Abstract
Fungal prosthetic joint infection after total knee arthroplasty (TKA) is a rare complication. Lacunae exist in the management of this complication. 62 year old lady presented with pain and swelling in left knee and was diagnosed as Candida tropicalis fungal infection after TKA. She underwent debridement, resection arthroplasty and antifungal plus antibiotic loaded cement spacer insertion, antifungal therapy with fluconazole followed by delayed revision TKA and further fluconazole therapy. Total duration of fluconazole therapy was 30 weeks. At 2 year followup, she has pain less range of motion of 10°-90° and there is no evidence of recurrence of infection.
Keywords: Candida tropicalis, fluconazole therapy, infected total knee arthroplasty, revision total knee arthroplasty
INTRODUCTION
Prosthetic joint infections (PJI) are a serious complication associated with total knee replacement (TKA).1 Fungal PJI is a rare occurrence with few cases reported.1,2,3,4,5,6 Phelan et al. reported the first case of candidal PJI in 1979.3 Candida albicans is the most commonly isolated fungus.3 To the best of our knowledge, this is the first fungal PJI reported from India, with Candida tropicalis being the causative organism.
CASE REPORT
A 62 year old hypertensive non diabetic female presented with pain, swelling in the left knee and difficulty in walking in the left knee for the last 6 weeks. A TKA of the left knee was done 2 years ago. She had an uneventful period after the TKA.
On examination, a 15 cm vertical midline surgical scar healed by primary intention of the initial TKA was present on anterior aspect of knee. The local temperature was raised. The range of motion was terminally restricted in flexion and was associated with pain. No deformity was noted, however, mediolatera instability was present. Patient was neurologically intact and distal pulsations were well felt.
Radiologically, there was osteolysis over the anterior femoral cortex, posterior femoral condyles and under the tibial base plate [Figure 1]. Complete hematological study and urine microscopy revealed no significant abnormality besides elevated erythrocyte sedimentation rate (ESR) (75 mm at 1 hour) and C-reactive protein (CRP) (84 mg/l).
Figure 1.
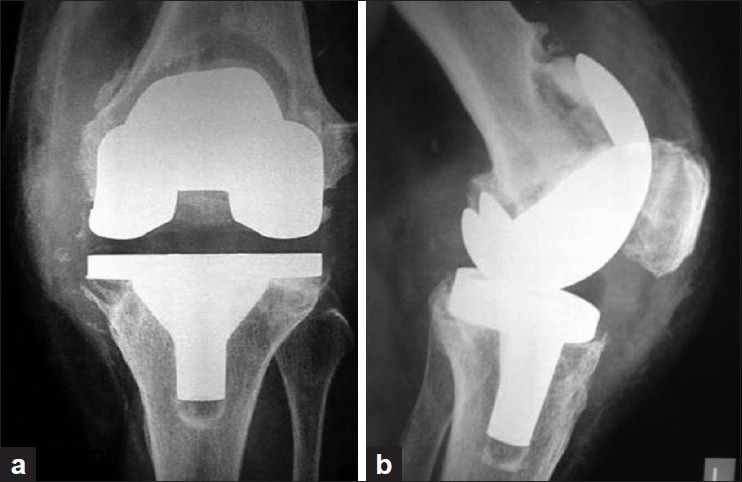
Anteroposterior (a) and lateral radiographs (b) of knee joint showing osteolysis around femoral and tibial components. TKA was done 2 years ago
Knee joint aspiration was carried out under sterile conditions. The fluid obtained was sent for analysis. Characteristics of the aspirate were 5 ml fluid, cloudy with low viscosity, white blood cell count was 15,000/cubic mm, with 68% polymorphonuclear leucocytes. Gram staining was negative, but 10% KOH mount, done to rule out fungal infection as a standard hospital protocol, was positive suggesting a fungal infection.
A decision to perform 1st stage of revision TKA was taken after consultation with the patient and her family. In consultation with infectious disease specialist, it was decided to culture and identify the organism on intraoperative samples. The previous vertical incision was used to approach the joint. Per-operatively there was turbid synovial fluid, granulation tissue, implant loosening and adherent cement Synovial fluid and tissue was sent for culture and sensitivity studies.
