Abstract
Background:
Unicompartmental knee arthroplasty (UKA) has specific indications, producing excellent results. It, however, has a limited lifespan and needs eventual conversion to total knee arthroplasty (TKA). It is, therefore, a temporizing procedure in select active young patients with advanced unicompartmental osteoarthritis (UCOA). Being a less morbid procedure it is suggested as an alternative in the very elderly patients with tricompartmental osteoarthritis (TCOA). We performed UKA in a series of 45 octogenarians with TCOA predominant medial compartment osteoarthritis (MCOA) and analyzed the results.
Materials and Methods:
Forty five octogenarian patients with TCOA predominant MCOA underwent UKA (19 bilateral) from January 2002 to January 2012. All had similar preoperative work-up, surgical approach, procedure, implants and postoperative protocol. Clinicoradiological assessment was done at 3-monthly intervals for the first year, then yearly till the last followup (average 72 months, range 8-128 months). Results were evaluated using the knee society scores (KSS), satisfaction index [using the visual analogue scale (VAS)] and orthogonal radiographs (for loosening, subsidence, lysis or implant wear). Resurgery for any cause was considered failure.
Results:
Four patients (six knees) died due to medical conditions, two patients (three knees) were lost to followup, and these were excluded from the final analysis. Barring two failures, all the remaining patients were pain-free and performing well at the final followup. Indications for resurgery were: medial femoral condyle fracture needing fixation subsequent conversion to TKA at 2 years (n=1) and progression of arthritis and pain leading to revision TKA at 6 years (n=1).
Conclusion:
UKA has shown successful outcomes with regards to pain relief and function with 96.4% implant survival and 94.9% good or excellent outcomes. Due to lower demands, early rehabilitation, less morbidity, and relative short life expectancy, UKA can successfully manage TCOA in the octogenarians.
Keywords: Octogenarian, tricompartmental osteoarthritis, unicompartmental knee arthroplasty
INTRODUCTION
Unicompartmental osteoarthritis (UCOA) is normally the result of mechanical malalignment.1 Correction of this malalignment is paramount to prevent its deterioration to tricompartmental osteoarthritis (TCOA). A variety of factors, intrinsic (genetics, bone stock, pre-existing bony/joint deformity) and extrinsic (gender, weight, inflammatory arthritis, osteoporosis, trauma, previous surgery, etc.), have been accused of contributing to this altered alignment.1
Surgical treatment of advanced UCOA (with functionally intact ligaments) is possible with corrective femoral or tibial osteotomy (lateral closed wedge, medial open wedge, and/or modifications thereof), and has shown success when judiciously selected.2,3 An apt alternative in properly selected younger patients is the unicompartmental knee arthroplasty2,3,4 (UKA). UKA functions primarily by recreating joint space in the compartment that has collapsed, and partially realigning the mechanical axis. In both high tibial osteotomy (HTO) and UKA, the cruciate ligaments and extensor mechanism are left intact, providing for near-normal knee kinematics.3,5 Literature review shows slightly better results for UKA in terms of survivorship and functional outcome, compared to HTO.2,6 Revision of a failed HTO to TKA is also technically more demanding, adding to surgical time and difficulty.6,7
The UKA has shown to fail over time due to progression of arthritis in the other compartments. This occasionally occurs due to overcorrection of the alignment, and occasionally due to early wear and loosening of the prostheses, more so when used in poorly selected or extended indications.4,8,9 Recent reports10,11,12 of UKA for UCOA have shown more than 90% long term survivorships, even in knees that would not be considered ideal indications.8,13 Eminent researchers have recommended the UKA as a temporizing procedure14 in select younger active patients with advanced UCOA. The silver lining is that the functional results and survivorship rates after revision to TKA are nearly the same as those for primary TKA.15
The risks of intra and postoperative bleeding, venous thrombosis, infection rates, and development of medical complications are higher with the TKA vis-à-vis the UKA.16,17 With an older patient, there is lower tolerance to alteration in hemodynamics and increased propensity to develop medical and surgical complications. Presence of medical comorbidity makes this patient more susceptible to minor complications, and increases the perioperative morbidity, which delays rehabilitation and functional recovery and consequently worsens the outcomes following a successful prosthetic implantation.17
The focus of treatment of TCOA of the knee in the octogenarian and nonagenarian patients is faster rehabilitation and early return to activities of daily living (ADL), which can be provided by the UKA, a smaller and less morbid procedure.17 The functional demand on the knee and overall expectations of the very elderly patients are very low. With recent reports showing survival up to two decades and more,11,12 the UKA would most likely outlive these elderly patients. Thus, a less morbid surgery can be provided with all the benefits and outcomes provided by a knee arthroplasty procedure.
We have been offering UKA to the octogenarian patients presenting to us with TCOA (predominant medial UCOA) since 2002, and have presented our early results in a small series of patients in a previous report.18 We have followedup these patients to the mid-term (8-10 years), and present an analysis of these results. Through the results of our series, we aim to study the outcomes of the UKA as a definitive surgical treatment of painful TCOA in the octogenarian patient.
