Abstract
Background
Periodontal infections are hypothesized to increase the risk of adverse systemic outcomes through inflammatory mechanisms. The magnitude of effect, if any, of anti-infective periodontal treatment on systemic inflammation is unknown, as are the patient populations most likely to benefit. We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to test the hypothesis that anti-infective periodontal treatment reduces systemic c-reactive protein (CRP).
Methods and Findings
MEDLINE, EMBASE, CENTRAL and CINAHL databases were searched using sensitivity-enhancing search terms. Eligible RCTs enrolled patients with periodontal infection, compared a clearly defined anti-infective periodontal intervention (experimental group) to an “inactive control” (no periodontal intervention) or to an “active control” (lower treatment intensity than the experimental group). Mean differences in final CRP values at the earliest post-treatment time point (typically 1-3 months) between experimental and control groups were analyzed using random-effects regression. Among 2,753 possible studies 20 were selected, which included 2,561 randomized patients(median=57). Baseline CRP values were >3.0 mg/L in 40% of trials. Among studies with a control group receiving no treatment, the mean difference in CRP final values among experimental treatment vs. control groups was -0.37 mg/L [95%CI=-0.64, -0.11], (P=0.005), favoring experimental treatment. Trials for which the experimental group received antibiotics had stronger effects (P for interaction=0.03) and the mean difference in CRP final values among experimental treatment vs. control was -0.75 mg/L [95%CI=-1.17,-0.33]. No treatment effect was observed among studies using an active treatment comparator. Treatment effects were stronger for studies that included patients with co-morbidities vs. studies that included “systemically healthy” patients, although the interaction was not significant (P=0.48).
Conclusions
Anti-infective periodontal treatment results in short-term modest reductions in systemic CRP.
Introduction
Periodontal infections have been hypothesized as a risk factor for several adverse health outcomes. Observational studies have linked periodontal infection with increased risk for developing subclinical and clinical cardiovascular disease[1–5], poor glycemic control among individuals with diabetes[6–9], increased diabetes risk[10–14], adverse pregnancy outcomes[15,16], and the development of rheumatoid arthritis[17–20].
Chronic inflammation is a potential mechanism linking periodontal infection with the aforementioned systemic inflammatory outcomes. Elevated inflammatory biomarkers, such as C-reactive protein (CRP), have been consistently shown to increase the risk for clinical outcomes such as cardiovascular disease[21,22] and type 2 diabetes[23,24]. Exposure to select microbes in dysbiotic subgingival biofilms might elicit a chronic low-grade inflammatory phenotype. Therefore, anti-infective periodontal therapies that reduce exposure to subgingival pathogenic microbes are a plausible anti-inflammatory intervention. A recent American Heart Association Scientific Statement on periodontal infections and atherosclerotic vascular disease (AVD) concluded that “periodontal interventions result in a reduction in systemic inflammation”[25] based on several randomized controlled trials (RCTs) showing reductions in inflammatory markers after periodontal treatment. The Scientific Statement also recognized that “the effects of therapy on specific inflammatory markers are not consistent across studies”[25] which is supported by the current literature including several RCTs showing either no treatment effect or increased inflammatory biomarkers after periodontal treatment. The heterogeneity observed in previous studies could arise from a number of factors including study bias, variation in treatment protocols and differences in patient characteristics/co-morbidities.
Therefore, at least three critical questions remain unanswered: i) the overall magnitude of effect, if any, of anti-infective periodontal treatment on systemic inflammation and the clinical meaningfulness of these effects; ii) whether adjunctive antibiotics result in greater reductions in inflammation; iii) and whether treatment effects are greater among patients with underlying co-morbidities. These questions are important for both future research and current clinical practice.
We have conducted a systematic review and meta-analysis of randomized controlled trials to comprehensively assess the overall evidence regarding CRP effects following anti-infective periodontal treatment. We further examined whether or not the influence of treatment on CRP levels varied according to treatment protocol or patient co-morbidities. CRP is the primary outcome in the study because it is a common surrogate of systemic inflammation and the only inflammatory outcome for which clinical recommendations exist (for patients at intermediate cardiovascular disease risk)[26].
Methods
The a priori review protocol was published with the International Prospective Register of Systematic Reviews (PROSPERO) under registration# CRD42011001775. This report complies with the preferred reporting items of PRISMA for systematic reviews and meta-analyses[27].
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials with available CRP data. There was no minimum trial duration.
Types of participants
Trials that enrolled adult patients with periodontal infection (i.e., gingivitis or periodontitis) were eligible.
Types of interventions
Eligible studies used any surgical or nonsurgical periodontal treatment with or without antibiotics or other chemical adjuncts. Scaling and root planing (SRP), a mainstay in periodontal therapy, was reported in all but one study and is defined by the American Academy of Periodontology as “a non-surgical procedure where the therapist removes plaque and calculus from the periodontal pocket and around the tooth root and smooths the root surfaces to promote healing.” Control groups were defined as
“inactive” if any of the following occurred during the same study period as the experimental group: i) there was no periodontal treatment; ii) oral hygiene instruction (OHI) was provided; iii) supragingival cleaning was performed; iv) teeth with disease so severe that treatment was not indicated were extracted. We also considered trials in which the control group received an “active” periodontal treatment with a distinctly lower treatment intensity than the experimental group, e.g., SRP + antibiotic treatment in the experimental group vs. SRP alone in the control group. Referral to “community periodontal care” was considered an active treatment protocol.
Types of outcome measures
The primary outcome was the CRP level after periodontal treatment because it is commonly studied as an inflammatory outcome in periodontal treatment studies and also has clinical utility[26]. The primary outcome was based on the CRP measurement at the shortest duration from treatment completion, with the requirement that at least two weeks separated treatment completion and post-treatment CRP measurement. In a secondary analysis, we considered the CRP level at 3-month follow-up, as it was the most frequently reported post-treatment time point assessed. Secondary outcomes included the local clinical measures of inflammation, bleeding on probing and probing depth, which serve as markers of anti-infective treatment success.
Search methods for identification of studies
We searched Pubmed/MEDLINE (up to February 6th, 2013) and the Cochrane Oral Health Group Specialized Register, EMBASE, CENTRAL and CINAHL(up to March 2012). There was no date restriction but only publications in the English language were reviewed. The search equation for MEDLINE is reported in Table S1 in File S1. In addition we searched the references of all identified studies for more trials as well as the conference proceedings from the three most recent years of the two main meetings for the following specialties: dentistry, cardiology, obstetrics, neurology, endocrinology, rheumatology. We also searched the WHO international clinical trials register platform.
