Abstract
Background:
Total knee arthroplasty (TKA) can result in major postoperative blood loss which can impact on the recovery and rehabilitation of patients. It also requires expensive transfusions. The purpose of the study was to investigate whether a hemostatic matrix, composed of cross-linked gelatin and a thrombin solution, would reduce blood loss in patients following TKA.
Materials and Methods:
This was a prospective, randomized, controlled study (Trial registration: Hospital S. Salvatore L’Aquila ADJ00843) conducted in 93 patients. Criteria for participation were unilateral TKA for osteoarthritis, and a preoperative hemoglobin level >13 g/dL. The outcomes measured were postoperative hemoglobin and hematocrit levels measured at 24h, 72 h, and 7 days. The mean total postoperative blood loss was calculated from drainage volume, patient blood volume, hematocrit, and red blood cell volume. In addition, the drain output within 24 h following surgery and any transfusion requirements were determined.
Results:
Hemostatic matrix-treated patients (n = 51) showed significant reductions in calculated postoperative blood loss of 32.3% and 28.7% versus control in men and women, respectively (P < 0.01). Postoperative blood loss after 24 h in drain was significantly less with the hemostatic matrix versus control, as were decreases in hemoglobin levels 7 days post-surgery (each P < 0.01). Three patients in the control group required blood transfusion, whereas no blood transfusions were necessary in the hemostatic matrix group.
Conclusion:
The use of a hemostatic matrix provides a safe and effective means to reduce blood loss and blood transfusion requirements in TKA.
Keywords: Blood loss, blood transfusion, hemostatic matrix, postoperative outcomes, total knee arthroplasty
INTRODUCTION
Blood management is essential for the successful outcome of total knee arthroplasty (TKA).1 TKA is a major orthopedic operation that involves substantial postoperative blood loss of approximately 800-1500 ml.2 In addition to having a major impact on the recovery and rehabilitation of TKA patients, such a magnitude of blood loss frequently necessitates allogenic blood transfusions, which have been associated with the transmission of infectious diseases, increased postoperative bacterial infection, and other immunological and non-infectious transfusion complications.3,4,5
Surgeons have pursued various strategies for dealing with blood loss, such as preoperative autologous donation, cell salvage, and the use of erythropoietin. These approaches have been shown to offer relatively small benefits in terms of reducing the need for allogenic blood transfusion and they can also incur increased cost.6,7 Indeed, the most effective way to reduce the need for allogenic blood is to control the amount of blood lost during an operation. Nowadays, it is common practice to perform TKA using pneumatic tourniquets to ensure negligible blood loss during the procedure, and to improve the visibility of the surgical site. Unfortunately, studies also show that artificial ischemia of the operated knee can increase the activity of the fibrinolytic system, which may in turn accentuate postoperative bleeding.8,9,10 Fibrin has been used as a hemostatic agent for over 100 years.11 During the 1970s, improvements in plasma fractionation methods and the availability of concentrated fibrinogen led to significant progress in the optimization of the rheological properties of fibrin tissue adhesives. Other recent advances include the use of screening and vapor heat treatment for viral safety and the use of spray devices for optimal delivery of adhesive onto the wound surface.
These recent advances have resulted in the use of fibrin tissue adhesive technology across a range of surgical settings, including cardiac,12 vascular,13 spinal,14 pediatric adenoidectomy,15 laparoscopic partial nephrectomy,16 and endoscopic sinus surgery.17
The aim of this study was to evaluate the hemostatic efficacy of a hemostatic matrix, composed of a bovine-derived cross-linked gelatin matrix and a human-derived thrombin solution, in patients undergoing TKA by determining postoperative (1) hemoglobin levels, (2) hematocrit levels, (3) mean total blood loss, and to assess (4) blood transfusion requirements and any adverse effects.
MATERIALS AND METHODS
This was a prospective, randomized, controlled trial conducted in 93 patients and no patient declined to participate in the study during the accrual process. The randomization was performed through a computer assisted program. All procedures took place in the same institution and were performed using the same standard surgical procedure. Criteria for participation were unilateral TKA for osteoarthritis, and a preoperative hemoglobin level >13 g/dL. Patients with inflammatory arthritis, heart disease, peripheral arterial disease, cerebrovascular disease, allergies to bovine products, or a history of bleeding disorders were excluded from the study. Between November 2007 and January 2010, 93 patients undergoing elective primary unilateral TKA for osteoarthritis who met the inclusion criteria were enrolled. The patients were followed up according to the predefined study protocol. The study was approved by the local ethics committee of the hospital (registration number ADJ00843). The study was conducted according to the Declaration of Helsinki; the patients gave their informed consent prior to their inclusion.
