Abstract
Background
Survivorship care plans (SCPs), including a treatment summary and follow-up plan, intend to promote coordination of posttreatment cancer care; yet, little is known about the provision of these documents by oncologists to primary care physicians (PCPs). This study compared self-reported oncologist provision and PCP receipt of treatment summaries and follow-up plans, characterized oncologists who reported consistent provision of these documents to PCPs, and examined associations between PCP receipt of these documents and survivorship care.
Methods
A nationally representative sample of medical oncologists (n = 1130) and PCPs (n = 1020) were surveyed regarding follow-up care for breast and colon cancer survivors. All statistical tests were two-sided. Multivariable regression models identified factors associated with oncologist provision of treatment summaries and SCPs to PCPs (always/almost always vs less frequent).
Results
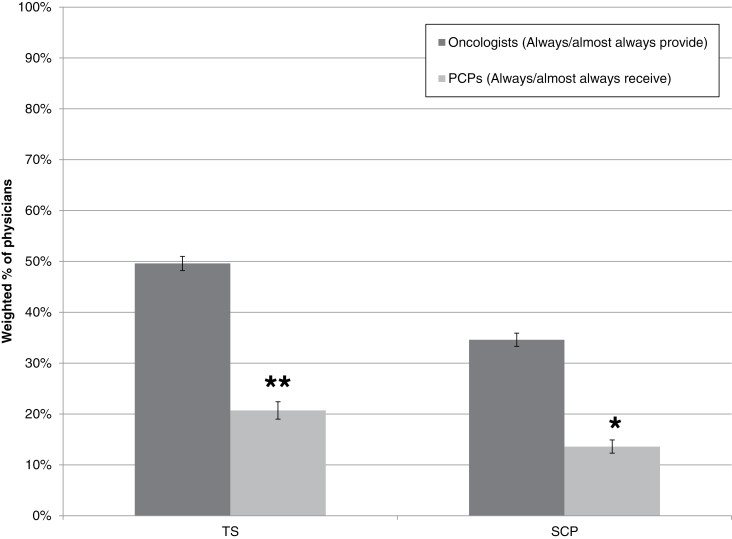
Nearly half of oncologists reported always/almost always providing treatment summaries, whereas 20.2% reported always/almost always providing SCPs (treatment summary + follow-up plan). Approximately one-third of PCPs indicated always/almost always receiving treatment summaries; 13.4% reported always/almost always receiving SCPs. Oncologists who reported training in late- and long-term effects of cancer and use of electronic medical records were more likely to report SCP provision (P < .05). PCP receipt of SCPs was associated with better PCP-reported care coordination, physician–physician communication, and confidence in survivorship care knowledge compared to receipt of neither treatment summaries nor SCPs (P < .05).
Conclusions
Providing SCPs to PCPs may enhance survivorship care coordination, physician–physician communication, and PCP confidence. However, considerable progress will be necessary to achieve implementation of sharing SCPs among oncologists and PCPs.
The number of cancer survivors in the United States continues to grow (1) and is currently estimated at nearly 14 million (2). Survivorship is often accompanied by physical and psychosocial sequelae and ongoing cancer surveillance needs. Both necessitate comprehensive follow-up care (3). Currently in the United States, follow-up care involves multiple providers, including oncologists and primary care physicians (PCPs). There is no clear delineation of survivorship care responsibilities, and providers may have inadequate training regarding survivors’ needs and limited communication with each other (4–8). A growing body of literature highlights challenges in meeting the complex needs of survivors (3,9) and the relationships between care coordination, physician–physician communication, and quality of follow-up care (10,11).
The Institute of Medicine (IOM) recommended that oncologists provide all patients completing primary cancer treatment with a comprehensive treatment summary (TS) and an individualized follow-up plan, which together are referred to as a survivorship care plan (SCP). The purpose of the SCP is to promote care coordination, physician–physician communication, PCP knowledge regarding survivorship care (3,12), and survivor education about future healthcare needs. The American Society of Clinical Oncology describes the follow-up plan as a desirable (but optional) addition to the TS (12). However, the utility of an SCP (TS plus follow-up plan) compared to that of a TS alone has not yet been empirically tested. Nonetheless, in 2015, the American College of Surgeons Commission on Cancer will require institutions seeking accreditation to provide SCPs to survivors (13).
One way the goals of SCPs can be achieved is through sharing of care plans between providers. However, data are limited regarding the prevalence of SCP sharing between oncologists and PCPs (14). The only published efficacy study on SCPs to date focuses on patient experiences, not those of providers (15). Little is known about the factors that facilitate or hinder sharing of SCPs among providers.
This study explores the sharing of SCPs among oncologists and PCPs based on a nationally representative survey of practicing physicians. We compared oncologist and PCP-reported provision/receipt of TSs and SCPs (combined TS and care plan); characterized oncologists who report consistently providing TSs and SCPs to PCPs; and examined associations between PCP-reported receipt of TSs or SCPs and PCP-perceived indicators of care coordination, physician–physician communication, and confidence in knowledge about survivorship care.
