Abstract
Objective
To test the effectiveness of a telephone care management intervention to increase the use of primary and preventive care, reduce hospital admissions, and reduce emergency department visits for Medicaid beneficiaries with disabilities in a managed care setting.
Data Source
Four years (2007–2011) of Medicaid claims data on blind and/or disabled beneficiaries, aged 20–64.
Study Design
Randomized control trial with an intervention group (n = 3,540) that was enrolled in managed care with telephone care management and a control group (n = 1,524) who remained in fee-for-service system without care management services. Multi-disciplinary care coordination teams provided telephone services to the intervention group to address patients' medical and social needs.
Data Collection/Extraction
Medicaid claims and encounter data for all participants were obtained from the state and the managed care organization.
Principal Findings
There was no significant difference in use of primary care, specialist visits, hospital admissions, and emergency department between the intervention and the control group. Care managers experienced challenges in keeping members engaged in the intervention and maintaining contact by telephone.
Conclusions
The lack of success for Medicaid beneficiaries, along with other recent studies, suggests that more intensive and more targeted interventions may be more effective for the high-needs population.
Only about 7 percent of Medicaid beneficiaries are blind and/or disabled, but they account for 40 percent of Medicaid spending (Vladeck 2003). Because they are low income as well, they are likely to be a vulnerable and hard-to-reach group that experiences greater difficulty navigating the health care system (Agency for Healthcare Research and Quality 2008; Kaiser Family Foundation 2010). Many states are looking for cost-effective strategies to provide medical services to this population. One such strategy is care management.
Care management describes programs that are intended to increase appropriate use of medical care while reducing unnecessary services, such as emergency department (ED) visits and hospitalizations (Wagner et al. 2001; Mattke, Seid, and Ma 2007). In care management programs, to meet patients' needs, care managers (who are usually nurses or Master's level clinicians) encourage patients to seek appropriate treatment, help them find and make appointments with health care professionals, make sure they are keeping appointments and taking prescribed medications, educate them about treatment effectiveness, and identify other needs that patients might have (Wagner et al. 2001; Rittenhouse and Robinson 2006). Care managers also often work with primary care physicians (PCPs), providing them with information designed to help them monitor a patient's overall health care use and communicate with other health care providers.
Care management programs have traditionally focused on patients with chronic conditions such as diabetes mellitus, asthma, depression, coronary artery disease, and congestive heart failure (Wagner et al. 2001; Mattke, Seid, and Ma 2007). Studies have shown that care management can improve health outcomes for patients with particular chronic health conditions, such as diabetes (Sidorov et al. 2002; Dorr et al. 2005; Glazier et al. 2006; Chin et al. 2007), cardiovascular disease (Harris et al. 2003; Sequist et al. 2006), and congestive heart failure (Gorski and Johnson 2003; DeWalt et al. 2006). For patients with depression, care management has encouraged patients to talk to mental health specialists, increased their use of antidepressants, reduced their depression, improved their health, and improved their work performance and job retention (Wang et al. 2007; Mohr et al. 2008; Kroenke et al. 2010). In addition, care management has been found to reduce the costs of care in some settings (Handley, Shumway, and Schillinger 2008), although this might not be the norm (Peikes et al. 2009).
Despite the success of care management in some settings, there has not been a rigorous evaluation of this approach in a diverse set of Medicaid beneficiaries with multiple chronic conditions. For example, studies of Medicaid care management in Florida (Afifi et al. 2007; Kominski et al. 2008) and Virginia (Zhang et al. 2008) have found improvements such as fewer hospital stays and ED visits. However, those studies used nonrandomly chosen comparison groups, and the results may have confounded the effects of the programs with other unobserved differences between the groups (Rosenbaum and Rubin 1983; Bell et al. 1995; Michalopoulos, Bloom, and Hill 2004). This is an important gap in the research as more than 20 states operate some form of care management for this population (Rosenman et al. 2006; Arora et al. 2008). This article begins to fill this gap in knowledge by presenting results from a randomized study of a telephone care management program for blind and/or disabled Medicaid beneficiaries in Colorado, many of whom often have multiple chronic conditions.
Methods
Sample and Recruitment
Individuals were eligible for the study if they were blind and/or disabled and receiving Medicaid in Colorado through the fee-for-service (FFS) system in five Denver-area counties (Adams, Arapahoe, Boulder, Broomfield, and Weld). Individuals were excluded if they were under 18 or more than 64 years of age, were dually eligible for both Medicare and Medicaid, were in a long-term care facility, or were AIDS or brain injury patients receiving Home and Community Based Services (another Medicaid program available to individuals with disabilities).
From April 2008 to May 2009, the Department of Health Care Policy and Financing (HCPF), which administers Medicaid for Colorado, generated a list of Medicaid beneficiaries who were eligible for the intervention, but not yet included in the study. The evaluation team randomly assigned 70 percent of individuals on the list to the intervention group and 30 percent to the control group. A higher proportion was assigned to the intervention group to meet the managed care organization's requirements for a minimum program size. The random assignment occurred in April to November 2008 and January to May 2009. Letters were sent to the intervention group explaining that they were being placed into managed care and asking them to choose a managed care plan or to opt out of managed care within 3 months. If the person did not respond by that deadline, he or she was placed in the managed care program studied in this article. Individuals could also opt out of this managed care plan on the anniversary of their passive enrollment. A total of 5,064 Medicaid beneficiaries were randomly assigned, with 3,540 beneficiaries to the intervention group and 1,524 beneficiaries to the control group. About 83 percent of the intervention and control group members remained enrolled in Medicaid for the entire follow-up period.
