Abstract
Background:
After lumbar or lumbosacral fusion for various spine disorders, adjacent segment disease has been reported. Most of the studies have focused on proximal segment disease. The author has reported sacroiliac joint degeneration in these patients. Based on our own experiences with an increasing number of patients with sacroiliac joint (SIJ) arthralgia after multi-level lumbar or lumbosacral fusion procedures, we evaluated a surgical procedure called distraction arthrodesis of the SIJ for patients with refractory severe pain of the SIJ.
Materials and Methods:
Nineteen (19) consecutive patients were recruited and evaluated prospectively after undergoing distraction arthrodesis of the SIJ. The inclusion criteria for the surgical procedure were degeneration of the SIJ and failed conservative treatment. Magnetic resonance imaging (MRI) scans and CT scans were performed in all cases. The clinical outcome was assessed using the Visual Analog Scale and the Oswestry Disability Index (ODI). CT scans were performed postoperatively and again at the final followup to evaluate assess fusion. The data was analyzed using the SPSS software (version 10.0; SPSS, Chicago, IL) and statistical analysis was performed. The P values were based on the Student t-test.
Results:
The mean followup was 13.2 months. All patients had an instrumented lumbar or lumbosacral fusion. The overall fusion rate of SIJ was 78.9% (15/19 joints). All patients demonstrated significant improvement in VAS and ODI scores compared to preoperative values. The mean VAS score was 8.5 before surgery and was 6 at final followup, demonstrating 30% improvement. The mean ODI scores were 64.1 before surgery and 56.97 at the final followup, demonstrating 12% improvement.
Conclusions:
Refractory sacroiliac pain as a result of multi-level fusion surgery can be successfully treated with minimally invasive arthrodesis. It offers a safe and effective treatment for severe SIJ pain. Careful patient selection is important.
Keywords: Arthrodesis, distraction, interference, recesses, sacroiliac joint
INTRODUCTION
Instrumented lumbar or lumbosacral fusion is often used to treat a variety of spinal disorders. However, adjacent segment degeneration is reported following instrumented fusion segments.1,2 Multiple factors, including the type of surgical procedure, number of levels fused, health of the adjacent segment and sagittal curvature of the lumbar spine, have been implicated. The incidence of adjacent segmental disease has been reported to range from 5.2% to 49%,3 but most of these biomechanical and clinical studies have focused on the proximal segments adjacent to the instrumented lumbar/lumbosacral fusion.
The sacroiliac joint (SIJ) forms the lowest segment of the spine axis and distributes the force coming from the upper body.4 Movements occurring in the SIJ play an important role in distributing the force and is influenced by the movement of the lumbosacral spine.4 According to recent studies,5,6 approximately 15% of patients who reported lower back pain experienced lower back and buttock pain resulting from SIJ arthralgia.
However, only one study7 examined the cause-and-effect relationship between fusion and SIJ degeneration after instrumented posterolateral lumbar or lumbosacral fusion. The authors reported a 75% incidence of SIJ degeneration in the fusion after instrumented lumbar or lumbosacral fusion.7 SIJ degeneration developed more often in patients undergoing lumbosacral fusion, regardless of the number of fusion segments.7 The SIJ is currently subject of discussion in literature as a source of pain after lumbar or lumbosacral fusion and in patients with failed back syndrome.1,2
Authors prefer conservative treatment as first choice.2 Surgical techniques should be offered to patients with inadequate conservative treatment response. More well controlled studies are necessary for further clarifications.2
This study evaluates outcome of patients with SIJ arthralgia after multi-level lumbar or lumbosacral fusion procedures using distraction interference arthrodesis of the SIJ.