Methods
Sample and Data Collection
The Survey of Physician Attitudes Regarding the Care of Cancer Survivors (SPARCCS) assessed physician-reported practices and attitudes regarding posttreatment follow-up care of early-stage breast and colon cancer survivors (http://healthservices.cancer.gov/surveys/sparccs/; for methods, see Potosky et al (7)). SPARCCS focused on these cancers due to the high prevalence of survivors and their long survivorship periods (7). Study approval was obtained from the National Cancer Institute’s Institutional Review Board and the US Office of Management and Budget. Questionnaires were mailed in 2009 to a nationally representative sample of medical oncologists and PCPs generated from the American Medical Association Physician MasterFile using stratified sampling to achieve even representation across specialties, census region, metropolitan statistical area, age, sex, and “mail undeliverable” status. Consent was implied by returned questionnaire.
The SPARCCS sample consisted of 1130 oncologists and 1072 PCPs (overall weighted response rate = 57.7%). Nonrespondents and respondents were similar on all variables examined (age, sex, board certification status, specialty, region, and US vs foreign training). The current analytic sample excluded PCPs who reported having never seen a breast or colon cancer survivor in clinical practice (n = 51) and who self-reported practicing outside of primary care (n = 1). Excluded PCPs were more likely to be male, nonwhite, not board certified, from the south or west census region, and foreign trained (P < .05).
Measures
Most survey items were adapted from previous physician surveys (11,16–19). The items assessing confidence in knowledge, training in late and long-term effects, and preferred model of follow-up care were developed by SPARCCS investigators (7).
Provision/receipt of TSs and SCPs.
Oncologists reported how often they provide the following to the PCPs of breast and colon cancer survivors using a five-point Likert scale (never, rarely, sometimes, often, always/almost always) (19): a comprehensive summary including detailed cancer treatment information (TS), and an explicit follow-up plan documenting recommendations for future care and surveillance. Because recommendations suggest every survivor should receive an SCP (20), an “always/almost always” response for TSs constituted provision of TSs. An “always/almost always” response for both TSs and follow-up plans constituted provision of SCPs. PCP-reported receipt of TSs and SCPs was assessed using analogous questions and operational definitions.
We assessed PCP perceptions of seven aspects of survivorship care, organized into three domains: care coordination, physician– physician communication, and confidence in survivorship care knowledge (Table 1).
Table 1.
Survivorship care domains assessed among primary care physicians (PCPs)
| Survivorship care domain | Components of care | Operational definition |
|---|---|---|
| Care coordination (two items) | “How often do you …” | Never vs more frequently |
| Experience uncertainty about which physician (oncology specialist or PCP) is providing patients’ general preventive health care | ||
| Encounter difficulties transferring patient care responsibilities between you and the oncology specialist | ||
| Physician–physician communication (two items) | “How often do you routinely communicate with your patients’ other physician(s) about which physician will …” | Always vs less frequently |
| Follow them for their cancer | ||
| Handle other medical issues | ||
| Confidence in knowledge regarding survivorship care (three items) | “How confident do you feel about your knowledge of …” | Very confident vs less confident |
| Appropriate surveillance testing to detect recurrent cancer | ||
| Long-term and late physical adverse effects of cancer and cancer treatment | ||
| Potential adverse psychosocial outcomes of cancer or its treatment |
Care coordination.
PCPs reported the frequency with which they encounter two problems related to care coordination on a five-point Likert scale (“never” to “always/almost always”): uncertainty about which physician (oncologist or PCP) is providing patients’ general preventative health care, and difficulties transferring patient care responsibilities between themselves and the oncologist (21). For each item, one 2-level variable was created: “never” vs “more frequently.”
Physician–physician communication.
PCPs reported the fre quency with which they communicated with their patients’ other physician(s) regarding which physician would 1) provide cancer-related follow-up care and 2) handle other medical issues. Responses were reported on a five-point Likert scale (“never” to “always/almost always”) (18). For each item, a two-level variable was created: “always” vs “less than always.”
Confidence in survivorship care knowledge.
PCPs reported their degree of confidence regarding their knowledge of three areas for breast and colon cancer: surveillance testing to detect recurrent cancer, long-term and late physical adverse effects of cancer and cancer treatment, and potential adverse psychosocial outcomes of cancer or its treatment (7). For each item, a two-level variable was created, “very confident” vs “less confident.”
Physician demographic and practice characteristics.
Physicians indicated their race/ethnicity, percentage of time spent in patient care, number of patients seen per week, number of patients ever diagnosed with breast or colon cancer seen per week (oncologists) or per year (PCPs), percentage of patients uninsured/insured by Medicaid, practice size (number of physicians), medical record system (paper medical records vs electronic), and productivity-based salary (11,17). Age, sex, specialty, census region, and metropolitan statistical area were obtained from the American Medical Association MasterFile.