MATERIALS AND METHODS
Forty five very elderly patients (64 knees) with TCOA (predominant MCOA), 19 with bilateral knee involvement, were operated upon over a 10-year period (from January 2002 to January 2012). The average age of the patients was 83 years (range 79-94 years), and comprised 17 females and 28 males. The inclusion criteria included: age above 79 years, pain disrupting normal ADL, a minimum 6 months failed conservative treatment trial of lifestyle modification, physiotherapy, and intermittent analgesic therapy, radiological evidence of TCOA [Figure 1a] with predominant medial UCOA, and an otherwise active lifestyle. All patients were carefully screened through weight-bearing radiographs to demonstrate TCOA. All had patellofemoral compartment involvement, and lateral tibiofemoral osteophytes, though the lateral joint space was never completely obliterated [Figure 1a].
Figure 1.
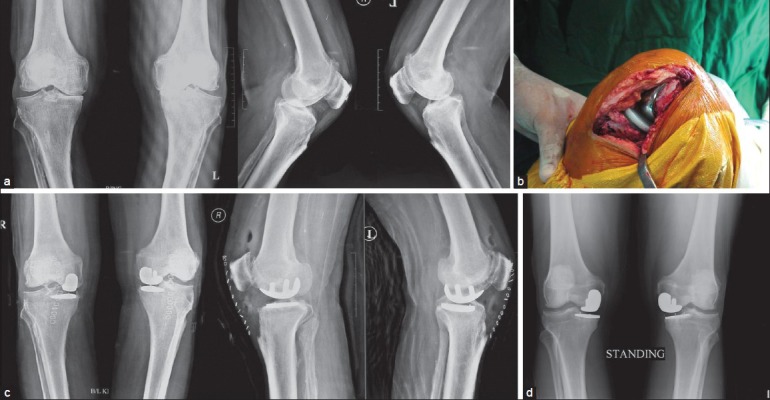
(a) Preoperative X-rays of (case E31) showing bilateral tricompartmental OA. (b) Intraoperative clinical photograph showing the Allegretto™ fixed-bearing UKA system (Zimmer Warsaw, IN, USA). (c) Postoperative X-rays anteroposterior and lateral views of both knees showing bilateral UKA. (d) X-rays anteroposterior views at 4 years followup showing no signs of wear, lysis, loosening or subsidence
Patients with inflammatory arthritis (rheumatoid arthritis, seronegative arthritis, gouty arthritis, etc.), obvious anterior cruciate ligament incompetence,8 inadequate conservative treatment trial, nonambulatory status, and advanced lateral compartment osteoarthritis (LCOA) on weight-bearing films were excluded. High body mass index19 (BMI) was not an exclusion criterion. All patients had preoperative anterior and medial knee joint line pain, with mild or no lateral joint line pain. All patients had varus alteration of the mechanical axis (average 8°, range 0°-15°). The mean preoperative range of motion (ROM) was 90° (range 75°-115°). Knee society scores (KSS; clinical and function) were recorded. Preoperative demographics (including coexistent medical conditions) were recorded [Table 1]. After routine preoperative anesthetic work-up, all patients were explained the possibility of conversion to TKA if evidence of severe LCOA was found intraoperatively, and their consent was obtained.
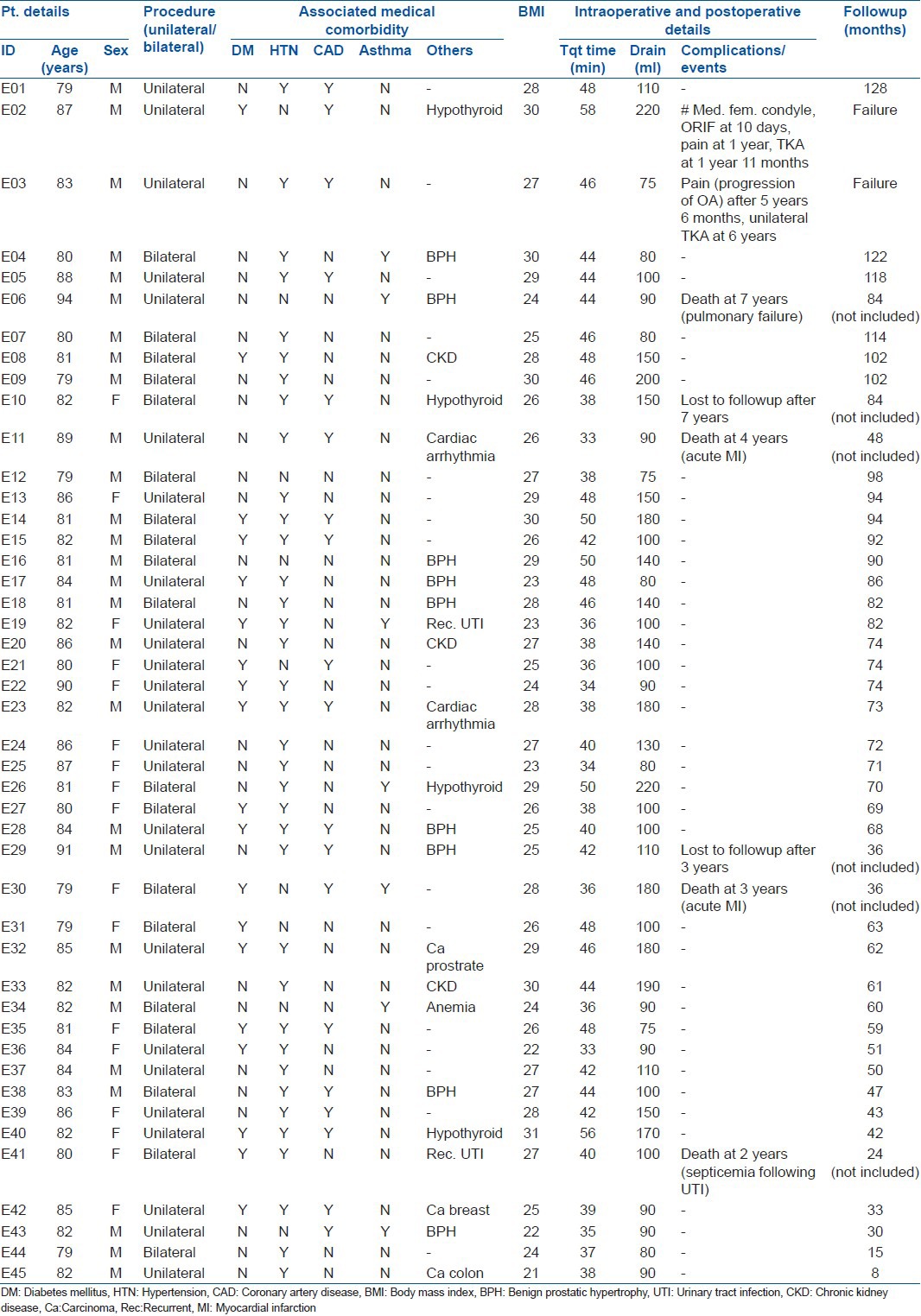
Table 1.
Clinical details of patients
