Summary
Falls are frequent in the elderly and affect mortality, morbidity, loss of functional capacity and institutionalization. In the older patient the incidence of falls can sometimes be underestimated, even in the absence of a clear cognitive impairment, because it is often difficult to reconstruct the dynamics. It is quite common that forms due to syncope are associated with retrograde amnesia and in 40 to 60% of the cases falls happen in the absence of witnesses. The pathogenesis of falls is often multifactorial, due to physiological age-related changes or more properly pathological factors, or due to the environment. The identification of risk factors is essential in the planning of preventive measures. Syncope is one of major causes of falls. About 20% of cardiovascular syncope in patients older than 70 appears as a fall and more than 20% of older people with Carotid Sinus Syndrome complain of falls as well as syncope. These data clearly state that older patients with history of falls should undergo a cardiovascular and neuroautonomic assessment besides the survey of other risk factors. Multifactorial assessment requires a synergy of various specialists. The geriatrician coordinates the multidisciplinary intervention in order to make the most effective evaluation of the risk of falling, searching for all predisposing factors, aiming towards a program of prevention. In clear pathological conditions it is possible to enact a specific treatment. Particular attention must indeed be paid to the re-evaluation of drug therapy, with dose adjustments or withdrawal especially for antihypertensive, diuretics and benzodiazepines. The Guidelines of the American Geriatrics Society recommend modification of environmental hazards, training paths, hip protectors and appropriate use of support tools (sticks, walkers), which can be effective elements of a multifactorial intervention program. Balance exercises are also recommended. In conclusion, an initial assessment, supported by a comprehensive cardiovascular and neuroautonomic evaluation, allows for reaching a final diagnosis in most cases, demonstrating a key role in the real identification of the etiology of the fall and implementing the treatment measures.
Keywords: falls, elderly, multifactorial assessment, prevention strategies
Definition
Falls are defined as accidental events in which a person falls when his/her centre of gravity is lost and no effort is made to restore balance or this effort is ineffective; the underlying mechanism could be a seizure, a stroke, a loss of consciousness or non contestable forces (1).
Only few studies consider the transient loss of consciousness as a possible cause of fall (2, 3), defining this last as “an accidental movement toward the floor with or without loss of consciousness or injury”. Although falls are frequent in the elderly and affect mortality, morbidity, loss of functional capacity and institutionalization (4), they have not always been identified as a public health problem, indeed before the 40s they were considered unpredictable events and still many older people do not consult a doctor about them. During the last 20 years there has been instead growing interest in the field of falls in the elderly and several studies have demonstrated the incidence, the consequences, the multifactorial etiology of falls and the possible intervention on risk factors through a multi-disciplinary approach (5). However, the prevention of falls is still not sufficiently implemented outside purely geriatric contexts, which is why falls still remain a relevant health problem.
Epidemiology and consequences
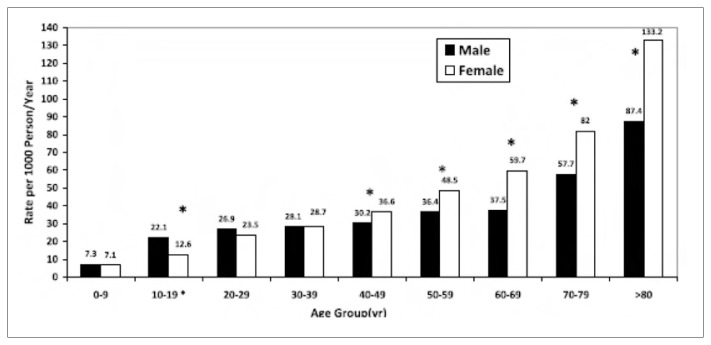
In the older patient the incidence of falls can sometimes be underestimated, even in the absence of a clear cognitive impairment, because it is often difficult to reconstruct the dynamics. It is quite common that forms due to syncope are associated with retrograde amnesia (6) and in 40 to 60% of the cases falls happen in the absence of witnesses. It is estimated that 34% of patients ≥ 65 years old, 50% of non-institutionalized octogenarians, 26% of inpatients and 43% of patients in nursing homes, experience at least one fall a year (7). The prevalence increases with the age (Figure 1); in the United States women older than 70 years of age are more predisposed to fall and have a double rate of injury compared to same aged men (4). The incidence of falls in patients older than 65 in nursing homes and in hospitals is about three times higher compared to falls in community-dwelling persons (on average 1.5 per bed per year), probably due to the inherent fragility of this population and to the better control in such environments.