We tested the hypothesis that the application of a hemostatic matrix, composed of a bovine-derived cross-linked gelatin matrix and a human-derived thrombin solution, would reduce bleeding following TKA when compared with electrocoagulation, the standard method of hemostasis (control). The outcomes were postoperative hemoglobin and hematocrit levels measured at 24 h, 72 h, and 7 days. The mean total postoperative blood loss was calculated. In addition, the drain output 24 h following surgery and any transfusion requirements were determined.
Low contact stress uncemented rotating platform prostheses (Depuy, Leeds, UK) without patellar resurfacing were used for all implants. The hemostatic matrix used in this study (Floseal®, Baxter Healthcare Corporation, Fremont, USA) consists of a bovine-derived cross-linked gelatin matrix containing a human-derived thrombin component (500 I.U/mL). It was prepared in accordance with the manufacturer's instructions.18
Operative procedure
All operations were performed in a bloodless field with the use of a pneumatic tourniquet. In all cases, the drill hole created for the intramedullary guide rod was occluded with bone prior to implantation of the femoral component in order to reduce blood loss. After insertion of the prosthesis without cement, the tourniquet was deflated and hemostasis was achieved by the use of an electrocoagulator. Patients did not receive tranexamic acid at any point throughout the procedure.
Before closure of the soft tissues, the knee joint and the entire operative field were thoroughly rinsed with sterile (non-heparinized) saline solution to remove all debris and were meticulously dried. For patients randomized to receive hemostatic matrix, 10 ml of the hemostatic matrix was applied, using an applicator tip (or syringe tip) to dispense, into the joint itself, on to the raw surfaces of the bone, muscles and tendons, and around the subcutaneous tissues. The hemostatic matrix was applied to the anatomical regions where it is difficult to use an electrocoagulator. All the hidden pouches of the joint were exposed to ensure that as much surface area was covered with hemostatic matrix as possible, excluding the bone under the implant.
In both patient groups, drains were used in the joint and connected to a high-vacuum, suction-drain bottle for 24 h. The knee joint was then closed in layers. All patients received low molecular weight heparin, (4000 IU enoxaparin sodium) as thromboprophylaxis 12 h before the operation and every 24 h postoperatively. A calf pump was used during recovery to reduce the risk of deep vein thrombosis (DVT). The mean duration of therapy was 30 days, usually until the patient regained adequate leg motion. Any blood transfusion requirement or complications, such as signs of infection or DVT, were recorded. The criteria for transfusion were based upon a number of factors including the pre- and postoperative hemoglobin levels and intraoperative blood loss. The attending surgeons made the decision to transfuse patients with a postoperative hemoglobin level of 8.5-9 g/dL, only if they had relevant symptoms, such as fainting, tachycardia, or asthenia. No patients had a hemoglobin level <8.5 g/dL at any point of time postoperatively. Patients with a hemoglobin level >10 g/dL were not transfused.
Calculation of total blood loss
Loss of blood at the end of the operation was recorded by measuring the volume in the suction apparatus. A substantial amount of postoperative blood loss is not evacuated by suction drainage which is extravasated in tissues.19 Consequently, we estimated postoperative blood loss by calculating the patient's blood volume (PBV) using the method of Nadler et al. (1962).:20
PBV = (k1 × height3 (m)) + (k2 × weight (kg)) + k3
For male patients: k1 = 0.3669, k2 = 0.03219, and k3 = 0.6041
For female patients: k1 = 0.3561, k2 = 0.03308, and k3 = 0.1833
Multiplying the PBV by the hematocrit (Hct) gives the red blood cell (RBC) volume. Thus, a change in the RBC volume can be calculated from a change in the hematocrit level, as follows:
Total RBC volume loss = PBV × (Hct preoperative − Hct postoperative)
Transfusions (mean volume per unit = 285 ml) were taken into account by calculating the total blood loss as follows:
Total blood loss (L) = Total RBC volume loss + (Number of units transfused × 0.285) ÷ ((Hct preoperative + Hct postoperative) ÷ 2).
Statistical analysis
The sample size was calculated by a power analysis and participants were allocated to treatment group by the surgeon, using a computer-generated list of random numbers. Data analyses were performed using the Student's t-test, the Chi-squared test, and Pearson's correlation coefficient. A p value of 0.05 or less was considered to be statistically significant for all analysis performed.
RESULTS
The flow of patients through the study is illustrated in Figure 1. Of 93 randomized patients, 51 were allocated to treatment with hemostatic matrix as well as the standard method of hemostasis (hemostatic matrix group), and 42 were allocated to treatment with the standard method of hemostasis only (control group). All 93 patients completed the study. Baseline patient characteristics are presented in Table 1. There were no significant differences in baseline patient characteristics between the hemostatic matrix and control groups for men (n = 41) or women (n = 52).
Figure 1.