Training in late- and long-term effects of cancer.
Physicians reported receipt of training regarding the late and long-term effects of cancer (no; yes, somewhat; or yes, in detail).
Preferred model of follow-up care.
Physicians indicated their preferred model of survivorship care: primary responsibility assigned to oncologists, to PCPs, to specialized survivorship clinics, or shared responsibility between oncologists and PCPs (18). Responses were recoded according to the respondent’s preferred role: primary responsibility, shared responsibility, or someone else has responsibility.
Statistical Analysis
SAS (version 9.2) survey procedures were used to incorporate sampling weights into analyses. Estimates represent the entire population of practicing medical oncologists and PCPs and account for survey design and nonresponse (22). All tests were two-sided. The χ2 test evaluated differences between the proportion of oncologists reporting they always/almost always provide TSs and SCPs and the proportion of PCPs reporting they always/almost always receive these documents.
Multiple logistic regression was used to identify factors uniquely associated with oncologist-reported provision of 1) TSs and 2) SCPs to PCPs, based on a set of factors expected to be associated with care practices (demographics, practice characteristics, preferred model of survivorship care). To balance parsimony and inclusiveness, variables were included in the adjusted model if they were associated with provision of TSs or SCPs in bivariate tests (P < .2). Next, we examined PCP perceptions of seven components of survivorship care within three overarching domains (care coordination, physician–physician communication, and confidence in knowledge regarding survivorship care; Table 1). The proportion of PCPs reporting desired outcomes for each component of survivorship care were calculated from a multiple regression model adjusting for PCP age and number of breast/colon cancer survivors seen per year. Adjusted logistic regression models regressed each of seven care components on receipt of TSs and SCPs in two ways: 1) with receipt of neither document as the reference group (TS alone vs neither and SCP vs neither), and 2) with receipt of TS alone as the reference group (SCP vs TS alone). Multivariable models included a reduced number of participants due to missing data for some variables. Respondents excluded due to missing data were similar to those with complete data except that excluded oncologists were younger, and excluded PCPs were older, than included oncologists and PCPs (P < .05).
Results
Oncologists were more likely than PCPs to be male, to be Asian, to prefer primary responsibility for cancer follow-up, and to have received detailed training in late and long-term effects (Table 2). PCPs spent a greater proportion of their time in patient care, were more likely to report paper vs electronic medical records in their practices, and were more likely to have a solo practice (all P < .05). Oncologists saw, on average, 35 breast or colon cancer survivors per week, whereas PCPs saw approximately 38 breast or colon cancer survivors per year.
Table 2.
Characteristics of physician respondents*
| Characteristic | Oncologists (n = 1130) | PCPs (n = 1020) | Oncologists vs PCPs | ||
|---|---|---|---|---|---|
| Mean (95% CI) | Median (Range) | Mean (95% CI) | Median (Range) | P | |
| Age, y | 47.2 (46.7 to 47.6) | 47 (47) | 48.3 (47.7 to 48.9) | 48 (47) | .0033 |
| Percentage of time spent in patient care | 82.1 (80.9 to 83.4) | 90 (80) | 88.7 (87.8 to 89.5) | 94 (80) | <.0001 |
| No. | Weighted % | No. | Weighted % | P | |
| Specialty | –† | ||||
| Medical oncology | 553 | 47.8 | — | — | |
| Hematology/oncology | 566 | 51.3 | — | — | |
| General internal medicine | — | — | 480 | 37.8 | |
| Family medicine | — | — | 458 | 43.4 | |
| Obstetrics–gynecology | — | — | 82 | 18.7 | |
| Other | 11‡ | 1.0 | — | — | |
| Sex | <.0001 | ||||
| Male | 837 | 72.9 | 679 | 64.2 | |
| Female | 293 | 27.1 | 341 | 35.8 | |
| Race/ethnicity | <.0001 | ||||
| Non-Hispanic white | 726 | 62.7 | 710 | 70.7 | |
| Hispanic white | 36 | 3.2 | 37 | 4.1 | |
| Non-Hispanic black | 25 | 2.2 | 46 | 4.9 | |
| Asian | 299 | 28.2 | 174 | 15.1 | |
| Other/multiple | 13 | 1.1 | 11 | 1.1 | |
| Metropolitan statistical area (MSA) | .012 | ||||
| MSA population ≥1 million | 728 | 65.6 | 622 | 61.5 | |
