secondary outcome variables at 6-week and 16-week follow-up, mixed model repeated measures (MMRM) ANOVA was used. The between-group factor was group (PSBI vs TAU) and the within-groups factor was assessment time point (baseline, 6 and 16 weeks). From these models, 3 parameters are tested: (a) main effect for group (overall, regardless of time, are there significant differences between the PSBI and TAU groups?); (b) main effect for time (overall, regardless of group, are there significant changes over time?); and (c) interaction between group and time (do the groups differ significantly over time?). A Toeplitz covariance matrix model was used to model the relationships between observations at the various assessment time points. Within each MMRM, planned comparisons (reported as t statistics) were used to compare differences between the groups from baseline to each of the 2 end points (6 and 16 weeks, end point analyses). MMRM are preferred to traditional ANOVA models in the analysis of clinical trial data in psychiatry because all available data are scrutinized, missing data does not have to be imputed, and the relationship between observations at various time points can be modeled.32 For all analyses, alpha (α) was set at the .05 level. No adjustments were made for multiple comparisons because of reduced power, increased risk of Type II errors, and missing important findings.33
Results
Participant Flow and Sample Characteristics
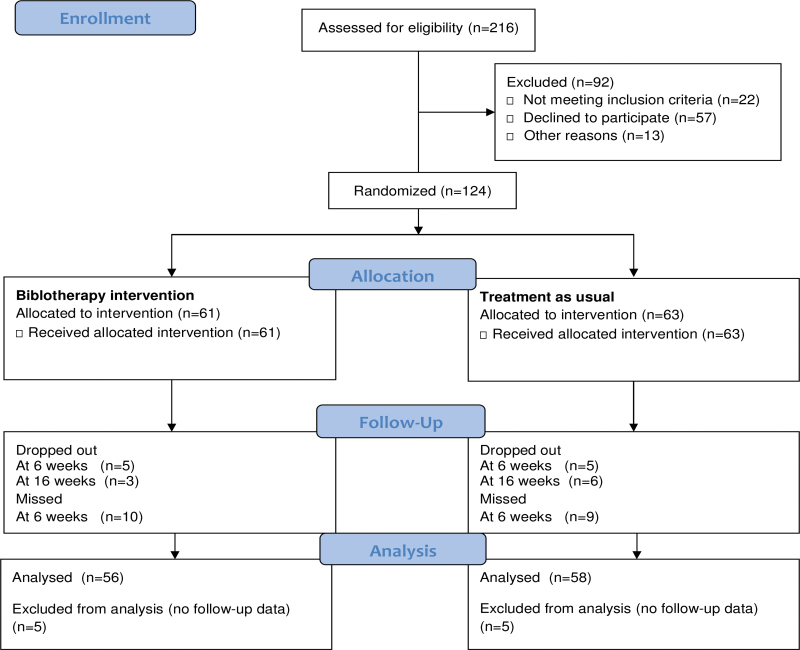
There were 216 individuals who were assessed for eligibility, of which 57.4% (n = 124) met the inclusion/exclusion criteria and consented to participate (figure 1). Reasons for exclusion included already receiving intensive support (n = 1), difficulties with conversing in, or reading, English (n = 18), and carer had a serious mental illness (n = 3).
Fig. 1.
CONSORT flowchart of participants through the study.
Sixty-one carers were randomized to the PSBI and 63 to TAU. Seventy-five carers were recruited from OYH and 49 from RAPPS. Table 1 depicts the demographic characteristics of the 124 carers. The majority were female, a parent of, and lived with the client. The majority of carers were also born in Australia, had tertiary-level qualifications, and earned between AU$ 20 000 and 50 000 per annum. The majority of clients were in the recovery phase. Carers reported that their support role had adversely affected their mental health (76.4%, n = 94), employment (62.7%, n = 69), physical health (59.3%, n = 73), and socialization (59.3%, n = 73).
Table 1.