Figure 1.
The prevalence of fall according to the increasing of age (4).
The annual incidence of falls in community-dwelling patients older than 65 is around 28–35% and reaches 40% in ≥ 75 years old (8). 8–10% of the admissions to the Emergency Department every year concern fall-related traumas; falls are also responsible for 56% of the hospitalization for trauma and for 6% of urgent hospitalization in patients older than 65 years of age (5). 5–10% of the older patients have fractures, concussions, injuries with a growing risk of hospitalization (9). In about 1% of the patients with falls, a femur fracture occurs with a 20–30% one-year mortality and negative impact on functional capacity (10).
In 30–70% of the cases a depressive syndrome occurs, due to the fear of a new onset fall, with consequent disability and institutionalization. Furthermore, in the elderly there is a strict relationship between high incidence of falls and high damage susceptibility, due to age-related changes and co-morbidity, in particular osteoporosis. This considerably increments the risk of fractures, pneumonia, dehydration and rhabdomyolysis as consequences of immobilization and the inability to get up from the ground.
Etiology
The pathogenesis of falls is often multifactorial due to physiological age-related changes (Table 1) or more properly pathological factors (Table 2), or due to the environment. The identification of risk factors is essential in the planning of preventive measures (11). Ambulatory problems and muscle weakness are responsible for 10–25% of the falls (12). An extensive longitudinal study showed indeed that 10% of the people over 65 need assistance in walking across a room, 20% need help in climbing stairs and 40% are unable to walk more than 500 meters (8). Muscle weakness is quite common in the elderly and some studies have shown the prevalence of weakness of the lower limbs in 48% of non-institutionalized patients (12) and in 80% of patients in nursing homes (13). Case-control studies showed that patients with falls have more problems in walking than those without a history of falls (14). Although the reduction of muscle strength is part of the physiological aging process, much of this reduction is probably attributable to the presence of co-morbidity and to physical inactivity. It has recently been documented that distal muscle weakness leads to significant postural instability and that the proximal muscle weakness reduces the compensatory movement of the arms (15).
Table 1.
Age-related physiological changes (11).
| Sight | Reduction of: ability to accommodate, visual acuity, tolerance to glare, discriminative capacity for colors. |
| Hearing | Reduced discrimination capability between contemporary voices in conversation; reduced perception of pure tones, increased production of earwax with frequent development of caps. |
| Locomotor | Sarcopenia, reduced muscle strength, reduced range of motion. |
Table 2.
Falls predisposing pathologic conditions (11).
Neurologic
|
Musculoskeletal
|
Cardiovascular
|
Genitourinary
|
Gastrointestinal
|
Psychiatric
|
Endocrine and internal medicine
|
Iatrogenic
|
Environmental barriers are responsible for 30–50% of the falls, even though falls are often determined by interaction within the environment or dangerous activities and increased individual susceptibility. The external environment contains many risks, but above all older people fall at home, maybe because they spend most of their time there and, feeling more confident, are more careless (16). At home, barriers are represented by thresholds, stairs, carpets, slippery surfaces. Inadequate lighting or, on the contrary, excessive or dazzling illumination, are possible causes, too.
In institutionalized patients most of the falls occurs during activities with inherent risk because of the postural changes and the vasovagal reflexes involved, for example getting out of bed, getting into or out of the bath (17, 1). In urban areas barriers are represented by sidewalks, unprotected crossing, etc. A meta-analysis investigated the relationship between falls and drugs: taking more than 4 drugs determined a significant rise in the risk of falling, especially as regards antiarrhythmic, digoxin, diuretics, antidepressants, benzodiazepines, antipsychotics. Benzodiazepines are one of the main fall risk factors both in acute and in chronic use (19).
In the evaluation process it is particularly important to consider the interaction and the synergism between multiple causes of falls, the etiology is indeed multifactorial (20). It has also been demonstrated that the greater the number of risk factors, the greater the risk of falling; the proportion of community-dwelling patients with recurrent falls increases from 10% to 69% when the number of risk factors increases from 1 to 4 or more (16).