Implant removal, debridement and antibiotic (vancomycin) plus antifungal (amphotericin B) impregnated cement spacer insertion was done [Figure 2]. Post-operative period was uneventful [Figure 3]. Medical therapy included intravenous fluconazole 400 mg OD for 6 weeks followed by oral fluconazole 400 mg BD for 12 weeks. Bacterial culture was negative. Fungal culture was positive for Candida tropicalis. Sabouraud dextrose agar and the rapid API 20 microtube system were used for identification of species. Antifungal sensitivity was performed on the isolate.
Figure 2.
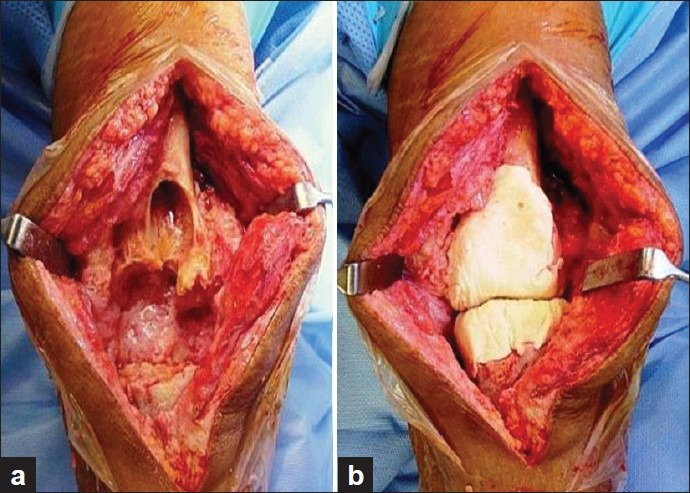
Peroperative clinical photographs showing first stage of revision total knee replacement, after implant (a) removal and cement spacer inserted (b)
Figure 3.

Anteroposterior radiograph of the knee joint showing cement spacer
Patient was followed up at weekly intervals and after 20 weeks, the ESR (23 mm at 1 hour) and CRP (6.3 mg/l) were within normal limits. Repeat aspiration was sterile. During the 2nd stage of revision, TKA quadriceps snip technique was used. Spacer was removed; the defect was non contained involving cortical and metaphyseal bone. TC3 Depuy system and fluted stems were implanted (Depuy, India). Posterior femoral augmentation and reconstruction with allograft was done. Femoral head allograft was used as bone graft to fill up the defect. There was no maltracking of patella [Figure 4]. Tissue was sent for microbial analysis, which turned negative. Postoperative period was uneventful and patient was discharged on oral fluconazole 400 mg BD for 10 weeks.
Figure 4.
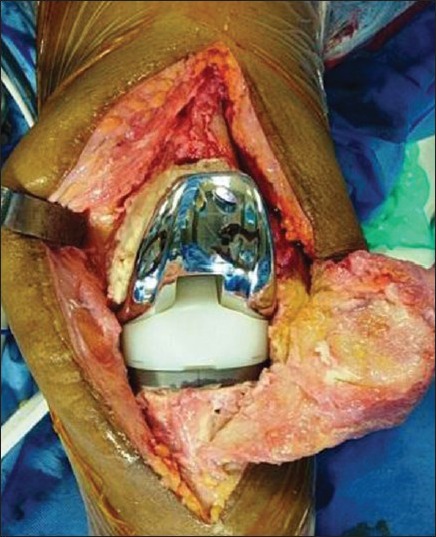
Peroperative clinical photograph showing second stage of revision total knee replacement with final implants
The surgical wound healed adequately and after physiotherapy, a painless range of motion of 10-90° with a stable knee was obtained. We did not use any scoring system pre or postoperatively. Patient maintained status quo until last followup 24 months after 2nd stage of revision surgery [Figure 5].
Figure 5.
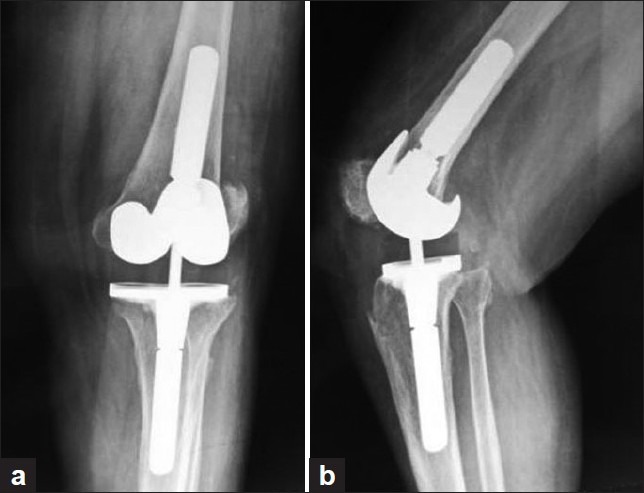
Anteroposterior (a) and lateral (b) photographs of knee joint at 24 months followup showing implant in situ
DISCUSSION
Fungal PJI is known to occur in patients who are immunocompromised, have a underlying systemic illness or prolonged use of antibiotics.1,2,3,4,5 Despite this almost half the cases occur in patients without any identifiable risk factor.3 Our patient had no identifiable risk factor.