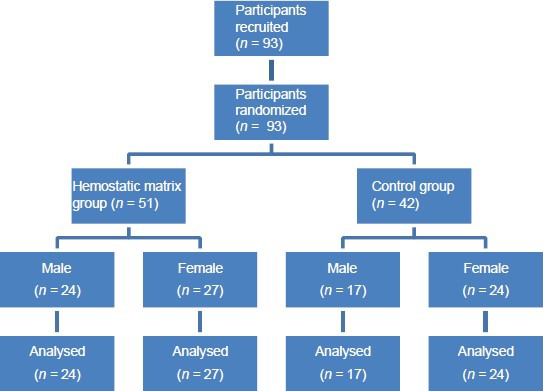
Patient flow through the study
Table 1.
Baseline patient characteristics for each group by gender
Drainage postoperative blood loss
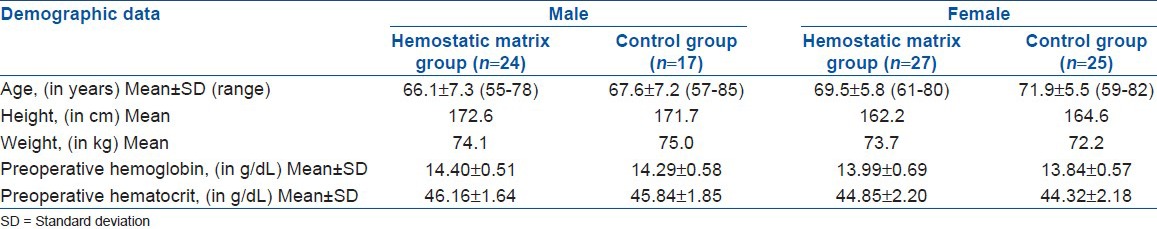
The mean (± standard deviation (SD)) volumes of drainage postoperative blood loss 24 h after TKA are shown in Figure 2. Levels were significantly reduced in the hemostatic matrix group compared with the control group for both men (0.22 ± 0.04 vs. 0.72 ± 0.12 L; 69.65% reduction; P < 0.01) and women (0.19 ± 0.03 vs. 0.65 ± 0.11 L; 70.05% reduction; P < 0.01).
Figure 2.
A bar diagram showing mean drainage postoperative blood loss (after 24 h) in each group by gender
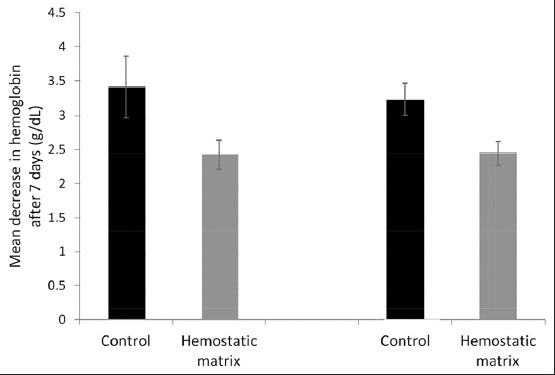
Postoperative hemoglobin and hematocrit levels
The mean (±SD) decrease in hemoglobin levels 24 h after TKA was lower in the hemostatic matrix group than the control group for men (1.79 ± 0.20 vs. 2.49 ± 0.21 g/dL) and women (1.73 ± 0.19 vs. 2.28 ± 0.21 g/dL). The percentage reduction in hemoglobin with hemostatic matrix versus control was 5.00% lower in men (12.41% vs. 17.41%; P < 0.01) and 4.14% lower in women (12.39% vs. 16.53%; P < 0.01).
