Abstract
Background:
The relationship between medial meniscus tear and posterior cruciate ligament (PCL) injury has not been exactly explained. We studied to investigate the biomechanical effect of partial and complete PCL transection on different parts of medial meniscus at different flexion angles under static loading conditions.
Materials and Methods:
Twelve fresh human cadaveric knee specimens were divided into four groups: PCL intact (PCL-I), anterolateral bundle transection (ALB-T), posteromedial bundle transection (PMB-T) and PCL complete transection (PCL-T) group. Strain on the anterior horn, body part and posterior horn of medial meniscus were measured under different axial compressive tibial loads (200-800 N) at 0°, 30°, 60° and 90° knee flexion in each groups respectively.
Results:
Compared with the PCL-I group, the PCL-T group had a higher strain on whole medial meniscus at 30°, 60° and 90° flexion in all loading conditions and at 0° flexion with 400, 600 and 800 N loads. In ALB-T group, strain on whole meniscus increased at 30°, 60° and 90° flexion under all loading conditions and at 0° flexion with 800 N only. PMB-T exihibited higher strain at 0° flexion with 400 N, 600 N and 800 N, while at 30° and 60° flexion with 800 N and at 90° flexion under all loading conditions.
Conclusions:
Partial PCL transection triggers strain concentration on medial meniscus and the effect is more pronounced with higher loading conditions at higher flexion angles.
Keywords: Biomechanics, medial meniscus, posterior cruciate ligament
INTRODUCTION
The menisci are critical components of a healthy knee joint and play a crucial role in load bearing, load transmission, shock absorption, as well as lubrication and nutrition of articular cartilage.1,2,3,4,5 Ahmed et al. showed that menisci can transmit 50% to 70% tibiofemoral compressive load in extension knee and up to 85% to 90° in flexed knee.6 Meniscal injury is the most common knee injury, the overall rate being 0.7 per 1000 people per year.7 The National Center of Health Statistics8 reported more than 450,000 arthroscopic meniscectomies performed each year in United States. Complete or partial loss of a meniscus can decrease tibiofemoral contact area, increase contact stress on the articular cartilage and reduce its shock-absorbing capabilities, leading to serious long term sequelae.9,10
The clinical and biomechanical data on relationship between PCL injuries and menisci are scanty.11,12,13 Pearsall et al. showed that meniscal strain increased with complete PCL injury and returned to normal after PCL reconstruction.14 Little is known about the biomechanical disorder in partial PCL transection cases and its impact on different parts of meniscal strain under various loading conditions.
Based on this background, we hypothesized that the resultant force on medial meniscus was significantly elevated in incomplete PCL transection. We employed a biomechanical testing system to measure the strain on the different parts of medial meniscus (anterior, posterior horn and body of meniscus) with intact PCL (PCL-I), anterolateral bundle transection (ALB-T), posteromedial bundle transection (PMB-T) and PCL complete transection (PCL-T) under different axial compressive tibial loads (200-800 N) at 0°, 30°, 60° and 90° of knee flexion, respectively.
MATERIALS AND METHODS
Specimen preparation
The experiment was performed with the approval of the local hospital ethics committee. Twelve fresh frozen male cadaveric knee specimens (six left and six right specimens) were used in this study, with an average age of 32.7 years (range 26-39 years). All the specimens underwent macroscopic inspection and the posterior drawer test to rule out gross anomalies like degenerative changes, fracture, tumor and PCL damage. Prior to experiments, the femur and tibia were cut to approximately 30 cm from the joint line; the proximal portion of fibula was retained and secured to tibia at its anatomic position using a cortical screw. Each specimen was dissected to the joint capsule withcare taken to maintain the meniscocapsular attachments to tibia. The collateral and cruciate ligaments, tibiofemoral joint and popliteus were left intact.