C.albicans is the most common cause for fungal PJI reported in English literature.1,2,3,4,5,6,7,8,9,10 Most of the reported cases, do not have systemic fungal disease.4 Wu and Hsu reported a patient with preoperative cutaneous candidiasis who developed candidal PJI.10 No primary source of candidal infection was identified in our case. There is very minimal probability of being implanted during the primary surgery (The primary TKA was over 2 years and symptoms are 6 weeks old). Late infections probably are hematogenous; however, a definitive answer cannot be given.
Debridement with successful retention of the implants and suppressive antifungal therapy has been reported.4,6,7,8 In few initial reports, surgeons performed debridement and resection arthroplasty alone, but this led to poor functional outcomes.3 Delayed reimplantation offers the best chance to a successful functional outcome.1,2,3 We followed the same principle and performed a two stage revision arthroplasty.
There wasn’t any significant slimy layer at bone cement interface in our case. However, biofilms do form in fungal infection similar to the bacterial infections. One in vitro study on fungal biofilm has shown C.albicans producing quantitatively more biofilm than Candida parapsilosis, Candida glabrata and C. tropicalis. These films have rapidly developed resistance to fluconazole.11
The optimal time to reimplantation has been debated.3 Hwang et al. have performed reimplantation at an average of 9.5 weeks.1 It has been recommended that in cases of PJI with unusual or virulent organisms, the period between resection and reimplantation should be prolonged.3 After keeping patient on an extended course of antifungal therapy in consultation with infectious disease specialist, we performed a delayed reimplantation at 20 weeks. We ensured that the ESR, CRP was normalized; repeat aspiration was negative prior to reimplantation surgery.
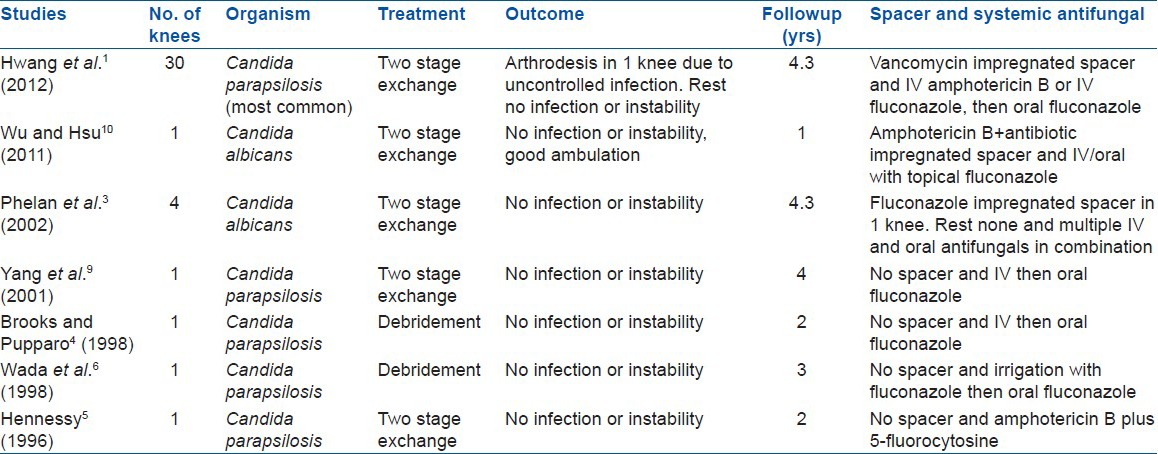
The choice and duration of antifungal therapy also remains controversial. Amphotericin B is the gold standard, but is nephrotoxic and may not be useful for long term administration.3,10 Fluconazole has demonstrated fewer side effects and can be used long term in patients. Successful treatment with fluconazole as the sole antifungal agent has been reported.3,6,7 A high bio-availability, extended half-life, absence of serious side effect and high concentration in joint fluid make fluconazole an excellent choice.10 Our choice was fluconazole for the above mentioned reasons. We followed the recommendations of Infectious Disease Society of America and gave fluconazole in a combination of parenteral and oral formulation for a total period of 30 weeks [Table 1].1,2,3,7,10
Table 1.
