Abstract
Background
The goal of advanced access scheduling is to eliminate wait times for physician visits by ensuring access to same-day appointments, regardless of urgency or health care need. The intent is to reduce delays in access, leading to improvements in clinical care and patient satisfaction, and reductions in the use of urgent care.
Objective
To evaluate whether implementation of an advanced access scheduling system reduced other types of health service utilization and/or improved clinical measures and patient satisfaction among adults with chronic diseases.
Data Sources and Review Methods
A literature search was performed on January 29, 2012, for studies published from 1946 (OVID) or 1980 (EMBASE) to January 29, 2012. Systematic reviews, randomized controlled trials, and observational studies were eligible if they evaluated advanced access implementation in adults with chronic diseases and reported health resource utilization, patient outcomes, or patient satisfaction. Results were summarized descriptively.
Results
One systematic review in a primary care population and 4 observational studies (5 papers) in chronic disease and/or geriatric populations were identified. The systematic review concluded that advanced access did not improve clinical outcomes, but there was no evidence of harm. Findings from the observational studies in chronic disease populations were consistent with those of the systematic review. Advanced access implementation was not consistently associated with changes in clinical outcomes, patient satisfaction, or health service utilization.
Limitations
All studies were retrospective: 3 studies (4 papers) included historical controls only, and 1 included contemporaneous controls. Findings were inconsistent across studies for a number of outcomes.
Conclusions
Based on low to very low quality evidence, advanced access did not have a statistically (or clinically) significant impact on health service utilization among patients with diabetes and/or coronary artery disease (CAD). Very low quality evidence showed a significant reduction in the proportion of patients with diabetes and CAD admitted to hospital whose length of stay was greater than 3 days. Evidence was inconsistent for changes in clinical outcomes for patients with diabetes or CAD. Very low quality evidence showed no increase in patient satisfaction with an advanced access scheduling system.
Plain Language Summary
Timeliness of health care access—reducing wait times and delays for those receiving and providing care—is a key measure of health system quality. However, in international comparison studies, Canada ranked either last or next to last when it came to timely access to regular doctors. Efforts in Ontario to address delays in access have included the implementation of the Advanced Access and Efficiency for Primary Care initiative through the Quality Improvement and Innovation Partnership, later incorporated into Health Quality Ontario.
Advanced access is a physician appointment scheduling system that aims to eliminate wait times for physician visits and ensure same-day access for all patients, regardless of urgency or health care need. While it can generally be agreed that timely access to health care is necessary for all patients, same-day access may not always be required. Indeed, advanced access may adversely affect the care of patients with chronic diseases if clinics implement strict same-day appointment rules and patients cannot pre-book follow-up appointments. This review evaluated the effect of advanced access scheduling on clinical outcomes, patient satisfaction, and health service utilization in patients with selected chronic diseases, as part of the Optimizing Chronic Disease Management in the Outpatient (Community) Setting mega-analysis.
In patients with diabetes or coronary artery disease, advanced access implementation had little or no impact on acute health care use (hospitalizations, emergency department visits, and/or urgent care visits) and had inconsistent effects on clinical outcomes (blood glucose, low-density lipoprotein [LDL] cholesterol, and blood pressure). Two studies reported reduced monitoring of patients with chronic diseases after implementation of advanced access. Another study reported improved patient management (regular blood glucose and cholesterol testing) after advanced access implementation, but this was attributed to improved provider continuity rather than to reduced appointment wait times. There was no increase in patient satisfaction with the advanced access scheduling system. The quality of the evidence ranged from low to very low.
Background
In July 2011, the Evidence Development and Standards (EDS) branch of Health Quality Ontario (HQO) began developing an evidentiary framework for avoidable hospitalizations. The focus was on adults with at least 1 of the following high-burden chronic conditions: chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), atrial fibrillation, heart failure, stroke, diabetes, and chronic wounds. This project emerged from a request by the Ministry of Health and Long-Term Care for an evidentiary platform on strategies to reduce avoidable hospitalizations.
After an initial review of research on chronic disease management and hospitalization rates, consultation with experts, and presentation to the Ontario Health Technology Advisory Committee (OHTAC), the review was refocused on optimizing chronic disease management in the outpatient (community) setting to reflect the reality that much of chronic disease management occurs in the community. Inadequate or ineffective care in the outpatient setting is an important factor in adverse outcomes (including hospitalizations) for these populations. While this did not substantially alter the scope or topics for the review, it did focus the reviews on outpatient care. HQO identified the following topics for analysis: discharge planning, in-home care, continuity of care, advanced access scheduling, screening for depression/anxiety, self-management support interventions, specialized nursing practice, and electronic tools for health information exchange. Evidence-based analyses were prepared for each of these topics. In addition, this synthesis incorporates previous EDS work, including Aging in the Community (2008) and a review of recent (within the previous 5 years) EDS health technology assessments, to identify technologies that can improve chronic disease management.
HQO partnered with the Programs for Assessment of Technology in Health (PATH) Research Institute and the Toronto Health Economics and Technology Assessment (THETA) Collaborative to evaluate the cost-effectiveness of the selected interventions in Ontario populations with at least 1 of the identified chronic conditions. The economic models used administrative data to identify disease cohorts, incorporate the effect of each intervention, and estimate costs and savings where costing data were available and estimates of effect were significant. For more information on the economic analysis, please contact either Murray Krahn at murray.krahn@theta.utoronto.ca or Ron Goeree at goereer@mcmaster.ca.
HQO also partnered with the Centre for Health Economics and Policy Analysis (CHEPA) to conduct a series of reviews of the qualitative literature on “patient centredness” and “vulnerability” as these concepts relate to the included chronic conditions and interventions under review. For more information on the qualitative reviews, please contact Mita Giacomini at giacomin@mcmaster.ca.
The Optimizing Chronic Disease Management in the Outpatient (Community) Setting mega-analysis series is made up of the following reports, which can be publicly accessed at http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/ohtas-reports-and-ohtac-recommendations.
Optimizing Chronic Disease Management in the Outpatient (Community) Setting: An Evidentiary Framework
Discharge Planning in Chronic Conditions: An Evidence-Based Analysis
In-Home Care for Optimizing Chronic Disease Management in the Community: An Evidence-Based Analysis
Continuity of Care: An Evidence-Based Analysis
Advanced (Open) Access Scheduling for Patients With Chronic Diseases: An Evidence-Based Analysis
Screening and Management of Depression for Adults With Chronic Diseases: An Evidence-Based Analysis
Self-Management Support Interventions for Persons With Chronic Diseases: An Evidence-Based Analysis
Specialized Nursing Practice for Chronic Disease Management in the Primary Care Setting: An Evidence-Based Analysis
Electronic Tools for Health Information Exchange: An Evidence-Based Analysis
Health Technologies for the Improvement of Chronic Disease Management: A Review of the Medical Advisory Secretariat Evidence-Based Analyses Between 2006 and 2011
Optimizing Chronic Disease Management Mega-Analysis: Economic Evaluation
How Diet Modification Challenges Are Magnified in Vulnerable or Marginalized People With Diabetes and Heart Disease: A Systematic Review and Qualitative Meta-Synthesis
Chronic Disease Patients’ Experiences With Accessing Health Care in Rural and Remote Areas: A Systematic Review and Qualitative Meta-Synthesis
Patient Experiences of Depression and Anxiety With Chronic Disease: A Systematic Review and Qualitative Meta-Synthesis
Experiences of Patient-Centredness With Specialized Community-Based Care: A Systematic Review and Qualitative Meta-Synthesis
Objective of Analysis
The objective of this analysis was to evaluate whether implementation of an advanced access scheduling system—intended to ensure that patients have access to same-day appointments with a physician (primary care or specialty care)—reduced other types of health service utilization (hospital, emergency department [ED], acute care length of stay) and/or affected clinical measures and patient satisfaction among adults with chronic diseases.
Clinical Need and Target Population
The Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century (1) identified timeliness (defined as reducing waits and sometimes harmful delays for those who receive and give care) as 1 of 6 key areas for health care improvement in the United States. Wait times and delays are also an issue for Canadians: the Commonwealth Fund’s 2010 International Health Policy survey (2) compared health care systems in 11 developed countries, including Canada, and found that Canadians ranked last or next to last on questions of timely access to health care. Only 45% of surveyed Canadians reported that they were able to see a doctor or nurse the same or the next day when they needed care (compared to 93% of respondents from Switzerland), and 33% indicated that it took 6 or more days to see a doctor when they were last sick, compared to fewer than 10% of respondents from the United Kingdom, New Zealand, the Netherlands, and Switzerland. (2) Canadians also fared the worst in terms of access to after-hours health care and had the highest rates of ED use in the preceding 2 years. (2) These results are consistent with a previous version of the same survey, in which Canadians were found to be the heaviest users of EDs, with 16% of patients reporting an ED visit for a condition their physician could have treated if he or she had been available. (3)
However, while there is little disagreement about the importance of availability and access to health care—specifically access to primary care (4)—the definition of timely access is not clear. According to the federal report The Health of Canadians: The Federal Role, (5) timely access means that service is provided in a manner consistent with clinical practice guidelines to ensure that a patient’s health is not negatively affected while waiting for care. In other words, timely access does not necessarily mean immediate access.
Patients also appear to make this distinction. In a repeat cross-sectional telephone survey (2001 and 2004), Canadians ranked 10 priorities according to their importance for primary care performance evaluation. (6) Consistently in both years, waiting time for an appointment with a family physician for a nonurgent problem was ranked lowest. The top 3 primary care priorities—clinical knowledge, diagnostic skills, and ability to explain things to patients—were also consistent over time. Other priorities ranked higher than wait times for nonurgent care included timely referrals to specialists; health care provider sensitivity and caring nature; and whether health care providers or their staff contacted patients with routine follow-up reminders. (6) The authors commented: “We note the consistently low prioritization of access to care. Waiting time for a nonurgent appointment remains the lowest priority for primary care performance, despite attention at the federal and provincial levels to issues of access and ways to address them.” (6)
Nevertheless, while acceptable access to health care has still yet to be defined, Ontario has identified shorter wait times as a priority and has proceeded with the implementation of advanced access scheduling for primary care. The goal of advanced access scheduling is to eliminate wait times for physician visits, regardless of urgency or health care need, as a means of reducing the use of urgent care and improving clinical care and patient satisfaction. It remains to be determined whether patients need same-day access to ensure timely care and whether advanced access scheduling is associated with improvements in clinical care or patient outcomes.
Technology/Technique
Advanced access scheduling (also known as open access or same-day access scheduling) was developed by Mark Murray, Catherine Tantau, and Donald Berwick. (7-9) The authors applied queuing theory and principles of industrial engineering adapted to clinical settings, and posited that access delays could be reduced substantially without employing additional resources. Advanced access is premised on the idea that demand for appointments is predictable and, by balancing supply and demand and working through an existing appointment backlog, it is possible to implement an appointment system that allows patients to see a physician within 24 hours of requesting an appointment. (7-9)
The 6 steps to advanced access implementation are:
Match demand and supply daily.
Reduce (existing) backlog.
Simplify appointment types and times.
Create contingency plans.
Reduce demand for unnecessary visits.
Optimize the team care.