Baseline Demographic Characteristics of the Total Group, as Well as the Problem-Solving Bibliotherapy Intervention and Treatment as Usual (TAU) Groups
| Total(n = 124) | Bibliotherapy(n = 61) | TAU(n = 63) | Statistic | Value | df | P value | ||
|---|---|---|---|---|---|---|---|---|
| Gender, % female | % (n) | 82.3 (102) | 80.3 (49) | 84.1 (53) | χ2 | 0.31 | 1 | .580 |
| Age | M (SD) | 47.2 (8.3) | 47.1 (8.3) | 47.3 (8.3) | t test | −0.18 | 120 | .860 |
| Relationship with first-episode psychosis patient, % parent | % (n) | 91.1 (113) | 93.4 (57) | 88.9 (56) | χ2 | 0.80 | 1 | .373 |
| Living with client, % yes | % (n) | 82.3 (102) | 86.9 (53) | 77.8 (49) | χ2 | 1.76 | 1 | .184 |
| Country of birth % other than Australia | % (n) | 34.7 (43) | 32.8 (20) | 36.5 (23) | χ2 | 0.19 | 1 | .663 |
| Length of time (months) in Australia if born in other countries | % (n) | 345.0 (187.5) | 335.8 (212.3) | 353.8 (165.4) | −0.30 | 39 | .763 | |
| Language spoken at home, % English | % (n) | 91.9 (113) | 90.2 (55) | 93.5 (58) | χ2 | 0.47 | 1 | .492 |
| Work status | ||||||||
| Professional/management/business | % (n) | 35.5 (44) | 37.7 (23) | 33.3 (21) | χ2 | 0.60 | 1 | .740 |
| Clerical/trade/retail/hospitality | % (n) | 25.0 (31) | 26.2 (16) | 23.8 (15) | ||||
| Other | % (n) | 39.5 (49) | 36.1 (22) | 42.9 (27) | ||||
| Still working in occupation, % yes | % (n) | 79.2 (95) | 85.0 (51) | 73.3 (44) | χ2 | 2.48 | 1 | .116 |
| Highest level of eduction | ||||||||
| Primary school | % (n) | 4.8 (6) | 3.3 (2) | 6.3 (4) | χ2 | 0.78 | 3 | .853 |
| High school | % (n) | 35.5 (44) | 37.7 (23) | 33.3 (21) | ||||
| TAFE | % (n) | 21.8 (27) | 21.3 (13) | 22.2 (14) | ||||
| Tertiary education | % (n) | 37.9 (47) | 37.7 (23) | 38.1 (24) | ||||
| Yearly household income | ||||||||
| Below AU$ 20,000 | % (n) | 15.0 (18) | 15.3 (9) | 14.8 (9) | χ2 | 1.04 | 3 | .792 |
| Between AU$ 20,000 and AU$ 50,000 | % (n) | 38.3 (46) | 33.9 (20) | 42.6 (26) | ||||
| Between AU$ 51,000 and AU$ 100,000 | % (n) | 32.5 (39) | 35.6 (21) | 29.5 (18) | ||||
| Above AU$ 100,000 | % (n) | 14.2 (17) | 15.3 (9) | 13.1 (8) | ||||
| Characteristics of first-episode psychosis patient | ||||||||
| Time since diagnosis of psychosis (in months) | M (SD) | 10.7 (8.8) | 12.4 (9.6) | 9.0 (7.7) | t test | 2.15 | 120 | .033 |
| Duration of support from early intervention service (in months) | M (SD) | 8.3 (6.5) | 9.4 (7.2) | 7.3 (5.6) | t test | 1.76 | 122 | .083 |
| Number of contacts with early intervention service | M (SD) | 2.6 (2.5) | 2.6 (2.1) | 2.6 (2.8) | t test | −0.031 | 120 | .975 |
| Phase of recovery | ||||||||
| Acute | % (n) | 14.7 (17) | 17.9 (10) | 11.7 (7) | χ2 | 0.887 | 1 | .346 |
| Recovery | % (n) | 85.3 (99) | 82.1 (46) | 88.3 (53) | ||||
There was a significantly longer time since diagnosis for the PSBI compared with the TAU group, t(120) = 2.15, P = .033. No other between-group differences were observed at baseline on any of the demographic variables (table 1) or with respect to any of the outcome measures.
Study Retention
Nineteen carers dropped out of the study (15.3%), 8 in the PSBI group (13.1%) and 11 in the TAU group (17.5%) with no significant between-group difference, χ2(1) = 0.45, P = .502. At 6 weeks, 5 in the PSBI group and 5 in the TAU group withdrew, and at 16 weeks, 3 in the PSBI and 6 in the TAU group withdrew. Nineteen carers missed the 6-week assessment but completed the 16-week assessment. There were no significant differences between completers and noncompleters of the study in terms of demographic variables. Noncompleters (M = 12.5, SD = 5.3), however, had experienced significantly more problems with services (ECI) at baseline compared with those who completed the study (M = 9.5, SD = 5.8), t(120) = −2.14, P = .035.