Twelve specimens were fixed in cylindrical clamps of universal testing machine (CSS-88100, Chang Chun, China) which was capable of applying a specific load or positioning the knee at a predetermined flexion angle with the femur on lower and tibia on the upper fixture [Figure 1a]. The strain transducer gauge (BX120-1AA, HY Corp., ZheJiang, China) was used that converts tissue strain into voltage change that could be recorded by a computer equipped with an analog-to-digital converter.15,16,17 In our experiment, 5 × 5 mm tissue in the anterior horn, body and posterior horn of medial meniscus were exposed and burnished with abrasive paper, followed by degreasing. When dried, a strain gauge was fixed vertically with α-cyanoacrylate in a direction consistent with the load [Figure 1b]. The joint capsule was closed and strain foil inside was connected to the output of static strain indicator (DH-3818, DH Corp., JiangSu, China).
Figure 1.
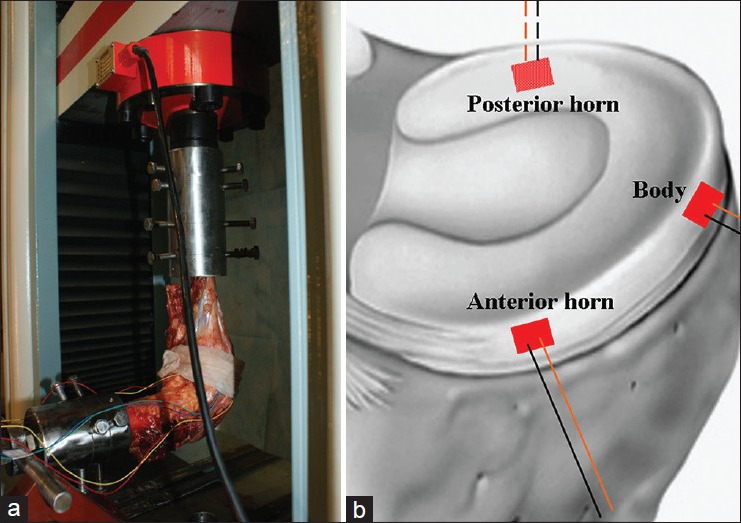
Photographs showing (a) Biomechanical test instrumentation setup and (b) transducer strain gauges fixed in different parts of medial meniscus
Experimental design
The specimens were divided into four groups: PCL-I as control, ALB-T, PMB-T and PCL-T groups. The experiment was conducted in three statges. Stage I: 12 specimens with PCL-I. Stage II: 12 specimens were randomly divided in ALB-T and PMB-T groups. State III: 12 specimens with PCL-T. In each stage, the specimens were positioned at 0°, 30°, 60° and 90° of knee flexion in sequence.
At the beginning, we loaded the specimens 20 times at 200 N with a speed of 0.5 mm/s to eliminate the influence of innate viscosity. After that, the static strain measuring device was calibrated in balance and then continuous axial load (0-800 N) was loaded at a speed of 0.5 mm/s. Data at 200, 400, 600 and 800 N from every channel of the device were documented (μe, microstrain). The same procedure was repeated when it came to 30°, 60° and 90° of flexion, with an interval of 10 min to allow restoration of elasticity. Finishing the aforementioned tests, we separated the 12 specimens randomly and equally into ALB-T and PMB-T groups, followed by same test as mentioned earlier. Next, the PCL of all 12 specimens was severed completely, modeling complete PCL transection. Then, the same biochemical test was performed on the newly treated specimens again. During the whole test, the specimens were kept at a humidity of 60-80% and a temperature of 25°C.
Statistical analysis
Data analysis was performed with SPSS version 17.0 (Chicago, IL, USA). Data were expressed as mean ± SD. Differences were considered statistically significant when P < 0.05. A one-way analysis of variance (ANOVA) was performed to determine whether there were statistically significant differences among the experimental groups. When the populations from which the samples were normally or approximate normal distribution and the variances of the populations were equal, the Student's t-test was employed to compare the means of two independent groups. While the variances of the strain value in anterior horn and body of meniscus under loads of 200 and 400 N at 0° of flexion were not equal among the groups, comparisons between groups were made using Mann–Whitney U test.