| All other MSAs | 402 | 34.4 | 398 | 38.5 | |
| Breast and colon cancer patients seen per week, no. | –† | ||||
| 0–21 | 358 | 32.7 | — | — | |
| 22–39 | 362 | 31.5 | — | — | |
| ≥40 | 404 | 35.2 | — | — | |
| Breast and colon cancer patients seen per year, no. | –† | ||||
| 0–14 | — | — | 309 | 31.5 | |
| 15–34 | — | — | 327 | 32.5 | |
| ≥35 | — | — | 354 | 33.2 | |
| Patient load | <.0001 | ||||
| ≤50 patients/week | 320 | 28.9 | 140 | 13.6 | |
| 51–100 patients/week | 606 | 53.4 | 540 | 53.0 | |
| ≥101 patients/week | 193 | 16.4 | 321 | 31.8 | |
| Percentage of patients uninsured or insured by Medicaid | <.0001 | ||||
| ≤5 | 101 | 8.7 | 165 | 17.1 | |
| 6–10 | 260 | 22.3 | 217 | 19.9 | |
| 11–20 | 361 | 31.8 | 312 | 30.9 | |
| ≥21 | 338 | 30.0 | 294 | 29.3 | |
| Salary based on productivity | .34 | ||||
| Yes | 387 | 34.0 | 355 | 33.5 | |
| No | 666 | 59.2 | 635 | 63.7 | |
| Practice size (physicians), no. | <.0001 | ||||
| 1 | 122 | 10.1 | 253 | 24.1 | |
| 2–5 | 436 | 39.2 | 422 | 42.8 | |
| 6–15 | 339 | 29.6 | 223 | 21.9 | |
| ≥16 | 212 | 19.2 | 103 | 9.5 | |
| Medical record system | <.0001 | ||||
| Paper records | 247 | 21.7 | 388 | 40.0 | |
| Partial electronic records or in transition to electronic records | 498 | 43.6 | 288 | 27.8 | |
| Full electronic medical records | 375 | 33.4 | 327 | 30.7 | |
| Received training regarding late or long-term effects of cancer treatment | <.0001 | ||||
| No | 83 | 7.1 | 329 | 34.3 | |
| Yes, somewhat | 637 | 56.7 | 627 | 60.2 | |
| Yes, in detail | 406 | 35.9 | 48 | 4.2 | |
| Preferred model of survivorship care | <.0001 | ||||
| I have primary responsibility | 643 | 56.5 | 103 | 9.3 | |
| Oncologist and PCP share responsibility | 182 | 16.0 | 407 | 37.3 | |
| Someone else has primary responsibility§ | 263 | 23.9 | 428 | 45.8 | |
* Percentages do not always sum to 100 due to missing data. CI = confidence interval; PCP = primary care physician.
† Statistical tests not conducted where variables were not applicable to both oncologists and PCPs. All statistical tests were two-sided.
‡ Hematology (n = 8 [0.7%]), radiation oncology (n = 2 [0.2%]), surgical oncology (n = 1 [0.1%]).
§ Responsibility belongs to specialized survivorship clinics, to the oncologist (for PCPs only), or to the PCP (for oncologists only).
Provision/Receipt of TSs and SCPs
Nearly half of oncologists (49.1%; 95% confidence interval [CI] = 46.4% to 51.8%) reported always/almost always providing TSs, whereas 34.2% (95% CI = 30.8% to 37.7%) of PCPs reported always/almost always receiving TSs (χ 2 (1) = 44.4, P < .001) (Figure 1). Furthermore, 20.2% of oncologists (95% CI = 17.7% to 22.9%) reported always/almost always providing SCPs, whereas 13.4% (95% CI = 11.0% to 16.1%) of PCPs reported always/almost always receiving SCPs (χ 2 (1) = 11.4, P = .001). Fewer than 5% of oncologists and PCPs reported always/almost always providing or receiving care plans without TSs. A greater proportion of oncologists reported providing TSs and SCPs at least “often” (76.0% and 47.7%, respectively); 63.9% and 34.2% of PCPs reported receipt of TSs and SCPs, respectively, at least “often.” Fewer than 5% of oncologists and PCPs reported they “never” provide/receive TSs or SCPs.
Figure 1.
Physician-reported provision and receipt of treatment summaries and survivorship care plans. Survivorship care plans are defined as a treatment summary plus follow-up care plan. Error bars reflect the 95% confidence interval for weighted estimates. Statistically significant differences between oncologists and primary care physicians (PCPs), based on χ2 tests, are indicated by *P = .001 and **P < .001. All statistical tests were two-sided.
Characteristics of Oncologists Who Report Providing TSs or SCPs
Detailed training in late and long-term effects, use of partial or full electronic medical records in clinical practice, Asian or “other” race/ethnicity, and older age were positively associated with always/almost always providing TSs to PCPs (P < .05, Table 3). Detailed training in late and long-term effects, use of partial or full electronic medical records in clinical practice, and Asian race/ethnicity were positively associated with always/almost always providing SCPs to PCPs, whereas an oncology practice size of 6 or more physicians was inversely associated with SCP provision (P < .05, Table 3).