Primary Outcomes
Of the 10 ECI subscales, there was a significant interaction between group and assessment time for positive personal experiences, F(2, 165.38) = 3.56, P = .031. The TAU group showed significantly greater reductions in positive personal experiences from baseline to 6 weeks, t(156.2) = −2.44, P = .016, and baseline to 16 weeks, t(112.2) = −2.12, P = .036, compared with the PSBI group.
For the ECI need to back up subscale, or carers’ appraisal of the necessity to provide additional support to the young person, the interaction was close to being significant, F(2, 159.39) = 2.46, P = .088. Planned comparisons indicated that the PSBI group demonstrated a greater drop in negative appraisals of need to back up than the TAU group, from baseline to 6 weeks, t(161.34) = 2.08, P = .039 (tables 1 and 2).
Table 2.
Means (±SE) Derived From Mixed Effects Model Repeated Measures ANOVA for Measures of Experience of Caring, Psychological Distress, Expressed Emotion, and Emotional and Physical Functioning
| Baseline | 6 Weeks | 16 Weeks | ||||||
|---|---|---|---|---|---|---|---|---|
| BI | TAU | BI | TAU | P Valuea | BI | TAU | P Valueb | |
| Primary outcome measures | ||||||||
| Experience of caregiving | ||||||||
| Difficult behaviors | 14.9 (1.0) | 14.8 (0.9) | 13.9 (1.0) | 14.6 (1.0) | .519 | 13.1 (1.0) | 13.0 (1.0) | .936 |
| Negative symptoms | 13.8 (0.7) | 14.0 (0.7) | 11.9 (0.8) | 13.5 (0.8) | .151 | 12.1 (0.8) | 11.9 (0.8) | .761 |
| Stigma | 7.5 (0.6) | 7.4 (0.6) | 6.1 (0.6) | 7.0 (0.6) | .751 | 6.1 (0.6) | 5.7 (0.6) | .110 |
| Problems with services | 10.4 (0.8) | 9.5 (0.7) | 9.8 (0.8) | 9.3 (0.8) | .760 | 8.8 (0.8) | 8.5 (0.8) | .625 |
| Effects on family | 11.2 (0.8) | 11.5 (0.8) | 10.2 (0.8) | 10.5 (0.8) | .983 | 10.5 (0.8) | 9.7 (0.8) | .307 |
| Need to back up | 12.2 (0.7) | 12.4 (0.7) | 10.5 (0.8) | 12.3 (0.7) | .039 | 10.9 (0.7) | 11.3 (0.7) | .733 |
| Dependency | 12.3 (0.5) | 12.3 (0.5) | 10.5 (0.6) | 10.9 (0.6) | .630 | 10.7 (0.6) | 9.9 (0.6) | .253 |
| Loss | 13.7 (0.7) | 13.9 (0.7) | 10.9 (0.8) | 11.9 (0.7) | .255 | 11.2 (0.7) | 11.0 (0.7) | .678 |
| Total negative scale | 96.0 (4.5) | 95.8 (4.4) | 83.9 (4.8) | 90.3 (4.7) | .179 | 83.3 (4.7) | 81.6 (4.7) | .791 |
| Positive personal experiences | 15.9 (0.7) | 16.8 (0.7) | 16.9 (0.7) | 15.6 (0.8) | .016 | 15.7 (0.8) | 14.6 (0.7) | .036 |
| Good aspects of relationship | 14.5 (0.5) | 14.6 (0.5) | 13.7 (0.6) | 13.8 (0.6) | .957 | 13.8 (0.6) | 12.7 (0.6) | .127 |
| Total positive scale | 30.4 (1.1) | 31.4 (1.1) | 30.6 (1.2) | 29.4 (1.2) | .152 | 29.5 (1.2) | 27.3 (1.2) | .037 |
| Psychological distress | ||||||||
| K10 | 22.9 (1.1) | 22.1 (1.1) | 19.9 (1.2) | 21.8 (1.2) | .048 | 19.3 (1.1) | 21.0 (1.1) | .074 |
| Secondary outcome measures | ||||||||
| Family questionnaire | ||||||||
| Critical comments | 22.5 (0.8) | 21.9 (0.9) | 20.6 (0.9) | 22.1 (0.9) | .031 | 21.5 (0.9) | 21.6 (0.9) | .547 |
| Emotional overinvolvement | 27.6 (0.8) | 26.9 (0.7) | 25.3 (0.8) | 26.2 (0.8) | .096 | 24.5 (0.8) | 24.3 (0.8) | .645 |
| Health outcomes | ||||||||
| SF-12-physical health | 36.6 (1.1) | 34.1 (1.1) | 38.1 (1.2) | 36.8 (1.2) | .409 | 39.0 (1.2) | 35.8 (1.2) | .556 |
| SF-12-mental heatlh | 39.5 (1.4) | 38.2 (1.4) | 42.8 (1.5) | 42.1 (1.5) | .723 | 43.7 (1.5) | 39.8 (1.4) | .145 |
a P values derived from planned comparisons within mixed model repeated measures (reported as t statistics) of change from baseline to 6 weeks.