MATERIALS AND METHODS
Nineteen (19) consecutive patients who underwent distraction arthrodesis of the SIJ were included in study between May 2010 and November 2011 and evaluated prospectively [Figure 1]. The inclusion criteria for the surgical procedure were degeneration of the SIJ (history, pain drawing and SIJ provocation tests, 75% pain relief after SIJ injection with local anesthesia) and failed conservative treatment. The exclusion criteria consisted of inflammatory diseases and infection. In our practice, all patients with SIJ pain undergo a protocol of vigorous conservative treatment in the form of: (1) medications; (2) physical therapy; (3) a minimum of two CT guided SIJ blocks. To confirm the diagnosis, preoperative plain radiographs, magnetic resonance imaging (MRI) scans and CT scans were performed in all cases. A diagnosis of SIJ degeneration was based on the presence of one or more of the following CT findings: Sclerosis, erosion, osteophyte, joint space narrowing, intraarticular bone fragment and/or subchondral cyst.
Figure 1.
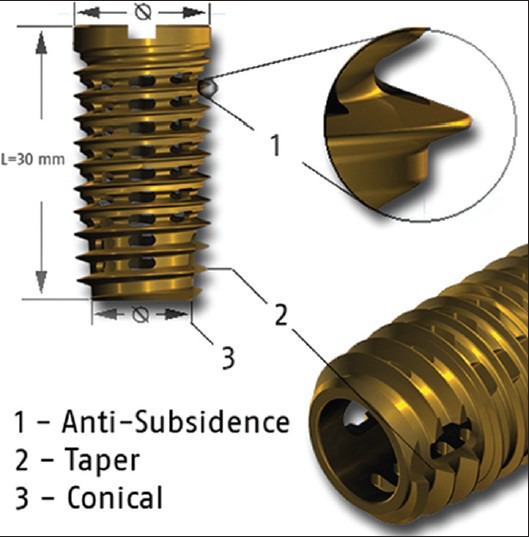
A photograph showing implant, which is available in four sizes. The length for all sizes is 30 mm, the outer and inner diameter is obtainable between 13/12 mm, 15/12 mm, 17/16 mm and 19/18 mm
The clinical outcome was assessed using a pain score based on a 10-point Visual Analog Scale (VAS; range, 1-10). A VAS score of 1 was defined as no pain and a score of 10 was defined as the worst pain imagined by the patient. The patients assessed the pain outcome subjectively. The VAS score was measured before surgery and at the final followup. The outcome was assessed using the Oswestry Disability Index (ODI) at the same time points as the clinical outcome assessments presented with the VAS. The clinical and functional outcomes, characterized by the decrease from baseline in the mean VAS and ODI scores respectively, were compared.
CT scans were performed postoperatively and again at the final followup to evaluate hardware placement and assess fusion. Fusion was identified as a lack of loosening around the implants and positive evidence of bone bridging around the implant from the sacrum to the ilium.
Operative procedure
The skin incision was made about 4-6 cm midline. The extraarticular recess is identified and the bone surfaces were prepared for bone substitute using appropriate curettes and, preferably, a micro burr. Bone substitute (30-40 cc beta-tricalcium-phosphate) was packed into all recesses and spaces with a small instrument. Care was taken to pack the bone substitute into the extension of the joint at the inferior aspect of the extraarticular recess. The next step was insertion of a guide pin into the recess at the S2 transverse process at an angle of approximately 45° to the frontal plane (laterally) and at approximately 45° to a transverse plane (distally). The placement was confirmed by lateral, anteroposterior (AP) and vertical oblique fluoroscope imaging. Then the insertion instruments were applied in order to facilitate the implantation of the hollow screw. The size of the implant was determined by the threaded distractor and by the helix [Figure 1]. Advancement of the instruments was done with rotary motions. The process began with the smallest size. At the end point the surgeon had felt a noticeable resistance. Position was checked with X-rays and c-arm [Figures 2-7].
Figure 2.