Evaluation
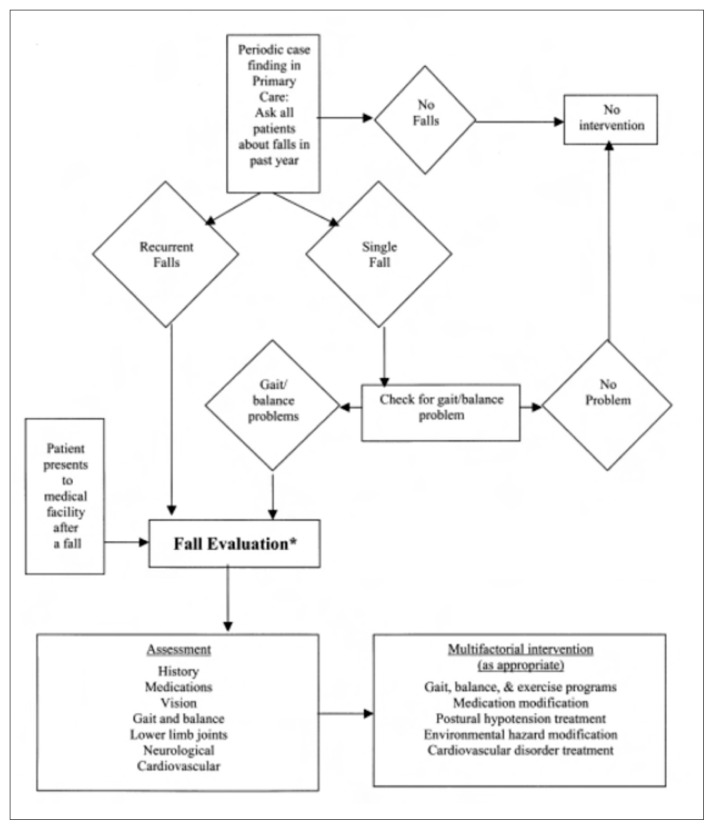
The Guidelines for the prevention of falls in older persons, of the American Geriatrics Society proposes a specific diagnostic algorithm (Figure 2) (20).
Figure 2.
Diagnostic algorithm in patient with falls (20).
Multifactorial assessment requires a synergy of various specialists (geriatricians, physiotherapists, social workers, orthopedists). The geriatrician coordinates the multidisciplinary intervention in order to make the most effective evaluation of the risk of falling, searching for all predisposing factors –medical, social and environmental – aiming towards a program of prevention (1).
Prevention strategies
In clear pathological conditions it is possible to enact a specific treatment, for example, the administration of antiarrhythmic drugs or pacemaker implantation in case of cardiac arrhythmia, clearly related to falling. Hypovolaemia or dehydration require fluid administration to restore the hemodynamic balance. Treatment of orthostatic hypotension or autonomic disorders involves behavioral maneuvers or, if ineffective, medication such as midodrine, that has proved to be more effective than epinephrine and could be considered the first choice, although its effectiveness is conditioned by the use of full and refracted doses. Ephedrine and pseudoephedrine have beta1-and beta2-stimulating action, which solves the vasoconstrictor effect. In those patients in which the administration of fluids and sodium have failed, a good therapeutic option is 9-alpha-fluoro-hydrocortisone, provided through an adequate dosage and not through daily assumption. There are also “additional” drugs, used in the absence of response to any previous maneuvers. The use of desmopressin is linked to the fact that in case of autonomic failure, there is a reduced release of vasopressin, caused by hypothalamus suprachiasmatic nucleus degeneration. Other pharmacologically active molecules are: inhibitors of cyclo-oxygenase, beta-adrenergic agonist, clonidine, yohimbine, somatostatin, dihydroergotamine and dopamine agonists (21).
Particular attention must be paid to the re-evaluation of drug therapy, with dose adjustments or withdrawal especially for antihypertensive, diuretics and benzodiazepines. The Guidelines of the American Geriatrics Society (20) recommend modification of environmental hazards, training paths, hip protectors and appropriate use of support tools (sticks, walkers), which can be effective elements of a multifactorial intervention program; however, their isolated use, without adequate attention towards other risk factors, cannot be recommended.
Balance exercises are also recommended. Although physical exercise has shown proven benefits, the optimal type, duration and intensity necessary to prevent falls remains unclear (8). A South Korean research has shown that Tai Chi can be effective in improving balance and therefore in preventing falls in the elderly (22).