Murray and Tantau noted that some appointments—such as follow-up appointments scheduled by the physician or appointments booked on the day of a patient’s choosing rather than on the day of calling—are consistent with advanced access scheduling, but the volume of these appointment types should be taken into consideration when measuring demand and assigning open supply. (7) For example, practices with a larger proportion of elderly patients or patients with chronic diseases may need to accommodate more prescheduled appointments. (9) The developers also stressed the importance of physician-patient continuity: (7;9) “A patient calling to request an appointment with a physician not present that day should be given the choice of seeing another physician today or waiting to schedule an appointment with his or her physician later in the week.” (9) Despite these considerations, “the anchor metric for advanced access (success) is delays, measured as the time in days to the third next available routine appointment.” (9)
Advanced access scheduling has received substantial support in the United States and the United Kingdom: it has been endorsed by the Institute for Healthcare Improvement, (9) undergone rapid evaluation in the National Health Service in the United Kingdom, (10) and has been implemented by the United States Department of Veterans’ Affairs, (11) as well as in a number of managed care organizations in the United States and in some Canadian settings, including primary care practices in Ontario.
However, concerns about advanced access scheduling centre on its implementation and on variability in short- and long-term success rates (specifically reductions in wait times). In a number of evaluations, substantial variability in implementation and in short-term success have been noted, (10-14) as well as an inability to sustain shorter wait times over the long term (1 study reported on wait times 2 years after implementation). (14) Other potential unintended effects of advanced access implementation include reductions in provider continuity and follow-up; (15-18) acute problems crowding out chronic disease prevention and management; and disadvantages for specific populations, such as the frail elderly or those with cognitive impairments, language barriers, or socioeconomic barriers, (18;19) especially if advanced access is dogmatically implemented.
Ontario Context
The Advanced Access and Efficiency for Primary Care initiative was initially implemented in Ontario in 2008 by the Quality Improvement and Innovation Partnership and continues to be implemented through Health Quality Ontario. The aim of the program is to realize improvements in access to primary care and efficiency in the delivery of primary care within 6 months of initiating the program. The core objective is to ensure that patients calling to schedule a physician visit are offered an appointment with their primary care provider on the same day or a day of their choosing. As such, the program stresses the importance of continuity, as well as same-day access to care. Measures of successful implementation include time to the third next available appointment (less than 1 day) and that 85% of patients from multi-provider practices see their own provider at each visit. (20) As of the date of writing (July 2012), Ontario was completing wave 4 of the project; 413 primary care physicians had participated in the first 4 waves. Recruitment for wave 5 began in June 2012, with implementation scheduled to begin in September 2012.
Evidence-Based Analysis
Research Question
What is the effectiveness and cost-effectiveness of advanced access scheduling compared to traditional scheduling for the management of chronic diseases (atrial fibrillation, chronic obstructive pulmonary disease, chronic wounds, coronary artery disease [CAD], diabetes, heart failure, stroke, or multiple chronic conditions) in Ontario adults?
Research Methods
Literature Search
Search Strategy
A literature search was performed on January 29, 2012, using OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Wiley Cochrane Library, and the Centre for Reviews and Dissemination database, for studies published from 1946 (OVID) or 1980 (EMBASE) to January 29, 2012. While no date cut-off was used to limit the search, advanced access was developed in the late 1990s and more widely applied in the early 2000s; no literature exists on this intervention prior to that time.
Titles and abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search.
This review adopted the model of advanced access as developed by Murray and Tantau. (7;9;21) Studies of other scheduling interventions (such as carve-out scheduling) were not included. Of note, advanced access is largely implemented in primary care, but the search strategy and inclusion/exclusion criteria were not limited to this setting.
Inclusion Criteria
English language full-text reports
published before January 29, 2012
studies that described implementation and evaluation of advanced access scheduling
studies in a general chronic disease population or in 1 of the selected chronic disease populations (atrial fibrillation, chronic obstructive pulmonary disease, chronic wounds, CAD, diabetes, heart failure, stroke, or multiple chronic conditions)
studies with a comparison group (historical, contemporaneous)
studies that report at least 1 of the outcomes of interest (see below)
Exclusion Criteria
letters to the editor, commentaries, descriptions of implementation without an evaluation
studies in pediatric populations
studies to assess access to diagnostic testing or technologies
animal studies
duplicate publications
grey literature
Outcomes of Interest
Patient-Specific Outcomes
disease-specific clinical outcomes (e.g., hemoglobin A1c [HbA1c], cholesterol)
health-related quality of life
functional status
patient satisfaction
survival/mortality
Health System Outcomes
acute care hospital admissions and readmissions
ED visits
length of stay in hospital long-term care admissions
Statistical Analysis
Given the variability in implementation, study design, populations, and outcomes assessed among the included studies, it was not possible to conduct a meta-analysis of results; instead, the results are summarized descriptively. P values of less than 0.05 were considered significant.
Quality of Evidence
The quality of the body of evidence for each outcome was examined according to the GRADE Working Group criteria. (22) The overall quality was determined to be very low, low, moderate, or high using a step-wise, structural methodology.
Study design was the first consideration; the starting assumption is that randomized controlled trials are high quality, whereas observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias—were then taken into account. Limitations in these areas resulted in downgrading the quality of evidence. Finally, 3 main factors that may raise the quality of evidence were considered: large magnitude of effect, dose response gradient, and accounting for all residual confounding factors. (22) For more detailed information, please refer to the latest series of GRADE articles. (22)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | Very confident that the true effect lies close to the estimate of the effect |
| Moderate | Moderately confident in the effect estimate—the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
| Low | Confidence in the effect estimate is limited—the true effect may be substantially different from the estimate of the effect |
| Very Low | Very little confidence in the effect estimate—the true effect is likely to be substantially different from the estimate of effect |
Risk of Bias Assessment
Given that no randomized controlled trials (RCTs) were found, the risk of bias for each included study was assessed using updated criteria from the Effective Practice and Organization of Care (EPOC) group of the Cochrane collaboration, (23) which are more tailored to observational research than the criteria used by GRADE. Each study was evaluated, taking into consideration study design, randomization, allocation concealment, blinding, power/sample size, withdrawals/dropouts, intention-to-treat analyses, presence of control groups, assessment, and management of bias using design and statistical methods.
Assessment criteria differentiate between studies that include a contemporaneous control group and those that include historical controls, but factors that are common to both include the following:
potential for incomplete data
whether the intervention allocation is concealed
management of missing data
whether the paper is free from selective outcome reporting
other sources of bias
In addition to the above, studies with contemporaneous controls were assessed for baseline outcome measurements and baseline characteristics. Studies with historical controls were assessed for the following:
whether the intervention was independent of other changes
whether the intervention effect was prespecified
whether the intervention itself affected data collection
Results of Evidence-Based Analysis
The database search yielded 3,075 citations published before January 29, 2012 (with duplicates removed). Articles were excluded based on information in the title and abstract. The full texts of potentially relevant articles were obtained for further assessment. Figure 1 shows the breakdown of when and for what reason citations were excluded in the analysis.
Figure 1: Citation Flow Chart.
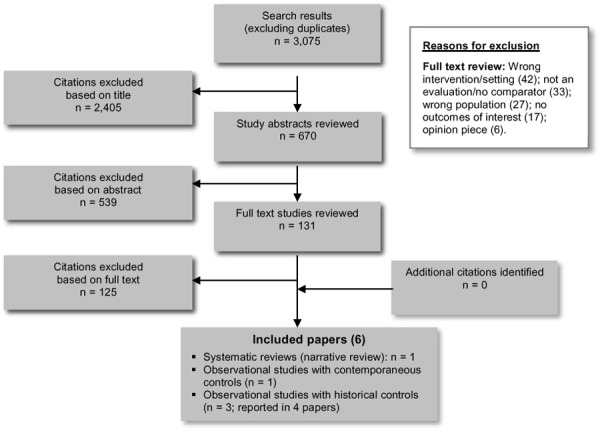
Six papers (1 systematic review, 1 observational with concurrent controls, and 4 observational with historical controls) met the inclusion criteria. Two of the papers reported on the same study; (24;25) the findings from these papers are presented separately, as they reported on different populations and outcomes, but when describing the studies and assessing risk of bias they were treated as 1 study. The reference lists of included studies and health technology assessment websites were hand-searched to identify any additional potentially relevant studies; no additional citations were identified.
The included studies were limited to advanced access implementation in primary care or geriatric care settings. Because no studies were identified in specialty care settings, it is not possible to draw any conclusions about the effect of advanced access on specialist access or outcomes of care from the results of this review.
For each included study, the study design was identified and is summarized below in Table 1, which is a modified version of a hierarchy of study design by Goodman. (26)
Table 1: Body of Evidence Examined According to Study Design.
| Study Design | Number of Eligible Studies |
|---|---|
| RCT Studies | |
| Systematic review of RCTs | 0 |
| Large RCT | 0 |
| Small RCT | 0 |
| Observational Studies | |
| Systematic review of non RCTs with contemporaneous controls | 1 |
| Non RCT with non-contemporaneous controls | 0 |
| Non RCT with contemporaneous controls | 1 |
| Non RCT with historical controls | 3a |
| Database, registry, or cross-sectional study | 0 |
| Case series | 0 |
| Retrospective review, modelling | 0 |
| Studies presented at an international conference | 0 |
| Expert opinion | 0 |
| Total | 5a |
Abbreviation: RCT, randomized controlled trial.
One study was reported in 2 papers.
Systematic Review of Advanced Access Implementation in Primary Care
Description of Review
Rose et al (27) conducted a systematic review of advanced access implementation in primary care settings. While the review did not specifically evaluate advanced access scheduling in chronic disease populations, it did include studies that were specific to adults with chronic diseases. The review evaluated 28 articles representing 24 studies and included publications and grey literature up to August 2010. Publications included articles, research letters, and brief reports written or translated into English. The authors did not limit inclusion based on study design, but they did exclude reports that were not written in scientific format or that did not have a full description of methods, study population, baseline data, or results. Because of heterogeneity among the publications, the authors did not conduct a meta-analysis; they restricted their analysis to a narrative review.
Impact of Advanced Access in Primary Care
Outcomes included in the review—along with the findings for each outcome—are reported in Table 2.
Table 2: Systematic Review—Outcomes, Measures, and Results.
| Outcome | Measure (# of Studies) | Results |
|---|---|---|
| Successful implementation of advanced access | Time to third next appointment (8 studies) | Advanced access was associated with a decrease in time to third next appointment in all studies, with statistically significant declines reported in 5 studiesa |
| No-show rate | Percent of patients who miss booked appointments (11 studies) | Ten studies showed some improvement in no-show rates, with statistically significant improvement reported in 5 studies |
| Continuity of care | Any measure used to assess how often patients saw their own primary care physician (9 studies) | There was an improvement in continuity of care in 7 studies and a decline in 2 studies. Statistically significant improvements were reported in 3 studies |
| Health care utilization (ED visits, urgent care visits, and hospital admissions) | Percent of patients who had a visit to an ED, an urgent care clinic, or a hospital admission at least once (2 studies) | Neither study reported significant changes in ED visits or hospitalizations. One study reported a significant reduction in urgent care visits |
| Clinical indicators | HbA1c, lipids, blood pressure (3 studies)b | Two studies reported statistically significant improvements in HbA1c, but the difference was clinically significant in only 1 study. One study reported a statistically significant improvement in lipid control, while another study reported a statistically significant decline in blood pressure control. |
| Patient satisfaction | Overall patient satisfaction (4 studies) | Two studies reported improvements in patient satisfaction; this finding was statistically significant in 1 study |
| Appointment-system satisfaction (4 studies) | Two studies showed some improvement in satisfaction, but these findings were not statistically significant. One study reported a statistically significant decline in satisfaction |
Abbreviations: ED, emergency department; HbA1c, hemoglobin A1c.