Data collection
Selection of studies
Two independent reviewers blinded to the results of the other reviewer first screened all records at the title level. To enhance sensitivity, records were only removed if both reviewers excluded at the title level. The second level of review was at the abstract level followed by another round of review at the full-text level.
Data extraction and management
Two independent reviewers (in duplicate) abstracted data using a standardized form. When there was disagreement it was resolved by discussion with a third review author. There were no discrepancies in the determination of CRP outcome values or bias assessments. Corresponding authors were contacted via e-mail at least three times to obtain data if the CRP outcomes could not be readily abstracted from the publication.
Assessment of risk of bias in selected trials
Two reviewers independently assessed risk of bias using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions[28]. Risk of bias was rated as low, high or unclear regarding: i) sequence generation; ii) allocation concealment; iii) blinding; and iv) completeness of outcome data.
Data synthesis
Measure of treatment effect and meta-analyses
For the primary outcome - CRP values at the earliest time point after treatment completion - we measured the treatment effect using mean difference (MD) in final values between the experimental and control groups. Negative values favor experimental group over control group. For the secondary outcomes - bleeding on probing (as a percentage) and probing depth in millimeters (mm) - the treatment effect was measured using mean differences in final values between the experimental and control groups. Trials with multiple experimental groups were included separately using a shared control group divided out approximately evenly among the comparisons. Because of the expected clinical diversity, meta-analyses were performed by using DerSimonian and Laird random-effects models. To assess heterogeneity across trials, we used forest plots as well as Cochran’s heterogeneity statistics and Higgins I2 coefficients. We produced funnel plots to assess small-study effects.
Active-inactive trials and active-active trials were synthesized separately. We repeated all syntheses with the measurements at 3-month follow-up. The same methods were used to synthesize data regarding bleeding on probing and probing depth.
Sensitivity analyses
To incorporate potential differences in baseline values within or between trials, we also analyzed change scores. For the analysis of change scores, the within-group correlation coefficient (ρ) between baseline and final values is required but was never reported. We requested, and were provided with, the original CRP data from the largest trial included in this meta-analysis[29]. Among the 620 participants from that trial, the correlation between pre- and post-treatment raw CRP values was 0.43 and the correlation between log-transformed values was 0.64. We performed a sensitivity analysis using a variety of values for ρ (0, 0.25, 0.5 and 0.75). As results were very similar and based on correlations observed in the original data provided by Michalowicz et al. [29], we report the results for ρ=0.5. We also performed a meta-regression analysis of final CRP values regressed on baseline CRP values and intervention status.
To account for the potentially skewed distribution of CRP, we performed a sensitivity analysis by transforming the data to the logarithmic scale[30]. The meta-analysis of data on the logarithmic scale gave similar results; thus we chose to present the non log transformed results to simplify interpretation.
To account for incomplete outcome data, we performed sensitivity analyses by imputing missing outcome data. First, we conservatively assumed that the mean CRP final value among patients with missing outcome data in the experimental group was 10% larger than observed for complete cases in the experimental group and that mean CRP final values among controls with missing data were 10% lower[31]. Second, we assumed that the mean CRP final value in participants with missing outcome data was equal to that in complete cases in the control group.
Subgroup analyses
We performed two subgroup analyses based on the use of antibiotics (periodontal interventions that included antibiotics vs. those that did not), and on the presence of comorbidities (healthy patients vs. patients with type 2 diabetes vs. patients with other comorbidities). Interaction tests were performed through meta-regression models.
All analysis were done using Stata MP version 11.0.
Results
Description of studies
Results of the search
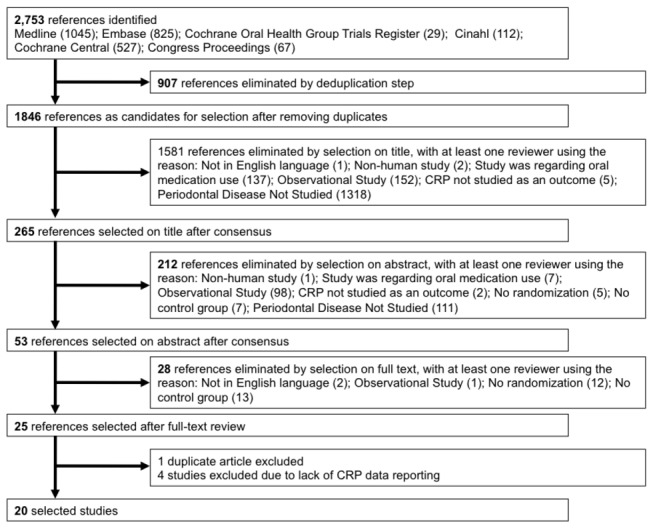
Among the initial 2,753 records identified, 53 articles were reviewed at the full-text level and 25 were eligible (Figure 1). Among those, we could not exclude the possibility that two papers included a group of patients common to both studies arising from one three-arm trial[32,33]; we selected the original report[32] as the subsequent publication reported results for two arms only. Among the 24 trials, appropriate CRP data could not be abstracted from 8 trials (typically because data were presented graphically and not numerically). The corresponding and/or first authors from these 8 trials were contacted and we obtained CRP data for 4 out of 8 trials, yielding a total of 20[29,32,34–51] included trials.
Figure 1. Study selection flow diagram.
Characteristics of included trials and interventions
Characteristics of included trials and interventions are summarized in Table 1 and in Tables S1-S2 in File S1. All but 3 trials were single-center trials. The 20 included trials were conducted across 14 different countries and 5 continents.
Table 1. Descriptive characteristics of 20 selected trials.