RESULTS
Strain analysis at 0° flexion
At 0° flexion, the strain value in whole medial meniscus was negative in response to axial load, indicating that the strain in this position was a compressive strain [Figure 2]. Under 200 N load, the strain on whole medial meniscus in ALB-T, PMB-T and PCL-T groups were not statistically different from those in the PCL-I group (P > 0.05). Under 400 and 600 N loads, the strain on whole medial meniscus in ALB-T group was not statistically different from those in the PCL-I group (P > 0.05). However, the strain on whole medial meniscus in the PMB-T and PCL-T groups were markedly greater than those in the PCL intact group (P < 0.05). Under 800 N load, the ALB-T, PMB-T and PCL-T groups had significantly increased strain values (P < 0.05) in comparison to the PCL-I group.
Figure 2.
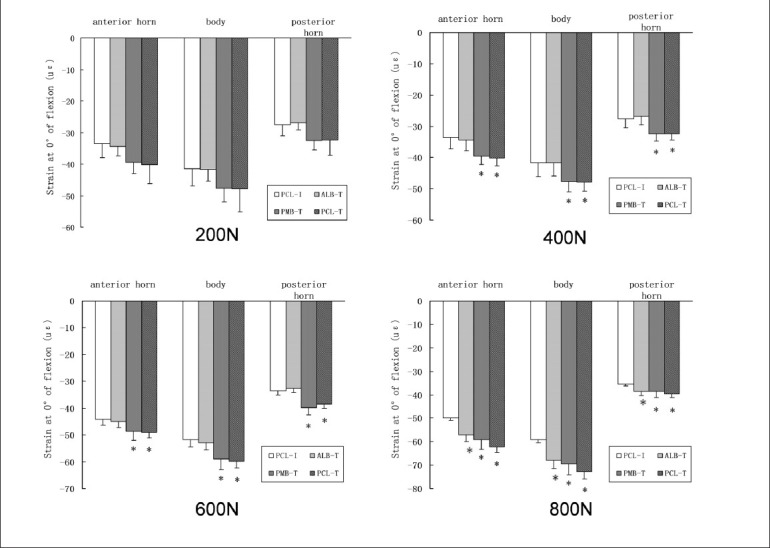
A bar diagram showing strain value on medial meniscus at 0° of flexion (εμ, microstrain; *P<0.05 compared to PCL-I)
Strain analysis at 30° flexion
At 30° of flexion, compression strain was found in body of meniscus in all groups, in anterior horn of meniscus in ALB-T and PCL-T groups and in posterior horn of meniscus in PCL-I and PMB-T groups. The strain value in anterior horn of meniscus in PCL-I and PMB-T groups and in posterior horn of meniscus in ALB-T and PCL-T groups was positive in response to axial load, indicating that the strain was a tension strain. ALB-T and PCL-T groups had higher strain than PCL-I in all parts of medial meniscus under all 4 loading conditions. Compared with the PCL-I group, PMB-T group did not have significantly increased strain values under loads of 200, 400 and 600 N (P > 0.05), whereas under 800 N load the strain values were markedly increased (P < 0.05) [Figure 3].
Figure 3.