Table 3.
Logistic regression models: oncologist characteristics associated with always/almost always providing treatment summaries (TSs) and survivorship care plans (SCPs) to primary care physicians (PCPs)*
| Characteristic | Treatment summaries (N=1058) | Survivorship care plans† (N=997) |
|---|---|---|
| Adjusted OR (95% CI) †† | Adjusted OR (95% CI) | |
| Received training in late or long-term effects of cancer | Wald F = 4.43, P = .014 | Wald F = 5.94, P = .004 |
| No | Ref | Ref |
| Yes, somewhat | 1.22 (0.74 to 2.01) | 1.43 (0.72 to 2.87) |
| Yes, in detail | 1.74 (1.04 to 2.92)§ | 2.33 (1.15 to 4.70)§ |
| Medical record system | Wald F = 7.75, P <.001 | Wald F = 7.99, P < .001 |
| Paper records and charts | Ref | Ref |
| Partial electronic medical records or in transition to electronic records | 1.64 (1.16 to 2.33)¶ | 1.63 (1.03 to 2.58)§ |
| Full electronic medical records | 2.13 (1.45 to 3.12)‖ | 2.53 (1.58 to 4.06)‖ |
| Practice size | Wald F = 2.70, P = .050 | Wald F = 3.80, P = .013 |
| 1 physician | Ref | Ref |
| 2–5 physicians | 1.09 (0.68 to 1.77) | 0.78 (0.49 to 1.23) |
| 6–15 physicians | 0.77 (0.49 to 1.21) | 0.52 (0.29 to 0.95)§ |
| 16+ physicians | 0.65 (0.37 to 1.15) | 0.38 (0.21 to 0.71)¶ |
| Patient load | Wald F = 0.85, P = .429 | -- |
| ≤50 patients/week | Ref | -- |
| 51–100 patients/week | 1.10 (0.78 to 1.54) | -- |
| ≥101 patients/week | 1.32 (0.85 to 2.05) | -- |
| Percent of patients uninsured/insured by Medicaid | -- | Wald F = 2.04, P = .114 |
| ≤5 | -- | Ref |
| 6 to 10 | -- | 1.09 (0.57 to 2.08) |
| 11 to 20 | -- | 0.70 (0.37 to 1.32) |
| ≥21 | -- | 1.00 (0.53 to 1.88) |
| Race/ethnicity | Wald F = 6.25, P = .003 | Wald F = 5.32, P = .006 |
| Non-Hispanic White | Ref | Ref |
| Asian | 1.68 (1.16 to 2.42)¶ | 1.77 (1.24 to 2.52)¶ |
| Other | 2.00 (1.16 to 3.47)§ | 1.59 (0.86 to 2.96) |
| Age, y | 1.03 (1.01 to 1.04)‖ | -- |
* OR = odds ratio, CI = confidence interval.
† SCPs = treatment summary and care plan
†† Models include factors associated with provision of treatment summaries (TSs) or survivorship care plans (SCPs) at P<.2 in bivariate models. Number of survivors seen per week, preferred model of care, % of time spent in patient care, salary based on productivity, rural vs urban status, and physician sex were not related to either provision of TSs or SCPs at P<.2. All statistical tests were two-sided.
§ P<.05,¶ P<.01, ‖ P<.001
Associations Between PCP-Reported Receipt of TSs or SCPs and Care Outcomes
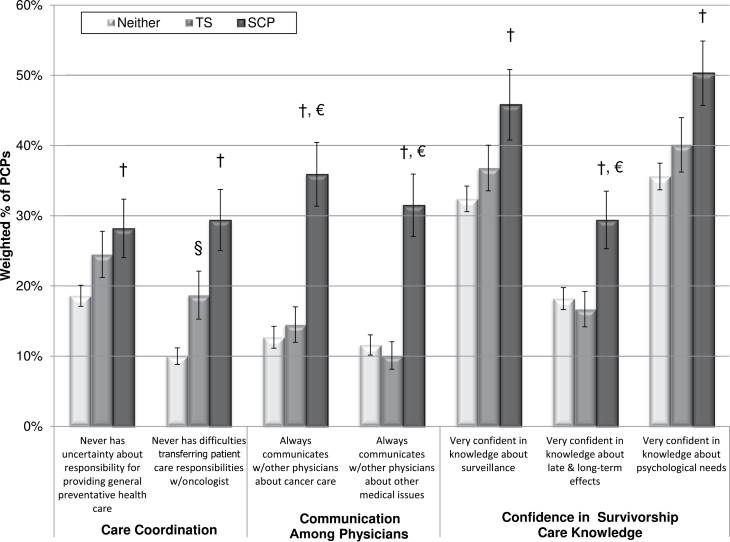
Compared to PCPs who received neither TSs nor SCPs, PCPs who reported always/almost always receiving SCPs were more likely to report never having uncertainty or difficulties related to care coordination, always communicating with other physicians about cancer care and care for other medical issues, and being very confident in knowledge about surveillance, late and long-term effects, and psychosocial needs (all P < .05, Figure 2). Moreover, PCPs who reported always/almost always receiving SCPs were more likely than PCPs who received TSs alone to report always communicating with other physicians about cancer care and other medical issues, and being very confident in knowledge about late and long-term effects (P < .05). PCPs receiving TSs alone were more likely than PCPs who received neither document to report never having difficulties transferring patient care responsibilities (P < .05).