Combined spinal epidural anesthesia was used in all patients, with epidural analgesia continued till the second postoperative day. Nineteen patients underwent simultaneous bilateral UKA, while the remaining 26 had unilateral UKA. All underwent medial UKA through a small medial paramedian incision and minimal medial parapatellar approach. Intraoperatively, all patients had radiological and visible degenerative changes in the lateral and patellofemoral compartment (Ahlbäck stages II or III), but no additional procedure (patelloplasty or lateral condylar shaving) was done. The Allegretto™ fixed-bearing UKA system by Zimmer (Warsaw, IN, USA) [Figure 1b] was used in all, with standard femoral (sizes 1-3), and metal-backed monoblock tibial (sizes 38-44 mm, poly 7.5-11 mm) components. Both components were cemented in place after bony preparation using a single packet of manually pressurized 20 g CMW1 gentamicin bone cement. The surgical wound was closed over a suction drain, and tight compression padded dressing was applied before releasing the tourniquet. Routine deep vein thrombosis (DVT) chemoprophylaxis (0.4 ml of low molecular weight heparin through daily subcutaneous injection) supplemented with graduated compression stockings was implemented till discharge (average: 4 days in unilateral, 6 days in bilateral UKA).
Postoperatively, the patients were made to stand and walk full weight bearing with a walking stick on the first postoperative day. The patient was gradually weaned off the stick and made to walk independently by about 2 weeks (unilateral UKA) and 3 weeks (bilateral UKA). Knee bending was progressed from 30° on the first day to 90° by 2 weeks, and beyond thereafter. A third-generation cephalosporin (cefuroxime) was given intravenously for 2 days, followed by the same antibiotic orally for an additional 3 days in every patient.
Patients were evaluated at 3, 6, 9, and 12 months postoperatively and then yearly thereafter. Clinical evaluation included the KSS (clinical and function), return to ADL, and patient satisfaction index using the visual analogue scale (VAS). The preoperative, immediate (3-month) and 12-month postoperative, and final scores of each patient have been presented in Table 2. Radiological evaluation was performed by taking orthogonal radiographs at each visit for radiological evidence of implant loosening, wear, lysis, or subsidence [Figure 1c]. Resurgery for any reason (pain progression, fracture, loosening, lysis, secondary LCOA necessitating conversion to TKA, etc.) was considered as failure endpoint.