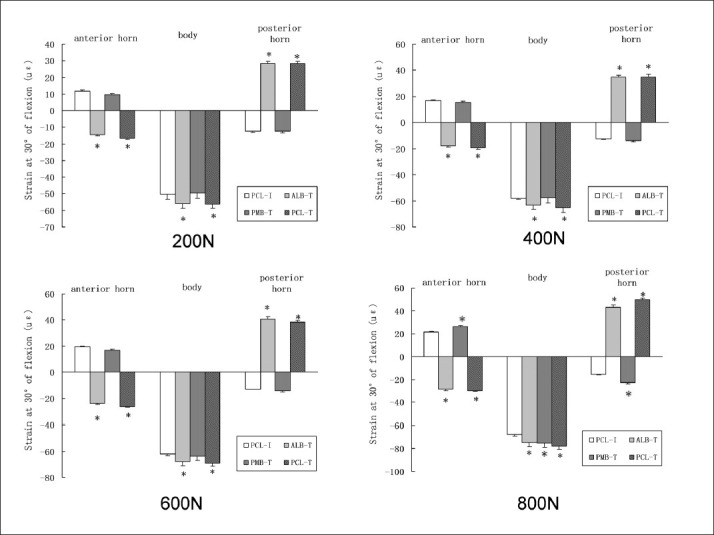
A bar diagram showing strain value on medial meniscus at 30° of flexion (εμ, microstrain; *P<0.05 compared to PCL-I)
Strain analysis at 60° flexion
The trends with respect to strain state were similar between 60° of flexion and 30° of flexion [Figure 4]. Compared to the control, strain value increased significantly on whole meniscus in ALB-T and PCL-T groups under all four loading conditions and in PMB-T group under 800 N load (P < 0.05).
Figure 4.
A bar diagram showing strain value on medial meniscus at 60° of flexion (εμ, microstrain; *P<0.05 compared to PCL-I)
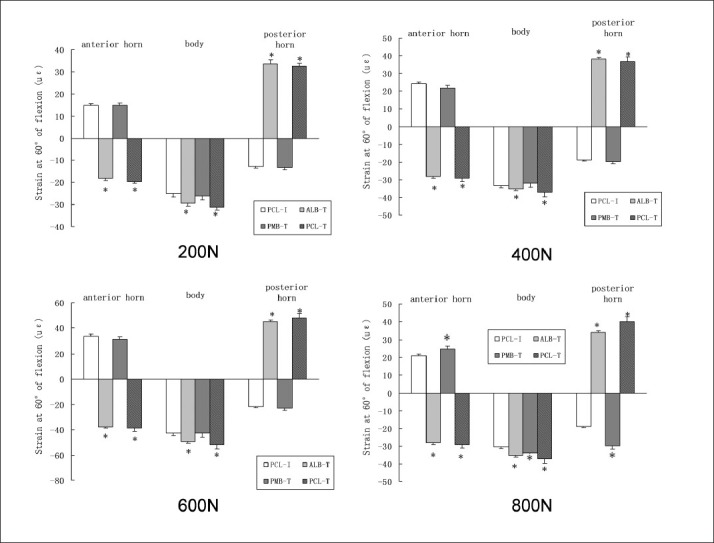
Strain analysis at 90° of flexion
Strain state in whole medial meniscus at 90° of flexion was similar to that at 30° of flexion [Figure 5]. Significant higher strain value on whole meniscus was observed in ALB-T, PMB-T and PCL-T groups compared with the PCL-I group all four loading conditions (P < 0.05).
Figure 5.
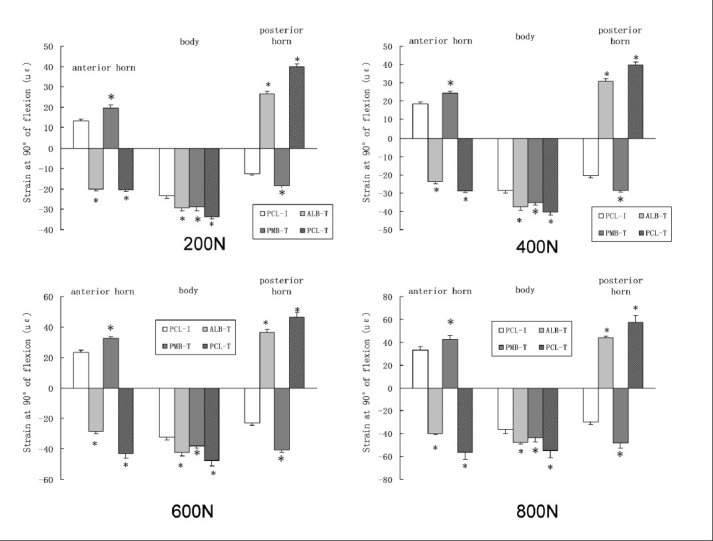
A bar diagram showing strain value on medial meniscus at 90° of flexion (εμ, microstrain; *P<0.05 compared to PCL-I)
DISCUSSION
PCL is considered to be the primary restraint to posterior knee translation and a secondary restraint to varus, valgus and external rotation of knee joint.18,19,20 Although an isolated PCL injury is often regarded as less disabling than an isolated injury to the ACL, many authors have reported clinical sequela associated with PCL injury.21,22,23 Boynton et al. reported that eight (21%) patients had meniscal injury after PCL injuries.24 Biomechanical studies have shown increased contact pressures in the patellofemoral and medial compartments following PCL loss.25 Normally, the medial meniscus carries 50% of the medial compartment load with knee fully extended. The interrelationship between the loss of the load-bearing role of the meniscus after meniscectomy and the development of osteoarthritis is well documented.26,27 Therefore, secondary damage of the medial meniscus may be considered as a reason of the development of medial compartment osteoarthritis, followed by PCL deficiency.