No studies reported a time to third next appointment of less than 1 day, the goal of advanced access scheduling.
One study conducted in the Veterans’ Administration reported significant clinical improvements but was excluded by the authors because a number of other concurrent quality improvement initiatives were underway.
Results varied substantially across studies; this finding may be attributed at least in part to differences in implementation and the success of advanced access scheduling. Generally, implementation reduced no-show rates and improved access, and some (but not all) studies were able to reduce wait times to 2 days or fewer. The reviewers additionally reported small to neutral changes in patient satisfaction and continuity of care, but with some inconsistency in the findings. The effects on clinical outcomes were mixed, and there were no clinically and statistically significant reductions in health service utilization, with the exception of a reduction in urgent care visits noted in 1 study.
With respect to improvements in patient access, the authors concluded the following: “Most practices attempting advanced access reduce wait time substantially, although few achieve same-day access. For practices with high no-show rates, advanced access appears to yield marked improvements; however, it is less effective for practices with lower baseline no-show rates.” (27)
However, while the authors suggested that wait times for primary care access were improved, they were equivocal about the effect of advanced access on clinical outcomes: “Overall, it does not appear that advanced access in itself is a particularly robust method of improving clinical outcomes. However, we found no compelling evidence of harm.” (27)
Limitations
This review had a number of limitations, most stemming from those of the original studies. Few of the studies were high quality or rigorous; 1 cluster RCT was included, but it had evidence of substantial contamination, possibly explaining the lack of significant findings in this study. While a few studies included contemporaneous controls, most were before-and-after designs, and did not account for secular trends or other improvement initiatives that were concurrently underway. Almost all of the included studies involved self-selection of participating sites, and the authors noted that the overall risk of bias was high. Measurement was inconsistent for some of the included outcomes (e.g., continuity of care, patient satisfaction), but the authors reported combined results nevertheless. Finally, the authors had intended to include studies that evaluated advanced access implementation in primary care practice, but they also included studies that were specific to pediatric or geriatric populations. While these studies may have been reflective of primary care, the specificity of their populations warranted a separate analysis.
Health Quality Ontario Comments
This systematic review was intended to explore advanced access scheduling in a general primary care population and so included patient populations beyond the scope of this review.
Studies of Advanced Access Implementation in Chronic Disease Populations
Description of Studies
Four observational studies (reported in 5 papers) also met the inclusion criteria for this review, 3 of which were also included in the systematic review by Rose et al. (27) Table 3 describes the included studies and the relevant review-specific outcomes reported in each.
Table 3: Description of Study Elements and Outcomesa.
| Study, Setting | Design | Research Question | Population | All Reported Outcomes | Review-Specific Outcomes, Y/N | ||||
|---|---|---|---|---|---|---|---|---|---|
| Hospitalizations | ED Visits | Inpatient LOS | Clinicals Measures | Patient Satisfaction | |||||
| Subramanian et al, (28) Indiana, United States | Pre/post observational study with concurrent controls | What is the effect of OA scheduling on processes and outcomes of diabetes care and health care utilization in OA clinics compared to control clinics (traditional scheduling)? | Indiana University Medical Group, primary care clinic patients with diabetes who were covered under the Wishard Advantage health plan and receiving care in 1 of 12 participating clinics (6 intervention, 6 control)
|
Health service utilization: mean number of hospitalizations, mean number of outpatient visits (ED/urgent care and primary care) Clinical measures: HbA1c, LDL-C, SBP Process of care: annual measurement of HbA1c, urine protein, LDL-C |
Y | Ya | N | Y | N |
| Solberg et al, (24) Minnesota, United States | Pre/post observational study with historical controls | Is implementation of advanced access in a large, multispecialty medical group associated with changes in utilization or costs for patients with diabetes, CHD, or depression? | Patients with diabetes, CHD, or depression who were receiving care in 17 primary care clinics in a multispecialty medical group (about 240,000 plan members) Diabetes
CHD
|
Health service utilization: mean number of primary care visits per patient; % of patients who had 1+ ED visits, urgent care visits, or hospitalizations; hospital LOS > 3 days Advanced access: continuity of care Proportion of visits in primary care that were for chronic conditions Total costs of care for patients |
Y | Y | Y | N | N |
| Sperl-Hillen et al, (25) Minnesota, United States (diabetes population only) | Does implementation of advanced access affect composite measures of diabetes care? Specifically, does improved availability of appointments and continuity resulting from advanced access affect diabetes quality of care measures? | Patients with diabetes who were receiving care in 17 primary care clinics in a multispecialty medical group (about 240,000 plan members)
|
Health service utilization: primary care visits, urgent care, and/or ED visits Clinical measures: composite measures of LDL-C and HbA1c Process of care: composite measures of % of patients with 1+ LDL-C and HbA1c in 1 year Advanced access: continuity of care, wait times for appointments |
N | Ya | N | Y | N | |
| Gladstone et al, (29) Ontario, Canada | Pre/post observational study with historical controls | What is the effect of advanced access scheduling on the care of patients with chronic diseases (hypertension, type 2 diabetes, and CAD) in a Canadian family practice? | Patients in a single family physician practice in Brantford, Ontario (panel size about 2,000) with a clinical record of hypertension, type 2 diabetes, and/or CAD
|
Clinical measures: HbA1c, LDL-C, SBP Process of care: number of visits for chronic disease management, total number of visits |
N | N | No | Y | N |
| Cherniack et al, (18) Florida, United States (Veterans Affairs) | Pre/post observational study with historical controls | What is the impact of advanced access scheduling on geriatric patients (in a geriatric practice setting)? | Patients in a Veterans’ Affairs geriatric clinic in Miami, Florida. Patient population of 1,000; sample of patients included was not specified | Patient satisfaction Patient visits Advanced access: missed appointments |
N | N | N | N | Y |
Abbreviations: CAD, coronary artery disease; CHD; coronary heart disease; ED, emergency department; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; LOS, length of stay; OA, open access; SBP, systolic blood pressure.
This table is ordered to reflect the quality of the included studies.
All studies conducted a retrospective, pre-versus-post analysis. One study included concurrent controls, but a number of patient and clinic characteristics differed significantly between the intervention and control populations. (28) Intervention sites were self-selected in all studies, and all included 1 year of data from the baseline (pre-implementation) period and 1 year of data from the post-implementation period. One study (24;25) defined a separate 1 year implementation period, for which data were separately collected and reported in 1 of the papers. (25) The other 3 studies did not define an implementation period, instead using a single date to distinguish between pre- and post-implementation. (18;28;29)
Two of the 5 papers included multiple chronic disease populations. Solberg et al (24) reported on the impact of advanced access scheduling on patients with diabetes (diabetes type was not distinguished), depression, and/or coronary heart disease (CHD) in a multicentre, primary care network. Gladstone and Howard (29) included patients with hypertension, type 2 diabetes, and CAD in a solo practice primary care setting. Neither study specifically identified a multiple morbidity cohort, but they did report prevalence rates that were indicative of multiple morbidity. Instead, patients with multiple conditions were included in several different single-condition cohorts, which created the potential for double counting. The study by Sperl-Hillen et al (25) was a follow-up publication to Solberg et al (24), focusing on the population with diabetes (with or without other conditions). The populations in the other 2 studies were patients with diabetes (diabetes type not distinguished) in a health care plan in Indiana (28) and the patient population of a United States Veterans’ Affairs geriatric clinic in Florida. (18)
In four of the papers, identification of chronic disease populations was based on either chart review using information from patients’ clinical and medication histories (29) or on validated administrative data algorithms using International Classification of Disease, 9th Edition codes. (24;25;28) The final study assessed the impact of advanced access scheduling in a geriatric clinic population, and the entire patient panel was included in the analysis. (18)
Only 2 studies specifically reported measures of successful advanced access implementation. Sperl-Hillen et al (25) reported the time to third next appointment, and Cherniack et al (18) reported missed appointment rates and follow-up rates.
Hospitalizations
The association between advanced access implementation and hospitalization rates was assessed in 2 papers. One study included patients with diabetes, (28) and the other study included patients with diabetes and/or CHD. (24) See Table 4 for details.
Table 4: Impact of Advanced Access Implementation on Hospitalization Ratesa.
| Study | Results |
|---|---|
| Subramanian et al (28) | The mean number of all-cause hospitalizations (per patient) increased nonsignificantly in both OA (0.30 to 0.35) and non-OA clinics (0.24 to 0.27) in the post-implementation period Rate ratio, OA clinics to non-OA clinics = 0.95 (95% CI, 0.81–1.11)b |
| Solberg et al (24) |
Diabetes: The percentage of patients who were admitted at least once increased nonsignificantly between the pre- and post-implementation periods, from 9.5% to 9.7% (P = 0.70)c CHD: The percentage of patients who were admitted at least once decreased slightly but significantly between the pre- and post-implementation periods, from 58.4% to 57.3% (P = 0.002)c |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; OA, open access.
The table is ordered to reflect the quality of the included studies.
Based on multivariate modelling adjusted for patient and clinic characteristics.
Rates were adjusted for age, sex, and modified Charlson score.
For patients with diabetes, both studies reported a nonsignificant increase in hospitalizations. Subramanian et al compared outcomes for open access (OA) and non-OA clinics but did not find a difference in hospitalization rates between the two clinic types. (28)
For patients with CHD, Solberg et al (24) reported a slight but significant reduction in hospitalizations in the post-implementation period compared to the pre-implementation period; however, rates in both periods were high, and the absolute reduction was less than 1%, suggesting that the study may have been overpowered for this outcome.
Emergency Department and/or Urgent Care Visits
The association between advanced access implementation and ED and/or urgent care visits was assessed in 3 papers (2 studies). See Table 5 for details.
Table 5: Impact of Advanced Access Implementation on Emergency Department/Urgent Care Visitsa.
| Study | Results |
|---|---|
| Subramanian et al (28) | The mean number of all-cause ED and urgent care visits (per patient) did not change in either the OA (1.1 visits in both periods) or non-OA clinics (0.9 visits in both periods) between the pre- and post-implementation periods Rate ratio, OA clinics to non-OA clinics = 0.97 (95% CI, 0.92–1.02)b |
| Solberg et alc (24) |
Diabetes: The percentage of patients who had 1+ ED visits increased nonsignificantly between the pre- and post-implementation periods, from 14.4% to 15.1% (P = 0.08)d CHD: The percentage of patients who had 1+ ED visits decreased nonsignificantly between the pre- and post-implementation periods, from 51.5% to 50.9% (P = 0.07)d |
| Sperl-Hillen et alc (25) | The percentage of patients who had 1+ ED or urgent care visits decreased significantly between the pre- and post-implementation periods, from 41.0% to 37.6% (P < 0.001) The decline between the pre-implementation and implementation periods was not significant (41.0% to 40.1%, P = 0.26); no comparison was made between the implementation and post-implementation periods |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; ED, emergency department; OA, open access.