Figure 1 illustrates the flow of individuals into the programs. Among those who were assigned to the intervention group, 2,602 were enrolled in the managed care plan at some point. Another 864 opted out of that managed care and remained in FFS Medicaid, while 74 people opted for other managed care plans in the region that were not part of the study. Although the State allowed control group members to opt into any managed care program, only 64 people (about 4 percent) volunteered for managed care (of which 14 individuals opted into the managed care program that provided care management [not shown in Figure 1]).
Figure 1.
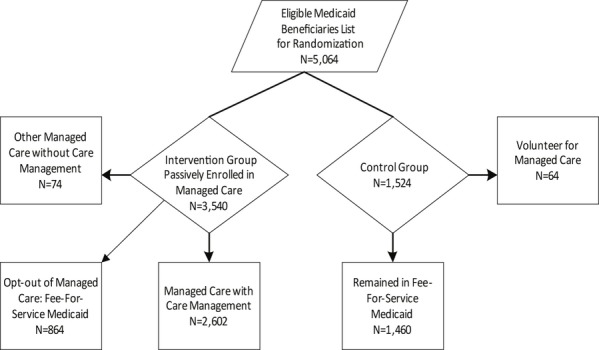
Participant Enrollment
The study sample size was chosen to provide sufficient statistical power for an intent-to-treat analysis even with a 50 percent opt-out rate. The design was sensitive enough to detect impacts of 5–7 percentage points on outcomes such as the proportion hospitalized and the proportion with any ED visit (using two-tailed tests and 10 percent significance level) on those who actually received the intervention even with an opt-out rate of 50 percent. As it was projected by the managed care organization that there would be a reduction of 10 percentage point in outcomes such as hospital admissions and ED use, the design was determined to have sufficient statistical power.
The Intervention Group
Care managers' first responsibility was to enroll individuals assigned to the intervention group into the care management program. Outreach was done telephonically and care managers often required 10–20 calls to reach a member. Early on, the care manager assessed each individual's health care and social service needs. Based on these assessments, about 10 percent of individuals were considered to have few health care needs and to be compliant with their treatment plans. Care managers followed up annually with this group. The majority of the intervention group (about 70 percent) had about one contact every 3 months because they had moderate to high medical costs and had new or serious diagnoses such as diabetes, congenital health failure, or chronic obstructive pulmonary disease. They often had psychological or emotional instability with poor coping mechanisms as well. The remaining 20 percent of the intervention group had high medical expenses but were already well connected to a treatment system. This group was contacted by the care manager every 6 months. There were no enrollment length criteria for the intervention group, but 60 percent of the intervention group members remained in the program for at least 90 percent of the follow-up months.
Care managers came from diverse professional backgrounds, including mental health counseling, quality improvement in the health field, psychology, clinical research, and geriatric nursing. There were several bilingual Spanish speakers available at any given time. Two registered nurses supervised care managers. The care managers held weekly multi-disciplinary consultations and reviewed the cases with nurse supervisors.
Care managers were given considerable discretion in how they addressed the needs of the patients. Care managers made sure that each individual had a primary care provider and helped to coordinate care across providers. Care managers also developed care plans with goals related to health care (such as reducing ED use) and social service needs (such as arranging for transportation to a doctor or helping the individual to find stable housing). In addition to medical and social services, the care managers made appropriate referrals to behavioral or mental health services for individuals with psychiatric and/or substance use disorders. Because the care managers did not work exclusively with the study population, their total caseload could have ranged between 300 and 800 cases, of which about 100 cases represented the intervention group. The caseload included members with a range of needs and frequency of contact requirements.
The Control Group
The control group remained in the FFS system without care coordination services for the follow-up period. To receive permission from the Centers for Medicare & Medicaid Services to allow individuals to be randomized, control group members were allowed to volunteer to join a managed care plan, including the plan that offered care management. Few control group members were expected to enroll in the latter plan and few did.
Data Sources
HCPF provided Medicaid claims data (April 2007 to May 2011) with information on the use of services for the entire sample prior to random assignment and for individuals who remained in FFS Medicaid following random assignment. For individuals in the managed care plan, data on health care use came from the managed care plan until the end of February 2010, at which point it came from HCPF. The change in data sources was due to a change in the contract between the managed care plan and HCPF. Prior to March 2010, the managed care organization received a monthly payment for individuals in their program. After that point, while the managed care plan continued to provide care management, health care services were paid by FFS.
Two important sources of data are missing. Colorado provides behavioral health care for Medicaid beneficiaries through behavioral health carve-outs. Data from these organizations were not available for the evaluation. In addition, data from other managed care plans that did not participate in the study were not available, even though some study participants opted to enroll in these plans.
Outcome Measures
The main outcome variables measured are use of health care services, including outpatient care, inpatient care, and ED use. The National Provider Identifier (NPI) registry from the Centers for Medicare & Medicaid Services (2008) was used to categorize outpatient visits and define the type of providers. NPI provides a standard unique health identifier for health care providers. A visit to a PCP was defined as any visit to general practice, family medicine, internal medicine, obstetric and gynecology, nurse practitioner, and physician assistant. Nonphysician visits included visits to physical medicine/rehabilitation, occupational therapy, podiatry, optometry, audiology, and speech therapy. Specialist visits were defined as visits to physicians in specialty fields such as neurology, radiology, ophthalmology, oncology, nephrology, and orthopedic surgery. The number of visits is the average per patient.