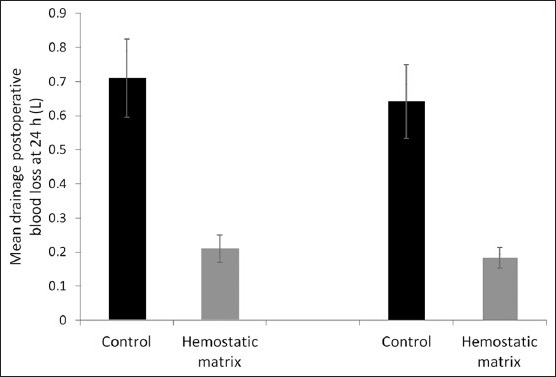
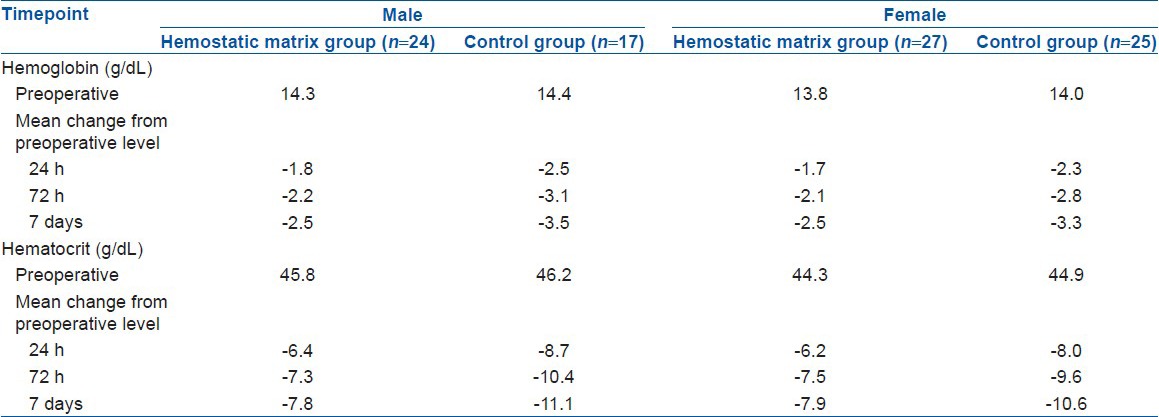
The mean (±SD) hemoglobin levels 7 days after TKA are shown in Figure 3. Hemoglobin levels were lower in the hemostatic matrix group than the control group for men (2.47 ± 0.21 vs. 3.46 ± 0.45 g/dL) and women (2.49 ± 0.18 vs. 3.28 ± 0.23 g/dL). The percentage reduction in hemoglobin with hemostatic matrix vs. control 7 days after TKA was 7.05% lower in men (17.15% vs. 24.20%; P < 0.01) and 5.62% lower in women (17.81% vs. 23.43%; P < 0.01) [Table 2].
Figure 3.
A bar diagram showing mean decrease in hemoglobin (after 7 days) in each group by gender
Table 2.
Mean reduction in hemoglobin and hematocrit levels compared with preoperative levels for each group
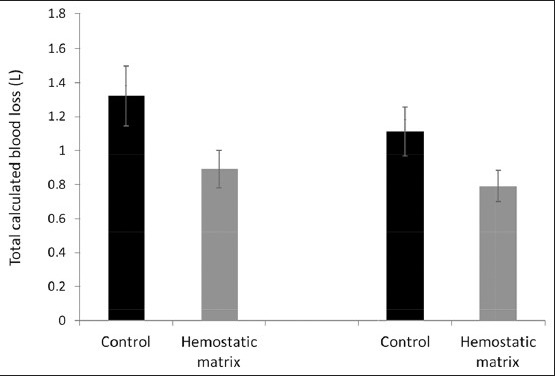
Calculated total blood loss
Total blood loss was lower in the hemostatic matrix group than the control group for men (0.91 ± 0.11 vs. 1.34 ± 0.18 L) and women (0.81 ± 0.09 vs. 1.13 ± 0.14 L). A significant decrease in total blood loss with hemostatic matrix was observed versus control, with a 32.32% reduction in men and a 28.66% reduction in women (P < 0.01) [Figure 4].
Figure 4.
A bar diagram showing total calculated blood loss in each group by gender
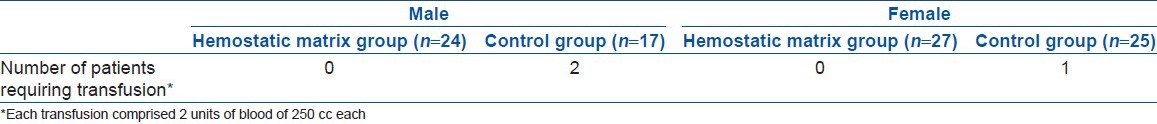
The mean (±SD) levels of calculated total blood loss in the control groups were significantly greater in men than in women (1.34 ± 0.18 vs. 1.13 ± 0.14 L; P < 0.01). In contrast, the mean (±SD) total blood loss in the hemostatic matrix groups was similar in men and women (0.91 ± 0.11 vs. 0.81 ± 0.09 L). No blood transfusions were required in the hemostatic matrix groups, whereas three patients in the control groups required transfusions [Table 3]; however, this difference was not statistically significant. The patients requiring transfusions had hemoglobin levels of 8.5, 8.7, and 8.9 g/dL.
Table 3.
Transfusion requirements for each group by gender
Two patients from the control group developed a superficial wound infection; these infections were treated successfully with oral antibiotics. No deep infections were observed. One patient in the female hemostatic matrix group received intravenous antibiotics for a chest infection following surgery. One female patient from the hemostatic matrix group developed a femoral DVT and another from the same group suffered a pulmonary embolism. There were no immunologic rejection and no fatalities.