The table is ordered to reflect the quality of the included studies.
Based on multivariate modelling adjusted for patient and clinic characteristics.
Solberg et al (24) and Sperl-Hillen et al (25) reported on findings from the same study but used different outcome measures.
Rates were adjusted for age, sex, and modified Charlson score.
For patients with diabetes, Subramanian et al (28) detected no change in the mean number of combined, all-cause ED and urgent care visits between the pre- and post-implementation periods and did not find a significant difference in the change in visit rates between intervention (OA) and control (non-OA) clinics.
Also for patients with diabetes, Solberg et al (24) reported a nonsignificant increase in the percentage of patients who had more than 1 ED visit between the pre- and post-implementation periods; however, Sperl-Hillen et al (25) reanalyzed these data combining ED and urgent care visits and reported a significant decline between the pre- and post-implementation periods, but no significant decline between the pre- implementation and implementation periods. The difference in findings between these 2 papers from the same study is likely due to a change in outcome definition.
For patients with CHD, Solberg et al (24) reported a slight, nonsignificant decrease in the percentage of patients who attended an ED at least once.
Acute Care Length of Stay
Solberg et al (24) analyzed the association between advanced access implementation and acute care length of stay (LOS) in patients with diabetes and/or CHD. See Table 6 for details.
Table 6: Impact of Advanced Access Implementation on Acute Care Length of Stay.
| Study | Results |
|---|---|
| Solberg et al (24) |
Diabetes: The percentage of patients who had an acute care LOS of more than 3 days decreased significantly between the pre- and post-implementation periods, from 58.2% to 54.4% (P = 0.03)a CHD: The percentage of patients who had an acute care LOS of more than 3 days decreased significantly between the pre- and post-implementation periods, from 55.7% to 51.9% (P = 0.003)a |
Abbreviations: CAD, coronary artery disease; LOS, length of stay.
Rates were adjusted for age, sex, and modified Charlson score.
For both populations, the authors reported a significant decline in the percentage of patients who stayed in hospital for more than 3 days after advanced access implementation.
Disease-Specific Clinical Outcomes
The association between advanced access implementation and specific clinical disease outcomes was assessed in 3 studies. See Table 7 for details.
Table 7: Impact of Advanced Access Implementation on Disease-Specific Clinical Outcomesa.
| Study | Results |
|---|---|
| Subramanian et al (28) | OA clinic patients had a significant decrease in mean HbA1c, but a significant increase in mean SBP compared to non-OA clinic patients. There was no difference in change in LDL-C between OA and non-OA clinic patients Mean difference OA to non-OA clinics: HbA1c (%): –0.12 (95% CI, –0.21, –0.03) SBP (mm Hg): 6.4 (95% CI, 5.4, 7.5) LDL-C (mg/dL): –0.2 (95% CI, –2.0, 1.5) |
| Sperl-Hillen et al (25) | The percentage of patients with HbA1c < 7% increased significantly between the pre- and post-implementation periods, from 44.4% to 52.3% (P < 0.001)b The percentage of patients with LDL-C < 100 mg/dL increased significantly between the pre- and post-implementation periods, from 29.8% to 38.7% (P < 0.001)b |
| Gladstone et al (29) | Mean HbA1c
decreased nonsignificantly between the pre- and post-implementation periods, from 7.2% to 7.1% (P = 0.17) Mean LDL-C decreased slightly but significantly between the pre- and post-implementation periods, from 2.7 mmol/L to 2.6 mmol/L (P = 0.04) |
Abbreviations: CI, confidence interval; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; OA, open access; SBP, systolic blood pressure.
The table is ordered to reflect the quality of the included studies.
Utilization rates were adjusted for age, sex, and modified Charlson score.
Among patients with diabetes, Subramanian et al (28) reported that intervention (OA) sites had a larger mean reduction in HbA1c but a significant increase in mean systolic blood pressure over time compared to control (non-OA) sites. There was no difference in change in low-density lipoprotein cholesterol (LDL-C) between intervention and control sites.
Also among patients with diabetes, Sperl-Hillen et al (25) and colleagues reported a significant increase in the percentage of patients with controlled HbA1c and/or LDL-C after advanced access implementation compared to the pre-implementation period.
Among patients with CAD and/or diabetes, Gladstone et al (29) also reported declines in both clinical measures, but the change in HbA1c was not statistically significant, and the authors reported that the change in LDL-C, although statistically significant, was not clinically meaningful.
Patient Satisfaction
Only 1 study specifically measured patient satisfaction with advanced access scheduling. Cherniack et al (18) reported that 55% of a convenience sample of 125 patients in a geriatric clinic preferred advanced access scheduling to traditional appointment scheduling, but no statistical analyses were conducted.
Other Reported Outcomes
Process-of-Care Measures
Process-of-care measures for chronic disease management were assessed in 3 papers.
Subramanian et al (28) conducted multivariate analyses on process-of-care measures in OA clinics compared to non-OA clinics. In OA clinics, the percentage of patients who underwent testing for HbA1c, LDL-C, and urine microalbumin changed very little in the post-implementation year compared to the pre-implementation year, but there were substantial improvements in the non-OA clinics in all 3 measures. As a result, the odds ratios associated with processes of care suggested that OA clinics had significantly fewer improvement in their processes of diabetes care than non-OA clinics for HbA1c and urine microalbumin (the odds ratio associated with urine microalbumin screening was significant only for non-African American patients). The authors did not mention that other quality-improvement initiatives were underway during the study period; it may be that to see significant improvements in quality of care, efforts may be better directed at improving clinical care rather than increasing access to care.
Conversely, Sperl-Hillen et al (25) reported that significantly higher proportions of patients underwent HbA1c (2 or more in 1 year) and LDL-C (1 or more in 1 year) testing after the implementation of advanced access scheduling. The study authors conducted multivariate analyses (controlling for age, sex, CAD, and study year) to assess the independent association between wait times and provider continuity and composite measures of the following:
process of care (patients had 2 or more HbA1c measurements and 1 or more fasting lipid profiles during the year)
good clinical control (HbA1c < 8% and LDL-C < 130 mg/dL)
excellent clinical control (HbA1c < 7% and LDL-C < 100 mg/dL)
Higher provider continuity was significantly associated with improvements in clinical process (P = 0.01), good clinical control (P = 0.03), and excellent clinical control (P < 0.001). On the other hand, lower wait times were not associated with any of these composite measures. The authors concluded that diabetes care could be improved by increasing continuity of care by primary care physicians, and that there was no direct relation between wait time and improved care. The authors also noted that shorter provider wait times were only weakly associated with increased continuity of care and that “…gains in continuity of care should be attributed only cautiously to advanced access.” (25)
The third study to report on process-of-care measures was from a primary care practice in Ontario. (29) This study reported significant declines in the mean number of measurements of blood pressure (3.3 to 2.9, P = 0.001), HbA1c (1.7 to 1.5, P= 0.01) and LDL-C (1.5 to 1.2, P < 0.001) between the pre-implementation year and the post-implementation year. The authors also reported a significant decline in the number of visits for chronic disease management after advanced access implementation (from 2.6 visits to 2.2 visits per year, P= 0.02), although there was no change in the average number of visits per patient in the pre- versus post-implementation years (4.3 visits in both), suggesting a shift away from chronic disease management visits towards visits for acute problems; these increased from 1.7 to 2.1 visits during the same period (P= 0.02). (29)
Such a reduction in the proportion of visits for chronic disease management echoes the findings of Solberg et al, (24) who reported an absolute increase in the total number of visits and the number of chronic disease visits for all 3 cohorts (diabetes, CHD, and/or depression) but also noted a significant decline in the proportion of total visits that were specifically for chronic disease care for patients with CHD (P = 0.002) and/or diabetes (P < 0.001). It is not possible to determine whether patients are receiving adequate chronic disease care from either of these studies. (24;29)
Costs
Solberg et al (24) also reported on total costs of care. The authors reported a 10% to 20% increase in total costs of care (inpatient, outpatient, and skilled nursing facilities) in the post-implementation period compared to the pre-implementation period for all 3 patient cohorts (diabetes, CHD, and/or depression); this may have been partly related to the increased number of visits noted above. These costs did not include the costs of the actual intervention. Without a control group comparison, it is not possible to make an association between advanced access implementation and costs, but the increases in the number of visits and total health care costs merits further investigation.
Missed Appointments
Cherniack et al (18) looked at the impact of advanced access implementation in a geriatric clinic population. While this study did not examine clinical outcomes or processes of care, the authors did look at rates of missed appointments (i.e., no-show rates) and number of patient visits per month. The authors reported a significant reduction in the proportion of missed appointments per month (as a percentage of total visits) after advanced access implementation (from 18% to 11%, P < 0.001), but they also reported a decrease in total number of visits per month in the early period after advanced access implementation. (18) This decrease was addressed by hiring a medical assistant part-way through the study, who called patients to schedule regular follow-up appointments. This implies that without additional resources, this clinic may have seen a significant reduction in patient follow-up. The authors suggested the following:
“…because an open access scheduling system requires patients to take the initiative to schedule their appointments, it may disadvantage frail elderly individuals, who have more sensory or cognitive impairments and are thus less able to schedule appointments on their own … the system may also disadvantage less educated patients, who might be less likely to schedule important follow-up visits for diseases for which they are asymptomatic.” (18)
Limitations
There are a number of study limitations that limit the strength of evidence for this review. None of the studies employed an RCT design, although a cluster randomized design would have been possible, especially in some of the larger implementations. (11;25;28;30) Even though an RCT design was not available, the identification of control sites and measurement of outcomes in these sites should have been undertaken. Only 1 study included control sites, but even in this study, intervention and control sites were self-selected and differed significantly with respect to clinic and population characteristics. As well, the authors did not report blind assessment of outcomes, although this should have been possible.
Advanced access is often implemented as part of larger quality-improvement programs, but only 1 study identified other quality-improvement efforts underway. (24) Even in this study, however, the authors did not attempt to adjust their findings to take these additional programs (1 of which was in diabetes management) into account. For this reason, changes may have been attributed to advanced access rather than to other improvement efforts.
The study by Subramanian et al (28) used administrative data to assess outcomes and determined that care outside of the health insurance plan would not be captured. They indicated that since the study population was from a lower socioeconomic group, it was unlikely that they would receive care outside the insured health system, but there was no effort to quantify outside use. The other American study that assessed outcomes (24;25) did not discuss the possibility of health service use outside of the health plan, even though this would likely be an issue for outcome assessment in this study as well. Such lack of capture could have resulted in undercounting of events (e.g., hospitalizations, ED use) possibly leading to an overestimated effect of advanced access.
Two studies included multiple chronic disease cohorts, but neither study attempted to distinguish patients with multiple chronic diseases. (24;29) As a result, both studies attributed outcomes such as numbers of visits, hospitalizations, and process of care measures to multiple disease cohorts, and may have led to double counting of outcomes. The impact of this error could both positively and negatively affect the assessment of advanced access.