Revenue codes were used to determine when a patient was admitted to a hospital. This information was used to define all admissions and readmission within 30 days. ED visits were also defined using revenue codes, including ED visits that led to admission. All outcomes were calculated for the first and second year of the intervention period, months 1 through 12 and 13 through 24 following study enrollment.
Covariates
Demographic information available in the data includes age, gender, and county of residence. ICD-9 diagnosis codes from Medicaid claims for the year prior to study enrollment were used to categorize chronic conditions according to the Chronic Illness and Disability Payment System (CDPS), as shown in Table 1 (Kronick et al. 2000). The CDPS is a method used to predict health care costs in the next year by using groupings of diagnoses and expenditures that are associated with care. Measures of health care use and diagnoses in the year prior to study enrollment were also used as covariates. Measures of health care use include number of visits to PCP, nonphysicians, specialists, ED, and inpatient stays.
Table 1.
Demographic and Health Care Use in Year Prior to Study Entry
| Characteristic | Full Sample | Intervention Group | Control Group | p-value§ |
|---|---|---|---|---|
| Average age (years)† | 44.23 | 44.30 | 44.05 | .54 |
| Female | 58.81 | 58.42 | 59.71 | .39 |
| Health care use in prior year | ||||
| Ever had an emergency department (ED) visit (%) | 42.69 | 42.54 | 43.05 | .74 |
| Average number of ED visits | 1.27 | 1.28 | 1.24 | .64 |
| Ever had a hospital admission (%) | 17.54 | 17.37 | 17.91 | .64 |
| Average number of total inpatient days | 3.01 | 2.84 | 3.40 | .21 |
| Average CDPS score‡ | 1.58 | 1.54 | 1.67 | .02* |
| Total Medicaid cost in prior year ($) | 15,050 | 14,645 | 15,990 | .16 |
| Chronic conditions (%) | ||||
| Cardiovascular | 36.83 | 36.78 | 36.94 | .91 |
| Central nervous system | 21.74 | 21.53 | 22.24 | .57 |
| Cerebrovascular | 3.36 | 3.45 | 3.15 | .58 |
| Diabetes, type 1 | 5.11 | 4.69 | 6.10 | .05* |
| Diabetes, type 2 | 12.15 | 12.26 | 11.88 | .70 |
| Eye | 6.60 | 6.47 | 6.89 | .58 |
| Gastrointestinal | 21.90 | 21.72 | 22.31 | .64 |
| Hematological | 4.98 | 4.83 | 5.32 | .48 |
| Infectious | 8.99 | 8.53 | 10.04 | .09 |
| Metabolic | 11.65 | 11.72 | 11.48 | .81 |
| Psychiatric | 29.98 | 29.72 | 30.58 | .54 |
| Pulmonary | 25.02 | 24.46 | 26.31 | .16 |
| Renal | 11.91 | 11.27 | 13.39 | .04* |
| Skeletal and connective | 23.56 | 23.45 | 23.82 | .77 |
| Skin | 10.13 | 9.94 | 10.56 | .50 |
| Substance abuse | 10.80 | 10.68 | 11.09 | .67 |
| Sample size | 5,064 | 3,540 | 1,524 | |
Notes. *Significant at p ≤ .05; **significant at p ≤ .01.
Fifty-nine cases had missing age.
CDPS, Chronic Illness and Disability Payment System.
t-test statistics was done to test for differences in age, gender, health care use, and chronic conditions between the study groups.
Data Analysis
Estimating Intent-to-Treat Effects
Estimated impacts for use of health care services (binary outcomes) are based on logistic regression-adjusted intent-to-treat comparisons of the intervention and control groups. Zero-inflated negative binomial (ZINB) regression models were used for outcomes related to number of visits and admissions. ZINB models were indicated by specification tests for excessive zeros and overdispersed counts. The regression models controlled for age, gender, and counties where participants lived and their diagnosed conditions. Any health care use in the year prior to the program start date was also controlled.
High-Needs Subgroup
The second part of the analysis focused on a subgroup of patients who were expected to be high health care users. It was expected that the telephone care management would have its largest effects for individuals with the most chronic conditions, the highest likelihood of being hospitalized, and the greatest use of ED care. To define this subgroup, individuals were ranked based on the costs of Medicaid services used in the year prior to entering the study and their CDPS score. The two rankings were added together, and the top 20 percent highest ranking cases were considered to have high health care needs that could be affected through coordinated care. The same regression models that were used for the full sample were used for this subgroup analysis to estimate the impact of telephone care management on use of health care services.
Additional Analysis on Managed Care Participation: Predicted Probability of Enrollment with Matched Samples and High Enrollment Subgroup
Because a large portion of the intervention group opted out of managed care, the intent-to-treat analysis may understate the effects of the care management intervention. To try to isolate the effects of the intervention, baseline characteristics were used to define a subgroup that was more or less likely to participate in the managed care program with care management. To define the subgroup, a logistic regression was run using intervention group members to determine which baseline characteristics were associated with enrollment in the program. Results of the logistic regression were used to calculate a predicted probability of enrollment for each person in the study.