| Trial size* | 57 [12-796] |
|---|---|
| Comparisons | # of trials |
| Active periodontal treatment versus inactive control | 18 randomized comparisons (16 trials) |
| 1. SRP versus no treatment | 4 [32,38,48] |
| 2. OHI+SRP versus no treatment | 6 [29,34,35,39,41,47] |
| 3. OHI+SRP versus OHI | 2 [44,49] |
| 4. SRP+antibiotics versus no treatment | 2 [32,45] |
| 5. OHI+SRP+antibiotics versus no treatment | 3 [40,43,46] |
| 6. OHI+SRP+antibiotics versus OHI | 1 [36] |
| Active periodontal treatment versus active treatment but with a lower intensity | 6 randomized comparisons (6 trials) |
| 1. Intensive SRP versus SRP | 1 [48] |
| 2. OHI+SRP vs. community care | 1 [37] |
| 3. SRP+antibiotic versus SRP | 1 [32] |
| 4. OHI+SRP+antibiotics versus OHI+SRP | 3 [42,50,51] |
| Patient characteristics | |
| Age, years† | 44 [26-60] |
| Female sex† | 54% [15%-100%] |
| Comorbities/conditions | |
| Healthy | 5 |
| Pregnant | 2 |
| Diabetes | 7 |
| Other comorbidities | 6 |
| Baseline PD, mm† | 3.4 [2.1-5.1] |
| Baseline % of periodontal sites with BOP† | 54% [32.5-70.5] |
| Baseline CRP, mg/L† | 3.1[0.8- 9.3] |
BOP: Bleeding on probe; PD: Probing depth; SRP: Scaling and root planning;
Baseline PD, BOP and CRP values were not reported in 9, 5 and 1 trials, respectively
Median [min-max]
Overall mean [min-max mean values] across trials
Among the 20 selected trials, 18 were two-arm trials and 2 were three-arm trials. Among the three-arm trials, one compared SRP+antibiotics versus SRP versus no treatment, the other compared SRP at baseline and 3 months versus SRP at baseline only versus no treatment. Overall, there were 18 randomized comparisons between an active periodontal treatment and an “inactive” control group (no periodontal treatment, OHI or supragingival cleaning) and 6 randomized comparisons of an active periodontal treatment to an “active” control but with lower treatment intensity(Table 1 and Table S3 in File S1). The 4 excluded studies[52–55] (because CRP data could not be obtained) addressed comparisons of an active periodontal treatment to an active control with lower treatment intensity.
Characteristics of patients
The 20 selected studies included 2,561 randomized patients. The median trial size was 57 patients. All patients were adults between the ages of 26 and 60 years, with an overall mean age of 44 years; the two studies with the lowest mean patient ages enrolled pregnant women. Both genders were well represented (Table 1). Patients were frequently enrolled based on the presence of co-morbidities or pregnancy, 7 studies enrolled patients with pre-diabetes or diabetes mellitus, 6 studies enrolled patients with a variety of other co-morbidities and 2 studies enrolled pregnant women (Table 1).
All patients had periodontitis although the definitions used for inclusion varied greatly. All but two studies[45,48] required clinical evidence of current periodontal inflammation
(i.e., multiple sites with either bleeding on probing (BOP) or probing depths (PD) ≥4 mm). At baseline, the overall mean values of PD and % of periodontal sites with BOP were 3.4 mm and 54% across all studies, respectively. The median CRP value at baseline was 3.1 mg/L and 90% and 40% of study populations had a mean CRP level of ≥1.0 mg/L or >3.0 mg/L, respectively.
Risk of bias of included trials
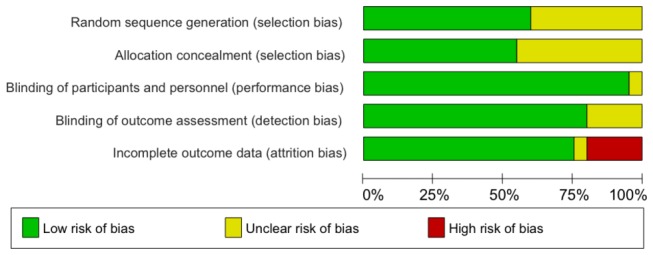
Overall, 10 trials had a low risk of selection bias as the sequence of generation and allocation concealment were adequate (Figure 2 and Figure S1 in File S1); in the remaining 10 trials, the risk of bias was unclear because it was not explicitly described whether sequence generation and/or allocation concealment was adequately done. Of note, 3 trials used an unequal randomization ratio of 2:1[34,36,47]. Protection against performance and detection biases was adequate as participants, personnel and outcome assessment (CRP level is objectively measured) were blinded. However, there was high risk of attrition bias in 4 trials because the proportion of patients with missing outcome data was substantial, ranging from 22% to 51%, with imbalances between the experimental and control group in 2 trials.
Figure 2. Risk of bias graph.
Efficacy of active periodontal treatment versus inactive control on systemic CRP
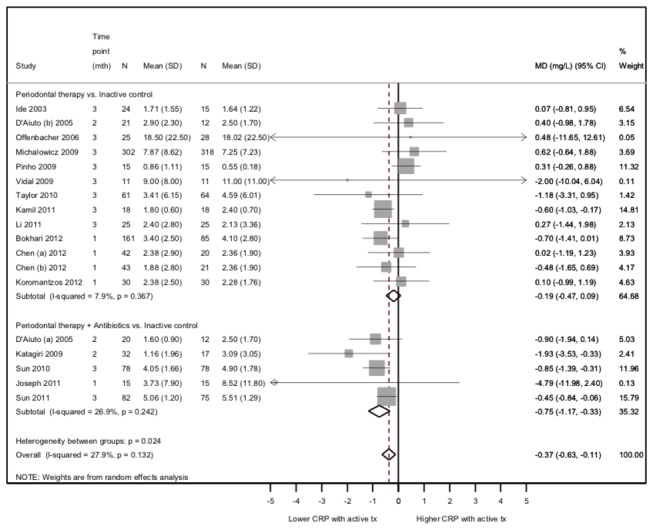
Overall, 16 trials contributed to 18 randomized comparisons between an active periodontal treatment, with or without antibiotics, and an inactive control group. The meta-analysis showed that final CRP values (earliest follow-up time point) were significantly lower, on average, in the active periodontal group than in the inactive control group (combined MD=-0.37 mg/L, 95%CI=-0.64 to -0.11, P=0.005, Figure 3). Statistical heterogeneity was moderate (Cochran’s heterogeneity test P=0.10; I2 coefficient=32%).
Figure 3. Efficacy of active periodontal therapy versus inactive control on post-treatment CRP values.
The meta-analysis of change scores yielded stronger results (combined MD=-1.50, 95%CI=-2.11 to -0.89, P<0.001, Figure S2 in File S1), although heterogeneity was considerable. The meta-regression analysis also showed that the mean final CRP values were strongly positively associated with mean pre-treatment values, but were lower after active periodontal treatment than inactive control (mean difference in final CRP values between active periodontal treatment and inactive control, adjusted for mean baseline CRP values=-0.34 mg/L (95%CI=-0.60 to -0.10), P=0.006, Figure S3 in File S1).
A reanalysis following imputation of missing outcome data indicated that our results were robust for the 2 hypotheses considered (Figures S4-S5 in File S1). Results were also consistent when only considering studies that reported CRP outcomes at 3 months (Figure S6 in File S1).