Figure 2.
Associations between primary care physician (PCP) perceptions of receipt of treatment summaries (TSs) and survivorship care plans (SCPs) and three domains of survivorship care: care coordination, physician–physician communication, and confidence in knowledge regarding survivorship care. Sample sizes range from 938 to 950 PCPs. Statistically significant differences (P < .05) based on multiple logistic regression are indicated with § (TSs vs neither), † (SCPs vs neither), and € (SCPs vs TSs). Data are adjusted for number of breast/colon cancer survivors seen per year and PCP age. Error bars reflect the 95% confidence interval for weighted estimates. All statistical tests were two-sided.
Discussion
Nearly half of oncologists reported consistently providing TSs to PCPs, and approximately 1 in 5 oncologists reported consistently providing SCPs. PCPs reported receiving these documents less frequently: approximately one-third of PCPs reported consistent receipt of TSs, whereas 13% reported consistent receipt of SCPs. Discrepancies may reflect differences in response bias, a lack of understanding about the definition of SCPs, or a lack of awareness of receipt and integration of these documents into patient records. Alternatively, PCPs surveyed may not have shared care with oncologists surveyed. Regardless, the infrequent sharing of TSs and SCPs according to both groups suggests that there is a serious gap in implementing the IOM recommendations (3) and pending accreditation standards (13) regarding survivorship care planning.
PCP-reported receipt of SCPs was associated with better PCP-perceived care coordination, physician–physician communication, and confidence in knowledge for all 7 components of survivorship care assessed. In contrast, receipt of TSs alone was only associated with fewer perceived difficulties in transferring care from the oncologist to the PCP. This finding highlights the potential importance of the combined TS and care plan in supporting improved communication and coordination of follow-up care. However, randomized trials testing the utility of providing SCPs to PCPs are necessary. The only randomized trial testing the impact of SCPs was conducted in Canada and did not find substantial effects for patient-reported distress or patient-perceived care coordination (15). However, PCP perceptions of care were not reported, and the validity of this trial and the generalizability of the findings to the United States have been debated (23–25). Future trials should test the utility of SCPs for facilitating communication between oncologists and PCPs; this research would benefit from including PCPs to understand their side of the care transition process (26). Expert consensus guidelines (3) and accreditation standards (13) may need to be expanded to address when and how SCPs should be shared with PCPs. Variation in PCP roles, resources, and practice habits, both within the United States and between the United States and other countries, may affect PCPs’ willingness to provide survivorship care and the impact of SCPs. Although research suggests that PCPs from the United States, Canada, and Europe (16,21,27,28) are willing to care for survivors, particularly given appropriate oncologist–PCP communication, future research should further consider important contextual factors. Future research should also explore the impact of the care planning process (eg, how SCPs are shared, discussed, and modified; the best timing of discussions). Communication and training efforts beyond SCP documents may be necessary to achieve optimal survivorship care (29).
Modifiable factors associated with oncologists’ provision of TSs and SCPs to PCPs represent future intervention targets. Our findings suggest that detailed training in survivorship issues might increase the provision of SCPs. Training may increase oncologists’ evaluation of the importance of care planning or their self-efficacy in developing SCPs. Furthermore, our findings suggest that electronic records may enable implementation of SCPs. Adoption of electronic medical records has been historically low (30), but has increased with federal incentives (31). The “meaningful use” functionality requirements of electronic record systems—namely, care coordination through the exchange of clinical information and patient access to information—are concordant with the goals of SCPs. Electronic medical records may allow oncology teams to populate SCPs more quickly and accurately than paper records, but future research on the utility of electronic records for care planning and how new technologies can best be incorporated into practice workflow is important (32). Our finding that oncologists in larger practices are less likely to provide SCPs merits examination. One might expect larger practices to have more resources to manage sharing these documents; larger practices are perhaps more focused on efficiency and provider time (33). Finally, the reasons that a higher proportion of Asian and other nonwhite oncologists reported provision of TSs and/or SCPs in this study are unknown; potential explanations, including foreign training, warrant further exploration. To best inform future interventions, research should seek to explain why these characteristics were associated with SCP provision.