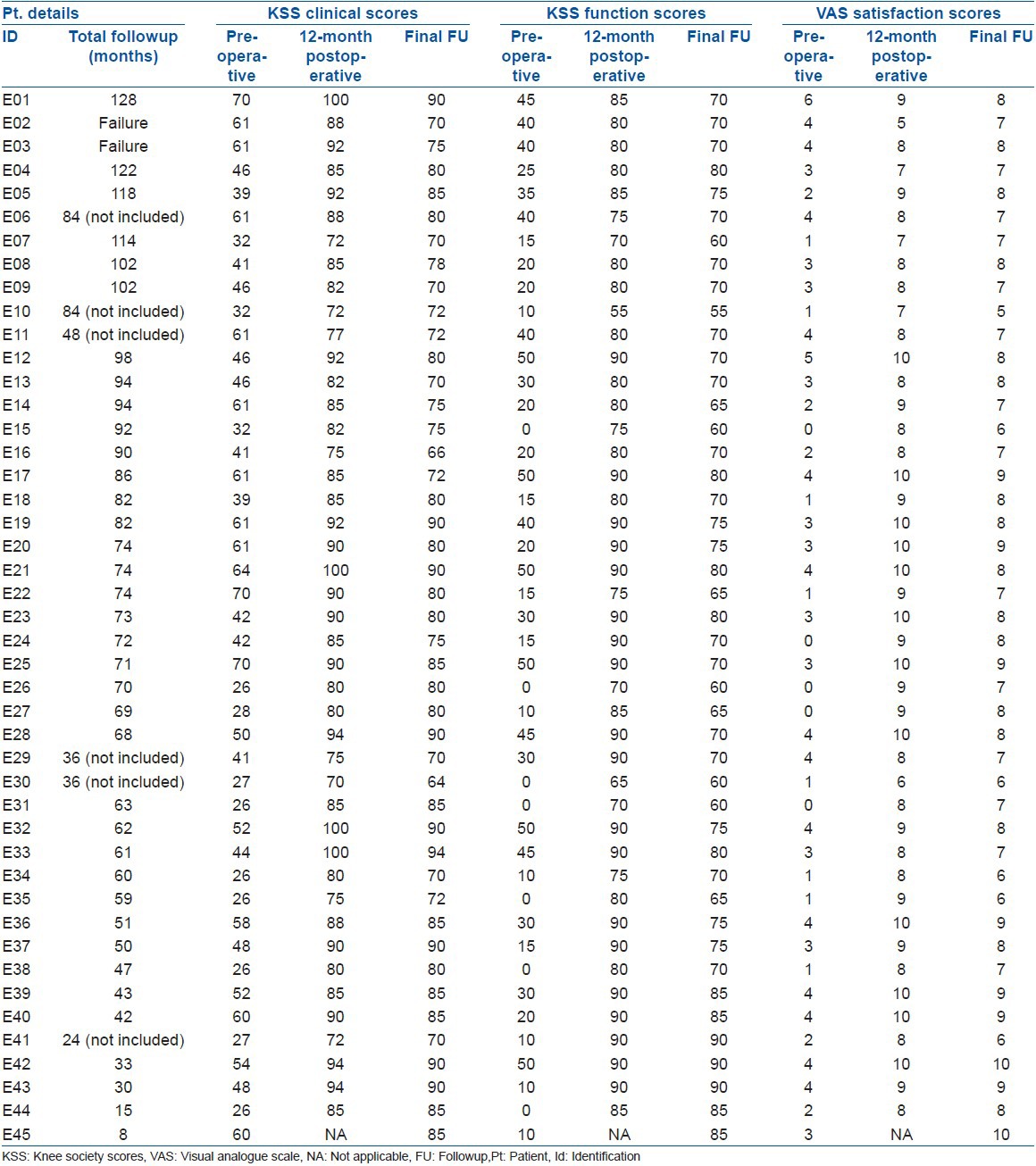
Table 2.
Preoperative, 1-year postoperative and final followup scores
RESULTS
Of 45 patients, 39 were available for final evaluation. The average duration of followup was 72 months (range 8-128 months). The mean duration of surgery was 42 min (range 33-58 min) for a knee. A tourniquet was used in all cases, and the average postoperative blood loss (measured by collection in the drain) was 120 ml (range 70-220 ml). Average length of hospital stay was 4 days for unilateral UKA and 6 days for bilateral UKA.
During the followup period, four patients (two with bilateral UKA) died due to medical complications. Two patients died following acute myocardial infarction (at followup of 3 and 4 years), one succumbed to pulmonary failure following pneumonia (at 7 years), and one developed fatal septicemia following recurrent urinary infection (at 2 years) [Table 1]. Two patients (one with bilateral UKA) were lost to followup (at 3 and 7 years, respectively). These seven patients (nine UKAs) have not been included in the outcome analysis.