Only 2 papers reported on the successful implementation of advanced access, (18;25) and only 1 assessed the association between reductions in wait times for appointments with outcomes. (25) It is possible that the lack of findings for a number of outcomes was associated with the unsuccessful implementation of advanced access.
Discussion
Advanced access scheduling has been shown to be effective at reducing wait times for appointments and no-show rates, and it may even improve health care provider satisfaction (although this was not assessed in this review), but it appears to have limited impact on patients’ health service utilization and clinical outcomes. It is possible that a review that specifically assesses the impact of advanced access scheduling in chronic disease populations will be limited in its ability to detect important benefits. However, it is also possible that because advanced access is best suited to managing acute problems, its benefits are substantially greater for populations without chronic disease. Still, given the increasing burden of chronic disease in Ontario and the typically higher rates of health service utilization and costs in such populations, any health care reforms undertaken must not negatively affect people with chronic diseases.
This review and the systematic review by Rose et al (27) found that advanced access seems to be most effective at improving access, particularly for practices with significantly greater access-related problems. As such, advanced access should be considered an optional intervention for practices for which access to care is a significant issue, with the caveat that continuity of care should not be compromised simply to increase access.
In contrast, advanced access has shown little benefit in terms of patient outcomes, and may in fact negatively impact the regular management of chronic disease. Four studies in this analysis reported on process-of-care measures and/or follow-up, but the findings were inconsistent. A study of advanced access implementation in a geriatric population found that some patients were at risk of not receiving adequate follow-up as a result of advanced access implementation. (18) To address this, the clinic hired an additional medical assistant to ensure that patients were being contacted and follow-up appointments booked; this suggests that advanced access may negatively impact the ability of older patients to receive timely follow-up.
Gladstone et al (29) reported fewer chronic disease visits during the post-implementation year (compared to the pre-implementation year) and also noted a commensurate reduction in regular cholesterol and blood glucose testing. Similarly, Subramanian et al (28) reported significantly lower rates of HbA1c, LDL-C, and urine microalbumin testing among patients with diabetes in advanced access clinics compared to control clinics. The findings from these 2 independent studies suggest that advanced access implementation may negatively affect chronic disease management. While both studies reported reduced rates of patient monitoring and/or follow-up, clinical outcomes were inconsistent, which may be due to the process of implementation and the short follow-up periods (neither study followed patients for more than 1 year after implementation).
The third study that evaluated process-of-care measures reported improvements in clinical care after advanced access implementation, but the authors attributed this (in multivariate modelling) to improvements in provider continuity rather than to shorter appointment wait times. (25) In fact, the authors concluded that continuity of care was more important for patients with diabetes, and that shorter wait times were only slightly associated with improvements in continuity of care. This suggests that if advanced access is to be implemented, ensuring that patients see their own physician whenever possible is more important than getting patients an appointment within 24 hours.
One of the drivers of advanced access implementation is the belief that by increasing access to primary care, urgent care utilization and hospitalization rates will decrease. The idea is that by addressing problems at the primary care level, they will not progress toward the need for more costly, acute care. Unfortunately, the research findings do not support this, either in general primary care or in specific chronic disease populations. In the 2 studies (3 papers) that examined hospitalizations, ED visits, and urgent care visits, advanced access was inconsistently associated with changes in acute care utilization. (24;25;28) Two papers reported no change in hospitalization rates or ED and/or urgent care visits for patients with diabetes (24;28) and the 1 paper that reported on hospitalization rates for patients with CHD reported a statistically significant decline that was likely not clinically relevant. (24) The study by Solberg et al (24) was re-analyzed by Sperl-Hillen et al (25) and combined ED visits and urgent care utilization and reported a significant reduction after advanced access implementation, but it is difficult to interpret this inconsistency beyond attributing it to the change in definition.
Since advanced access scheduling improves access to health care, it may be important to focus resources on this intervention, but only for those practices where access is truly an issue. Where access is not an issue, or if the issue has already been addressed successfully, quality-improvement efforts should focus instead on improving the continuity and quality of care received by patients.
Summary
Table 8: Summary of Findings.
| Outcome | Number of Studies | Results | GRADE |
|---|---|---|---|
| Diabetes Population | |||
| Hospitalizations | 2 studies (24;28) | No significant change in hospitalization rates in either study Subramanian et al (28) reported a nonsignificant increase in the mean number of all-cause hospitalizations in both OA and non-OA clinics post-implementation. The rate ratio of OA clinics to non-OA clinics was 0.95 (95% CI, 0.81–1.11) Solberg et al (24) reported that the percentage of patients who were admitted at least once increased nonsignificantly between the pre- and post-implementation periods, from 9.5% to 9.7% (P = 0.70) |
Low |
| ED visits | 1 study (24) | No significant change in ED visit rates: % with 1+ ED visits, pre vs. post = 14.4% to 15.1% (P = 0.08) | Very low |
| ED visits and/or urgent care visits | 2 studies (25;28) | Inconsistent findings across studies Subramanian et al (28) reported no significant change in the mean number of ED and/or urgent care visits either between pre- and post-implementation periods (within OA clinics) or when comparing the change in rates in OA vs. non-OA clinics; rate ratio, OA clinics to non-OA clinics = 0.97 (95% CI, 0.92–1.02). Sperl-Hillen et al (25) reported a significant reduction in the percent of patients with 1 or more urgent care and/or ED visit, from 41.0% to 37.6% (P < 0.001) |
Very low |
| LOS | 1 study (24) | Significant reduction in % of patients with LOS > 3 days, pre vs. post = 58.2% vs. 54.4% (P = 0.03) | Very low |
| HbA1c, LDL-C, SBP | 3 studies (25;28;29) | Inconsistent findings across studies Subramanian et al (28) showed improvement (HbA1c), deterioration (SBP), and no difference (LDL-C) Gladstone et al (29) reported small but statistically significant reductions in LDL-C but no other changes in clinical measures; the authors indicate this difference was not clinically important Sperl-Hillen et al (25) showed improved control for HbA1c and LDL-C |
Very low |
| CAD/CHD Population | |||
| Hospitalizations | 1 study (24) | Significant reduction in hospitalization rates: % with 1+ admission (all-cause), pre vs. post = 58.4% vs. 57.3% (P = 0.002) | Very low |
| ED visits | 1 study (24) | No significant change in ED visit rates: % with 1+ ED visits, pre vs. post = 51.5% vs. 50.9% (P = 0.07) | Very low |
| LOS | 1 study (24) | Significant reduction in % of patients with LOS > 3 days, pre vs. post = 55.7% vs. 51.9% (P = 0.003) | Very low |
| HbA1c, LDL-C, SBP | 1 study (29) | Inconsistent findings Small but statistically significant reductions in LDL-C, but no other changes in clinical measures; the authors indicate this difference was not clinically important |
Very low |
| Geriatric Population | |||
| Patient satisfaction | 1 study (18) | 55% of a convenience sample (n = 125) of patients preferred advanced access scheduling to traditional scheduling (no statistical tests were reported) | Very low |
Abbreviations: CAD, coronary artery disease; CHD, coronary heart disease; ED, emergency department; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; LOS, length of stay; OA, open access; SBP, systolic blood pressure.
Conclusions
Advanced Access in a Diabetes Population
There were no significant changes in hospitalization rates for patients with diabetes; the quality of the evidence was low.
There were no significant changes in ED visit rates for patients with diabetes; the quality of the evidence was very low.
There was inconsistent evidence of changes in combined ED/urgent care visits for patients with diabetes. One study found no reduction, while the second study reported a significant reduction; the quality of the evidence was very low.
There was a significant reduction in the proportion of patients with diabetes admitted to hospital whose length of stay was greater than 3 days; the quality of the evidence was very low.
There was inconsistent evidence of changes in chronic disease clinical measures (HbA1c, LDL-C, systolic blood pressure) for patients with diabetes; the quality of the evidence was very low.
Advanced Access in a CAD/CHD Population
There was a significant reduction in hospitalization rates for patients with CHD; the quality of the evidence was very low.
There were no significant changes in ED visit rates for patients with CHD; the quality of the evidence was very low.
There was a significant reduction in the proportion of patients with CHD admitted to hospital whose length of stay was greater than 3 days; the quality of the evidence was very low.
There was inconsistent evidence of changes in chronic disease clinical measures (HbA1c, LDL-C, systolic blood pressure) for patients with CAD/CHD; the quality of the evidence was very low.
Advanced Access in a Geriatric Population
The authors reported that a majority of patients (55%) were satisfied with an advanced access scheduling system over traditional appointment scheduling systems, but no statistical analysis was conducted, and the quality of the evidence was very low.
Acknowledgements
Editorial Staff
Jeanne McKane, CPE, ELS(D)
Medical Information Services
Kaitryn Campbell, BA(H), BEd, MLIS
Kellee Kaulback, BA(H), MISt
Expert Panel for Health Quality Ontario: Optimizing Chronic Disease Management in the Community (Outpatient) Setting
| Name | Title | Organization |
|---|---|---|
| Shirlee Sharkey (chair) | President & CEO | Saint Elizabeth Health Care |
| Theresa Agnew | Executive Director | Nurse Practitioners’ Association of Ontario |
| Onil Bhattacharrya | Clinician Scientist | Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Arlene Bierman | Ontario Women’s Health Council Chair in Women’s Health | Department of Medicine, Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Susan Bronskill | Scientist | Institute for Clinical Evaluative Sciences |
| Catherine Demers | Associate Professor | Division of Cardiology, Department of Medicine, McMaster University |
| Alba Dicenso | Professor | School of Nursing, McMaster University |
| Mita Giacomini | Professor | Centre of Health Economics & Policy Analysis, Department of Clinical Epidemiology & Biostatistics |
| Ron Goeree | Director | Programs for Assessment of Technology in Health (PATH) Research Institute, St. Joseph’s Healthcare Hamilton |
| Nick Kates | Senior Medical Advisor | Health Quality Ontario – QI McMaster University Hamilton Family Health Team |
| Murray Krahn | Director | Toronto Health Economics and Technology Assessment (THETA) Collaborative, University of Toronto |
| Wendy Levinson | Sir John and Lady Eaton Professor and Chair | Department of Medicine, University of Toronto |
| Raymond Pong | Senior Research Fellow and Professor | Centre for Rural and Northern Health Research and Northern Ontario School of Medicine, Laurentian University |
| Michael Schull | Deputy CEO & Senior Scientist | Institute for Clinical Evaluative Sciences |
| Moira Stewart | Director | Centre for Studies in Family Medicine, University of Western Ontario |
| Walter Wodchis | Associate Professor | Institute of Health Management Policy and Evaluation, University of Toronto |
Appendices
Appendix 1: Literature Search Strategies
Search date: January 29th, 2012
Databases searched: OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, Wiley Cochrane, EBSCO CINAHL, Centre for Reviews and Dissemination.