The results in our study showed that partial and complete PCL transaction did not increase medial meniscus strain under 200 N load at 0° flexion. Pearsall et al. reported.14 that PCL injury minimally changes posterior tibial translation at 0° under 200 N load, thereby having a minimal effect on meniscal strain. However, PMB and PCL transection increased medial meniscus strain under 400, 600 and 800N loads. This may be due to PMB becoming tight and the ALB slack when the knee is at 0° of flexion.28 PMB transection can cause posterior tibial translocation in extension increasing the strain on medial meniscus. The present study showed that ALB and PCL transection increased medial meniscus strain at 30°, 60° and 90° of flexion under all loading conditions. In higher flexion, the ALB is tight, whereas the PMB is slack.28 Therefore, ALB transection can increase posterior tibial translocation in flexion, which results in increased strain on the medial meniscus. While under 800 N load, both partial and complete PCL transaction increased medial meniscus strain. The posterior tibial translation increased gradually with increasing knee loads after PCL transaction, which can lead to increased meniscal strain. At 90° of flexion, both partial and complete PCL transaction also increased medial meniscus strain. Castle et al.29 assessed static squatting with PCL deficiency resulting in a mean increase in posterior translation of 7.4 mm for high angle squats (70-90° flexion) compared to 2.1 mm for low flexion squats (32-50° flexion). Increase in posterior tibial translation in PCL deficient knee at higher flexion angle may explain increased medial meniscal strain. The current data also demonstrate that the effect of PCL state on meniscal strain was more pronounced under higher loading conditions at higher flexion angles.
It has been reported that ALB get strained in the process of flexion28 and the PMB rupture, strained medial meniscus at 0° under 400, 600 and 800 N loads, which suggested that PMB played significant role in anterior movement constraint in full extension.28 In view of this, we can easily recognize that the two bundles of PCL contribute to the stabilization of knee joint in a complementary manner and medial meniscus strain may remarkably elevate no matter which part of PCL is transected.
This study also showed that in physiological status, the knee joint harbored the biggest strain at 0° and 30° of flexion on body part of medial meniscus in PCL intact group. Physiologically, weight bearing area of medial meniscus locates on its body carries the maximum load between 0-30° flexion.17 Thus, abnormal strains generated from anterior/posterior translation and internal/external rotation of medial femoral condyle at the 0-30° flexion resulted in body tear of medial meniscus more easily.30 When flexed at an angle more than 60°, as the motion center of medial femoral condyle shifted, strain onthe body decreased so that the posterior horn instead of the body became the major weight bearing area. At this situation, posterior horn played the major part of knee joint stability maintenance and constrained the anterior translation of tibia.31 Therefore, the tear of posterior horn of the meniscus occurs more commonly at an angle more than 60° after PCL transection.