b P values derived from planned comparisons within mixed model repeated measures (reported as t tests) of change from baseline to 16 weeks.
The interaction between group and assessment time point was near significant for psychological distress, as assessed by the K10, F(2, 151.5) = 2.55, P = .081. Planned comparisons indicated that the level of psychological distress decreased at a greater rate in the PSBI group in comparison to the TAU group, from baseline to 6 weeks (P = .048), but this difference was not replicated between baseline and 16 weeks (P = .074).
Secondary Outcomes
With respect to the FQ, the interaction between group and assessment time point approached significance for critical comments (carer criticising the young person), F(2, 151.5) = 2.55, P = .081. The PSBI group demonstrated greater improvement from baseline to 6 weeks compared with the TAU group on the FQ critical comments, t(157.8) = 2.18, P = .031; however, no such difference was observed for the baseline to 16-week comparison. No between-group difference was found for the FQ emotional overinvolvement (EOI) subscale (carer being emotionally overinvolved with the young person; tables 1 and 2).
There were no significant between-group differences on the SF-12 subscales of emotional and physical functioning.
Supplementary Analyses
The analyses for primary and secondary outcomes were also conducted controlling for time since psychosis onset, which was found to have no impact. We also examined whether the 2 groups differed in their access of family support services within the two services. There was no difference between the 2 groups with respect to use of such services at week 6 [PSBI 25.0%, n = 11; TAU 22.7%, n = 10; χ2(1) = 0.063, P = .803] or at week 16 [PSBI 18.6%, n = 8; TAU 22.7%, n = 10; χ2(1) = 0.225, P = .635].
The relationship between completion of the manual and outcomes was examined in the PSBI group. Each week, participants noted how much of the recommended reading was completed on a scale from 1 “all” to 5 “none.” Completion of a week’s reading was defined on the basis of reading 1 “all” or 2 “most” of the module. A total score (dose of intervention) was derived on the basis of the number of weeks out of 5 that a module was completed. This variable was then correlated with primary and secondary outcome measures using Spearman’s rho (r s; preferred to Pearson’s Product Moment Correlation as dose is on an ordinal scale). Dose of intervention was significantly negatively but weakly related to ECI problems with services at 16 weeks (r s = −0.36, P = .009), indicating that greater dose was associated with more favorable outcome on this variable. Dose of intervention was very weakly and negatively associated with ECI good aspects of relationships at 16 weeks (r s = −0.28, P = .043) and ECI total positive score at 16 weeks (r s = −0.29, P = .038), indicating dose was associated with less favorable outcomes on these 2 variables.
Discussion
Primary Outcomes
We found partial support for our first primary hypothesis regarding the effect of bibliotherapy upon the experience of caring; in 2 of the 10 ECI subscales, there were differences between the PSBI and TAU groups. The PSBI group had a more favorable experience of caring for young people with FEP than the TAU group, and these effects were maintained at both follow-up time points. The PSBI group also experienced a greater reduction in negative appraisals of the need to provide additional support than the TAU group, though the effect was not sustained. The Gleeson et al.13 RCT demonstrated similar benefits for family members’ appraisal of caring for young people with FEP, however, the intervention in their study was more resource intensive and lengthy, comprising a CBT based manualized approach provided by a trained family therapist.