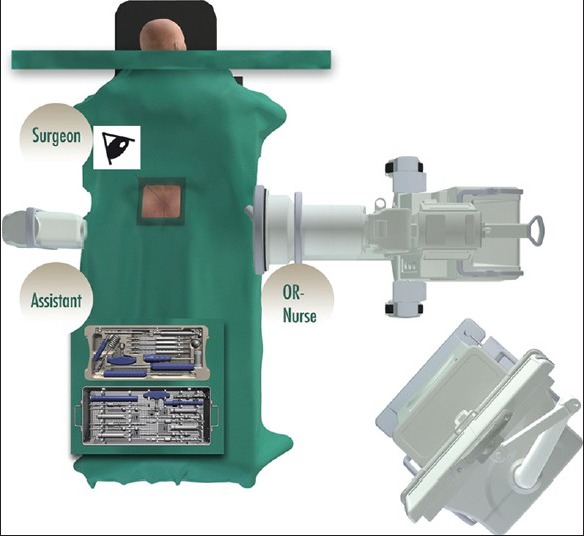
An image showing surgeon on the upper left side. Assistant on the upper right side and the scrub nurse stands on the lower left side. Surgeon and scrub nurse should have an unimpeded view on the monitors of the image intensifier. (Used by permission of SIGNUS-Medizintechnik GmbH)
Figure 7.

Maintenance of the distraction (a) is achieved by the wedge-shaped instrument (b). The preparation of the implant seat was performed with a reamer (c); afterwards, the helical implant could be inserted (d). Final position of the implant in three planes – lateral, a.p., vertical (e-g). (used by permission SIGNUS-Medizintechnik/ Dr. John G. Stark)
Figure 3.

An image showing position of the image intensifier for a vertical oblique imaging. (Used by permission of SIGNUS-Medizintechnik GmbH)
Figure 4.
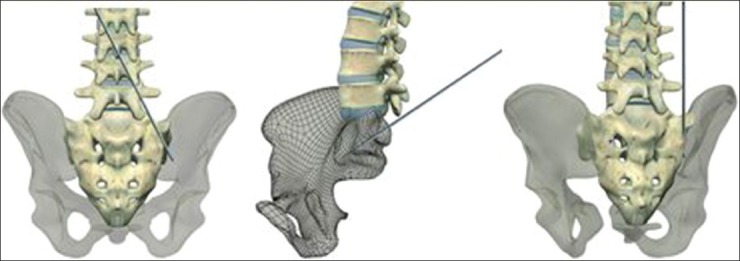
Insertion of the guide pin on the example of the 3D model. (Used by permission of SIGNUS-Medizintechnik GmbH)
Figure 5.

(a) Lateral image showing the guide pin in its correct orientation: The projected trajectory of the guide pin passes through the region of the S1/S2 disc, above the sciatic notch, to the most superior point of the acetabular dome. (b) A-P image showing the guide pin in its correct orientation: The projected trajectory of the guide pin passes through the inferior one third of the visible joint line, above the sciatic notch, to the most superior point of the acetabular dome. (c) The “Vertical”/oblique image showing the guide pin in its correct orientation: The projected trajectory of the guide pin passes vertically through the extraarticular recess, through the anterior column, to the most superior point of the acetabular dome. (SIGNUS-Medizintechnik/ Dr. John G. Stark)
Figure 6.
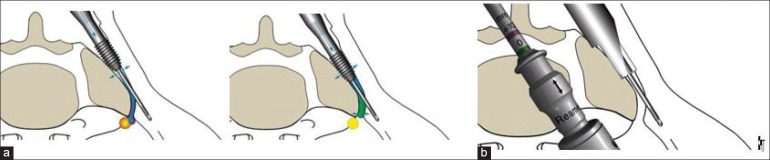
Line diagram showing (a) Joint distraction by incremental use of helical distraction instruments. (b) Wedge-shaped instrument which is positioned over the guide pin. (Used by permission of SIGNUS-Medizintechnik GmbH)
Postoperative care included “toe touch” weight bearing (which was about 10% to 30% body weight) at 6 to 12 weeks with crutches or walker. Avoidance of twisting, bending and lifting for 6 to 12 weeks is also recommended. Vitamin D should be substituted over a period of 6 weeks.
Ethical board approval of the University of Münster, Germany for the current study was obtained.
Statistical analysis
The data was analyzed using the SPSS software (version 10.0; SPSS, Chicago, IL) and statistical analysis was performed. The P values were based on the Student t-test for independent variables. The threshold for statistical significance was established at P ≤ 0.05.