There was no incidence of deep infection, DVT, or medical complications in the perioperative period (3 months). At 1 year postoperatively, all but one patient had no or mild pain, with near normal function and full return to ADL. This one patient [Figure 2a] complained of persistent pain a few days after discharge on stopping the oral analgesics; repeat radiographs done on the 8th postoperative day revealed an undisplaced fracture (possibly a missed intraoperative undisplaced fracture) of the medial femoral condyle [Figure 2b]. He was readmitted and treated with multiple screw fixation on the 10th postoperative day [Figure 2c], followed by immobilization in a long leg knee brace and protected weight bearing for 6 weeks, gentle ROM knee exercises, with no bearing on the clinical or functional scores at 6 months. However, he had recurrence of pain at 12 months, and finally underwent revision to TKA at nearly 2 years post index surgery [Figure 2d]. He was deemed a failure. One other patient [Figure 3a] (with unilateral UKA) had increasing pain with radiological progression of arthritis in the lateral compartment and subsequently underwent revision to TKA at 6 years postoperatively [Figure 3c]. On retrospect evaluation, the UKA implant had been placed in valgus correction postoperatively [Figure 3b]. He was termed a failure.
Figure 2.

(a) Preoperative X-ray anteroposterior and lateral views of (R) knee joint (case E02) showing tricompartmental OA of the right knee. (b) Immediate postoperative X-ray anteroposterior and lateral views after UKA surgery showing implant in situ (c) X-ray anteroposterior and lateral views showing screw fixation of medial femoral condyle fracture under the UKA. (d) X-ray after revision to TKA
Figure 3.
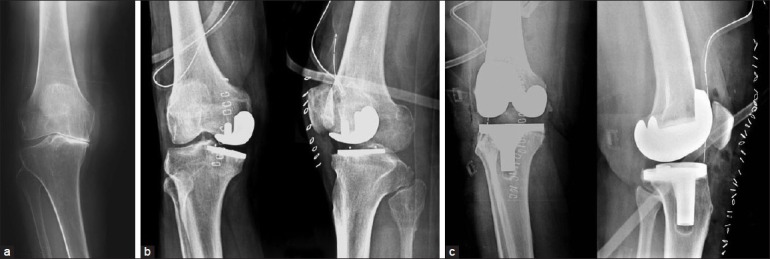
(a) Preoperative X-ray anteroposterior view (standing) (case E03) showing severe osteoarthritic changes (b) Postoperative X-ray anteroposterior and lateral views following UKA showing possible valgus placement. (c) Postoperative X-ray anteroposterior and lateral views after revision to TKA
Barring these two, all the remaining patients had mild or no pain and were functionally performing well at final followup, with good clinical and functional scores, and were satisfied with their surgery. They were all walking independently, and had an average knee ROM of 115° (range 100°-125°). We observed no radiological signs of wear, lysis, loosening, or subsidence in any patient [Figure 1d]. No patient had any of the complications20 associated with TKA, viz. DVT, pulmonary embolism (PE), subluxation, patellar problems, or mid-flexion instability.
Excluding the patients who died or were lost to followup, we had an implant survival rate of 96.4% (53/55), with excellent results (KSS > 70, VAS > 7, return to ADL, no adverse radiological signs) in 71.8% of patients (28/39) and good results (KSS > 60, VAS > 5, return to ADL, no adverse radiological signs) in 94.9% patients (37/39) at an average of 6 years post surgery. As a group, the mean Knee Society clinical scores improved from 46 (range 26-70) preoperatively to 83 (range 72-100) immediately (3 months) postoperatively, and fell only to 81 (range 66-90) at the final followup. Similarly, the mean Knee Society function scores improved from 24 (range 0-50) to 82 (range 55-90) postoperatively, falling to 73 (range 55-90) at the final followup. Satisfaction with the procedure showed the most dramatic improvement. VAS improved from a mean preoperative of 3 (range 0-6) to 9 (7-10) at 12 months postoperatively, with a value of 8 (range 5-9) at the final followup [Table 2].
If all patients (including those lost to followup or died) were included in the analysis, our mean Knee Society clinical scores improved from 46 (range 26-70) preoperatively to 82 (range 72-100) immediately postoperatively, and fell to 79 (range 62-90) at the final followup. The mean Knee Society function scores improved from 24 (range 0-50) to 80 (range 50-90) immediately postoperatively, falling to 72 (range 50-90) at the final followup. VAS scores defining satisfaction with the procedure improved from a mean preoperative of 3 (range 0-6) to 9 (7-10) at 6 months postoperatively, with a final value of about 7.5 (range 5-9) [Table 2].
Our implant failure rate was 3.6% (2/55) at an average 6 years followup, slightly higher than the results of most series of UKA. The overall implant failure rate (worst-case scenario, if patients lost to followup were considered failures) was 8.6% (5/58), leaving an overall patient success rate (good or excellent result) of 90.2% (37/41), nearly consistent with the results of the UKA procedure in most series of young patients.12,16
DISCUSSION
Advanced UCOA, after sufficient trial of conservative treatment, has been treated by distal femoral or proximal tibial osteotomies with short-lived good results,2 followed by a steep decline in joint function due to accelerated degeneration, eventually necessitating TKA.7 Revision of an HTO to TKA is technically difficult with poor midterm to long term results compared to those undergoing a primary TKA.7 The UKA is an alternative offered to patients with UCOA with strict inclusion criteria.4 Price et al.12 have reported that though seemingly unsuitable for highly active younger patients, UKAs last 15 years or more in up to 91% of such young active patients. So, longevity up to about a decade seems successfully possible with a well executed UKA, more so in centers specializing in the procedure.12,13 Though our overall followup period is short, in our study, we have seen best case scenario implant survival rates of 96.4% and worst case scenario implant survival rates (considering the patients lost to followup or dying due to unrelated causes as failures) of 89.8%.