Subgroup Analysis
Among studies using untreated control groups, the difference in final CRP values was larger for experimental groups receiving adjunctive antibiotics (combined MD=-0.75, 95%CI=-1.17 to -0.33, with low heterogeneity) than for groups without antibiotics (combined MD=-0.19, 95%CI=-0.47 to 0.09, with low heterogeneity; P for interaction=0.03; Figure 3). Among studies with an active comparator, only 3 of 6 trials compare periodontal therapy+antibiotics to periodontal therapy alone[50,51,56] and these results show no evidence that antibiotic therapy provides stronger reductions in CRP. However, there is considerable heterogeneity between study.
The difference in final CRP values between active periodontal treatment and inactive control was larger in patients with diabetes or another comorbidity than in healthy patients (two of which included only pregnant women), although there was no statistically significant interaction (P=0.32; Figure S7 in File S1).
Funnel plots did not show evidence of small-study bias (Figure S8 in File S1).
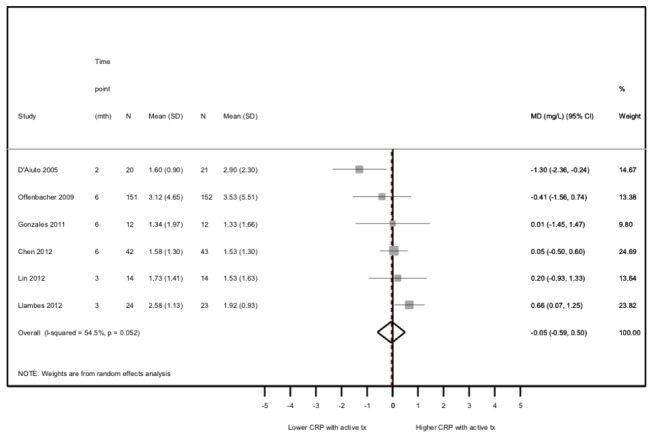
Efficacy of active periodontal treatment versus active control on systemic CRP
Overall, 6 trials contributed to comparisons between an active periodontal treatment and an active control group but with lower intensity (totaling 527 patients). The meta-analysis showed that, on average, final CRP values (earliest follow-up time point) did not differ between the two (combined MD=-0.05, 95%CI=-0.59,0.50; Figure 4), with moderate statistical heterogeneity (Cochran’s heterogeneity test P=0.05; I2 coefficient=55%). Among the 4 studies excluded because CRP data were not obtained[52–55], 362 patients were enrolled; one showed greater CRP reductions in the experimental group, three showed greater reductions in the control group but none reported statistically significant CRP treatment effects.
Figure 4. Efficacy of active periodontal therapy versus active control on post-treatment CRP values.
Efficacy of experimental interventions on periodontal inflammation
Among studies reporting BOP outcomes, treatment reduced absolute BOP values by 20% on average (P<0.05; substantial heterogeneity across trials); when considering both the earliest post-intervention time point or a 3-month time point, results were notably stronger for designs using an inactive control (Figure S9 in File S1). Similarly, mean probing depth values decreased by 0.61 mm more, on average, among treated than control groups (P<0.05; substantial heterogeneity across trials) although the effect of treatment was stronger and only statistically significant for studies without an active treatment comparator (Figure S10 in File S1).
Discussion
We have found that anti-infective periodontal treatment reduces post-treatment systemic CRP values by ~0.4 mg/L, among adult men and women. When considering periodontal interventions that included antibiotics, as compared to untreated control groups, the CRP reductions were 0.75 mg/L, although greater CRP reductions were not observed in studies using active comparators. There was also evidence to suggest that anti-infective treatment resulted in greater CRP reductions among individuals with comorbidities such as diabetes mellitus as compared to CRP reductions observed in studies enrolling apparently healthy patients although the interaction was not statistically significant.
The finding that anti-infective periodontal treatment reduces levels of an established systemic inflammatory biomarker strengthens the hypothesis that adverse exposure to microbes in dysbiotic periodontal biofilms contribute to chronic systemic inflammation. Accordingly, the current findings further strengthen the hypothesis that periodontal infections may independently contribute to the development of chronic diseases such as diabetes and cardiovascular disease since inflammation is a commonly cited biological mechanism underlying these associations[4,57].
To our knowledge, the only recommendation for use of CRP in clinical and/or public health practice was published by a joint American Heart Association (AHA)/Centers for Disease Control (CDC) working group[26]. The working group endorsed the optional use of hs-CRP in primary prevention settings to identify “patients at intermediate risk (eg, 10% to 20% risk of coronary heart disease over 10 years), in whom the physician may need additional information to guide considerations of further evaluation”.
While it is not known whether the magnitude of CRP reductions associated with periodontal intervention in this meta-analysis can reduce clinical cardiovascular outcomes, results from two trials published subsequent to the AHA/CDC statement have demonstrated that statin therapies which reduced clinical cardiovascular outcomes also lowered CRP. In the Justification for the Use of Statins in Prevention (JUPITER) trial, patients without an LDL-cholesterol indication for statin treatment randomized to Rosuvastatin realized a reduction in median CRP values that were 1.2 mg/L greater than patients randomized to placebo. This translated into a 44% reduction in incident clinical cardiovascular events after 12 months[58]. Similarly, the Pravastatin or Atorvastatin Evaluation and Infection Therapy- Thrombolysis in Myocardial Infarction 22 (PROVE IT–TIMI 22) study[59] reported that after treatment with 40 mg of pravastatin vs. 80 mg of atorvastatin CRP levels were reduced 0.7 and 0.8 mg/L after 30 days and four months, respectively, and that these declines resulted in CVD event rate reductions equivalent to what was observed for patients who achieved LDL-cholesterol treatment goals. Therefore, CRP reductions associated with anti-infective periodontal treatment in this meta-analysis are of a similar magnitude as CRP reductions that have been associated with reduced clinical CVD event rates.
In the context of primary diabetes prevention, we are unaware of trials that have investigated CRP reduction for the prevention of diabetes development. However, high-quality observational data from the Women’s Health Study offer some insights. Pradhan et al. reported that during a four-year follow up period, elevated baseline CRP was associated with a 30% increase in the risk for incident diabetes when comparing participants in the second vs. first quartile of CRP, which corresponded to a difference in median CRP values of 1.2 mg/L[23]. Elevated CRP has been recently shown in a systematic review and meta-analysis to be associated with an ~30% increase in the risk of diabetes development[60]. The results were based on ten prospective studies including >19,000 participants and >4,000 diabetes cases.