There are several limitations to this study. First, the dissection of soft tissue surrounding the knee joint could have some influence on the exact value in different loading conditions. It is suggested to simulate normal muscle forces acting around the knee. Secondly, the weight-bearing lunge was scanned at each flexion angle in the current study and did not measure dynamic motion of the joint. Thirdly, it is a cadaveric study and so cannot simulate the complex loading conditions in the normal knee such as tibial rotation and mediolateral forces.
Subject to these limitations, the current study demonstrates that similar to complete PCL transection, partial PCL transection triggers strain concentration on medial meniscus and the effect is more pronounced with higher loading conditions at higher flexion angles. Increased load on meniscus may lead to meniscal degeneration and rupture.
Footnotes
Source of Support: The study was supported by the National 863 project of China (2011AA030101), National Natural Science Foundation of China (NO. 81201420, 81272034), the Young Teacher's boosting project of the Fundamental Research Funds for the Central Universities in Central South University (2012QNZT103, 2012QNZT095) and National Clinical Key Department Construction Projects of China
Conflict of Interest: None.
REFERENCES
- 1.Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: Structure-function, pathophysiology, current repair techniques and prospects for regeneration. Biomaterials. 2011;32:7411–31. doi: 10.1016/j.biomaterials.2011.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishimuta JF, Levenston ME. Response of cartilage and meniscus tissue explants to in vitro compressive overload. Osteoarthritis Cartilage. 2012;20:422–9. doi: 10.1016/j.joca.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai JH, Levenston ME. Meniscus and cartilage exhibit distinct intra-tissue strain distributions under unconfined compression. Osteoarthritis Cartilage. 2010;18:1291–9. doi: 10.1016/j.joca.2010.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lubowitz JH, Poehling GG. Save the meniscus. Arthroscopy. 2011;27:301–2. doi: 10.1016/j.arthro.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Tissakht M, Ahmed AM, Chan KC. Calculated stress-shielding in the distal femur after total knee replacement corresponds to the reported location of bone loss. J Orthop Res. 1996;14:778–85. doi: 10.1002/jor.1100140515. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed A, Burke D. In-vitro measurement of static pressure distribution in synovial joints, part I: Tibial surface of the knee. J Biomech Eng. 1983;105:216–25. doi: 10.1115/1.3138409. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen AB, Yde J. Epidemiology of acute knee injuries: A prospective hospital investigation. J Trauma. 1991;31:1644–8. doi: 10.1097/00005373-199112000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Vol. 2003. Hyattsville: NCHS; 1996. National Center for Health Statistics. Number of ambulatory surgery procedures by procedure category in the US; p. 7. [Google Scholar]
- 9.Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: A comparative in vivo study. J Biomed Eng. 1983;5:157–61. doi: 10.1016/0141-5425(83)90036-5. [DOI] [PubMed] [Google Scholar]
- 10.McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–56. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 11.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg. 1982;64A:883–8. [PubMed] [Google Scholar]
- 12.Kohn D. Arthroscopy in acute injuries of anterior cruciate-deficient knees: Fresh and old intraarticular lesions. Arthroscopy. 1986;2:98–102. doi: 10.1016/s0749-8063(86)80022-6. [DOI] [PubMed] [Google Scholar]
- 13.Wickiewicz TL. Meniscal injuries in the cruciate-deficient knee. Clin Sports Med. 1990;9:681–94. [PubMed] [Google Scholar]