RESULTS
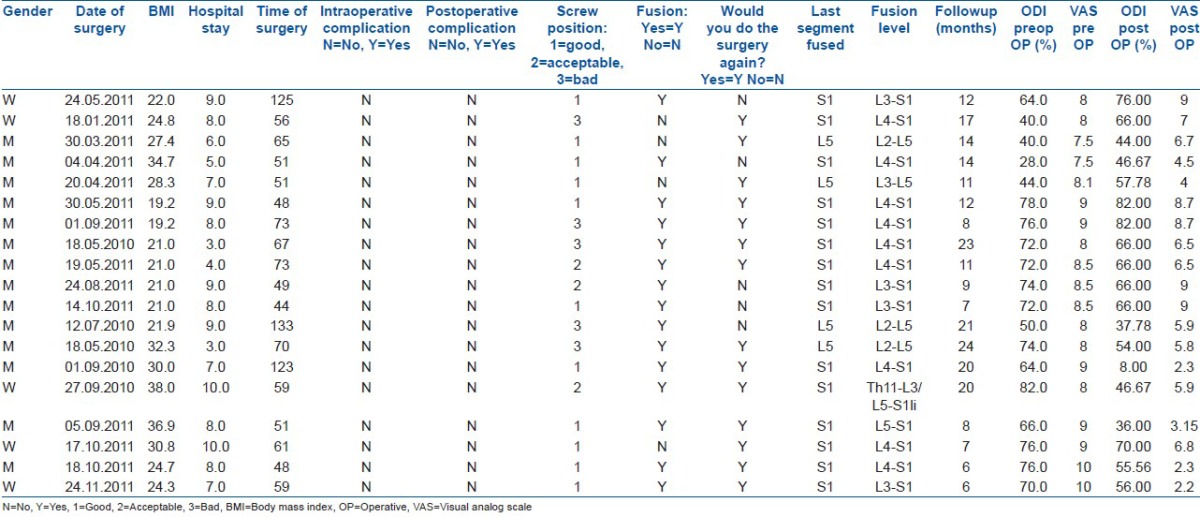
Nineteen (19) patients (14 males/5 females) were included in the final followup. The mean age at the time of surgery was 60.9 years (range 36-76 years, SW: 9.88) and the mean followup period was 13.2 months (range 6-24 months, SW: 5.83). All patients had a multi-level lumbar or lumbosacral fusion at L2-L5 (n = 3); L3-S1 (n = 4); L4-S1 (n = 9); L5-S1 (n = 1); L3-L5 (n = 1); Th11-S1 n = 1) without harvesting an iliac bone graft during the last fusion procedure (all more than 12 month ago). The indication for lumbar surgery was lumbar instability in most cases except one who had a scoliosis and two patients who had lumbar spondyolisthesis. The average body mass index was 26.2 (range 19.2-36.9, SW: 5.87). The average intra-operative blood loss was recorded as <150 mL in all cases. The average length of stay was 7.3 days (range 3-10 days, SW: 2.09;). All patients completed the questionnaires pre-operatively and postoperatively. The overall fusion rate was 78.9% (15/19 joints), as measured at the postoperative CT scan at final followup [Figure 8].
Figure 8.