Literature review
The cement spacer was loaded with Amphotericin B, based on previous literature, for local action, but we do not have any analysis of the elution rate or the concentration it achieved in the joint. At present, there is no consensus on the type, dose or efficacy of antifungal used in cement spacers.1,2,3,10 Further research is required in this area.
To conclude based on our experience and review of literature, we say that fungal PJI, though rare, is a serious complication and is more difficult to manage than bacterial PJI. Protocols for diagnosis and management need to be established. Resection arthroplasty with antifungal therapy followed by delayed reimplantation offers the best possible result. Despite this, further modalities of treatment including options during 1st stage of revision TKA, the choice and total duration of antifungal therapy and time of reimplantation should be explored.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Hwang BH, Yoon JY, Nam CH, Jung KA, Lee SC, Han CD, et al. Fungal peri-prosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br. 2012;94:656–9. doi: 10.1302/0301-620X.94B5.28125. [DOI] [PubMed] [Google Scholar]
- 2.Azzam K, Parvizi J, Jungkind D, Hanssen A, Fehring T, Springer B, et al. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: A multi-institutional experience. J Bone Joint Surg Am. 2009;91(Suppl 6):142–9. doi: 10.2106/JBJS.I.00574. [DOI] [PubMed] [Google Scholar]
- 3.Phelan DM, Osmon DR, Keating MR, Hanssen AD. Delayed reimplantation arthroplasty for candidal prosthetic joint infection: A report of 4 cases and review of the literature. Clin Infect Dis. 2002;34:930–8. doi: 10.1086/339212. [DOI] [PubMed] [Google Scholar]
- 4.Brooks DH, Pupparo F. Successful salvage of a primary total knee arthroplasty infected with Candida parapsilosis. J Arthroplasty. 1998;13:707–12. doi: 10.1016/s0883-5403(98)80017-x. [DOI] [PubMed] [Google Scholar]
- 5.Hennessy MJ. Infection of a total knee arthroplasty by Candida parapsilosis. A case report of successful treatment by joint reimplantation with a literature review. Am J Knee Surg. 1996;9:133–6. [PubMed] [Google Scholar]
- 6.Wada M, Baba H, Imura S. Prosthetic knee Candida parapsilosis infection. J Arthroplasty. 1998;13:479–82. doi: 10.1016/s0883-5403(98)90019-5. [DOI] [PubMed] [Google Scholar]
- 7.Fukasawa N, Shirakura K. Candida arthritis after total knee arthroplasty – A case of successful treatment without prosthesis removal. Acta Orthop Scand. 1997;68:306–7. doi: 10.3109/17453679708996709. [DOI] [PubMed] [Google Scholar]
- 8.Simonian PT, Brause BD, Wickiewicz TL. Candida infection after total knee arthroplasty. Management without resection or amphotericin B. J Arthroplasty. 1997;12:825–9. doi: 10.1016/s0883-5403(97)90015-2. [DOI] [PubMed] [Google Scholar]
- 9.Yang SH, Pao JL, Hang YS. Staged reimplantation of total knee arthroplasty after Candida infection. J Arthroplasty. 2001;16:529–32. doi: 10.1054/arth.2001.21458. [DOI] [PubMed] [Google Scholar]
- 10.Wu MH, Hsu KY. Candidal arthritis in revision knee arthroplasty successfully treated with sequential parenteral-oral fluconazole and amphotericin B-loaded cement spacer. Knee Surg Sports Traumatol Arthrosc. 2011;19:273–6. doi: 10.1007/s00167-010-1211-4. [DOI] [PubMed] [Google Scholar]
- 11.Kuhn DM, Chandra J, Mukherjee PK, Ghannoum MA. Comparison of biofilms formed by Candida albicans and Candida parapsilosis on bioprosthetic surfaces. Infect Immun. 2002;70:878–88. doi: 10.1128/iai.70.2.878-888.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]