We found incomplete support for the effectiveness of bibliotherapy in reducing psychological distress. Overall, the results indicated that the effect of bibliotherapy on this construct was near significant, with the PSBI group reporting a lower level of distress compared with the TAU group. More subtle analysis indicated that the level of psychological distress decreased at a significantly greater rate from baseline to 6 weeks in the PSBI compared with the TAU group, but end point analysis for 16 weeks (group differences in change from baseline to 16 weeks) failed to reach significance, with reductions in levels of psychological distress evident across both groups. These findings are consistent with other FEP intervention studies that have reported decreased family/carer burden and distress,13,14 and they potentially reflect the initial high level of distress associated with having a relative develop an episode of psychosis and the subsequent improvement over time as the initial crisis stabilizes and carers begin coming to terms with the diagnosis.
Secondary Outcomes
We identified partial support for the beneficial effect of the manual on EE. The findings showed, overall, that the influence of the manual on critical comments of carers toward the young person with FEP-approached significance, with the PSBI group reporting fewer of these comments than the TAU group. Again, more subtle analyses indicated that the PSBI group reported greater improvement from baseline to 6 weeks in comparison to the TAU group on critical comments; however, such group differences were not maintained from baseline to 16 weeks.
There was no significant difference between the groups for EOI of carers. Previous research by members of our group has shown that EOI in young FEP clients is predicted by family stress, whereas level of criticism is predicted by duration of untreated psychosis (DUP).34 Other researchers have argued that EOI is associated with a tendency on the part of carers to blame themselves for the psychosis.1
There is evidence that criticism is indicative of a poor relationship between the client and carer prior to the onset of psychosis, leading to a tendency to attribute problematic behavior to deliberate actions on the part of the young person.1 Regardless of the cause, high EE has been shown in some studies of FEP to be associated with increased DUP,34 risk of psychotic relapse, and nonrecovery.19 The influence of these factors may partly account for the lack of sustained effect in the current study because the intervention did not directly address the premorbid relationship between carer and client.
There were also no differences in terms of emotional and physical health. Possible explanations for this nonsignificant result are that stress associated with caregiving only affects physical health in the longer term, such that it needs to be assessed over an extended period.35 Additionally, changes that were detected in the experience of caregiving, psychological distress, and to a lesser extent, EE, were issues that were directly related to the carers’ immediate circumstance rather than more global changes in perceptions of general health. This is unsurprising as carer well-being is closely associated with carer-recipient circumstances.2,36
Study Retention and Dose of Intervention
The retention rate in the present study compares favorably with other FEP intervention studies of carers13,14 and may be attributable to the problem-solving and plain language approach, weekly telephone calls, and convenience of being able to complete the manual at a time, place, and pace that suited the carer.
Regarding dose of intervention, completion or near completion of the manual each week over 5 weeks was associated with more favorable carers’ appraisal of caregiving, specifically, with respect to the burden in dealings with services. Dose of intervention was negatively associated with perceptions of the good aspects of carer-to-care recipient relationships and the overall positive aspects of caregiving, though caution is required in interpreting correlations as the associations were weak. The findings highlight the benefits to carers in actually finishing each and every module in the manual.
Strengths and Limitations
This is the first study to evaluate the effect of problem-solving bibliotherapy for first-time carers of young people with FEP. Strengths of the study included the randomization of participants, the blinding of research assistants during recruitment and follow-up data collection, the manualized intervention, flexibility and access for carers, and the telephone protocol to ensure treatment fidelity. A possible limitation of the study is it may be underpowered and need a larger sample of carers to demonstrate a greater effect, particularly because both groups demonstrated improvement on many of the variables over time. Another limitation is that the self-help manual was only offered for 5 weeks, which may explain why the short-term benefits observed were not sustained at 16 weeks. In addition, the 16-week follow-up period may have been too brief to expect significant improvement in carer outcomes.
Conclusion
Caregiving in FEP gives rise to positive and negative experiences for carers.2 Problem-solving bibliotherapy can help ameliorate negative, and enhance positive, experiences. The bibliotherapy manual used provided some short-term benefits to carers’ experience of caring, level of psychological distress, and EE though these effects were not sustained in the longer term. These findings are consistent with those of other FEP intervention studies,13,14 although few others have adopted a problem-solving approach13 or used bibliotherapy. Moreover, even though the relationship between bibliotherapy and relapse was not assessed in this study, family intervention, when combined with appropriate pharmacotherapy, typically reduces relapse rates by 20%–50%37,38 in individuals with schizophrenia and in those with FEP in particular.39
Despite the limitations outlined above, this study provides preliminary evidence that problem-solving bibliotherapy can be used successfully by first-time carers of young people with FEP. It is a nonthreatening and low-cost therapy, with potentially good reach and penetration, in comparison to other more complex and resource-intensive family interventions. Therefore, the approach could make a significant contribution as an adjunct to gold standard specialist treatment, particularly in a climate of fiscal restraint. From a research perspective, our findings indicate the need to extend the period of intervention. Optimally, the duration of intervention should be more than 3 months, and a follow-up of a year or longer is advisable to identify significant long-term benefits.37 One way of doing this is to incorporate periodic booster sessions, which can help stabilize the effects of the intervention over a longer time frame. Another consideration is that a facilitator or telephone contact person could be included to answer carers’ questions about the readings, help solve problems about caring and the care recipient, and for carers to access emotional support. A final consideration is that, while one of the inclusion criteria was that carers should be able to communicate in conversational English, a future study should consider translating the manual into other languages.