From a secondary diabetes prevention standpoint, there is evidence from randomized controlled trials that anti-infective periodontal treatment improves glycemic control among patients with diabetes[61] and the current findings offer insights as to the possible biological mechanisms underlying those findings. Of note, in accordance with our current results, periodontal treatment trials targeting glycemic control among diabetics have also demonstrated stronger treatment effects when antibiotics are used[61].
If anti-infective periodontal treatment can be demonstrated to not only reduce systemic inflammation but also prevent adverse chronic disease outcomes it would be of high public health and clinical importance for at least two reasons. First, periodontal interventions have been shown to be safe[62,63] and often do not require pharmacological agents thus reducing the potential for adverse events and offering new treatment options for individuals with contraindications for anti-inflammatory medications such as statins or aspirin. The fact that recent evidence suggests a very modest increase in diabetes risk among statin users[64] is also a reason to possibly consider alternate anti-inflammatory treatment modalities among patients at intermediate CVD risk[26]. Moreover, because periodontal treatment is necessary for the maintenance of good oral health among patients with periodontitis, referring patients for periodontal evaluation, and possible treatment, is a reasonable first step in managing inflammatory burden among at risk patients.
Beyond their clinical and public health implications, the current findings also offer some useful insights for future research endeavors that are necessary to test whether or not anti-infective periodontal treatment can prevent the development of clinical outcomes such as diabetes and cardiovascular disease. Studies using “active control” groups that receive a lower intensity treatment regimen than the experiment treatment failed to demonstrate CRP reductions. This was possibly the result of small differences in realized levels of exposure to adverse microbial species (the treatment target) between groups that each received periodontal therapy. This notion is supported by the fact that designs using “low-intensity” treatments protocols in the control arm also reported much weaker reductions in clinical periodontal outcomes (i.e., probing depth and bleeding on probing). Consequently, future trials may need to be optimized via innovative designs that allow for an untreated control group so long as appropriate data safety and monitoring plans are in place to ensure patient safety.
Two previous meta-analyses have been published regarding the contribution of periodontal infection to systemic inflammation[65,66]. While these reports were informative they were limited in a few important ways. Ioannidou et al. reported a mean difference of CRP change between experimental and control groups from only two studies[32,67] one of which was not an RCT and post-treatment CRP was assessed on the same day[67]. In a second meta-analysis, Paraskevas et al. concluded that periodontal treatment significantly reduced CRP levels although only two studies[56,68] were included in the analysis that yielded a statistically significant 0.5 mg/L CRP reduction and neither of these two studies were randomized controlled trials.
The majority of studies identified in this review enrolled patients with mean CRP levels below the high risk AHA/CDC category (3.0 mg/L) which might have impacted the strength of findings since a certain threshold of inflammation might be necessary before anti-infective/inflammatory treatments can be useful[21]. However, the results demonstrate that CRP reductions were realized regardless of baseline CRP levels suggesting that anti-infective treatments can reduce inflammation even among participants with CRP<3.0 mg/L.
As with any meta-analysis, we cannot rule out the possibility that exclusion of unpublished trials or lack of data access and loss-to-follow-up among published trials might have biased our results towards a positive finding. The fact that there was no evidence of publication bias in addition to the consistent results showing treatment benefit arising from conservative sensitivity analyses substantially mitigates these concerns. Our attempts to obtain original data from studies for which results could not be abstracted also minimize the potential for bias. Another possible bias in this research area is the difficulty in using placebo controlled double-blind studies, which could result in overestimates of treatment effects. For example, patients who know they are receiving treatment might be more motivated to make other lifestyle changes (smoking cessation, dietary changes etc.) that could influence inflammatory outcomes.
We observed evidence of heterogeneity in treatment effects across studies which might be accounted for by a number of factors such as severity of baseline infection or CRP levels, different underlying patient co-morbidities or medications, or variation in treatment modalities. In regard to the latter, it is notable that heterogeneity was minimized when analyzing subgroups with more homogenous treatment protocols (e.g., periodontal treatment + antibiotics vs. control groups without any treatment).
Anti-infective periodontal therapy among adult men and women with periodontitis results in modest short-term systemic CRP reductions based on results from 20 randomized controlled trials conducted in 14 different countries across 5 continents. Whether or not these CRP reductions can translate into decreased rates of clinical cardiovascular disease or diabetes development remains to be determined in future clinical trials as no such trial has been conducted to date. Until such trials are performed, the evidence suggests that among patients with periodontal infection, periodontal treatment can confer the dual advantage of improved oral health and short-term reduction in systemic inflammatory activity.
Supporting Information
(DOC)
(DOCX)
Acknowledgments
We thank the OPT study team, and Dr. Jim Hodges in particular, for their collaborative spirit in providing the patient-level data for the largest intervention study included in this meta-analysis. We also thank all authors who responded to our queries and provided data clarifications; specifically, Drs. Jose Gonzales, Mark Ide, Sayaka Katagiri, Panagiotis Koromantzos, Hsein-Kun Lu, Joerg Meyle, and Karl Schenck
Funding Statement
This research was supported by NIH grants R00 DE-018739 (Dr. Demmer) and R01 DE-13094 (Dr. Desvarieux). Additional funding support was provided by a Calderone Research Award from the Mailman School of Public Health, Columbia University (Dr. Demmer); a Pilot & Feasibility Award from the Diabetes and Endocrinology Research Center, College of Physicians and Surgeons, Columbia University (Dr. Demmer); a Chair in Chronic Disease, École des Hautes Études en Santé Publique, France (Dr. Desvarieux). No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM (1993) Dental disease and risk of coronary heart disease and mortality. BMJ 306: 688-691. doi: 10.1136/bmj.306.6879.688. PubMed: 8471920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner KL et al. (2000) Periodontal disease and risk of cerebrovascular disease: the first national health and nutrition examination survey and its follow-up study. Arch Intern Med 160: 2749-2755. doi: 10.1001/archinte.160.18.2749. PubMed: 11025784. [DOI] [PubMed] [Google Scholar]