Limits: no year limit; English; NOT comments, editorials, letters
Database: Ovid MEDLINE(R) <1946 to January Week 3 2012>, Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations <January 27, 2012>, Embase <1980 to 2012 Week 04>
Search Strategy:
| # | Searches | Results |
| 1 | exp Coronary Artery Disease/ | 212075 |
| 2 | exp Myocardial Infarction/ use mesz | 133578 |
| 3 | exp heart infarction/ use emez | 216992 |
| 4 | (coronary artery disease or cad or heart attack).ti. | 44463 |
| 5 | ((myocardi* or heart or cardiac or coronary) adj2 (atheroscleros* or arterioscleros* or infarct*)).ti. | 149559 |
| 6 | or/1-5 | 539975 |
| 7 | exp Atrial Fibrillation/ use mesz | 28093 |
| 8 | exp heart atrium fibrillation/ use emez | 55522 |
| 9 | ((atrial or atrium or auricular) adj1 fibrillation*).ti,ab. | 73540 |
| 10 | or/7-9 | 99451 |
| 11 | exp heart failure/ | 300981 |
| 12 | ((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)).ti,ab. | 234590 |
| 13 | 11 or 12 | 381953 |
| 14 | exp Stroke/ | 178088 |
| 15 | exp Ischemic Attack, Transient/ use mesz | 16370 |
| 16 | exp transient ischemic attack/ use emez | 19680 |
| 17 | exp stroke patient/ use emez | 5637 |
| 18 | exp brain infarction/ or exp cerebrovascular accident/ use emez | 101006 |
| 19 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA).ti,ab. | 281375 |
| 20 | or/14-19 | 391798 |
| 21 | exp Diabetes Mellitus, Type 2/ use mesz | 68223 |
| 22 | exp non insulin dependent diabetes mellitus/ use emez | 101711 |
| 23 | exp diabetic patient/ use emez | 12920 |
| 24 | (diabetes or diabetic* or niddm or t2dm).ti,ab. | 765351 |
| 25 | or/21-24 | 790292 |
| 26 | exp Skin Ulcer/ | 72073 |
| 27 | ((pressure or bed or skin) adj2 (ulcer* or sore* or wound*)).ti,ab. | 28723 |
| 28 | (decubitus or bedsore*).ti,ab. | 8532 |
| 29 | or/26-28 | 90816 |
| 30 | exp Pulmonary Disease, Chronic Obstructive/ use mesz | 17049 |
| 31 | exp chronic obstructive lung disease/ use emez | 54779 |
| 32 | (chronic obstructive adj2 (lung* or pulmonary or airway* or airflow or respiratory) adj (disease* or disorder*)).ti,ab. | 54491 |
| 33 | (copd or coad).ti,ab. | 45716 |
| 34 | chronic airflow obstruction.ti,ab. | 1063 |
| 35 | exp Emphysema/ | 37444 |
| 36 | exp chronic bronchitis/ use emez | 6985 |
| 37 | ((chronic adj2 bronchitis) or emphysema).ti,ab. | 50848 |
| 38 | or/30-37 | 159366 |
| 39 | exp Chronic Disease/ | 340792 |
| 40 | ((chronic* adj2 disease*) or (chronic* adj2 ill*)).ti,ab. | 220217 |
| 41 | 39 or 40 | 506604 |
| 42 | exp Comorbidity/ | 143585 |
| 43 | (comorbid* or co-morbid* or multimorbid* or multi-morbid* or (complex* adj patient*) or “patient* with multiple” or (multiple adj2 (condition* or disease*))).ti,ab. | 203652 |
| 44 | 42 or 43 | 284365 |
| 45 | 6 or 10 or 13 or 20 or 25 or 29 or 38 or 41 or 44 | 2823779 |
| 46 | *“Appointments and Schedules”/ use mesz | 3033 |
| 47 | *Health Services Accessibility/ use mesz | 19867 |
| 48 | *Patient-Centered Care/ use mesz | 4514 |
| 49 | ((patient-driven or patientdriven or patient-centered or patientcentered or patient-centred or patientcentred or same-day or sameday) adj2 (access* or appointment* or booking? or schedul*)).ti,ab. | 218 |
| 50 | ((advanced adj2 access*) or (enhanc* adj access*) or ((advanc* access or open access) adj (appointment* or schedul*))).ti,ab. | 1613 |
| 51 | *Health Care Access/ use emez | 4305 |
| 52 | Patient Scheduling/ use emez | 736 |
| 53 | or/46-49,51-52 | 32391 |
| 54 | (45 and 53) or 50 | 3971 |
| 55 | Case Reports/ or Comment.pt. or Editorial.pt. or Letter.pt. use mesz | 2912209 |
| 56 | Case Report/ or Editorial/ or Letter/ use emez | 4609309 |
| 57 | 54 not (55 or 56) | 3672 |
| 58 | limit 57 to english language | 3529 |
| 59 | remove duplicates from 58 Ovid MEDLINE(R) <1946 to January Week 3 2012> (1518) Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations <January 27, 2012> (31) Embase <1980 to 2012 Week 04> (1208) |
2757 |
CINAHL
| # | Query | Limiters/Expanders | Results |
| S43 | (S34 AND S41) OR S40 | Limiters - English Language; Exclude MEDLINE records Search modes - Boolean/Phrase |
560 |
| S42 | (S34 AND S41) OR S40 | Search modes - Boolean/Phrase |
1883 |
| S41 | S35 OR S36 OR S37 OR S38 OR S39 | Search modes - Boolean/Phrase |
22053 |
| S40 | (advanced N2 access*) OR (enhanc* N1 access*) OR ((advanc* access OR open access) N1 (appointment* OR schedul*)) | Search modes - Boolean/Phrase |
379 |
| S39 | (patient-driven OR patientdriven OR patient-centered OR patientcentered OR patient-centred OR patientcentred OR same-day OR sameday) N2 (access* OR appointment* OR booking? OR schedul*) |
Search modes - Boolean/Phrase |
59 |
| S38 | (MM “Patient Centered Care”) | Search modes - Boolean/Phrase |
4423 |
| S37 | (MM “Health Services Accessibility+”) | Search modes - Boolean/Phrase |
14763 |
| S36 | (MM “Appointment and Scheduling Information Systems”) | Search modes - Boolean/Phrase |
69 |
| S35 | (MM “Appointments and Schedules+”) | Search modes - Boolean/Phrase |
2997 |
| S34 | S5 OR S8 OR S11 OR S15 OR S19 OR S22 OR S27 OR S30 OR S33 | Search modes - Boolean/Phrase |
221088 |
| S33 | S31 OR S32 | Search modes - Boolean/Phrase |
28945 |
| S32 | comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* N1 patient*) OR “patient* with multiple” OR (multiple N2 (condition* OR disease*)) | Search modes - Boolean/Phrase |
28945 |
| S31 | (MH “Comorbidity”) | Search modes - Boolean/Phrase |
16646 |
| S30 | S28 OR S29 | Search modes - Boolean/Phrase |
43734 |
| S29 | (chronic* N2 disease*) OR (chronic* N2 ill*) | Search modes - Boolean/Phrase |
43734 |
| S28 | (MH “Chronic Disease”) | Search modes - Boolean/Phrase |
23647 |
| S27 | S23 OR S24 OR S25 OR S26 | Search modes - Boolean/Phrase |
8774 |
| S26 | chronic N2 bronchitis OR emphysema | Search modes - Boolean/Phrase |
1820 |
| S25 | (MH “Emphysema”) | Search modes - Boolean/Phrase |
885 |
| S24 | chronic obstructive N2 disease* OR chronic obstructive N2 disorder* OR copd OR coad | Search modes - Boolean/Phrase |
7349 |
| S23 | (MH “Pulmonary Disease, Chronic Obstructive+”) | Search modes - Boolean/Phrase |
5342 |
| S22 | S20 OR S21 | Search modes - Boolean/Phrase |
16179 |
| S21 | pressure N1 ulcer* OR bedsore* OR bed N1 sore* OR skin N1 ulcer* OR pressure N1 wound* OR decubitus | Search modes - Boolean/Phrase |
9574 |
| S20 | (MH “Skin Ulcer+”) | Search modes - Boolean/Phrase |
14845 |
| S19 | S16 OR S17 OR S18 | Search modes - Boolean/Phrase |
70185 |
| S18 | diabetes OR diabetic* OR niddm OR t2dm | Search modes - Boolean/Phrase |
70185 |
| S17 | (MH “Diabetic Patients”) | Search modes - Boolean/Phrase |
3536 |
| S16 | (MH “Diabetes Mellitus, Type 2”) | Search modes - Boolean/Phrase |
18233 |
| S15 | S12 OR S13 OR S14 | Search modes - Boolean/Phrase |
38210 |
| S14 | stroke OR tia OR transient ischemic attack OR cerebrovascular apoplexy OR cerebrovascular accident OR cerebrovascular infarct* OR brain infarct* OR CVA | Search modes - Boolean/Phrase |
37713 |
| S13 | (MH “Cerebral Ischemia, Transient”) | Search modes - Boolean/Phrase |
1903 |
| S12 | (MH “Stroke”) OR (MH “Stroke Patients”) | Search modes - Boolean/Phrase |
25676 |
| S11 | S9 OR S10 | Search modes - Boolean/Phrase |
18862 |
| S10 | myocardi* failure OR myocardial decompensation OR myocardial insufficiency OR cardiac failure OR cardiac decompensation OR cardiac insufficiency OR heart failure OR heart decompensation OR heart insufficiency | Search modes - Boolean/Phrase |
18850 |
| S9 | (MH “Heart Failure+”) | Search modes - Boolean/Phrase |
14393 |
| S8 | S6 OR S7 | Search modes - Boolean/Phrase |
8072 |
| S7 | atrial N1 fibrillation* OR atrium N1 fibrillation* OR auricular N1 fibrillation* | Search modes - Boolean/Phrase |
8072 |
| S6 | (MH “Atrial Fibrillation”) | Search modes - Boolean/Phrase |
6490 |
| S5 | S1 OR S2 OR S3 OR S4 | Search modes - Boolean/Phrase |
30133 |
| S4 | TI myocardi* N2 infarct* OR TI heart N2 infarct* OR TI cardiac N2 infarct* OR TI coronary N2 infarct* OR TI arterioscleros* OR TI atheroscleros* | Search modes - Boolean/Phrase |
9643 |
| S3 | coronary artery disease OR cad OR heart attack* | Search modes - Boolean/Phrase |
7706 |
| S2 | (MH “Myocardial Infarction+”) | Search modes - Boolean/Phrase |
19219 |
| S1 | (MH “Coronary Arteriosclerosis”) | Search modes - Boolean/Phrase |
4646 |
Wiley Cochrane
| ID | Search | Hits |
| #1 | MeSH descriptor Coronary Artery Disease explode all trees | 2183 |
| #2 | MeSH descriptor Myocardial Infarction explode all trees | 7746 |
| #3 | (myocardi* or heart or cardiac or coronary) NEAR/2 (atheroscleros* or arterioscleros* or infarct*):ti or (coronary artery disease or cad or heart attack*):ti | 8469 |
| #4 | MeSH descriptor Atrial Fibrillation explode all trees | 2102 |
| #5 | (atrial NEAR/2 fibrillation* or atrium NEAR/2 fibrillation* or auricular NEAR/2 fibrillation*):ti | 2310 |
| #6 | MeSH descriptor Heart Failure explode all trees | 4710 |
| #7 | (myocardi* NEAR/2 (failure or decompensation or insufficiency)):ti or (heart NEAR/2 (failure or decompensation or insufficiency)):ti or (cardiac NEAR/2 (failure or decompensation or insufficiency)):ti | 5252 |
| #8 | MeSH descriptor Stroke explode all trees | 3899 |
| #9 | MeSH descriptor Ischemic Attack, Transient explode all trees | 466 |
| #10 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA):ti | 9902 |
| #11 | MeSH descriptor Diabetes Mellitus, Type 2 explode all trees | 6993 |
| #12 | (diabetes or diabetic* or niddm or t2dm):ti | 16585 |
| #13 | MeSH descriptor Skin Ulcer explode all trees | 1572 |
| #14 | (pressure or bed or skin) NEAR/2 (ulcer* or sore* or wound*):ti | 669 |
| #15 | (decubitus or bedsore*):ti | 98 |
| #16 | MeSH descriptor Pulmonary Disease, Chronic Obstructive explode all trees | 1754 |
| #17 | (chronic obstructive NEAR/2 (lung* or pulmonary or airway* or airflow or respiratory)):ti | 2415 |
| #18 | (copd or coad):ti | 3319 |
| #19 | (chronic airflow obstruction):ti | 72 |
| #20 | MeSH descriptor Emphysema explode all trees | 91 |
| #21 | (chronic NEAR/2 bronchitis) or emphysema:ti | 1183 |
| #22 | (Chronic Disease):ti | 4464 |
| #23 | (chronic* NEAR/2 disease* or chronic* NEAR/2 ill*):ti | 1670 |
| #24 | MeSH descriptor Comorbidity explode all trees | 1941 |