DISCUSSION
TKA can result in major postoperative blood loss which can impact on the recovery and rehabilitation of patients and also require expensive transfusions. In our experience at San Salvatore Hospital, a transfusion bag costs approximately 300 € (395 $ USD, 21700 INR) and each transfusion requires two bags of 250 cc of blood. In comparison, the unit price of a pack of the hemostatic matrix used in this study was approximately 240 € (316 $ USD, 17360 INR). Therefore, if blood loss and transfusion requirements could be reduced through the use of this hemostatic matrix, this could translate to cost savings.
Postoperative drains are used routinely to avoid hemarthrosis following TKA. Drainage output 24 h after surgery was reduced from 0.72 L (male) and 0.65 L (female) for the control groups, to 0.22 L (male) and 0.19 L (female) for the hemostatic matrix groups. These results support those from a similar study by Wang et al.,21 in which drainage output 12 h after surgery was reduced from 0.41 L for the control group to 0.18 L for patients treated with a fibrin-sealant. The larger drainage outputs for our study are most likely due to the additional 12 h drainage time. In the first postoperative day of the study by Wang et al.,21 the hemoglobin level decreased by 2.01 g/dL in the fibrin-sealant group and by 2.73 g/dL in the control group. In our study, similar decreases in hemoglobin levels were observed after 24 h: 1.79 g/dL (male) and 1.73 g/dL (female) in the hemostatic matrix groups, and 2.48 g/dL (male) and 2.28 g/dL (female) in the control groups.
It is well documented that whilst suction drainage is a good predictor of total blood loss, it represents only a fraction of total blood loss due to bleeding into tissues and residual blood in the joint.1 In this study, we therefore determined hematocrit values (7 days after surgery) in order to calculate the total blood loss as well. As expected, all the calculated blood loss values were considerably larger than those for suction drainage, as seen by comparing Figures 2 and 4. Significant reductions in calculated blood loss were exhibited by both the male and female patients treated with hemostatic matrix. These results suggest that the use of hemostatic matrix in TKA not only reduces blood loss by drainage suction, but also by extravasation of blood into the tissues. The potential benefits of effective hemostasis using hemostatic matrix include faster functional rehabilitation and lower rates of wound infection.22,23 Only two patients who develop superficial wound infections in this study were in the control groups.
A further benefit of employing a hemostatic matrix is the potential to optimize administration of thromboprophylaxis, which is used to decrease the incidence of DVT and pulmonary embolism associated with TKA.24,25 Due to concerns that thromboprophylaxis may increase the risk of postoperative bleeding, current recommended practice in the US is to administer the drug 12 h postoperatively. Effective hemostasis would allow the thromboprophylaxis to be administered preoperatively for optimal effect as indicated by Hull et al.26 Indeed, in many European countries low molecular weight heparin is administered preoperatively for hip or knee replacement surgery.27,28 In the current study, heparin was administered 12 h preoperatively and every 24 h postoperatively, and only one case of DVT and one of pulmonary embolism were recorded, though both occurred in the hemostatic matrix treatment group. Further studies are required to assess the risk of these adverse events after the use of a hemostatic matrix in orthopedic surgery; however, in a recent study of 127 patients who received a topical hemostatic matrix/agent during spinal surgery, only two cases of DVT were recorded.14
The results from this study suggest that hemostatic matrix can safely reduce blood drainage output, as well as total blood loss following TKA, while maintaining higher hemoglobin levels. Hemostatic matrix-treated patients (n = 51) showed significant reductions in calculated postoperative blood loss of 32.3 and 28.7% versus control in men and women, respectively (P < 0.01). Drainage postoperative blood loss after 24 h was significantly less with the hemostatic matrix versus control, as there was decrease in hemoglobin levels 7 days post-surgery (each P < 0.01). The evidence of the efficacy of a matrix hemostatic agent in orthopedic surgery is supported by studies in other surgical fields, including vascular, cardiac, spinal, and sinus surgery.12,14,15,29 To evaluate the efficacy of hemostatic matrix in orthopedic surgery, it is also important to assess any reduction in the rate of blood transfusion. In this study, three patients in the control group required blood transfusion, whereas no blood transfusions were necessary within the hemostatic matrix group; however, this result was not statistically significant.