The predicted probability was then divided into deciles for both the intervention and the control group. To match the intervention group members who were not enrolled in care management, a random sample was drawn of the control group members in the same deciles as the intervention group. The sample of control group members was selected so that the total sample size was proportionate to the nonenrollment rate of the intervention group, which was 26 percent. For the matched enrollment group, all the intervention group members who were enrolled in care management and control group members who were not selected for the nonenrolled matched group were selected, which was 74 percent of the intervention and the control group.
In an additional analysis, intervention group and control group members with predicted probabilities above the median were placed in the high probability of enrollment subgroup, while other individuals were placed in the low probability of enrollment subgroup. About 82 percent of intervention group members in this high enrollment subgroup were enrolled in managed care with telephone care management for at least 1 month, compared with 64 percent of the remaining intervention group. Thus, estimated effects should be substantially larger for the high enrollment subgroup as many more of them would presumably have received telephone care management. Because the predicted probability was calculated using baseline information, these analyses with predicted probability preserve the benefits of the intent-to-treat analysis. The results are consequently unbiased estimates of the program's effects for the subgroups. All analyses were done using SAS Enterprise Guide 4.3 and SAS 9.2 software (SAS Institute Inc. Cary, NC, USA).
Results
Characteristics of the Sample
Table 1 describes the study participants, their diagnoses, and their use of health care in the year prior to the study. Participants were 44 years old on average, and about 60 percent were female. The most common chronic condition was cardiovascular disease (nearly 40 percent of the sample), which included congestive heart failure, cardiomyopathy, and coronary atherosclerosis. A little less than a third had a psychiatric diagnosis, which included conditions such as bipolar affective disorder, depression, and phobic disorders. About a quarter of the sample also reported having skeletal and connective (e.g., rheumatoid arthritis, osteoporosis, and traumatic amputation of foot or leg), pulmonary (e.g., pulmonary hypertension, pneumonia, chronic obstructive asthma, and emphysema), gastrointestinal (e.g., chronic liver disease and cirrhosis, and regional enteritis and ulcerative colitis), or central nervous system conditions (e.g., muscular dystrophy, multiple sclerosis, other neuron diseases) (Kronick et al. 2000). A little less than one-fifth of the sample had diabetes (Type 1 and 2). On average, participants had three chronic conditions and for the high-needs group, five conditions (not shown). The CDPS score was 1.54 for the intervention group and slightly higher for the control group (1.67). These numbers mean that intervention group was expected to use about 54 percent more health care than typical Medicaid recipients with disabilities while the control group was predicted to use about 67 percent more health care than typical Medicaid recipients with disabilities.
Use of Health Care Services: Intent-to-Treat Analysis
During the 2 years of the intervention, the only significant difference between the intervention and the control group was nonphysician visits (Table 2). About 17 percent of the intervention group members had a visit to a nonphysician, which included services from an optometrist, physical therapist, podiatrist, or speech therapist, compared with 13 percent of the control group. The odds of having a nonphysician visit for the intervention group is about 40 percent higher than the odds for the control group (OR = 1.39, 95% CI:1.2–1.7) in the first year of follow-up. This positive impact persisted through the second year. There were no differences between the intervention and control group members in visits to PCPs or specialists. The intervention also did not have impact on hospital admissions or ED visits.
Table 2.
Estimated Impacts on Service Use during Year 1 and 2 Following Study Enrollment: Regression-Adjusted Means and Coefficients
| 95% Confidence Limits | |||||
|---|---|---|---|---|---|
| Outcomes† | Intervention Group (%) | Control Group (%) | Odds Ratio | Lower | Upper |
| Any use of health care, months 1–12 | |||||
| Had a primary care physician visit (PCP) | 65.09 | 65.82 | 0.96 | 0.82 | 1.11 |
| Had a nonphysician visit | 16.76 | 13.19 | 1.40 | 1.16 | 1.69*** |
| Had a specialist visit | 62.85 | 62.21 | 1.04 | 0.90 | 1.20 |
| Ever admitted to a hospital | 15.99 | 15.35 | 1.06 | 0.88 | 1.27 |
| Readmitted within 30 days | 3.51 | 3.03 | 1.20 | 0.82 | 1.74 |
| Ever used an emergency department (ED) | 40.46 | 39.88 | 1.03 | 0.90 | 1.18 |
| Any use of health care, months 13–24 | |||||
| Had a PCP visit | 61.36 | 61.74 | 0.98 | 0.85 | 1.13 |
| Had a nonphysician visit | 14.94 | 12.96 | 1.21 | 1.00 | 1.46* |
| Had a specialist visit | 58.24 | 57.11 | 1.06 | 0.92 | 1.22 |
| Ever admitted to a hospital | 12.73 | 13.15 | 0.96 | 0.79 | 1.16 |
| Readmitted within 30 days | 2.48 | 1.93 | 1.32 | 0.85 | 2.07 |
| Ever used an ED | 37.60 | 36.23 | 1.07 | 0.94 | 1.23 |
| Negative Binomial Model Predicting Number of Visits | |||||
|---|---|---|---|---|---|
| Outcomes‡ | Intervention Group | Control Group | Estimate | SE | p-value |
| Average number of visits for health care services, months 1–12 | |||||
| PCP visits | 4.72 | 4.61 | 0.01 | 0.12 | .91 |
| Nonphysician visits | 0.79 | 0.63 | −1.10 | 0.23 | <.001*** |
| Specialist visits | 6.90 | 6.56 | −0.06 | 0.14 | .65 |
| Hospital admissions | 0.29 | 0.24 | 0.17 | 0.26 | .50 |
| Inpatient days | 1.99 | 1.74 | −0.07 | 0.10 | .47 |
| Emergency department visits | 1.31 | 1.30 | 0.18 | 0.17 | .27 |
| Average number of visits for health care services, months 13–24 | |||||
| PCP visits | 4.19 | 4.27 | 0.01 | 0.11 | .91 |
| Nonphysician visits | 0.69 | 0.63 | −0.71 | 0.21 | <.001*** |
| Specialist visits | 5.72 | 5.94 | −0.08 | 0.13 | .51 |
| Hospital admissions | 0.21 | 0.21 | −0.01 | 0.38 | .99 |
| Inpatient days | 1.36 | 1.36 | 0.06 | 0.10 | .58 |
| Emergency department visits | 1.16 | 1.07 | −0.08 | 0.23 | .74 |
| Sample size (total = 5,064) | 3,540 | 1,524 | |||
Notes. *Significant at p ≤ .05; **significant at p ≤ .01; ***significant at p ≤ .001.