| #25 | (comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* NEXT patient*) OR “patient* with multiple” OR (multiple NEAR/2 (condition* OR disease*))):ti | 649 |
| #26 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25) | 61123 |
| #27 | MeSH descriptor Appointments and Schedules, this term only | 295 |
| #28 | MeSH descriptor Health Services Accessibility, this term only | 410 |
| #29 | MeSH descriptor Patient-Centered Care explode all trees | 203 |
| #30 | (patient-driven or patientdriven or patient-centered or patientcentered or patient-centred or patientcentred or same-day or sameday) NEAR/2 (access* or appointment* or booking? or schedul*):ti,ab,kw | 13 |
| #31 | (advanced NEAR/2 access*) or (enhanc* NEXT access*) or ((advanc* access or open access) NEXT (appointment* or schedul*)):ti,ab,kw | 26 |
| #32 | (#27 OR #28 OR #29 OR #30) | 902 |
| #33 | (( #26 AND #32) OR #31) | 119 |
Centre for Reviews and Dissemination
| Line | Search | Hits |
| 1 | MeSH DESCRIPTOR coronary artery disease EXPLODE ALL TREES | 230 |
| 2 | (coronary artery disease or cad or heart attack*):TI | 213 |
| 3 | ((myocardi* or heart or cardiac or coronary) adj2 (atheroscleros* or arterioscleros* or infarct*)):TI | 224 |
| 4 | MeSH DESCRIPTOR Atrial Fibrillation EXPLODE ALL TREES | 225 |
| 5 | (((atrial or atrium or auricular) adj1 fibrillation*):TI | 0 |
| 6 | ((atrial or atrium or auricular) adj1 fibrillation*):TI | 168 |
| 7 | MeSH DESCRIPTOR heart failure EXPLODE ALL TREES | 418 |
| 8 | ((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)):TI | 280 |
| 9 | MeSH DESCRIPTOR stroke EXPLODE ALL TREES | 549 |
| 10 | MeSH DESCRIPTOR Ischemic Attack, Transient EXPLODE ALL TREES | 32 |
| 11 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA):TI | 622 |
| 12 | MeSH DESCRIPTOR Diabetes Mellitus, Type 2 EXPLODE ALL TREES | 511 |
| 13 | (diabetes or diabetic* or niddm or t2dm):TI | 1223 |
| 14 | MeSH DESCRIPTOR Skin Ulcer EXPLODE ALL TREES | 253 |
| 15 | ((pressure or bed or skin) adj2 (ulcer* or sore* or wound*)):TI | 73 |
| 16 | ( decubitus or bedsore*):TI | 0 |
| 17 | MeSH DESCRIPTOR Pulmonary Disease, Chronic Obstructive EXPLODE ALL TREES | 237 |
| 18 | (chronic obstructive adj2 (lung* or pulmonary or airway* or airflow or respiratory)):TI | 219 |
| 19 | (copd or coad):TI | 108 |
| 20 | (chronic airflow obstruction):TI | 0 |
| 21 | MeSH DESCRIPTOR Emphysema EXPLODE ALL TREES | 10 |
| 22 | ((chronic adj2 bronchitis) or emphysema):TI | 47 |
| 23 | MeSH DESCRIPTOR Chronic Disease EXPLODE ALL TREES | 687 |
| 24 | ((chronic* adj2 disease*) or (chronic* adj2 ill*)):TI | 252 |
| 25 | MeSH DESCRIPTOR Comorbidity EXPLODE ALL TREES | 146 |
| 26 | (comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* adj1 patient*) OR “patient* with multiple” OR (multiple adj2 (condition* OR disease*))):TI | 22 |
| 27 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 | 4656 |
| 28 | MeSH DESCRIPTOR Appointments and Schedules EXPLODE ALL TREES | 84 |
| 29 | MeSH DESCRIPTOR Health Services Accessibility EXPLODE ALL TREES | 197 |
| 30 | MeSH DESCRIPTOR Patient-Centered Care EXPLODE ALL TREES | 40 |
| 31 | ((patient-driven or patientdriven or patient-centered or patientcentered or patient-centred or patientcentred or same-day or sameday) adj2 (access* or appointment* or booking? or schedul*)):TI | 2 |
| 32 | ((advanced adj2 access*) or (enhanc* adj1 access*) or ((advanc* access or open access) adj1 (appointment* or schedul*))):TI | 2 |
| 33 | #28 OR #29 OR #30 OR #31 | 310 |
| 34 | #27 AND #33 | 24 |
| 35 | #32 OR #34 | 26 |
Appendix 2: GRADE Tables and Risk of Bias Assessment
Table A1: GRADE Evidence Profile for Advanced Access in a Diabetes Population.
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Hospitalization | |||||||
| 2 (observational, 1 with concurrent controls) | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Emergency Department/Urgent Care Visits | |||||||
| 2 (observational, 1 with concurrent controls) | No serious limitations | Serious limitations (-1) | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Length of Stay | |||||||
| 1 (observational) | Serious limitations (-1)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| HbA1c | |||||||
| 3 (observational, 1 with concurrent controls) | No serious limitations | Serious limitations (-1) | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| LDL-C | |||||||
| 3 (observational, 1 with concurrent controls) | No serious limitations | Serious limitations (-1) | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Blood Pressure | |||||||
| 2 (observational, 1 with concurrent controls) | No serious limitations | Serious limitations (-1) | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
Abbreviations: HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; NA, not applicable.
Measure used (percent of patients admitted for greater than 3 days) was not explained and may not be valid.
Table A2: GRADE Evidence Profile for Advanced Access in a CAD/CHD Population.
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Hospitalization | |||||||
| 1 (observational) | Serious limitations (-1)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Emergency Department Visits | |||||||
| 1 (observational) | Serious limitations (-1)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Length of Stay | |||||||
| 1 (observational) | Serious limitations (-1)a,b | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| LDL-C | |||||||
| 1 (observational) | Serious limitations (-1)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Blood Pressure | |||||||
| 1 (observational) | Serious limitations (-1)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
Abbreviations: CAD, coronary artery disease; CHD, coronary heart disease; LDL-C, low-density lipoprotein cholesterol; NA, not applicable.
Study included patients in multiple cohorts, with attribution of outcomes to all in outcome assessment.
Measure used (percent of patients admitted for greater than 3 days) was not explained and may not be valid.
Table A3: GRADE Evidence Profile for Advanced Access in a Geriatric Population.
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Patient Satisfaction | |||||||
| 1 (observational) | Very serious limitations (-2)a | NA | No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
Abbreviation: NA, not applicable.
Intervention was altered part way through study, and no statistical analyses are reported.
Table A4: EPOC Risk of Bias Assessment—Observational Study With Contemporaneous Controls.
| Study | Allocation | Baseline Outcome Measurement | Baseline Characteristics | Incomplete Date | Intervention Allocation Concealed | Management of Missing Data | Free from Selective Outcome Reporting | Other Sources of Bias |
|---|---|---|---|---|---|---|---|---|
| Subramanian et al (28) | No Sites self-selected participation in intervention or control |
Unclear These were reported, but no statistical tests provided |
No Intervention and control sites differed significantly on a number of clinic and patient characteristics |
No | Unclear Not reported. Outcomes assessed using administrative data, but unclear whether those assessing outcomes were aware of intervention status |
Yes | Yes | Yes |
Abbreviations: EPOC, Effective Practice and Organization of Care.
Table A5: EPOC Risk of Bias Assessment—Observational Studies With Historical Controls.
| Study | Independent of Other Changes | Intervention Effect Prespecified | Intervention Affected Data Collection | Incomplete Data Addressed | Free from Selective Outcome Reporting | Other Sources of Bias |
|---|---|---|---|---|---|---|
| Solberg et al (24); Sperl-Hillen et al (25) | No Authors reported the implementation of a diabetes care program during the same period |
Yes | No | Unclear Sample sizes varied across time (cohorts differ) and the authors did not discuss use of services outside of the system |
Yes | Yes |
| Gladstone et al (29) | Unclear Authors did not account for other changes occurring in the practice |
Yes | No | Unclear Authors did not report on missing data and excluded people who were not seen after implementation |
Yes | Yes |
| Cherniack et al (18) | Unclear Authors did not discuss other initiatives that may have been underway |
No There was a change in clinic structure part way through the intervention |
Unclear Data collection was based on the appointment system and may have changed with implementation |
Unclear Authors did not report rates by patient and did not report missing data rates |
Yes | Yes |
Abbreviations: EPOC, Effective Practice and Organization of Care.
Suggested Citation
This report should be cited as follows: Degani N. Impact of advanced (open) access scheduling on patients with chronic diseases: an evidence-based analysis. Ont Health Technol Assess Ser [Internet]. 2013 September;13(7):1–48. Available from: http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-advanced-access-scheduling.pdf.
Indexing
The Ontario Health Technology Assessment Series is currently indexed in MEDLINE/PubMed, Excerpta Medica/EMBASE, and the Centre for Reviews and Dissemination database.
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to: EvidenceInfo@hqontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Conflict of Interest Statement
All reports in the Ontario Health Technology Assessment Series are impartial. There are no competing interests or conflicts of interest to declare.
Peer Review
All reports in the Ontario Health Technology Assessment Series are subject to external expert peer review. Additionally, Health Quality Ontario posts draft reports and recommendations on its website for public comment prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
Health Quality Ontario
130 Bloor Street West, 10th Floor
Toronto, Ontario
M5S 1N5
Tel: 416-323-6868
Toll Free: 1-866-623-6868
Fax: 416-323-9261
Email: EvidenceInfo@hqontario.ca
ISSN 1915-7398 (online)
ISBN 978-1-4606-1240-8 (PDF)
© Queen’s Printer for Ontario, 2013
About Health Quality Ontario
Health Quality Ontario (HQO) is an arms-length agency of the Ontario government. It is a partner and leader in transforming Ontario’s health care system so that it can deliver a better experience of care, better outcomes for Ontarians and better value for money.