The implantation of a knee prosthesis in ischemic conditions can induce significant activation of fibrinolysis. Various studies have proposed the use of aprotinin (natural) and tranexamic acid (synthetic) as antifibrinolytic agents to reduce blood loss and transfusion requirements in orthopedic surgery.30,31 Evaluations on the effectiveness of tranexamic acid on reducing postoperative blood loss in TKA have had varying outcomes.32,33 However, in studies that have shown effectiveness for tranexamic acid, the reduction in hemoglobin and hematocrit is similar to that achieved by the hemostatic matrix in the current study.34 A meta-analysis of intravenous antifibrinolytics in orthopedic surgery showed that, when compared with placebo, intravenous aprotinin and tranexamic acid reduced the need for allogenic blood transfusion (odds ratio 0.43 and 0.17, respectively), whereas epsilon-aminocaproic acid was not efficacious.35 Additionally, a second meta-analysis of 13 studies showed that tranexamic acid reduced total blood loss by a mean of 487 mL, which is comparable to the reduction in total blood loss observed with the hemostatic matrix in this study.36 Till date, there are no studies that directly compare the hemostatic matrix used in the current study with tranexamic acid for any indication. However, when cemented TKA patients received a fibrin spray, tranexamic acid or control, only the fibrin spray significantly affected blood loss volumes compared with control, although the study may not have been adequately powered.37 Additionally, in a study of uncemented TKA, both fibrin spray and tranexamic acid were equally effective at reducing blood loss when compared with control.33 A recent study has shown that blood loss is similar between cemented and uncemented TKAs,38 potentially indicating that the results of the current study could be transferable to cemented TKA.
A number of hemostatic agents are available based on collagen, gelatin, cellulose, and fibrin adhesives, which have demonstrated efficacy. All hemostatic agents require a functional clotting cascade or other clotting factors to work, however, making them unsuitable for use in patients with acquired or inherited coagulopathy.39 In addition, their use is further exacerbated by the difficulty to apply them to especially aggressive bleeding sites or difficult to access locations.40
The study has several limitations in that it included a relatively small number of patients and that every risk or complication associated with hemostatic matrix treatment and TKA surgery could not be extensively explored. Further studies in a multicenter setting with a larger population of patients are warranted to support the current study because this relatively small number of patients do not permit the study ofall possible complication and risk, in fact almost 1000 patients should be included to have adequate power to demonstrate a minimum clinically relevant difference in outcome.
The properties of the hemostatic matrix used in this study are derived from its composition and mechanism of action. Hemostatic matrix contains two components: cross-linked gelatin particles and a human-derived thrombin solution. The compound is granular in nature, which allows it to conform the shape of the wound. The granules swell by 10-20% upon contact with blood or other fluid, causing blood vessels to constrict and reducing the flow of blood to the site of injury. Platelets become activated by the thrombin component and platelet aggregation is stimulated by the collagen component, creating a temporary platelet plug at the site of injury. The activated platelets release a number of effector molecules which assist in the coagulation cascade. The thrombin component of the matrix interacts with the patients’ fibrinogen, forming a fibrin clot. During clot formation fibrin traps the granular matrix, promoting assembly of a stable clot.40
Our study suggests that the use of the hemostatic matrix provides a safe and effective means by which to reduce blood loss and blood transfusion requirements in TKA. Furthermore, the importance of these findings was enhanced by a significant reduction in blood loss, postoperative decrease in hemoglobin levels, and a decrease in blood transfusion requirements despite preoperative thromboprophylaxis with low molecular weight heparin. These findings are not only significant with regards to patient care options, but also have important consequences with respect to the cost of patient care and suggest that future health–economic evaluations of surgical options in TKA should be considered. Future studies are also warranted to explore the use of the hemostatic matrix in situations additional to TKA, such as total hip arthroplasty and traumatology.
ACKNOWLEDGMENTS
The authors wish to thank Francesca Zia for data collection and Michele Di Francesco for assistance with statistical analyses.
Footnotes
Source of Support: Editorial assistance in the preparation of this manuscript was provided by Fishawack Communications and funded by Baxter Bio Surgery, Italy
Conflict of Interest: None.