To our knowledge, this study is the first to assess physician-reported use of TSs and SCPs among a population-based sample of oncologists and PCPs. Several limitations should be considered. Self-reported provision or receipt of SCPs may be inaccurate. It is unclear how physicians defined these documents or responded if SCPs are handled by members of their team (eg, nurses, physician assistants), who may play an important role in delivering SCPs (34). Yet, the similar proportion of oncologists providing TSs to other providers observed in data from the American Society of Clinical Oncology’s Quality Oncology Practice Initiative (44%; Kristen McNiff, MPH, written communication, September 2012) increases confidence in our methodology. Development and sharing of SCPs may differ among providers caring for survivors at high risk of late effects, survivors with lower treatment burden (eg, surgery only), or survivors of cancers for which the follow-up surveillance treatment guidelines are less clear. Research could assess the quality, concordance with IOM recommendations, and usability of SCPs (from patient and provider perspectives), and the circumstances in which SCPs are prepared and delivered. Perceived confidence regarding survivorship care knowledge may differ from actual knowledge, which has been reported by other studies (35). Causal inferences cannot be made regarding receipt of SCPs and care outcomes from this cross-sectional study. Other unmeasured factors (eg, oncologist–PCP communication patterns, care setting) may contribute to observed associations. Longitudinal observational and intervention studies are needed to determine causal relationships between care planning, including specific components of the SCP, and a variety of survivorship care outcomes, including patient-reported outcomes, provider perceptions, objective indicators of PCP knowledge and care provided, and system-level outcomes.
In light of the high and increasing costs of cancer care (36) and projected imbalances between the growing population of cancer survivors and the oncology professionals available to treat them (37), enhancing care planning is important to ensure effective, patient-centered care after primary cancer treatment ends. This study benchmarks current rates of sharing of SCPs among oncologists and PCPs on a national level, improves our understanding of relevant outcomes associated with SCPs, and informs the targeting of future interventions intended to facilitate implementation of SCPs. Currently, most oncologists do not routinely provide PCPs with TSs or SCPs. The slow adoption among providers may in part be related to the lack of empirical evidence about the effect of SCPs upon clinical and patient-centered outcomes. Preliminary evidence presented in this report demonstrates an association between the provision of SCPs (rather than TSs alone) to PCPs and care coordination, physician–physician communication, and PCP confidence in knowledge about survivorship care. Future studies should test the effect of sharing SCPs among oncologists, PCPs, and survivors on care processes, care quality, and survivors’ health-related outcomes using randomized clinical trial designs. Interventions to enhance utilization of SCPs on a national level will likely need to address multiple levels of influence during implementation, including physician factors (eg, training), system-level factors (eg, medical record infrastructure), and other financial factors (eg, reimbursement for care planning process) (38). More research is needed on ways to facilitate the development and delivery of SCPs, such as utilization of nurses or other allied health providers and information technology platforms, so that care planning can be more feasible, scalable, and effective in improving survivorship care delivery across diverse populations and clinical settings.
Funding
This study was supported by the National Cancer Institute (contract number HHSN261200700068C) and the American Cancer Society Behavioral Research Center Intramural Research funds.
Notes
The views expressed in this paper are those of the authors and do not necessarily reflect the views of the Patient-Centered Outcomes Research Institute, the federal government, or the American Cancer Society. The authors have no conflicts of interest to report. The authors gratefully acknowledge Richard Lee (Information Management Services, Inc, Rockville, MD) for his assistance with the statistical analyses.
References
- 1. Parry C, Kent EE, Mariotto AB, Alfano C M, Rowland J H. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev. 2011;20(10):1996–2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Howlader N, Noone A, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations). Bethesda, MD: National Cancer Institute; 2012 [Google Scholar]
- 3. Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington DC: National Academies Press; 2006 [Google Scholar]
- 4. Bober SL, Recklitis CJ, Campbell EG, et al. Caring for cancer survivors: a survey of primary care physicians. Cancer. 2009;115(18 suppl):4409–4418 [DOI] [PubMed] [Google Scholar]
- 5. Cheung WY, Neville BA, Cameron DB, et al. Comparisons of patient and physician expectations for cancer survivorship care. J Clin Oncol. 2009;27(15):2489–2495 [DOI] [PubMed] [Google Scholar]