Table 3.
Tests of Fixed Effects in Mixed-Effects Model Repeated Measures ANOVA for Measures of Experience of Caring, Psychological Distress, Expressed Emotion, and Emotional and Physical Functioning
| Variable | Effects | F ratio | Numerator df | Denominator df | P Value |
|---|---|---|---|---|---|
| Primary outcome measures | |||||
| Experience of caregiving inventory | |||||
| Difficult behaviors | Group | 0.02 | 1 | 120.9 | .892 |
| Time | 4.30 | 2 | 175.5 | .015 | |
| Group × time | 0.32 | 2 | 175.5 | .744 | |
| Negative symptoms | Group | 0.30 | 1 | 121.2 | .570 |
| Time | 7.50 | 2 | 176.4 | .001 | |
| Group × time | 1.60 | 2 | 176.4 | .199 | |
| Stigma | Group | 0.04 | 1 | 123.7 | .835 |
| Time | 10.94 | 2 | 159.5 | <.001 | |
| Group × time | 2.11 | 2 | 159.5 | .125 | |
| Problems with services | Group | 0.36 | 1 | 122.7 | .551 |
| Time | 3.12 | 2 | 159.6 | .047 | |
| Group × time | 0.12 | 2 | 159.6 | .885 | |
| Effects on family | Group | 0.00 | 1 | 121.2 | .952 |
| Time | 4.39 | 2 | 189.0 | .014 | |
| Group × time | 0.66 | 2 | 189.0 | .520 | |
| Need to back up | Group | 0.80 | 1 | 122.7 | .372 |
| Time | 4.47 | 2 | 159.4 | .013 | |
| Group × time | 2.46 | 2 | 159.4 | .088 | |
| Dependency | Group | 0.03 | 1 | 122.8 | .864 |
| Time | 17.77 | 2 | 161.7 | <.001 | |
| Group × time | 1.39 | 2 | 161.7 | .252 | |
| Loss | Group | 0.14 | 1 | 123.5 | .712 |
| Time | 22.14 | 2 | 145.9 | <.001 | |
| Group × time | 1.42 | 2 | 145.9 | .246 | |
| Total negative scale | Group | 0.06 | 1 | 122.8 | .799 |
| Time | 13.59 | 2 | 152.7 | <.001 | |
| Group × time | 1.52 | 2 | 152.7 | .223 | |
| Positive personal experiences | Group | 0.27 | 1 | 123.7 | .605 |
| Time | 4.22 | 2 | 165.4 | .016 | |
| Group × time | 3.56 | 2 | 165.4 | .031 | |
| Good aspects of relationship | Group | 0.21 | 1 | 121.3 | .648 |
| Time | 5.42 | 2 | 184.7 | .005 | |
| Group × time | 1.53 | 2 | 184.7 | .220 | |
| Total positive scale | Group | 0.34 | 1 | 123.9 | .564 |
| Time | 5.64 | 2 | 172.2 | .004 | |
| Group × time | 2.36 | 2 | 172.2 | .097 | |
| Psychological distress | |||||
| K10 | Group | 0.43 | 1 | 122.2 | .516 |
| Time | 6.99 | 2 | 171.2 | .001 | |
| Group × time | 2.48 | 2 | 171.2 | .087 | |
| Secondary outcome measures | |||||
| Family questionnaire | |||||
| Critical comments | Group | 0.10 | 1 | 119.0 | .755 |
| Time | 1.46 | 2 | 151.5 | .236 | |
| Group × time | 2.55 | 2 | 151.5 | .081 | |
| Emotional overinvolvement | Group | 0.00 | 1 | 123.3 | .983 |
| Time | 16.71 | 2 | 157.4 | <.001 | |
| Group × time | 1.51 | 2 | 157.4 | .225 | |
| Health outcomes | |||||
| SF-12-physical | Group | 2.53 | 1 | 121.0 | .115 |
| Time | 7.05 | 2 | 170.4 | .001 | |
| Group × time | 0.90 | 2 | 170.4 | .409 | |
| SF-12-mental health | Group | 1.21 | 1 | 123.2 | .274 |
| Time | 11.15 | 2 | 153.1 | <.001 | |
| Group × time | 1.83 | 2 | 153.1 | .163 | |
Funding
Australian Rotary Health Research Fund (Mental Health). Trial registration: http://www.ANZCTR.org.au/ACTRN12609000064202.aspx.