REFERENCES
- 1.Lemaire R. Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br. 2008;90:1128–36. doi: 10.1302/0301-620X.90B9.21115. [DOI] [PubMed] [Google Scholar]
- 2.Lotke PA, Faralli VJ, Orenstein EM, Ecker ML. Blood loss after total knee replacement. Effects of tourniquet release and continuous passive motion. J Bone Joint Surg Am. 1991;73:1037–40. [PubMed] [Google Scholar]
- 3.Walker RH. Special report: Transfusion risks. Am J Clin Pathol. 1987;88:374–8. doi: 10.1093/ajcp/88.3.374. [DOI] [PubMed] [Google Scholar]
- 4.Fiebig E. Safety of the blood supply. Clin Orthop Relat Res. 1998;357:6–18. doi: 10.1097/00003086-199812000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Marcucci C, Madjdpour C, Spahn DR. Allogeneic blood transfusions: Benefit, risks and clinical indications in countries with a low or high human development index. Br Med Bull. 2004;70:15–28. doi: 10.1093/bmb/ldh023. [DOI] [PubMed] [Google Scholar]
- 6.Lemos MJ, Healy WL. Blood transfusion in orthopaedic operations. J Bone Joint Surg Am. 1996;78:1260–70. doi: 10.2106/00004623-199608000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Rizzi L, Bertacchi P, Ghezzi LM, Bellavita P, Scudeller G. Postoperative blood salvage in hip and knee arthroplasty. A prospective study on cost effectiveness in 161 patients. Acta Orthop Scand. 1998;69:31–4. doi: 10.3109/17453679809002352. [DOI] [PubMed] [Google Scholar]
- 8.Nakahara M, Sakahashi H. Effect of application of a tourniquet on bleeding factors in dogs. J Bone Joint Surg Am. 1967;49:1345–51. [PubMed] [Google Scholar]
- 9.Klenerman L, Chakrabarti R, Mackie I, Brozovic M, Stirling Y. Changes in haemostatic system after application of a tourniquet. Lancet. 1977;1:970–2. doi: 10.1016/s0140-6736(77)92276-0. [DOI] [PubMed] [Google Scholar]
- 10.Petaja J, Myllynen P, Myllyla G, Vahtera E. Fibrinolysis after application of a pneumatic tourniquet. Acta Chir Scand. 1987;153:647–51. [PubMed] [Google Scholar]
- 11.Radosevich M, Goubran HI, Burnouf T. Fibrin sealant: Scientific rationale, production methods, properties, and current clinical use. Vox Sang. 1997;72:133–43. doi: 10.1046/j.1423-0410.1997.7230133.x. [DOI] [PubMed] [Google Scholar]
- 12.Oz MC, Cosgrove DM, 3rd, Badduke BR, Hill JD, Flannery MR, Palumbo R, et al. Controlled clinical trial of a novel hemostatic agent in cardiac surgery. The Fusion Matrix Study Group. Ann Thorac Surg. 2000;69:1376–82. doi: 10.1016/s0003-4975(00)01194-2. [DOI] [PubMed] [Google Scholar]
- 13.Reuthebuch O, Lachat ML, Vogt P, Schurr U, Turina M. FloSeal: A new hemostyptic agent in peripheral vascular surgery. Vasa. 2000;29:204–6. doi: 10.1024/0301-1526.29.3.204. [DOI] [PubMed] [Google Scholar]
- 14.Renkens KL, Jr, Payner TD, Leipzig TJ, Feuer H, Morone MA, Koers JM, et al. A multicenter, prospective, randomized trial evaluating a new hemostatic agent for spinal surgery. Spine (Phila Pa 1976) 2001;26:1645–50. doi: 10.1097/00007632-200108010-00002. [DOI] [PubMed] [Google Scholar]
- 15.Mathiasen RA, Cruz RM. Prospective, randomized, controlled clinical trial of a novel matrix hemostatic sealant in children undergoing adenoidectomy. Otolaryngol Head Neck Surg. 2004;131:601–5. doi: 10.1016/j.otohns.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 16.Richter F, Schnorr D, Deger S, Trk I, Roigas J, Wille A, et al. Improvement of hemostasis in open and laparoscopically performed partial nephrectomy using a gelatin matrix-thrombin tissue sealant (FloSeal) Urology. 2003;61:73–7. doi: 10.1016/s0090-4295(02)02143-x. [DOI] [PubMed] [Google Scholar]
- 17.Gall RM, Witterick IJ, Shargill NS, Hawke M. Control of bleeding in endoscopic sinus surgery: Use of a novel gelatin-based hemostatic agent. J Otolaryngol. 2002;31:271–4. doi: 10.2310/7070.2002.29810. [DOI] [PubMed] [Google Scholar]
- 18.Floseal Hemostatic Matrix Instructions For Use. [Last Accessed on 2012 Apr 05]. Available from: http://www.baxter.com/products/biopharmaceuticals/downloads/FloSeal_PI.pdf .