Knee TCOA in octogenarians does not incapacitate the patient as much as in the younger active patient, as these very elderly patients have a relatively sedentary lifestyle, low demands, and fewer expectations.19 Registry data21,22 from Australia and Sweden have confirmed that patients older than 65 years of age have lower rates of revision and better outcomes with regards to survival, compared to those less than 65 years of age. This does not imply that they do not deserve such a procedure when otherwise indicated.22 There is no doubt that TKA surgery is better, in terms of pain relief, function, and longevity, in the young23 as well as in the elderly, with 90-95% survivorship at up to 20 years.24 However, TKA in this group of fragile, very elderly population can cause prolonged morbidity,25,26 delayed rehabilitation, and higher mortality risk (especially in patients with coexistent multiple medical morbidity). This risk can be mitigated by the relatively less morbid17 UKA procedure. This has been found to be true in our study as well wherein the surgical perioperative complication rate was 1.8% (1/55), and is substantiated by similar negligible rates seen in larger studies on simultaneous bilateral27 UKA. Studies comparing UKA and TKA for TCOA in very elderly low-demand patients have proven that UKA can provide similar results, with reduced morbidity.25,27,28
Traditionally reserved for nonobese, less active, young patients with advanced noninflammatory UCOA,1,3 the UKA procedure has (within these indications) demonstrated good success in function and longevity.11,16,29 However, patients with marginal other compartment involvement and ACL incompetence have shown matched good results in the short term as well.9,30,31 The UKA surgical technique is exacting and unforgiving. Overstuffing of the medial compartment in medial UKA produces alteration of the mechanical axis to a valgus alignment with rapid progression of osteoarthritis in the other compartments, leading to early failure and need for revision to a TKA.2 Berger et al.32 have shown that progression of arthritis in the lateral or patellofemoral compartments is not likely to affect the long term prognosis of UKA. Elderly patients have higher tolerance to pain, and this has been explained as being possibly due to reduced expectation.19 By understanding unicompartmental knee biomechanics, and the failures seen in our study, it would perhaps be prudent to state that one of our failures might have been prevented by an under-corrected position of the UKA. The progression of LCOA in the single patient (one knee) that necessitated conversion to TKA can possibly be attributed to valgus overcorrection at the time of the index UKA surgery [Figure 3b].
Many other advantages have been cited in favor of UKA vis-à-vis TKA. These include early restoration of and near-complete knee ROM17 (possibly due to maintenance of the suprapatellar space), preservation of the knee biology (bone stock, kinematics,5,8 proprioception, and function), lower morbidity33 (lesser blood loss, shorter hospital stay, lower risk of fat embolism or DVT), and early recuperation25,27 (smaller incision, minimal tissue trauma, fewer complications). Further, unlike in an osteotomy, conversion to TKA at any stage (during surgery or in the followup) is technically relatively easier, with eventual outcomes matching those following primary TKA.15,34 The UKA is also cost-effective, as demonstrated by survival data from the Norwegian arthroplasty register.35
The caveat to this utopic outlook for UKA is that initial excellent results at 8-10 years have given way to unacceptably high failure rates at 15 years in younger patients.10,15,29 These have been variously attributed to implant-related (problems with design, material, fixation method, and stability), patient-related (inappropriate indication, presence of tricompartmental arthritis, excessively active lifestyle, etc.), or surgeon-related (improper technique, partial injury to cruciate ligaments or unresurfaced tibiofemoral articular cartilage, failure to treat the underlying pathology producing the UCOA, etc.) issues.3,10,15 More recently, however, Seyler et al.30 have suggested that poor preoperative objectives and functional scores, and patellar osteophytes do not adversely impact the results of UKA, and might not constitute contraindications for this procedure.
The UKA procedure is technically exacting and requires strict adherence to principle.2 Meta-analyses of surgical outcomes following UKA confirm that the best outcomes are reported from centers that have developed the implant, and national registry data from many countries actually show revision rates 3-4 times higher than the rates reported by these centers.13 Analyses of the Swedish and Finnish registries15,29 have confirmed that good long term outcomes following UKA at a center are related to the number of UKAs performed at that center. Complications4,15,27,30 can occur with UKA, including spin out of mobile meniscus, dislocation, tibial plateau fractures, femoral condyle necrosis, implant loosening, and osteolysis. These are usually the result of poor surgical technique, and quite often than not, preventable.11,27 The medial femoral condyle fracture seen in one patient in our series can possibly be attributed to an incomplete fracture during the seating of the femoral component on osteoporotic metaphyseal bone.27 Prevention, early recognition, and appropriate management of such fractures are possible, and early rectification with intraoperative or postoperative screw fixation (as in our case) will sometimes suffice in the short term [Figure 2a]. However, the end result might likely be poor (as the fixation of the femoral component is probably jeopardized, leading to early loosening and subsequent pain), necessitating conversion to a TKA in the near future, as eventually required in that case.