Acknowledgments
Our thanks to the carer participants, the case managers, and carer support program for assistance with recruitment. Our appreciation to Flora McCann, Belinda Dimmock, and Dr Helen Baker for their contribution to data collection and Judith Johnston (nee McCann) for her contribution to the writing of the manual. The authors have declared that there are no conflicts of interest in relation to the conduct of this study. In the past 3 years, Dan Lubman has received speaking honoraria from Astra Zeneca and Janssen-Cilag and has provided consultancy support to Lundbeck.
References
- 1. Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis. Br J Psychiatry. 2010; 196:259–265 [DOI] [PubMed] [Google Scholar]
- 2. McCann TV, Lubman DI, Clark E. First-time primary caregivers’ experience of caring for young adults with first-episode psychosis. Schizophr Bull. 2011; 37:381–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berglund N, Vahlne JO, Edman A. Family intervention in schizophrenia–impact on family burden and attitude. Soc Psychiatry Psychiatr Epidemiol. 2003; 38:116–121 [DOI] [PubMed] [Google Scholar]
- 4. Asarnow JR, Tompson M, Hamilton EB, Goldstein MJ, Guthrie D. Family-expressed emotion, childhood-onset depression, and childhood-onset schizophrenia spectrum disorders: is expressed emotion a nonspecific correlate of child psychopathology or a specific risk factor for depression? J Abnorm Child Psychol. 1994; 22:129–146 [DOI] [PubMed] [Google Scholar]
- 5. Tompson MC, Pierre CB, Boger KD, McKowen JW, Chan PT, Freed RD. Maternal depression, maternal expressed emotion, and youth psychopathology. J Abnorm Child Psychol. 2010; 38:105–117 [DOI] [PubMed] [Google Scholar]
- 6. Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998; 55:547–552 [DOI] [PubMed] [Google Scholar]
- 7. Bebbington P, Kuipers L. The predictive utility of expressed emotion in schizophrenia: an aggregate analysis. Psychol Med. 1994; 24:707–718 [DOI] [PubMed] [Google Scholar]
- 8. Pilling S, Bebbington P, Kuipers E, et al. Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychol Med. 2002; 32:763–782 [DOI] [PubMed] [Google Scholar]
- 9. Jeppesen P, Petersen L, Thorup A, et al. Integrated treatment of first-episode psychosis: effect of treatment on family burden: OPUS trial. Br J Psychiatry Suppl. 2005; 48:s85–s90 [DOI] [PubMed] [Google Scholar]
- 10. Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2010. 10.1002/14651858.CD000088.pub2 [Google Scholar]
- 11. Onwumere J, Bebbington P, Kuipers E. Family interventions in early psychosis: specificity and effectiveness. Epidemiol Psychiatr Sci. 2011; 20:113–119 [DOI] [PubMed] [Google Scholar]
- 12. Grawe RW, Falloon IR, Widen JH, Skogvoll E. Two years of continued early treatment for recent-onset schizophrenia: a randomised controlled study. Acta Psychiatr Scand. 2006; 114:328–336 [DOI] [PubMed] [Google Scholar]
- 13. Gleeson JF, Cotton SM, Alvarez-Jimenez M, et al. Family outcomes from a randomized control trial of relapse prevention therapy in first-episode psychosis. J Clin Psychiatry. 2010; 71:475–483 [DOI] [PubMed] [Google Scholar]
- 14. Addington J, McCleery A, Addington D. Three-year outcome of family work in an early psychosis program. Schizophr Res. 2005; 79:107–116 [DOI] [PubMed] [Google Scholar]
- 15. Campbell LF, Smith TP. Integrating self-help books into psychotherapy. J Clin Psychol. 2003; 59:177–186 [DOI] [PubMed] [Google Scholar]
- 16. Jorm AF, Christensen H, Griffiths KM, Rodgers B. Effectiveness of complementary and self-help treatments for depression. Med J Aust. 2002; 176:S84–S96 [DOI] [PubMed] [Google Scholar]