Overlapping between syncope and falls
Syncope is one of major causes of falls; the low percentage of syncope-related falls (0.3–5%) (7) is probably an underestimation because many clinical trials exclude patients with this diagnosis. Even in those studies in which it is not explicitly excluded, the relevance of syncope in patients with history of falls is still underestimated, because these have a significantly higher probability of being hospitalized immediately and not being included in the study. It is also difficult to obtain the description of a syncope rather than most of the other causes of falls, because many patients present retrograde amnesia for the loss of consciousness (23) and because 40–60% of the syncopal episodes happen without witnesses. Even pre-syncope, that occurs in case of transient arrhythmias or orthostatic hypotension, could be a cause of fall and predicts the occurrence of a future syncopal episode. 26% of older patients referred to the Emergency Department had a syncope-related fall (24).
Syncope in the elderly is associated with a high risk of trauma; syncope-related fractures or major trauma range from 10 to 23%. The risk of a major trauma is 5.9 times higher for syncope-related falls and has also been associated with a higher risk of remaining on the ground for a longer time, compared to non-syncopal falls (16).
Older inpatients with syncope have a 13–33% one-year mortality (7) and 79% four-year mortality, compared to the expected value, also negatively influenced by age and co-morbidities.
About 20% of cardiovascular syncope in patients older than 70 appears as a fall, especially in the case of carotid-sinus syndrome (CSS) and orthostatic hypotension; more than 20% of older people with CSS complain of falls as well as syncope (25). Kenny analyzed patients older than 60 who were referred to the hospital for a fall or a syncope. Those with falls, who showed a CSS when subjected to Carotid Sinus Massage (CSM), showed retrograde amnesia for the loss of consciousness more frequently than patients with syncope (23).
In a large group of patients referred to the Emergency Department, 39% had had an accidental fall, 26% had had a fall strictly related to a clinical condition, 16% had dementia and 14% had had an unexplained fall. In this last group of patients, 34% had carotid sinus hypersensitivity, cardio-inhibitory type in 50% of the cases and the rate of fall and trauma respectively was reduced by 70 to 75% after a pacemaker implantation (26). These data clearly state that older patients with history of falls should undergo a cardiovascular and neuroautonomic assessment besides the survey of other risk factors. Tilt Testing (TT) and CSM are useful in confirming the hypothesis of a reflex syncope as a potential cause of unexplained falls and TT positivity tends to increase exponentially with age (27, 28). The evaluation of elderly patients with recurrent falls should also exclude atrial fibrillation, given the increasing prevalence of this condition with age (11), especially when patients report palpitation as a prodromal symptom, suggesting an arrhythmic etiology. The age-related changes in structure and cardiovascular function, especially the diastolic dysfunction, not only predispose to the development of atrial fibrillation, but may also reduce the hemodynamic tolerance to such arrhythmia, increasing the risk of syncope or fall.
In common clinical practice, the patient with a traumatic fall is defined under a general point of view and the cause of the fall is often under-investigated, being only limited to the treatment of consequences and ignoring the search for possible pathogenetic mechanisms. On the contrary, an initial assessment, supported by a comprehensive cardiovascular and neuroautonomic evaluation, allows for reaching a final diagnosis in most cases, demonstrating a key role in the real identification of the etiology of the fall. It is thus possible to implement treatment measures aimed at reducing disability, institutionalization, mortality and increased health care costs.
References
- 1.King MB. Falls. Principles of geriatric medicine and gerontology. 2003 [Google Scholar]
- 2.Rubenstein LZ, Robbins AS, Josephson KR, Schulman BL, Osterweil D. The value of assessing falls in an elderly population. A randomized clinical trial. Ann Intern Med. 1990;113:308–316. doi: 10.7326/0003-4819-113-4-308. [DOI] [PubMed] [Google Scholar]
- 3.McIntosh S, Da Costa D, Kenny RA. Outcome of an integrated approach to the investigation of dizziness, falls and syncope in elderly patients referred to a ‘syncope’ clinic. Age Ageing. 1993;22:53–58. doi: 10.1093/ageing/22.1.53. [DOI] [PubMed] [Google Scholar]