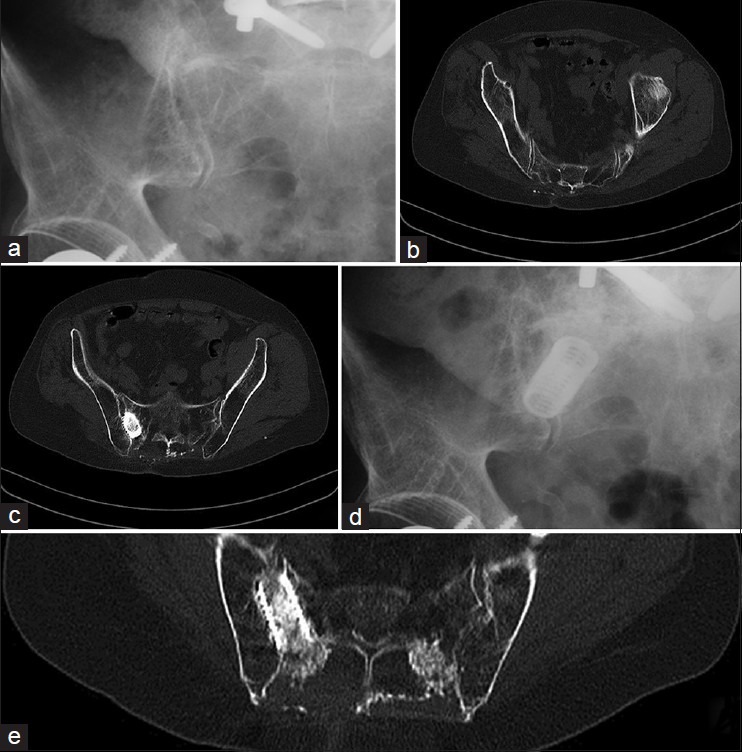
X-rays and CT scans showing arthrodesis of the SI joint. (a) Preoperative X-ray (b) preoperative CT scan showing degenerative arthritis of SI joint, (c) postoperative CT scan showing bone subsitute in position, (d) X-ray at final follow, (e) CT scan at final followup
At final follow up, all patients demonstrated significant improvement in VAS and ODI scores compared with the preoperative values. The mean VAS scores were 8.5 (range 7.5-9; SW: 0.7) before surgery and 6 (range 2.2-9; SW: 2.29) at the final followup, demonstrating a 30% improvement (P = 0.0001). The mean ODI scores were 64.1 (range: 40-82; SW: 15.27) before surgery and were 56.97 (range: 8-82; SW: 17.46) at the final followup, demonstrating a 12% improvement (P = 0.1887).
At their most recent visit, 78, 9% (15/19) of patients indicated they would go through the procedure again in order to achieve their current results [Table 1].
Table 1.
Clinical details of patients
DISCUSSION
The treatment of the SIJ degeneration with DIANA (distraction interference arthrodesis neurovascular anticipating) is aimed primarily on unrecognized and/or misinterpreted pain syndromes, whose treatment so far with non-surgical or surgical procedures had not led to long lasting success. It is worth mentioning that the SIJ degeneration may occur as a result of instrumented posterolateral lumbar/lumbosacral fusion.1,2 Alternative indications may be chronic pain originating from the SIJ as a result of posttraumatic arthrosis, ankylosing spondylitis, rheumatoid arthritis, or of an idiopathic nature.
Currently many techniques are described for SIJ arthrodesis.10,13,14,15,16 They include an anterior approach and internally fixing with plates and screws.10,15 Posterior fixation options include transiliac bars, cobra plates, tension band plates/transiliac reconstruction plates and iliosacral lag screws.14,15 There has also been some interest in percutaneous fixation using fluoroscopic or computed tomography guidance.13,16 These techniques can be successful, but only in experienced hands. Up to date there is no standard technique described in the literature.
Our article describes a new minimal-invasive technique for posterior sacroiliac arthrodesis which is called distraction interference arthrodesis. Using the previously described technique of distraction arthrodesis of the SIJ, we were able to achieve a fusion rate of 78.9%, which is similar to other techniques described in the literature involving large surgical exposures8,9,11,12 Also, we were able to achieve this result without any infection or neurovascular injury. VAS scores were slightly but significantly improved at the 6-month followup for back, leg and everyday activity pain. The ODI and the evaluation of VAS scores revealed success of this procedure even if the improvement was only between 12% and 30% respectively.
The advantages of the described technique were a minimally invasive procedure, including reduced tissue trauma due to the surgical approach. Another asset is the combined intrarticular and extraarticular fusion with bone graft or bone substitute and the intraarticular distraction due to the implant. The technique seems to be safe with regards to bowel and neurovascular structures. We observed no neurovascular complications as a result of a favorable surgical approach under anatomical aspects and a technique which is gentle to the tissues.