Probabilities percentages and odds ratio from logistic regression models adjusted for age, gender, county of residence, medical conditions, and prior health care use.
Number of visits for intervention and control group calculated from linear regression and negative binomial estimates from zero-inflated negative binomial models; both models adjusted for age, gender, county of residence, medical conditions, and prior health care use.
The results from models predicting number of visits from ZINB regressions are also shown in Table 2. There was a significant difference in the number of nonphysician visits (for the first and second year of follow-up). Although the adjusted number of nonphysician visits from the linear regression model controlling for age, sex, county of residence medical condition, and prior health care use was 0.8 for the intervention group and 0.6 for the control group during the 1 year follow-up, the intervention group visit rate is actually lower in the ZINB model. For example, during the first year follow-up, for the intervention group members, the expected number of visits to nonphysicians decreased by a factor of 0.33( = e−1.10) among those who had nonphysician visits. Similarly, for the second year follow-up, the intervention group members had fewer visits by a factor of 0.49( = e−0.71).
High-Needs Subgroup
The same analyses of examining the difference between the intervention and the control group were done for the subgroup of high health care users. They were expected to be among the top 20 percent highest ranking cases in terms of medical expenditure. The results (not shown in the table) showed that both the intervention and control group members from the top 20 percent did use more health care than the other 80 percent of the sample. However, there was no significant difference between the intervention and the control group among the top 20 percent.
Predicted Probability of Participation in Managed Care
Because a large proportion of the intervention group never received the intervention, additional analysis was done to try to isolate the effects of the intervention. The subgroup analysis with the intervention group enrolled in care management with matched control group found similar results as the full sample (Table 3). For example, the only significant outcome for the matched enrollment subgroup was nonphysician visits. This analysis indicates that the nonenrollees did not impact the results.
Table 3.
Estimated Impacts on Service Use during Year 1 and 2 Following Study Enrollment: Matched Predicted Probability of Participation in Managed Care
| 95% Confidence Limits | |||||
|---|---|---|---|---|---|
| Outcomes† | Intervention Group | Control Group | Odds Ratio | Lower | Upper |
| Any use of health care, months 1–12 | |||||
| Had a primary care physician visit (PCP) | 65.91 | 65.10 | 1.05 | 0.88 | 1.26 |
| Had a nonphysician visit | 16.77 | 13.19 | 1.38 | 1.12 | 1.72** |
| Had a specialist visit | 61.45 | 60.28 | 1.07 | 0.90 | 1.27 |
| Ever admitted to a hospital | 16.73 | 14.99 | 1.17 | 0.95 | 1.45 |
| Readmitted within 30 days | 3.70 | 3.04 | 1.28 | 0.82 | 1.99 |
| Ever used an emergency department (ED) | 42.74 | 40.64 | 1.12 | 0.95 | 1.32 |
| Any use of health care, months 13–24 | |||||
| Had a PCP visit | 62.30 | 60.90 | 1.08 | 0.92 | 1.28 |
| Had a nonphysician visit | 14.30 | 11.84 | 1.28 | 1.02 | 1.60* |
| Had a specialist visit | 56.13 | 54.69 | 1.08 | 0.92 | 1.26 |
| Ever admitted to a hospital | 13.09 | 13.70 | 0.94 | 0.76 | 1.17 |
| Readmitted within 30 days | 2.62 | 2.12 | 1.27 | 0.76 | 2.13 |
| Ever used an ED | 39.99 | 37.57 | 1.13 | 0.96 | 1.32 |
| Negative Binomial Model Predicting Number of Visits | |||||
|---|---|---|---|---|---|
| Outcomes‡ | Intervention Group | Control Group | Estimate | SE | p-value |
| Average number of visits for health care services, months 1–12 | |||||
| PCP visits | 4.39 | 4.41 | −0.13 | 0.15 | .40 |
| Nonphysician visits | 0.58 | 0.50 | −1.33 | 0.32 | <0.001*** |
| Specialist visits | 6.91 | 6.10 | −0.09 | 0.18 | .61 |
| Hospital admissions | 0.30 | 0.23 | −0.06 | 0.28 | .83 |
| Inpatient days | 1.82 | 1.50 | −0.18 | 0.12 | .12 |
| Emergency department visits | 1.42 | 1.32 | 0.20 | 0.20 | .32 |
| Average number of visits for health care services, months 13–24 | |||||
| PCP visits | 4.11 | 4.34 | −0.17 | 0.14 | .22 |
| Nonphysician visits | 0.45 | 0.46 | −0.89 | 0.24 | <0.001*** |
| Specialist visits | 5.80 | 5.78 | −0.16 | 0.16 | .31 |
| Hospital admissions | 0.23 | 0.22 | 0.31 | 0.43 | .48 |
| Inpatient days | 1.40 | 1.49 | 0.07 | 0.12 | .52 |
| Emergency department visits | 1.25 | 1.12 | 0.002 | 0.33 | .99 |
| Sample size (total = 3,722) | 2,602 | 1,120 | |||
Notes. *significant at p ≤ .05; **significant at p ≤ .01; ***significant at p ≤ .001.