- 4.Gangadhar Malasana MD, Brignole M, Marcos Daccarett MD, Sherwood Randall, Hamdan Mohamed H. The Prevalence and Cost of the Faint and Fall problem in the State of Utah. PACE. 2011;34:278–283. doi: 10.1111/j.1540-8159.2010.02930.x. [DOI] [PubMed] [Google Scholar]
- 5.Tinetti ME. Preventing falls in elderly persons. N Engl J Med. 2003;348:41–9. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 6.Cummings RS, Nevit MC, Kidd S. Forgetting falls, the limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:613–6. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- 7.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 8.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 10.Marottoli RA, Berkman LF, Cooney LM. Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;40:861–6. doi: 10.1111/j.1532-5415.1992.tb01980.x. [DOI] [PubMed] [Google Scholar]
- 11.Mayor S. NICE issues guideline to prevent falls in elderly people. BMJ. 2004;329(7477):1258. doi: 10.1136/bmj.329.7477.1258-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44:M112–M117. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 13.Robbins AS, Rubenstein LZ, Josephson KR, Schulman BL, Osterweil D, Fine G. Predictors of falls among elderly people. Results of two population-based studies. Arch Intern Med. 1989;149:1628–1633. [PubMed] [Google Scholar]
- 14.Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on the number of chronic disabilities. Am J Med. 1986;80:429–434. doi: 10.1016/0002-9343(86)90717-5. [DOI] [PubMed] [Google Scholar]
- 15.Horlings CG, Kung UM, van Engelen BG, Voermans NC, Hengstman GJ, van der Kooi AJ, Bloem BM, Allum JH. Balance control in patients with distal versus proximal muscle weakness. Neuroscience. 2009 doi: 10.1016/j.neuroscience.2009.09.063. [DOI] [PubMed] [Google Scholar]
- 16.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent non-syncopal falls. A prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 17.Berry G, Fisher RH, Lang S. Detrimental incidents, including falls, in an elderly institutional population. J Am Geriatr Soc. 1981;29:322–324. doi: 10.1111/j.1532-5415.1981.tb01273.x. [DOI] [PubMed] [Google Scholar]
- 18.Kalchthaler T, Bascon RA, Quintos V. Falls in the institutionalized elderly. J Am Geriatr Soc. 1978;26:424–428. doi: 10.1111/j.1532-5415.1978.tb05391.x. [DOI] [PubMed] [Google Scholar]
- 19.Hartikainen S, Lonnroon E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol. 2007;62A:1172–81. doi: 10.1093/gerona/62.10.1172. [DOI] [PubMed] [Google Scholar]
- 20.American geriatrics society, British geriatrics society, American academy of orthopaedic surgeons Panel on Falls Prevention. Guideline for the Prevention of Falls in Older Persons. J Am Geriatr Soc. 2001 [PubMed] [Google Scholar]
- 21.Freeman R. Neurogenic orthostatic hypotension. N Eng J Med. 2008;358:615–24. doi: 10.1056/NEJMcp074189. [DOI] [PubMed] [Google Scholar]
- 22.Faber MJ, Bosscher RJ, Chin APM, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87:885–896. doi: 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Parry SW, Steen IN, Baptist M, Kenny RA. Amnesia for loss of consciousness in carotid sinus syndrome: implications for presentation with falls. J Am Coll Cardiol. 2005;45:1840–1843. doi: 10.1016/j.jacc.2005.02.060. [DOI] [PubMed] [Google Scholar]
- 24.Davies AJ, Kenny RA. Falls presenting to the accident and emergency department: types of presentation and risk factor profile. Age Ageing. 1996;25:362–366. doi: 10.1093/ageing/25.5.362. [DOI] [PubMed] [Google Scholar]
- 25.Carey BJ, Potter JF. Cardiovascular causes of falls. Age Ageing. 2001;30( Suppl 4):19–24. doi: 10.1093/ageing/30.suppl_4.19. [DOI] [PubMed] [Google Scholar]
- 26.Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE, Bond J. Carotid sinus syndrome: a modifiable risk factor for nonaccidental falls in older adults (SAFE PACE) J Am Coll Cardiol. 2001;38:1491–1496. doi: 10.1016/s0735-1097(01)01537-6. [DOI] [PubMed] [Google Scholar]
- 27.Paling David, Vilches-Moraga Arturo, Akram Quasim, Atkinson Oliver, Staniland John, Paredes-Galan Emilio. Carotid sinus syndrome is common in very elderly patients undergoing tilt table testing and carotid sinus massage because of syncope or unexplained falls. Aging Clinical and Experimental Research. 23(4) doi: 10.1007/BF03324968. [DOI] [PubMed] [Google Scholar]
- 28.Anpalahan Mahesan, Gibson Stephen. The prevalence of Neurally Syncope in older patients presenting with unexplained falls. European Journal of internal Medicine. 2012:e48–e52. doi: 10.1016/j.ejim.2011.10.010. [DOI] [PubMed] [Google Scholar]