The limitation of our study is a relatively short followup duration and a small sample size. The long term results of these surgical procedures are needed. Also no control group was available to compare. 6 to 12 weeks of partial weight bearing, technically demanding procedure and a long fluoroscopy times (especially during the learning phase).
In conclusion, the technique described in the present study represents a minimally invasive and safe procedure that should be considered when contemplating sacroiliac arthrodesis in the instance of refractory SIJ pain as a result of multi-level fusion. It offers a safe and effective treatment for severe SIJ pain. Although it requires time to obtain a precise diagnosis, careful patient selection is important in predicting a good outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Yoshihara H. Sacroiliac joint pain after lumbar/Lumbosacral fusion: Current knowledge. Eur Spine J. 2012;21:1788–96. doi: 10.1007/s00586-012-2350-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liliang PC, Lu K, Liang CL, Tsai YD, Wang KW, Chen HJ. Sacroiliac joint pain after lumbar and lumbosacral fusion: Findings using dual sacroiliac joint blocks. Pain Med. 2011;12:565–70. doi: 10.1111/j.1526-4637.2011.01087.x. [DOI] [PubMed] [Google Scholar]
- 3.Park P, Garton H, Gala V, Hoff J, McGillicuddy J. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine (Phila Pa 1976) 2004;29:1938–44. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 4.Frigerio N, Stowe R, Howe J. Movement of the sacroiliac joint. Clin Orthop Relat Res. 1974;100:370–7. [PubMed] [Google Scholar]
- 5.Maigne J, Aivaliklis A, Pfefer E. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976) 1996;(21):1889–92. doi: 10.1097/00007632-199608150-00012. [DOI] [PubMed] [Google Scholar]
- 6.Schwarzer A, Aprill C, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995;20:31–7. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Ha K, Lee J, Kim K. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: A prospective cohort study over five-year followup. Spine (Phila Pa 1976) 2008;33:1192–8. doi: 10.1097/BRS.0b013e318170fd35. [DOI] [PubMed] [Google Scholar]
- 8.Berthelot J, Gouin F, Glemarec J. Possible use of arthrodesis for intractable sacroilitis in spondyloarthropathy: Report of two cases. Spine (Phila Pa 1976. 2001;26:2297–9. doi: 10.1097/00007632-200110150-00028. [DOI] [PubMed] [Google Scholar]
- 9.Buchowski J, Kebaish K, Sinkov V. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005;5:520–8. doi: 10.1016/j.spinee.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 10.Rand J. Anterior sacro-iliac arthrodesis for posttraumatic sacro-iliac arthritis. A case report. J Bone Joint Surg. 1985;67A:157–9. [PubMed] [Google Scholar]
- 11.Smith-Petersen M, Rogers W. End-result study of arthrodesis of the sacroiliac joint for arthritis-traumatic and nontraumatic. J Bone Joint Surg. 1926;8:118–36. [Google Scholar]
- 12.Waisbrod H, Krainick J, Gerbershagen H. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg. 1987;106:238–40. doi: 10.1007/BF00450461. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim N, Coombs R, Rusin J. Percutaneous CT-guided stabilization of complex sacroiliac joint disruption with threaded compression bars. Orthopaedics. 1992;15:1427–30. doi: 10.3928/0147-7447-19921201-08. [DOI] [PubMed] [Google Scholar]
- 14.Leighton R, Waddell J. Techniques for reduction and posterior fixation through the anterior approach. Clin Orthop. 1986;329:115–20. doi: 10.1097/00003086-199608000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Tile M. Baltimore: Williams and Wilkins; 1984. Fractures of the Pelvis and Acetabulum. [Google Scholar]
- 16.Khurana A, Guha A R, Mohanty K, Ahuja S. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws-clinical and radiological outcome. J Bone Joint Surg. 2009;91:627–31. doi: 10.1302/0301-620X.91B5.21519. [DOI] [PubMed] [Google Scholar]