Health Quality Ontario strives to promote health care that is supported by the best available scientific evidence. HQO works with clinical experts, scientific collaborators and field evaluation partners to develop and publish research that evaluates the effectiveness and cost-effectiveness of health technologies and services in Ontario.
Based on the research conducted by HQO and its partners, the Ontario Health Technology Advisory Committee (OHTAC) — a standing advisory sub-committee of the HQO Board — makes recommendations about the uptake, diffusion, distribution or removal of health interventions to Ontario’s Ministry of Health and Long-Term Care, clinicians, health system leaders and policy-makers.
This research is published as part of Ontario Health Technology Assessment Series, which is indexed in CINAHL, EMBASE, MEDLINE, and the Centre for Reviews and Dissemination. Corresponding OHTAC recommendations and other associated reports are also published on the HQO website. Visit http://www.hqontario.ca for more information.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, HQO and/or its research partners reviews the available scientific literature, making every effort to consider all relevant national and international research; collaborates with partners across relevant government branches; consults with clinical and other external experts and developers of new health technologies; and solicits any necessary supplemental information.
In addition, HQO collects and analyzes information about how a health intervention fits within current practice and existing treatment alternatives. Details about the diffusion of the intervention into current health care practices in Ontario add an important dimension to the review. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social, and legal issues relating to the intervention assist in making timely and relevant decisions to optimize patient outcomes.
The public consultation process is available to individuals and organizations wishing to comment on reports and recommendations prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
Disclaimer
This report was prepared by HQO or one of its research partners for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research. It also incorporates, when available, Ontario data and information provided by experts and applicants to HQO. It is possible that relevant scientific findings may have been reported since completion of the review. This report is current to the date of the literature review specified in the methods section, if available. This analysis may be superseded by an updated publication on the same topic. Please check the HQO website for a list of all publications: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
List of Tables
| Table 1: Body of Evidence Examined According to Study Design |
| Table 2: Systematic Review—Outcomes, Measures, and Results |
| Table 3: Description of Study Elements and Outcomesa |
| Table 4: Impact of Advanced Access Implementation on Hospitalization Ratesa |
| Table 5: Impact of Advanced Access Implementation on Emergency Department/Urgent Care Visitsa |
| Table 6: Impact of Advanced Access Implementation on Acute Care Length of Stay |
| Table 7: Impact of Advanced Access Implementation on Disease-Specific Clinical Outcomesa |
| Table 8: Summary of Findings |
| Table A1: GRADE Evidence Profile for Advanced Access in a Diabetes Population |
| Table A2: GRADE Evidence Profile for Advanced Access in a CAD/CHD Population |
| Table A3: GRADE Evidence Profile for Advanced Access in a Geriatric Population |
| Table A4: EPOC Risk of Bias Assessment—Observational Study With Contemporaneous Controls |
| Table A5: EPOC Risk of Bias Assessment—Observational Studies With Historical Controls |
List of Figures
| Figure 1: Citation Flow Chart |
List of Abbreviations
- CAD
Coronary artery disease
- CHD
Coronary heart disease
- CI
Confidence interval
- ED
Emergency department
- EPOC
Effective Practice and Organization of Care
- HbA1c
Hemoglobin A1c
- LDL-C
Low density lipoprotein cholesterol
- LOS
Length of stay
- OA
Open access (alternate term for advanced access)
- RCT
Randomized controlled trial
- SBP
Systolic blood pressure
References
- 1.Institute of Medicine Committee on Quality of Health Care in America. Cross the quality chasm: a new health system for the 21st century [Internet]. Washington, DC: National Academies Press; 2001. [[cited 2013 Jun 24]. 337 p.]. Available from: http://www.nap.edu/catalog.php?record_id=10027 .
- 2.Schoen C, Osborn R, Squires D, Doty MM, Pierson R, Applebaum S, et al. How health insurance design affects access to care and costs, by income, in eleven countries. Health Aff (Millwood) 2010 Dec;29(12):2323–34. doi: 10.1377/hlthaff.2010.0862. [DOI] [PubMed] [Google Scholar]
- 3.MacKinnon NJ, Sanmartin C. Middle of the health care pack: Canada’s performance in the 2007 Commonwealth Fund international survey. Can Fam Physician. 2008 Jul;54(7):965–1. [PMC free article] [PubMed] [Google Scholar]
- 4.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Standing Senate Committee on Social Affairs. The health of Canadians - the federal role. Volume 6: Recommendations for reform [Internet] [[cited 2012 Jun 11]. 325 p.];Ottawa (ON): Standing Senate Committee on Social Affairs. 2002 Oct;1 Available from: http://www.parl.gc.ca/Content/SEN/Committee/372/soci/rep/repoct02vol6-e.pdf . [Google Scholar]
- 6.Berta W, Barnsley J, Brown A, Murray M. In the eyes of the beholder: population perspectives on performance priorities for primary care in Canada. Healthc Policy. 2008 Nov;4(2):86–100. [PMC free article] [PubMed] [Google Scholar]
- 7.Murray MD, Tantau C. Same-day appointments: exploding the access paradigm. Fam Pract Manag. 2000;7(8):45–50. [PubMed] [Google Scholar]
- 8.Tantau C. Accessing patient-centered care using the advanced access model. J Ambulatory Care Manage. 2009;32(1):32–43. doi: 10.1097/01.JAC.0000343122.15467.48. [DOI] [PubMed] [Google Scholar]
- 9.Murray M, Bodenheimer T, Rittenhouse D, Grumbach K. Improving timely access to primary care: case studies of the advanced access model. JAMA. 2003;289(8):1042–6. doi: 10.1001/jama.289.8.1042. [DOI] [PubMed] [Google Scholar]
- 10.Pickin M, O’Cathain A, Sampson FC, Dixon S. Evaluation of advanced access in the national primary care collaborative. Br J Gen Pract. 2004;54(502):334–40. [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong B, Levesque O, Perlin JB, Rick C, Schectman G. Reinventing veterans health administration: focus on primary care. J Healthc Manag. 2005;50(6):399–408. [PubMed] [Google Scholar]
- 12.Goodall S, Montgomery A, Banks J, Salisbury C, Sampson F, Pickin M. Implementation of advanced access in general practice: postal survey of practices. Br J Gen Pract. 2006;56(533):918–23. [PMC free article] [PubMed] [Google Scholar]
- 13.Pope C, Banks J, Salisbury C, Lattimer V. Improving access to primary care: eight case studies of introducing advanced access in England. J Health Serv Res Policy. 2008;13(1):33–9. doi: 10.1258/jhsrp.2007.007039. [DOI] [PubMed] [Google Scholar]
- 14.Mehrotra A, Keehl-Markowitz L, Ayanian JZ. Implementing open-access scheduling of visits in primary care practices: a cautionary tale. Ann Intern Med. 2008;148(12):915–22. doi: 10.7326/0003-4819-148-12-200806170-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phan K, Brown SR. Decreased continuity in a residency clinic: a consequence of open access scheduling. Fam Med. 2009;41(1):46–50. [PubMed] [Google Scholar]
- 16.Mainous III AG, Salisbury C. Advanced access, open access, and continuity of care: Should we enforce continuity? Fam Med. 2009;41(1):57–8. [PubMed] [Google Scholar]
- 17.O’Connor ME, Matthews BS, Gao D. Effect of open access scheduling on missed appointments, immunizations, and continuity of care for infant well-child care visits. Arch Pediatr Adolesc Med. 2006 Sep;160(9):889–93. doi: 10.1001/archpedi.160.9.889. [DOI] [PubMed] [Google Scholar]
- 18.Cherniack EP, Sandals L, Gillespie D, Maymi E, Aguilar E. The use of open-access scheduling for the elderly. J Healthc Qual. 2007;29(6):45–8. doi: 10.1111/j.1945-1474.2007.tb00224.x. [DOI] [PubMed] [Google Scholar]
- 19.Dixon S, Sampson FC. O’Cathain A, Pickin M. Advanced access: more than just GP waiting times? Fam Pract. 2006;23(2):233–9. doi: 10.1093/fampra/cmi104. [DOI] [PubMed] [Google Scholar]
- 20.Health Quality Ontario. Wave 5 Outreach Information Package: Advanced access, efficiency and chronic disease management in primary care [Internet] Toronto, ON: Health Quality Ontario. [[updated 2012; cited 2012 Aug 1]]. Available from: http://hqolc.ca/documents/wave-5/pcwave5outreachinfopackageenaugust8pdf .
- 21.Murray M, Berwick DM. Advanced access: reducing waiting and delays in primary care. JAMA. 2003;289(8):1035–40. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 22.Guyatt G, Oxman A, Schunemann H, Tugwell P, Knottnerus A. GRADE Guidelines: a new series od articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380–2. doi: 10.1016/j.jclinepi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Cochrane Effective Practice and Organisation of Care Group. Suggested risk of bias criteria for EPOC reviews [Internet] New York: Cochrane Collaboration [Internet] [[updated 2012; cited 2012 Jun 11]]. Available from: http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/Suggested%20risk%20of%20bias %20criteria%20for%20EPOC%20reviews.pdf .
- 24.Solberg LI, Maciosek MV, Sperl-Hillen JM, Crain AL, Engebretson KI, Asplin BR et al. Does improved access to care affect utilization and costs for patients with chronic conditions? Am J Manag Care. 2004;10(10):717–22. [PubMed] [Google Scholar]
- 25.Sperl-Hillen JM, Solberg LI, Hroscikoski MC, Crain AL, Engebretson KI, O’Connor PJ. The effect of advanced access implementation on quality of diabetes care. Prev Chronic Dis. 2008;5(1):A16. [PMC free article] [PubMed] [Google Scholar]
- 26.Goodman C. Literature searching and evidence interpretation for assessing health care practices. [Stockhold]. [[cited: 2012 Jun 1]. 81 p. SBU Report No. 119E.];Sweden: Swedish Council on Technology Assessment in Health Care. 1996 doi: 10.1017/s0266462300008321. [DOI] [PubMed] [Google Scholar]
- 27.Rose KD, Ross JS, Horwitz LI. Advanced access scheduling outcomes: a systematic review. Arch Intern Med. 2011;171(13):1150–9. doi: 10.1001/archinternmed.2011.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subramanian U, Ackermann RT, Brizendine EJ, Saha C, Rosenman MB, Willis DR et al. Effect of advanced access scheduling on processes and intermediate outcomes of diabetes care and utilization. J Gen Intern Med. 2009;24(3):327–33. doi: 10.1007/s11606-008-0888-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gladstone J, Howard M. Effect of advanced access scheduling on chronic health care in a Canadian practice. Can Fam Physician. 2011;57(1):e21–e25. [PMC free article] [PubMed] [Google Scholar]
- 30.Solberg LI, Hroscikoski MC, Sperl-Hillen JM, O’Connor PJ, Crabtree BF. Key issues in transforming health care organizations for quality: the case of advanced access. Jt Comm J Qual Saf. 2004;30(1):15–24. doi: 10.1016/s1549-3741(04)30002-x. [DOI] [PubMed] [Google Scholar]