- 14.Pearsall AW, 4th, Hollis JM. The effect of posterior cruciate ligament injury and reconstruction on meniscal strain. Am J Sports Med. 2004;32:1675–80. doi: 10.1177/0363546504265937. [DOI] [PubMed] [Google Scholar]
- 15.Gao SG, Jiang W, Lei GH, Xu M, Yu F, Li KH. Effect of posterior cruciate ligament rupture on biomechanical features of the medial femoral condyle. Orthop Surg. 2011;3:205–10. doi: 10.1111/j.1757-7861.2011.00138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao SG, Lei GH, He HB, Liu H, Xiao WF, Wen T, et al. Biomechanical comparison of lumbar total disc arthroplasty, discectomy and fusion: Effect on adjacent-level disc pressure and facet joint force. J Neurosurg Spine. 2011;15:507–14. doi: 10.3171/2011.6.SPINE11250. [DOI] [PubMed] [Google Scholar]
- 17.Jiang W, Gao SG, Li KH, Luo L, Li YS, Luo W, et al. Impact of Partial and complete rupture of anterior cruciate ligament on medial meniscus: A cadavaric study. Indian J Orthop. 2012;46:514–9. doi: 10.4103/0019-5413.101040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pournaras J, Symeonides PP, Karkavelas G. The significance of the posterior cruciate ligament in the stability of the knee. An experimental study in dogs. J Bone Joint Surg Br. 1983;65:204–9. doi: 10.1302/0301-620X.65B2.6826632. [DOI] [PubMed] [Google Scholar]
- 19.Voos JE, Mauro CS, Wente T, Warren RF, Wickiewicz TL. Posterior cruciate ligament: Anatomy, biomechanics and outcomes. Am J Sports Med. 2012;40:222–31. doi: 10.1177/0363546511416316. [DOI] [PubMed] [Google Scholar]
- 20.Bowman KF, Jr, Sekiya JK. Anatomy and biomechanics of the posterior cruciate ligament, medial and lateral sides of the knee. Sports Med Arthrosc. 2010;18:222–9. doi: 10.1097/JSA.0b013e3181f917e2. [DOI] [PubMed] [Google Scholar]
- 21.Dandy DJ, Pusey R. The long term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg. 1982;64:92–4. doi: 10.1302/0301-620X.64B1.7068728. [DOI] [PubMed] [Google Scholar]
- 22.Keller P, Shelbourne K, McCdrroll J, Rettig A. Non-operatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21:132–6. doi: 10.1177/036354659302100122. [DOI] [PubMed] [Google Scholar]
- 23.Parolie JM, Bergfeld JA. Long term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35–8. doi: 10.1177/036354658601400107. [DOI] [PubMed] [Google Scholar]
- 24.Boynton M, Tietjens B. Long term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24:306–11. doi: 10.1177/036354659602400310. [DOI] [PubMed] [Google Scholar]
- 25.Levy BA, Boyd JL, Stuart MJ. Surgical treatment of acute and chronic anterior and posterior cruciate ligament and lateral side injuries of the knee. Sports Med Arthrosc. 2011;19:110–9. doi: 10.1097/JSA.0b013e3182191c75. [DOI] [PubMed] [Google Scholar]
- 26.Bae JY, Park KS, Seon JK, Kwak DS, Jeon I, Song EK. Biomechanical analysis of the effects of medial meniscectomy on degenerative osteoarthritis. Med Biol Eng Comput. 2012;50:53–60. doi: 10.1007/s11517-011-0840-1. [DOI] [PubMed] [Google Scholar]
- 27.Petty CA, Lubowitz JH. Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8 years’ followup. Arthroscopy. 2011;27:419–24. doi: 10.1016/j.arthro.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 28.Rudy TW, Livesay GA, Woo SL, Fu FH. A combined robotic/universal force sensor approach to determine in situ forces of knee ligaments. J Biomech. 1996;29:1357–60. doi: 10.1016/0021-9290(96)00056-5. [DOI] [PubMed] [Google Scholar]
- 29.Castle TH, Jr, Noyes FR, Grood ES. Posterior tibial subluxation of the posterior cruciate-deficient knee. Clin Orthop. 1992;284:193–202. [PubMed] [Google Scholar]
- 30.Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10:168–76. doi: 10.5435/00124635-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Bonnin M, Carret JP, Dimnet J, Dejour H. The weightbearing knee after anterior cruciate ligament rupture. An in vitro biomechanical study. Knee Surg Sports Traumatol Arthrosc. 1996;3:245–51. doi: 10.1007/BF01466627. [DOI] [PubMed] [Google Scholar]