The limitations of the study include patient selection bias, non-blinding of the study, small sample size, absence of a comparative control group, and nonobjective preoperative and intraoperative assessment of the lateral and patellofemoral compartment osteoarthritis. Also, alteration in outcome statistics due to the patients lost to followup and those who died provide greater variance in our standard deviation calculations, and may incorrectly reflect our results.
Results reported by us match those seen with similar patient cohorts reported in the literature.10,11,18,28,29,30,33,36 Our implant survival and patient satisfaction data indicate that the UKA is a successful option for the very elderly with TCOA (predominant medial UCOA). With precise patient selection and appropriate surgical technique, UKA can be suggested as the definitive surgery in a properly selected very elderly patient with knee TCOA (predominant UCOA).
To summarize, UKA in these very elderly patients with TCOA seems potentially good option as it affords the unique advantages of pain relief and return to function with minimal morbidity and mortality risk.11,15,16,18,20,27,29,33 Since recovery is quick and pain relief and rehabilitation are simpler, high satisfaction levels are achieved quickly. Return to ADL, which is perhaps most crucial in this age group of patients, is very rapid.26,28,33 Attention to appropriate surgical technique is essential to provide good outcomes, even though fear of conversion or revision surgery (and its attendant risks and complications) is marginal as the implant will most likely outlive the patient.12,26,28,36 Judicious patient selection and sound operative technique are the prerequisites for a good result.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Iorio R, Healy WL. Unicompartmental arthritis of the knee. J Bone Joint Surg Am. 2003;85:1351–64. doi: 10.2106/00004623-200307000-00025. [DOI] [PubMed] [Google Scholar]
- 2.Mont MA, Stuchin SA, Paley D, Sharkey PF, Parvisi J, Tria AJ, Jr, et al. Different surgical options for monocompartmental osteoarthritis of the knee: High tibial osteotomy versus unicompartmental knee arthroplasty versus total knee arthroplasty: Indications, techniques, results and controversies. Instr Course Lect. 2004;53:265–83. [PubMed] [Google Scholar]
- 3.Sikorski JM, Sikorska JZ. Relative risk of different options for medial compartment osteoarthritis of the knee. Orthopedics. 2011;34:e847–54. doi: 10.3928/01477447-20111021-04. [DOI] [PubMed] [Google Scholar]
- 4.Stern SH, Becker MW, Insall JN. Unicondylar knee arthroplasty: An evaluation of selection criteria. Clin Orthop Relat Res. 1993;286:143–8. [PubMed] [Google Scholar]
- 5.Patil S, Colwell CW, Jr, Ezzet KA, D’Lima DD. Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Joint Surg Am. 2005;87:332–8. doi: 10.2106/JBJS.C.01467. [DOI] [PubMed] [Google Scholar]
- 6.Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, Rossi R. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: A review of the literature. Iowa Orthop J. 2010;30:131–40. [PMC free article] [PubMed] [Google Scholar]
- 7.Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: Risk factors for failure. J Bone Joint Surg Am. 2004;86:474–9. doi: 10.2106/00004623-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Engh CA, Ammeen D. Is an intact anterior cruciate ligament needed in order to have well-functioning unicondylar knee replacement? Clin Orthop Relat Res. 2004;428:170–3. doi: 10.1097/01.blo.0000148895.78766.8a. [DOI] [PubMed] [Google Scholar]
- 9.Beard DJ, Pandit H, Ostlere S, Jenkins C, Dodd CA, Murray DW. Preoperative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg Br. 2007;89:1602–7. doi: 10.1302/0301-620X.89B12.19260. [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: Long term results. Clin Orthop Relat Res. 2001;392:272–8. [PubMed] [Google Scholar]
- 11.O’Rourke MR, Gardner JJ, Callaghan JJ, Liu SS, Goetz DD, Vittletoe DA, et al. Unicompartmental knee replacement: A minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. doi: 10.1097/01.blo.0000185451.96987.aa. [DOI] [PubMed] [Google Scholar]
- 12.Price AJ, Svard U. A second decade life-table survival analysis of the Oxford unicompartmental knee. Clin Orthop Relat Res. 2011;469:174–9. doi: 10.1007/s11999-010-1506-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labek G, Sekrya K, Pawelka W, Janda W, Stöckl B. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty. Acta Orthopaedica. 2011;82:131–5. doi: 10.3109/17453674.2011.566134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engh CA. Orthopaedic crossfire-can we justify unicondylar arthroplasty as a temporizing procedure? In the affirmative. J Arthroplasty. 2002;17:54–5. doi: 10.1054/arth.2002.32448. [DOI] [PubMed] [Google Scholar]