- 19.Marmor L, Avoy DR, McCabe A. Effect of fibrinogen concentrates on blood loss in total knee arthroplasty. Clin Orthop Relat Res. 1991;273:136–8. [PubMed] [Google Scholar]
- 20.Nadler SB, Hidalgo JU, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–32. [PubMed] [Google Scholar]
- 21.Wang GJ, Hungerford DS, Savory CG, Rosenberg AG, Mont MA, Burks SG, et al. Use of fibrin sealant to reduce bloody drainage and hemoglobin loss after total knee arthroplasty: A brief note on a randomized prospective trial. J Bone Joint Surg Am. 2001;83-A:1503–5. doi: 10.2106/00004623-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet. 1996;348:1055–60. doi: 10.1016/S0140-6736(96)04330-9. [DOI] [PubMed] [Google Scholar]
- 23.Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop Relat Res. 1998;347:188–93. [PubMed] [Google Scholar]
- 24.McKenna R, Bachmann F, Kaushal SP, Galante JO. Thromboembolic disease in patients undergoing total knee replacement. J Bone Joint Surg Am. 1976;58:928–32. [PubMed] [Google Scholar]
- 25.Stringer MD, Steadman CA, Hedges AR, Thomas EM, Morley TR, Kakkar VV. Deep vein thrombosis after elective knee surgery. An incidence study in 312 patients. J Bone Joint Surg Br. 1989;71:492–7. doi: 10.1302/0301-620X.71B3.2785998. [DOI] [PubMed] [Google Scholar]
- 26.Hull RD, Brant RF, Pineo GF, Stein PD, Raskob GE, Valentine KA. Preoperative vs Postoperative Initiation of Low-Molecular-Weight Heparin Prophylaxis Against Venous Thromboembolism in Patients Undergoing Elective Hip Replacement. Arch Intern Med. 1999;159:137–41. doi: 10.1001/archinte.159.2.137. [DOI] [PubMed] [Google Scholar]
- 27.Strebel N, Prins M, Agnelli G, Buller HR. Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med. 2002;162:1451–6. doi: 10.1001/archinte.162.13.1451. [DOI] [PubMed] [Google Scholar]
- 28.Perka C. Preoperative versus postoperative initiation of thromboprophylaxis following major orthopedic surgery: Safety and efficacy of postoperative administration supported by recent trials of new oral anticoagulants. Thromb J. 2011;9:17. doi: 10.1186/1477-9560-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jameson M, Gross CW, Kountakis SE. Flo Seal use in endoscopic sinus surgery: Effect on postoperative bleeding and synechiae formation. Am J Otolaryngol. 2006;27:86–90. doi: 10.1016/j.amjoto.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 30.Hiippala S, Strid L, Wennerstrand M, Arvela V, Mantyla S, Ylinen J, et al. Tranexamic acid (Cyklokapron) reduces perioperative blood loss associated with total knee arthroplasty. Br J Anaesth. 1995;74:534–7. doi: 10.1093/bja/74.5.534. [DOI] [PubMed] [Google Scholar]
- 31.Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: A prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br. 1996;78:434–40. [PubMed] [Google Scholar]
- 32.Engel JM, Hohaus T, Ruwoldt R, Menges T, Jurgensen I, Hempelmann G. Regional hemostatic status and blood requirements after total knee arthroplasty with and without tranexamic acid or aprotinin. Anesth Analg. 2001;92:775–80. doi: 10.1097/00000539-200103000-00041. [DOI] [PubMed] [Google Scholar]
- 33.Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland DE. Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: A prospective, randomised controlled trial. J Bone Joint Surg Br. 2007;89:306–9. doi: 10.1302/0301-620X.89B3.17565. [DOI] [PubMed] [Google Scholar]
- 34.Ortega-Andreu M, Perez-Chrzanowska H, Figueredo R, Gomez-Barrena E. Blood loss control with two doses of tranexamic Acid in a multimodal protocol for total knee arthroplasty. Open Orthop J. 2011;5:44–8. doi: 10.2174/1874325001105010044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zufferey P, Merquiol F, Laporte S, Decousus H, Mismetti P, Auboyer C, et al. Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology. 2006;105:1034–46. doi: 10.1097/00000542-200611000-00026. [DOI] [PubMed] [Google Scholar]
- 36.Zhang H, Chen J, Chen F, Que W. The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20:1742–52. doi: 10.1007/s00167-011-1754-z. [DOI] [PubMed] [Google Scholar]
- 37.McConnell JS, Shewale S, Munro NA, Shah K, Deakin AH, Kinninmonth AW. Reducing blood loss in primary knee arthroplasty: A prospective randomised controlled trial of tranexamic acid and fibrin spray. Knee. 2012;19:295–8. doi: 10.1016/j.knee.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Ishii Y, Matsuda Y. Perioperative blood loss in cementless or hybrid total knee arthroplasty without patellar resurfacing: A prospective, randomized study. J Arthroplasty. 2005;20:972–6. doi: 10.1016/j.arth.2004.12.059. [DOI] [PubMed] [Google Scholar]
- 39.Izzo F, Di Giacomo R, Falco P, Piccirillo M, Iodice R, Pio Orlando A, et al. Efficacy of a haemostatic matrix for the management of bleeding patients undergoing liver resection: Results from 237 cases. Curr Med Res Opin. 2008;24:1011–5. doi: 10.1185/030079908x280392. [DOI] [PubMed] [Google Scholar]
- 40.Oz MC, Rondinone JF, Shargill NS. Flo Seal Matrix: New generation topical hemostatic sealant. J Card Surg. 2003;18:486–93. doi: 10.1046/j.0886-0440.2003.00302.x. [DOI] [PubMed] [Google Scholar]