- 3. Desvarieux M, Demmer RT, Rundek T, Boden-Albala B, Jacobs DR Jr. et al. (2005) Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation 111: 576-582. doi: 10.1161/01.CIR.0000154582.37101.15. PubMed: 15699278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Demmer RT, Desvarieux M (2006) Periodontal infections and cardiovascular disease: The heart of the matter. J Am Dent Assoc 137 Suppl: 14S-20S. PubMed: 17012731. [DOI] [PubMed] [Google Scholar]
- 5. Desvarieux M, Demmer RT, Jacobs DR Jr., Rundek T, Boden-Albala B et al. (2010) Periodontal bacteria and hypertension: the oral infections and vascular disease epidemiology study (INVEST). J Hypertens 28: 1413-1421. doi: 10.1097/HJH.0b013e328338cd36. PubMed: 20453665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Taylor GW, Burt BA, Becker MP, Genco RJ, Shlossman M (1998) Glycemic control and alveolar bone loss progression in type 2 diabetes. Ann Periodontol 3: 30-39. doi: 10.1902/annals.1998.3.1.30. PubMed: 9722688. [DOI] [PubMed] [Google Scholar]
- 7. Taylor GW (2001) Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol 6: 99-112. doi: 10.1902/annals.2001.6.1.99. PubMed: 11887478. [DOI] [PubMed] [Google Scholar]
- 8. Janket SJ, Baird AE, Chuang SK, Jones JA (2003) Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95: 559-569. doi: 10.1067/moe.2003.107. PubMed: 12738947. [DOI] [PubMed] [Google Scholar]
- 9. Mealey BL (2006) Periodontal disease and diabetes. A two-way street. J Am Dent Assoc 137 Suppl: 26S-31S. PubMed: 17012733. [DOI] [PubMed] [Google Scholar]
- 10. Saito T, Shimazaki Y, Kiyohara Y, Kato I, Kubo M et al. (2004) The severity of periodontal disease is associated with the development of glucose intolerance in non-diabetics: the Hisayama study. J Dent Res 83: 485-490. doi: 10.1177/154405910408300610. PubMed: 15153457. [DOI] [PubMed] [Google Scholar]
- 11. Demmer RT, Jacobs DR Jr., Desvarieux M (2008) Periodontal disease and incident type 2 diabetes: results from the First National Health and Nutrition Examination Survey and its epidemiologic follow-up study. Diabetes Care 31: 1373-1379. doi: 10.2337/dc08-0026. PubMed: 18390797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Demmer RT, Desvarieux M, Holtfreter B, Jacobs DR Jr., Wallaschofski H et al. (2010) Periodontal status and A1C change: longitudinal results from the study of health in Pomerania (SHIP). Diabetes Care 33: 1037-1043. doi: 10.2337/dc09-1778. PubMed: 20185742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Choi YH, McKeown RE, Mayer-Davis EJ, Liese AD, Song KB et al. (2011) Association between periodontitis and impaired fasting glucose and diabetes. Diabetes Care 34: 381-386. doi: 10.2337/dc10-1354. PubMed: 21216848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Demmer RT, Squillaro A, Papapanou PN, Rosenbaum M, Friedewald WT et al. (2012) Periodontal Infection, Systemic Inflammation, and Insulin Resistance: Results from the Continuous National Health and Nutrition Examination Survey (NHANES) 1999-2004. Diabetes Care, 35: 2235–42. PubMed: 22837370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vergnes JN, Sixou M (2007) Preterm low birth weight and maternal periodontal status: a meta-analysis. Am J Obstet Gynecol 196:135: e1-e7. PubMed: 17306654. [DOI] [PubMed] [Google Scholar]
- 16. Conde-Agudelo A, Villar J, Lindheimer M (2008) Maternal infection and risk of preeclampsia: systematic review and metaanalysis. Am J Obstet Gynecol 198: 7-22. doi: 10.1016/j.ajog.2007.07.040. PubMed: 18166297. [DOI] [PubMed] [Google Scholar]
- 17. Al-Katma MK, Bissada NF, Bordeaux JM, Sue J, Askari AD (2007) Control of periodontal infection reduces the severity of active rheumatoid arthritis. J Clin Rheumatol 13: 134-137. doi: 10.1097/RHU.0b013e3180690616. PubMed: 17551378. [DOI] [PubMed] [Google Scholar]
- 18. de Pablo P, Dietrich T, McAlindon TE (2008) Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J Rheumatol 35: 70-76. PubMed: 18050377. [PubMed] [Google Scholar]
- 19. Ortiz P, Bissada NF, Palomo L, Han YW, Al-Zahrani MS et al. (2009) Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors. J Periodontol 80: 535-540. doi: 10.1902/jop.2009.080447. PubMed: 19335072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Demmer RT, Molitor JA, Jacobs DR Jr., Michalowicz BS (2011) Periodontal Disease, Tooth Loss and Incident Rheumatoid Arthritis: Results from the First National Health and Nutrition Examination Survey and its epidemiological follow-up study. J Clin Periodontol 38: 998-1006. doi: 10.1111/j.1600-051X.2011.01776.x. PubMed: 22092471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH (1997) Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. [see comments]. [erratum appears in N Engl J Med 1997 Jul 31;337(5):356]. N Engl J Med 336: 973-979. doi: 10.1056/NEJM199704033361401. PubMed: 9077376. [DOI] [PubMed] [Google Scholar]
- 22. Ridker PM, Hennekens CH, Buring JE, Rifai N (2000) C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 342: 836-843. doi: 10.1056/NEJM200003233421202. PubMed: 10733371. [DOI] [PubMed] [Google Scholar]
- 23. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM (2001) C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 286: 327-334. doi: 10.1001/jama.286.3.327. PubMed: 11466099. [DOI] [PubMed] [Google Scholar]
- 24. Hu FB, Meigs JB, Li TY, Rifai N, Manson JE (2004) Inflammatory markers and risk of developing type 2 diabetes in women. Diabetes 53: 693-700. doi: 10.2337/diabetes.53.3.693. PubMed: 14988254. [DOI] [PubMed] [Google Scholar]
- 25. Lockhart PB, Bolger AF, Papapanou PN, Osinbowale O, Trevisan M et al. (2012) Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association?: a scientific statement from the American Heart Association. Circulation 125: 2520-2544. doi: 10.1161/CIR.0b013e31825719f3. PubMed: 22514251. [DOI] [PubMed] [Google Scholar]
- 26. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd et al. (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107: 499-511. doi: 10.1161/01.CIR.0000052939.59093.45. PubMed: 12551878. [DOI] [PubMed] [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264-269, W64 doi: 10.7326/0003-4819-151-4-200908180-00135. PubMed: 19622511. [DOI] [PubMed] [Google Scholar]
- 28. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D et al. (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343: d5928. doi: 10.1136/bmj.d5928. PubMed: 22008217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Michalowicz BS, Novak MJ, Hodges JS, DiAngelis A, Buchanan W et al. (2009) Serum inflammatory mediators in pregnancy: changes after periodontal treatment and association with pregnancy outcomes. J Periodontol 80: 1731-1741. doi: 10.1902/jop.2009.090236. PubMed: 19905943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Higgins JP, White IR, Anzures-Cabrera J (2008) Meta-analysis of skewed data: combining results reported on log-transformed or raw scales. Statist Med 27: 6072-6092. doi: 10.1002/sim.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Higgins JGS (2011) Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 The Cochrane Collaboration, 2011.