Probabilities percentages and odds ratio from logistic regression models adjusted for age, gender, county of residence, medical conditions, and prior health care use.
Number of visits for intervention and control group calculated from linear regression and negative binomial estimates from zero-inflated negative binomial models; both models adjusted for age, gender, county of residence, medical conditions, and prior health care use.
Similarly, we found that when we defined the subgroups as high and low enrollment groups, it did not result in many significant findings (not shown in Table). The enrollment subgroups were defined by likelihood of enrolling in managed care with care management and the lack of significant findings suggest that the effect of the telephone care management is likely to be small even if more people had remained in managed care program and received telephone care management.
Lastly, we did an analysis to examine the difference between those who remained in the intervention group and enrolled in the care management program to those who never received care management intervention. We found that the individuals who never enrolled in managed care with telephone care management used more health care services and had higher total Medicaid cost in the prior year than those who remained in the care management program (not shown). The never enrolled group had, on the average, high Medicaid costs (about $25,000 vs. $11,000) and one more chronic condition on the average (three vs. two conditions). It appears that individuals with anticipated higher use of health care services were less likely to remain in the intervention group.
Discussion
The care management intervention described in this study was intended to improve the quality of care for Colorado Medicaid's highest needs and highest cost clients by supporting the patients and PCPs. The care managers were prepared to guide the patients on medical care, as well as social services. The intervention, however, proved to be more challenging than expected and care managers had some difficulty locating and engaging individuals in services. Our study's population included a diverse group of patients with different needs. About 18 percent had at least one hospitalization and 43 percent had at least one ED visit in the year prior to the intervention. The intervention lasted 2 years and did not result in fewer hospital stays or ED visits for the intervention group.
The only significant difference between the intervention and the control group is that a higher proportion of the intervention group members had visits to nonphysician providers such as optometrists and physical therapist. The effect on nonphysician providers was mostly attributed to visits to optometrists and it could be related to our study sample including people on Medicaid because they were legally blind. This finding suggest that future research may explore whether increasing nonphysician visits for blind patients can have positive impacts on outcomes such as quality of life. There was no difference between the intervention and control group in receipt of other health services such as specialist visits, ED visits, or hospital admissions.
Although this intervention was designed according to best practices at the time it began, it did not have many of the features of the most effective coordinated care programs. In the Medicare Care Coordination Demonstration (Brown et al. 2007), for example, a comparison of programs that reduced hospital admissions and health care costs to others indicated that the most effective programs tended to have six structural and operational components: (1) they targeted patients at substantial risk of hospitalization, (2) they averaged nearly one in-person contact per month, (3) they had timely access on hospital admissions and ED use to provide transitional care, (4) care managers interacted closely with primary care providers, (5) they developed care plans, coached patients on managing their conditions, and provided social supports, and (6) they relied primarily on nurses. However, the design of our intervention called for infrequent contact between care managers and patients, and care managers carried extremely high caseloads. It could be interpreted that the lack of significant findings in our study may partly be due to the intervention that was not effectively designed.
Recent studies on telephone-based care coordination also suggest that specifically targeting individuals may be more effective. For example, a study found that telephonic intervention that used care managers to target patients with chronic illness who were overdue on refills for medication had positive impact on increasing the rate of medication re-initiation (Lawrence et al. 2008). Telephone-based postdischarge intervention for chronically ill Medicaid managed care patients was also effective in lowering 60-day hospital readmission (Kansagara et al. 2012). Another randomized trial of a telephone care management tested targeting a specific group of patients by using predictive modeling to identify those who are likely to have higher health care need in the future (Wennberg et al. 2010). Wennberg et al. (2010) found that providing more outreach and care manager contact to a targeted population resulted in reduction in total health care costs for the intervention group.
Among the high-needs subgroup, our analyses did not find any significant outcomes. The intervention did not specifically target them and the care managers had a lot of discretion in terms of where to focus their effort and a majority of their caseloads included patients with moderate to high medical costs. In fact, the care managers reported that they ended up spending most of their time with patients who fell in the middle of the group in terms of needs. These individuals had new or serious diagnoses such as diabetes, chronic heart failure, and chronic obstructive pulmonary disease. By comparison to the best practices, the care management program did not target its services toward those with a high risk of hospital admission but provided services to a broad group of individuals with diverse chronic conditions.
The findings from this study do suggest some lessons for providing care management to a high-needs population such as blind and/or disabled Medicaid beneficiaries. For example, future projects should consider structuring the intervention so that care managers have closer ties to the health care providers and the health care system to help with patient's care coordination. Although our program initially stationed some care managers in high-volume clinics, this aspect of the intervention ended early and most services were provided by telephone. Likewise, the participating managed care organization initially planned to have care managers interact with PCPs, but it did not occur consistently to assess its effectiveness. This did not occur in part because, although the health care providers had contracts to see the patients in the study, the health care providers did not work under the same health care system as the care managers. A recent Congressional Budget Office report pointed out that direct interaction with physicians and in-person interaction with patients were associated with positive impacts, such as a drop in hospital admissions and a decrease in Medicare spending (Congressional Budget Office 2012).