- 15.Dudley TE, Gioe TJ, Sinner P, Mehle S. Registry outcomes of unicompartmental knee arthroplasty revisions. Clin Orthop Relat Res. 2008;466:1666–70. doi: 10.1007/s11999-008-0279-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: The 15-year results of a prospective randomized controlled trial. J Bone Joint Surg Br. 2009;91:52–7. doi: 10.1302/0301-620X.91B1.20899. [DOI] [PubMed] [Google Scholar]
- 17.Lombardi AV, Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res. 2009;467:1450–7. doi: 10.1007/s11999-009-0731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marya SK, Thukral R. Unicompartmental knee arthroplasty for tricompartment osteoarthritis in octogenarians. Indian J Orthop. 2009;43:361–6. doi: 10.4103/0019-5413.54970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh JA, Gabriel S, Lewallen DG. Higher body mass index is not associated with worse pain outcomes after primary or revision total knee arthroplasty (TKA) J Arthroplasty. 2011;26:366–74. doi: 10.1016/j.arth.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Memtsoudis SG, Gonza×lezDella Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res. 2008;466:2617–27. doi: 10.1007/s11999-008-0402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S. Unicompartmental knee arthroplasty in patients aged less than 65. Combined data from the Australian and Swedish Knee Registries. Acta Orthop. 2010;81:90–4. doi: 10.3109/17453671003587150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brander VA, Malhotra S, Jet J, Heinemann AW, Stulberg SD. Outcome of hip and knee arthroplasty in persons aged 80 years and older. Clin Orthop Relat Res. 1997;345:67–78. [PubMed] [Google Scholar]
- 23.Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: Survival in a community registry. Clin Orthop Relat Res. 2007;464:83–7. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 24.Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty: Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am. 1991;73:397–409. [PubMed] [Google Scholar]
- 25.Yang KY, Wang MC, Yeo SJ, Lo NN. Minimally invasive unicondylar versus total condylar knee arthroplasty-early results of a matched-pair comparison. Singapore Med J. 2003;44:559–62. [PubMed] [Google Scholar]
- 26.Krishnan SR, Randle R. ACL reconstruction with unicondylar replacement in knee with functional instability and osteoarthritis. J Orthop Surg Res. 2009;4:43. doi: 10.1186/1749-799X-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berend KR, Morris MJ, Skeels MD, Lombardi AV, Jr, Adams LB. Perioperative complications of simultaneous versus staged unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2011;469:168–73. doi: 10.1007/s11999-010-1492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sah AP, Springer BD, Scott RD. Unicompartmental knee arthroplasty in octogenarians. Clin Orthop Relat Res. 2006;451:107–12. doi: 10.1097/01.blo.0000223983.67325.61. [DOI] [PubMed] [Google Scholar]
- 29.Kosinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: A prospective followup study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–35. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 30.Seyler TM, Mont MA, Lai LP, Xie J, Marker DR, Zywiel MG, et al. Mid-term results and factors affecting outcome of a metal-backed unicompartmental knee design: A case series. J Orthop Surg Res. 2009;4:39. doi: 10.1186/1749-799X-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krishnan E, Fries JF, Kwoh CK. Primary knee and hip arthroplasty among nonagenarians and centenarians in the United States. Arthritis Rheumat. 2007;57:1038–42. doi: 10.1002/art.22888. [DOI] [PubMed] [Google Scholar]
- 32.Berger RA, Meneghini RM, Sheinkop MB, Della Valle CJ, Jacobs JJ, Rosenberg AG, et al. The progression of patellofemoralarthrosis after medial unicompartmental replacement: Results at 11 to 15 years. Clin Orthop Relat Res. 2004;428:92–9. doi: 10.1097/01.blo.0000147700.89433.a5. [DOI] [PubMed] [Google Scholar]
- 33.Repicci JA, Hartman JF. Minimally invasive unicondylar knee arthroplasty for the treatment of unicompartmental osteoarthritis: An outpatient arthritic bypass procedure. Orthop Clin North Am. 2004;35:201–16. doi: 10.1016/j.ocl.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Hang JR, Stanford TE, Graves SE, Davidson DC, de Steiger RN, Miller LN. Outcome of revision of unicompartmental knee replacement. 1,948 cases from the Australian Orthopedic Association National Joint Replacement Registry, 1999-2008. Acta Orthop. 2010;81:95–8. doi: 10.3109/17453671003628731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Slover J, Espehaug B, Havelin LI, Engesaeter LB, Furnes O, Tomek I, et al. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients: A Markov decision analysis. J Bone Joint Surg Am. 2006;88:2348–55. doi: 10.2106/JBJS.E.01033. [DOI] [PubMed] [Google Scholar]
- 36.Joshi AB, Markovic L, Gill G. Knee arthroplasty in octogenarians: Results at 10 years. J Arthroplasty. 2003;18:295–8. doi: 10.1054/arth.2003.50063. [DOI] [PubMed] [Google Scholar]