- 32. D'Aiuto F, Nibali L, Parkar M, Suvan J, Tonetti MS (2005) Short-term effects of intensive periodontal therapy on serum inflammatory markers and cholesterol. J Dent Res 84: 269-273. doi: 10.1177/154405910508400312. PubMed: 15723869. [DOI] [PubMed] [Google Scholar]
- 33. D'Aiuto F, Parkar M, Nibali L, Suvan J, Lessem J et al. (2006) Periodontal infections cause changes in traditional and novel cardiovascular risk factors: results from a randomized controlled clinical trial. Am Heart J 151: 977-984. doi: 10.1016/j.ahj.2005.06.018. PubMed: 16644317. [DOI] [PubMed] [Google Scholar]
- 34. Ide M, McPartlin D, Coward PY, Crook M, Lumb P et al. (2003) Effect of treatment of chronic periodontitis on levels of serum markers of acute-phase inflammatory and vascular responses. J Clin Periodontol 30: 334-340. doi: 10.1034/j.1600-051X.2003.00282.x. PubMed: 12694432. [DOI] [PubMed] [Google Scholar]
- 35. Offenbacher S, Lin D, Strauss R, McKaig R, Irving J et al. (2006) Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: a pilot study. J Periodontol 77: 2011-2024. doi: 10.1902/jop.2006.060047. PubMed: 17209786. [DOI] [PubMed] [Google Scholar]
- 36. Katagiri S, Nitta H, Nagasawa T, Uchimura I, Izumiyama H et al. (2009) Multi-center intervention study on glycohemoglobin (HbA1c) and serum, high-sensitivity CRP (hs-CRP) after local anti-infectious periodontal treatment in type 2 diabetic patients with periodontal disease. Diabetes Res Clin Practice 83: 308-315. doi: 10.1016/j.diabres.2008.10.016. PubMed: 19168253. [DOI] [PubMed] [Google Scholar]
- 37. Offenbacher S, Beck JD, Moss K, Mendoza L, Paquette DW et al. (2009) Results from the Periodontitis and Vascular Events (PAVE) Study: a pilot multicentered, randomized, controlled trial to study effects of periodontal therapy in a secondary prevention model of cardiovascular disease. J Periodontol 80: 190-201. doi: 10.1902/jop.2009.080007. PubMed: 19186958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pinho Mde N, Oliveira RD, Novaes AB Jr., Voltarelli JC (2009) Relationship between periodontitis and rheumatoid arthritis and the effect of non-surgical periodontal treatment. Braz Dent J 20: 355-364. PubMed: 20126902. [DOI] [PubMed] [Google Scholar]
- 39. Vidal F, Figueredo CM, Cordovil I, Fischer RG (2009) Periodontal therapy reduces plasma levels of interleukin-6, C-reactive protein, and fibrinogen in patients with severe periodontitis and refractory arterial hypertension. J Periodontol 80: 786-791. doi: 10.1902/jop.2009.080471. PubMed: 19405832. [DOI] [PubMed] [Google Scholar]
- 40. Sun WL, Chen LL, Zhang SZ, Ren YZ, Qin GM (2010) Changes of adiponectin and inflammatory cytokines after periodontal intervention in type 2 diabetes patients with periodontitis. Arch Oral Biol 55: 970-974. doi: 10.1016/j.archoralbio.2010.08.001. PubMed: 20889139. [DOI] [PubMed] [Google Scholar]
- 41. Taylor B, Tofler G, Morel-Kopp MC, Carey H, Carter T et al. (2010) The effect of initial treatment of periodontitis on systemic markers of inflammation and cardiovascular risk: a randomized controlled trial. Eur J Oral Sci 118: 350-356. doi: 10.1111/j.1600-0722.2010.00748.x. PubMed: 20662907. [DOI] [PubMed] [Google Scholar]
- 42. Gonzales JR, Harnack L, Schmitt-Corsitto G, Boedeker RH, Chakraborty T et al. (2011) A novel approach to the use of subgingival controlled-release chlorhexidine delivery in chronic periodontitis: a randomized clinical trial. J Periodontol 82: 1131-1139. doi: 10.1902/jop.2011.100287. PubMed: 21491990. [DOI] [PubMed] [Google Scholar]
- 43. Joseph R, Narayan V, Krishnan R, Melemadathil S (2011) Non-surgical periodontal therapy improves serum levels of C-reactive protein and edematous states in female patients with idiopathic edema. J Periodontol 82: 201-209. doi: 10.1902/jop.2010.100258. PubMed: 20681817. [DOI] [PubMed] [Google Scholar]
- 44. Kamil W, Al Habashneh R, Khader Y, Al Bayati L, Taani D (2011) Effects of nonsurgical periodontal therapy on C-reactive protein and serum lipids in Jordanian adults with advanced periodontitis. J Periodontal Res 46: 616-621. PubMed: 21631509. [DOI] [PubMed] [Google Scholar]
- 45. Li X, Tse HF, Yiu KH, Li LS, Jin L (2011) Effect of periodontal treatment on circulating CD34(+) cells and peripheral vascular endothelial function: a randomized controlled trial. J Clin Periodontol 38: 148-156. doi: 10.1111/j.1600-051X.2010.01651.x. PubMed: 21133981. [DOI] [PubMed] [Google Scholar]
- 46. Sun WL, Chen LL, Zhang SZ, Wu YM, Ren YZ et al. (2011) Inflammatory cytokines, adiponectin, insulin resistance and metabolic control after periodontal intervention in patients with type 2 diabetes and chronic periodontitis. Intern Med 50: 1569-1574. doi: 10.2169/internalmedicine.50.5166. PubMed: 21804283. [DOI] [PubMed] [Google Scholar]
- 47. Bokhari SA, Khan AA, Butt AK, Azhar M, Hanif M et al. (2012) Non-surgical periodontal therapy reduces coronary heart disease risk markers: a randomized controlled trial. J Clin Periodontol 39: 1065-1074. doi: 10.1111/j.1600-051X.2012.01942.x. PubMed: 22966824. [DOI] [PubMed] [Google Scholar]
- 48. Chen L, Luo G, Xuan D, Wei B, Liu F et al. (2012) Effects of non-surgical periodontal treatment on clinical response, serum inflammatory parameters, and metabolic control in patients with type 2 diabetes: a randomized study. J Periodontol 83: 435-443. doi: 10.1902/jop.2011.110327. PubMed: 21859323. [DOI] [PubMed] [Google Scholar]