Given that in-person contact between care managers and patients would require a higher project cost and may not work for programs that are looking for a cost-effective alternative strategy, previous findings suggest that targeting the right population for the intervention should help to curtail cost (Lawrence et al. 2008; Wennberg et al. 2010; Kansagara et al. 2012).
Limitations
A limitation of this study is that about 26 percent of those who were assigned to the intervention group did not receive any care management. Although the study was designed to have statistical power to detect modest effects even if only half of the intervention group received services, the high opt-out rate prevented the study from detecting small effects. Our analysis also indicates that individuals who opted out of the managed care plan with care management were different from those who remained. Individuals with greater expected need for future health care services were less likely to participate in care management and more likely to opt out to other plans.
Another limitation of the study is that health care utilization data came from two different sources for much of the follow-up period, with the participating managed care plan providing information on health care use for its members and HCPF providing information for those who remained in FFS Medicaid (which included most of the control group). The two data sources may have differed systematically in the way they recorded health care use, especially because the managed care plan that provided care management received capitated payments until March 2010 rather than payments that varied with the amount of care that was provided. In addition, data were unavailable for individuals who opted out to other managed care organizations and for behavioral health care provided by behavioral health carve-outs.
Lastly, detailed information is not available about the intensity of the interaction between care managers and patients. Care managers had considerable discretion to plan appropriate treatment for their patients and their efforts varied depending on patients' individual needs. The average number of contacts differed from one patient to another, but there was no comprehensive data on number of contacts. We also do not have any measures of satisfaction or quality of services received.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by grants from the Robert Wood Johnson Foundation and the Colorado Health Foundation. All of the analysis work for this article was performed at MDRC.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Afifi A, Morisky D, Kominski G, Kotlerman J. “Impact of Disease Management on Health Care Utilization: Evidence from the ‘Florida: A Healthy State (FAHS)’ Medicaid Program”. Preventive Medicine. 2007;44(6):547–53. doi: 10.1016/j.ypmed.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. 2008. “National Healthcare Disparities Report.”. [DOI] [PubMed]
- Arora R, Boehm J, Chimento L, Moldawer L, Tsien C. Designing and Implementing Medicaid Disease and Care Management Programs: A User's Guide. Rockville, MD: Agency for Healthcare Research and Quality; 2008. (Prepared by The Lewin Group under Contract No. 290-04-0011). AHRQ Publication No. 07-0063. February 2008. [Google Scholar]
- Bell SH, Orr LL, Blomquist JD, Cain GG. Program Applicants as a Comparison Group in Evaluating Training Programs. Kalamazoo, MI: W. E. Upjohn Institute for Employment Research; 1995. [Google Scholar]
- Brown R, Peikes D, Chen A, Ng J, Schore J, Soh C. The Evaluation of the Medicare Coordinated Care Demonstration: Findings for the First Two Years. Princeton, NJ: Mathematica Policy Research, Inc; 2007. [Google Scholar]
- Centers for Medicare & Medicaid Services. 2008. “National Provider Identifier Standard (NPI)“ [accessed on November 10, 2009]. Available at http://www.cms.hhs.gov/.] [PubMed]
- Chin MH, Drum ML, Guillen M, Rimington A, Levie JR, Kirchhoff AC, Quinn MT, Schaefer CT. “Improving and Sustaining Diabetes Care in Community Health Centers with the Health Disparities Collaboratives”. Medical Care. 2007;45(12):1135–43. doi: 10.1097/MLR.0b013e31812da80e. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. 2012. “Lessons from Medicare's Demonstration Projects on Disease Management, Care Coordination, and Value-Based Payment.” Issue Brief. January.
- DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP. “A Heart Failure Self-Management Program for Patients of All Literacy Levels: A Randomized, Controlled Trial [ISRCTN11535170]”. BMC Health Services Research. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorr DA, Wilcox A, Donnelly SM, Burns L, Clayton PD. “Impact of Generalist Care Managers on Patients with Diabetes”. Health Services Research. 2005;40(5 Pt 1):1400–21. doi: 10.1111/j.1475-6773.2005.00423.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazier RH, Bajcar J, Kennie NR, Willson K. “A Systematic Review of Interventions to Improve Diabetes Care in Socially Disadvantaged Populations”. Diabetes Care. 2006;29(7):1675–88. doi: 10.2337/dc05-1942. [DOI] [PubMed] [Google Scholar]
- Gorski LA, Johnson K. “A Disease Management Program for Heart Failure: Collaboration between a Home Care Agency and a Care Management Organization”. Lippincotts Case Manag. 2003;8(6):265–73. doi: 10.1097/00129234-200311000-00009. [DOI] [PubMed] [Google Scholar]
- Handley MA, Shumway M, Schillinger D. “Cost-Effectiveness of Automated Telephone Self-Management Support with Nurse Care Management Among Patients with Diabetes”. Annals of Family Medicine. 2008;6(6):512–8. doi: 10.1370/afm.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris DE, Record NB, Gilbert-Arcari J, Bunnell S, Record SS, Norton K. “Cardiac Rehabilitation with Nurse Care Management and Telephonic Interactions at a Community Hospital: Program Evaluation of Participation and Lipid Outcomes”. Lippincotts Case Manag. 2003;8(4):141–57. doi: 10.1097/00129234-200307000-00002. quiz 58–9. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Medicaid: A Primer. Washington, DC: Kaiser Family Foundaton; 2010. [Google Scholar]
- Kansagara D, Ramsay RS, Labby D, Saha S. “Post-Discharge Intervention in Vulnerable, Chronically ill Patients”. Journal of Hospital Medicine. 2012;7(2):124–30. doi: 10.1002/jhm.941. [DOI] [PubMed] [Google Scholar]
- Kominski G, Morisky D, Afifi A, Kotlerman J. “The Effect of Disease Management on Utilization of Services by Race/Ethnicity: Evidence from the Florida Medicaid Program”. American Journal of Managed Care. 2008;14(3):168–72. [PubMed] [Google Scholar]
- Kroenke K, Theobald D, Wu J, Norton K, Morrison G, Carpenter J, Tu W. “Effect of Telecare Management on Pain and Depression in Patients with Cancer: A Randomized Trial”. Journal of American Medical Association. 2010;304(2):163–71. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronick R, Gilmer T, Dreyfus T, Lee L. “Improving Health-Based Payment for Medicaid Beneficiaries: CDPS”. Health Care Financ Rev. 2000;21(3):29–64. [PMC free article] [PubMed] [Google Scholar]
- Lawrence DB, Allison W, Chen JC, Demand M. “Improving Medication Adherence with a Targeted, Technology-Driven Disease Management Intervention”. Disease Management. 2008;11(3):141–4. doi: 10.1089/dis.2007.0013. [DOI] [PubMed] [Google Scholar]
- Mattke S, Seid M, Ma S. “Evidence for the Effect of Disease Management: Is $1 Billion a Year a Good Investment?”. American Journal of Managed Care. 2007;13(12):670–6. [PubMed] [Google Scholar]
- Michalopoulos C, Bloom HS, Hill CJ. “Can Propensity-Score Methods Match the Findings from a Random Assignment Evaluation of Mandatory Welfare-to-Work Programs?”. The Review of Economics and Statistics, MIT Press. 2004;86(1):156–79. [Google Scholar]
- Mohr DC, Vella L, Hart S, Heckman T, Simon G. “The Effect of Telephone-Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta-Analysis”. Clinical Psychology: Science and Practice. 2008;15(3):243–53. doi: 10.1111/j.1468-2850.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peikes D, Chen A, Schore J, Brown R. “Effects of Care Coordination on Hospitalization, Quality of Care, and Health Care Expenditures among Medicare Beneficiaries: 15 Randomized Trials”. Journal of American Medical Association. 2009;301(6):603–18. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- Rittenhouse DR, Robinson JC. “Improving Quality in Medicaid: The Use of Care Management Processes for Chronic Illness and Preventive Care”. Medical Care. 2006;44(1):47–54. doi: 10.1097/01.mlr.0000188992.48592.cd. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P, Rubin D. “The Central Role of the Propensity Score in Observational Studies for Causal Effects”. Biometrika. 1983;70:4155. [Google Scholar]
- Rosenman MB, Holmes AM, Ackermann RT, Murray MD, Doebbeling CC, Katz B, Li J, Zillich A, Prescott VM, Downs SM, Inui TS. “The Indiana Chronic Disease Management Program”. Milbank Quarterly. 2006;84(1):135–63. doi: 10.1111/j.1468-0009.2006.00441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sequist TD, Marshall R, Lampert S, Buechler EJ, Lee TH. “Missed Opportunities in the Primary Care Management of Early Acute Ischemic Heart Disease”. Archives of Internal Medicine. 2006;166(20):2237–43. doi: 10.1001/archinte.166.20.2237. [DOI] [PubMed] [Google Scholar]
- Sidorov J, Shull R, Tomcavage J, Girolami S, Lawton N, Harris R. “Does Diabetes Disease Management Save Money and Improve Outcomes? A Report of Simultaneous Short-Term Savings and Quality Improvement Associated with a Health Maintenance Organization-Sponsored Disease Management Program among Patients Fulfilling Health Employer Data and Information Set Criteria”. Diabetes Care. 2002;25(4):684–9. doi: 10.2337/diacare.25.4.684. [DOI] [PubMed] [Google Scholar]
- Vladeck BC. “Where the Action Really Is: Medicaid and the Disabled”. Health Affairs (Millwood) 2003;22(1):90–100. doi: 10.1377/hlthaff.22.1.90. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. “Improving Chronic Illness Care: Translating Evidence into Action”. Health Affairs (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, Petukhova MZ, Kessler RC. “Telephone Screening, Outreach, and Care Management for Depressed Workers and Impact on Clinical and Work Productivity Outcomes: A Randomized Controlled Trial”. Journal of American Medical Association. 2007;298(12):1401–11. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg DE, Marr A, Lang L, O'Malley S, Bennett G. “A Randomized Trial of a Telephone Care-Management Strategy”. New England Journal of Medicine. 2010;363(13):1245–55. doi: 10.1056/NEJMsa0902321. [DOI] [PubMed] [Google Scholar]
- Zhang N, Wan T, Rossiter L, Murawski M, Patel U. “Evaluation of Chronic Disease Management on Outcomes and Cost of Care for Medicaid Beneficiaries”. Health Policy. 2008;86(2–3):345–54. doi: 10.1016/j.healthpol.2007.11.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