- 17. Cuijpers P, Donker T, van Straten A, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med. 2010; 40:1943–1957 [DOI] [PubMed] [Google Scholar]
- 18. Bilich LL, Deane FP, Phipps AB, Barisic M, Gould G. Effectiveness of bibliotherapy self-help for depression with varying levels of telephone helpline support. Clin Psychol Psychother. 2008; 15:61–74 [DOI] [PubMed] [Google Scholar]
- 19. Falloon IR. Expressed emotion: current status. Psychol Med. 1988; 18:269–274 [DOI] [PubMed] [Google Scholar]
- 20. D’Zurilla TJ, Nezu AM. Problem-solving therapy. In: Dobson KS, ed. Handbook of cognitive-behavioral therapies. New York: Guilford Press; 2010. 197–225 [Google Scholar]
- 21. D’Zurilla TJ, Nezu AM. Problem-solving therapy: A positive approach to clinical intervention. New York: Springer; 2007. [Google Scholar]
- 22. Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the Experience of Caregiving Inventory. Soc Psychiatry Psychiatr Epidemiol. 1996; 31:137–148 [DOI] [PubMed] [Google Scholar]
- 23. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002; 32:959–976 [DOI] [PubMed] [Google Scholar]
- 24. Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York: Springer Publishing; 1984. [Google Scholar]
- 25. Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health. 2001;25:494–497 [DOI] [PubMed] [Google Scholar]
- 26. Wiedemann G, Rayki O, Feinstein E, Hahlweg K. The Family Questionnaire: development and validation of a new self-report scale for assessing expressed emotion. Psychiatry Res. 2002; 109:265–279 [DOI] [PubMed] [Google Scholar]
- 27. Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34:220–233 [DOI] [PubMed] [Google Scholar]
- 28. Vaughn CE, Leff JP. Patterns of emotional response in relatives of schizophrenic patients. Schizophr Bull. 1981; 7:43–44 [DOI] [PubMed] [Google Scholar]
- 29. Leff JP, Vaughn C. Expressed Emotion in Families: It’s Significance for Mental Illness. New York: Guilford Press; 1985. [Google Scholar]
- 30. Tucker G, Adams R, Wilson D. New Australian population scoring coefficients for the old version of the SF-36 and SF-12 health status questionnaires. Qual Life Res. 2010; 19:1069–1076 [DOI] [PubMed] [Google Scholar]
- 31. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999; 319:670–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004; 61:310–317 [DOI] [PubMed] [Google Scholar]
- 33. Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990; 1:43–46 [PubMed] [Google Scholar]
- 34. Alvarez-Jiménez M, Gleeson JF, Cotton SM, et al. Differential predictors of critical comments and emotional over-involvement in first-episode psychosis. Psychol Med. 2010; 40:63–72 [DOI] [PubMed] [Google Scholar]
- 35. Dyck DG, Short R, Vitaliano PP. Predictors of burden and infectious illness in schizophrenia caregivers. Psychosom Med. 1999; 61:411–419 [DOI] [PubMed] [Google Scholar]
- 36. Askey R, Holmshaw J, Gamble C, Gray R. What do carers of people with psychosis need from mental health services? Exploring the views of carers, service users and professionals. J Fam Ther. 2009; 31:310–331 [Google Scholar]
- 37. Pitschel-Walz G, Leucht S, Bäuml J, Kissling W, Engel RR. The effect of family interventions on relapse and rehospitalization in schizophrenia–a meta-analysis. Schizophr Bull. 2001; 27:73–92 [DOI] [PubMed] [Google Scholar]
- 38. Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull. 2004; 30:193–217 [DOI] [PubMed] [Google Scholar]
- 39. Gleeson JF, Cotton SM, Alvarez-Jimenez M, et al. A Randomized Controlled Trial of Relapse Prevention Therapy for First-Episode Psychosis Patients: Outcome at 30-Month Follow-up. Schizophr Bull. 2011. 10.1093/schbul/sbr165. [DOI] [PMC free article] [PubMed] [Google Scholar]