- 49. Koromantzos PA, Makrilakis K, Dereka X, Offenbacher S, Katsilambros N et al. (2012) Effect of non-surgical periodontal therapy on C-reactive protein, oxidative stress, and matrix metalloproteinase (MMP)-9 and MMP-2 levels in patients with type 2 diabetes: a randomized controlled study. J Periodontol 83: 3-10. doi: 10.1902/jop.2011.110148. PubMed: 21627458. [DOI] [PubMed] [Google Scholar]
- 50. Lin SJ, Tu YK, Tsai SC, Lai SM, Lu HK (2012) Non-surgical periodontal therapy with and without subgingival minocycline administration in patients with poorly controlled type II diabetes: a randomized controlled clinical trial. Clin Oral Investig 16: 599-609. doi: 10.1007/s00784-011-0535-x. PubMed: 21416238. [DOI] [PubMed] [Google Scholar]
- 51. Llambés F, Silvestre FJ, Hernández-Mijares A, Guiha R, Bautista D et al. (2012) Efect of periodontal disease and non surgical periodontal treatment on C-reactive protein. Evaluation of type 1 diabetic patients. Med Oral Patol Oral Cir Bucal 17: e562-e568. PubMed: 22322513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tonetti MS, D'Aiuto F, Nibali L, Donald A, Storry C et al. (2007) Treatment of periodontitis and endothelial function. N Engl J Med 356: 911-920. doi: 10.1056/NEJMoa063186. PubMed: 17329698. [DOI] [PubMed] [Google Scholar]
- 53. Tüter G, Kurtiş B, Serdar M, Aykan T, Okyay K et al. (2007) Effects of scaling and root planing and sub-antimicrobial dose doxycycline on oral and systemic biomarkers of disease in patients with both chronic periodontitis and coronary artery disease. J Clin Periodontol 34: 673-681. doi: 10.1111/j.1600-051X.2007.01104.x. PubMed: 17590156. [DOI] [PubMed] [Google Scholar]
- 54. Tüter G, Serdar M, Kurtiş B, Walker SG, Atak A et al. (2010) Effects of scaling and root planing and subantimicrobial dose doxycycline on gingival crevicular fluid levels of matrix metalloproteinase-8, -13 and serum levels of HsCRP in patients with chronic periodontitis. J Periodontol 81: 1132-1139. doi: 10.1902/jop.2010.090694. PubMed: 20370419. [DOI] [PubMed] [Google Scholar]
- 55. López NJ, Quintero A, Casanova PA, Ibieta CI, Baelum V et al. (2012) Effects of periodontal therapy on systemic markers of inflammation in patients with metabolic syndrome: a controlled clinical trial. J Periodontol 83: 267-278. doi: 10.1902/jop.2011.110227. PubMed: 21749167. [DOI] [PubMed] [Google Scholar]
- 56. D'Aiuto F, Parkar M, Tonetti MS (2005) Periodontal therapy: a novel acute inflammatory model. Inflamm Res 54: 412-414. doi: 10.1007/s00011-005-1375-4. PubMed: 16283108. [DOI] [PubMed] [Google Scholar]
- 57. Kebschull M, Demmer RT, Papapanou PN (2010) "Gum bug, leave my heart alone!"--epidemiologic and mechanistic evidence linking periodontal infections and atherosclerosis. J Dent Res 89: 879-902. doi: 10.1177/0022034510375281. PubMed: 20639510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr. et al. (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359: 2195-2207. doi: 10.1056/NEJMoa0807646. PubMed: 18997196. [DOI] [PubMed] [Google Scholar]
- 59. Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM et al. (2005) C-reactive protein levels and outcomes after statin therapy. N Engl J Med 352: 20-28. doi: 10.1056/NEJMoa042378. PubMed: 15635109. [DOI] [PubMed] [Google Scholar]
- 60. Wang X, Bao W, Liu J, Ouyang YY, Wang D et al. (2013) Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 36: 166-175. doi: 10.2337/dc12-0702. PubMed: 23264288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Janket SJ, Wightman A, Baird AE, Van Dyke TE, Jones JA (2005) Does periodontal treatment improve glycemic control in diabetic patients? A meta-analysis of intervention studies. J Dent Res 84: 1154-1159. doi: 10.1177/154405910508401212. PubMed: 16304446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Michalowicz BS, Hodges JS, DiAngelis AJ, Lupo VR, Novak MJ et al. (2006) Treatment of periodontal disease and the risk of preterm birth. N Engl J Med 355: 1885-1894. doi: 10.1056/NEJMoa062249. PubMed: 17079762. [DOI] [PubMed] [Google Scholar]
- 63. Beck JD, Couper DJ, Falkner KL, Graham SP, Grossi SG et al. (2008) The Periodontitis and Vascular Events (PAVE) pilot study: adverse events. J Periodontol 79: 90-96. doi: 10.1902/jop.2008.070223. PubMed: 18166097. [DOI] [PubMed] [Google Scholar]
- 64. Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM et al. (2010) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375: 735-742. doi: 10.1016/S0140-6736(09)61965-6. PubMed: 20167359. [DOI] [PubMed] [Google Scholar]
- 65. Ioannidou E, Malekzadeh T, Dongari-Bagtzoglou A (2006) Effect of periodontal treatment on serum C-reactive protein levels: a systematic review and meta-analysis. J Periodontol 77: 1635-1642. doi: 10.1902/jop.2006.050443. PubMed: 17032104. [DOI] [PubMed] [Google Scholar]
- 66. Paraskevas S, Huizinga JD, Loos BG (2008) A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J Clin Periodontol 35: 277-290. doi: 10.1111/j.1600-051X.2007.01173.x. PubMed: 18294231. [DOI] [PubMed] [Google Scholar]
- 67. Ide M, Jagdev D, Coward PY, Crook M, Barclay GR et al. (2004) The short-term effects of treatment of chronic periodontitis on circulating levels of endotoxin, C-reactive protein, tumor necrosis factor-alpha, and interleukin-6. J Periodontol 75: 420-428. doi: 10.1902/jop.2004.75.3.420. PubMed: 15088881. [DOI] [PubMed] [Google Scholar]
- 68. Seinost G, Wimmer G, Skerget M, Thaller E, Brodmann M et al. (2005) Periodontal treatment improves endothelial dysfunction in patients with severe periodontitis. Am Heart J 149: 1050-1054. doi: 10.1016/j.ahj.2004.09.059. PubMed: 15976787. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)