- 6. Salz T, Oeffinger KC, Lewis PR, et al. Primary care providers’ needs and preferences for information about colorectal cancer survivorship care. J Am Board Fam Med. 2012;25(5):635–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Potosky AL, Han PKJ, Rowland J, et al. Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med. 2011;26(12):1403–1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Forsythe LP, Alfano CM, Leach CR, et al. Who provides psychosocial follow-up care for post-treatment cancer survivors? A survey of medical oncologists and primary care physicians. J Clin Oncol. 2012;30(23):2897–2905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24(32):5117–5124 [DOI] [PubMed] [Google Scholar]
- 10. Arora NK, Reeve BB, Hays RD, et al. Assessment of quality of cancer-related follow-up care from the cancer survivor’s perspective. J Clin Oncol. 2011;29(10):1280–1289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28(27):4154–4161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American Society of Clinical Oncology. ASCO’s library of treatment plans and summaries expands. J Oncol Prac. 2008;4:31–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Commission on Cancer Cancer Program Standards 2012: Ensuring Patient-Centered Care. V1.0. Chicago, IL: American College of Surgeons; 2012 [Google Scholar]
- 14. Stricker CT, Jacobs LA, Risendal B, et al. Survivorship care planning after the Institute of Medicine recommendations: how are we faring? J Cancer Surviv. 2011;5(4):358–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29(36):4755–4762 [DOI] [PubMed] [Google Scholar]
- 16. Del Giudice ME, Grunfeld E, Harvey BJ, et al. Primary care physicians’ views of routine follow-up care of cancer survivors. J Clin Oncol. 2009;27(20):3338–3345 [DOI] [PubMed] [Google Scholar]
- 17. Malin JL, Ko C, Ayanian JZ, et al. Understanding cancer patients’ experience and outcomes: development and pilot study of the Cancer Care Outcomes Research and Surveillance patient survey. Support Care Cancer. 2006;14(8):837–848 [DOI] [PubMed] [Google Scholar]
- 18. Cheung W, Neville B, Cameron D, et al. Comparisons of patient and physician expectations for cancer survivorship care. J Clin Oncol. 2009;27:2489–2495 [DOI] [PubMed] [Google Scholar]
- 19. Ganz PA. Survivorship care planning: Implementing the Survivorship Care Plain. In: Hewitt M, Ganz PA, eds. Implementing Cancer Survivorship Care Planning. Washington, DC: National Academies Press; 2007 [Google Scholar]
- 20. Institute of Medicine From cancer patient to cancer survivor: lost in transition. In: Hewitt M, Greenfield S, Stovall E, eds. Washington DC: National Academies Press; 2006 [Google Scholar]
- 21. Nissen MJ, Beran MS, Lee MW, et al. Views of primary care providers on follow-up care of cancer patients. Fam Med. 2007;39(7):477–482 [PubMed] [Google Scholar]
- 22. Thomas D, Rao J. Small-sample comparisons of level and power for simple goodness-of-fit statistics under cluster sampling. J Am Stat Assoc. 1987;82(398):630–636 [Google Scholar]
- 23. Stricker CT, Jacobs LA, Palmer SC. Survivorship care plans: an argument for evidence over common sense. J Clin Oncol. 2012;30(12):1392–1393 [DOI] [PubMed] [Google Scholar]
- 24. Jefford M, Schofield P, Emery J. Improving survivorship care. J Clin Oncol. 2012;30(12):1391–1392 [DOI] [PubMed] [Google Scholar]
- 25. Smith TJ, Snyder C. Is it time for (survivorship care) plan B? J Clin Oncol. 2011;29(36):4740–4742 [DOI] [PubMed] [Google Scholar]
- 26. Shalom MM, Hahn EE, Casillas J, et al. Do survivorship care plans make a difference? A primary care provider perspective. J Oncol Pract. 2011;7(5):314–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Grunfeld E, Mant D, Vessey MP, et al. Specialist and general practice views on routine follow-up of breast cancer patients in general practice. Fam Pract 1995;12(1):60–65 [DOI] [PubMed] [Google Scholar]
- 28. Paradiso A, Nitti P, Frezza P, et al. A survey in Puglia: the attitudes and opinions of specialists, general physicians and patients on follow-up practice. G.S.Bio.Ca.M. Ann Oncol. 1995;6(suppl 2):53–56 [DOI] [PubMed] [Google Scholar]
- 29. Mayer DK, Gerstel A, Leak AN, et al. Patient and provider preferences for survivorship care plans. J Oncol Pract. 2012;8(4):e80–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. New Engl J Med. 2008;359(1):50–60 [DOI] [PubMed] [Google Scholar]
- 31. Marcotte L, Seidman J, Trudel K, et al. Achieving meaningful use of health information technology: a guide for physicians to the EHR Incentive Programs. Arch Intern Med. 2012;172(9):731–736 [DOI] [PubMed] [Google Scholar]
- 32. Kaplan B, Harris-Salamone KD, Health IT. Success and failure: recommendations from literature and an AMIA workshop. J Am Med Inform Assoc. 2009;16(3):291–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tollen L. Physician organization in relation to quality and efficiency of care: a synthesis of recent literature. Commonwealth Fund Pub; No. 1121; 2008 [Google Scholar]
- 34. Hewitt ME, Bamundo A, Day R, et al. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25(16):2270–2273 [DOI] [PubMed] [Google Scholar]
- 35. Nekhlyudov L, Aziz N, Lerro C, et al. Oncologists’ and primary care providers’ awareness of late effects of cancer treatment: implications for survivorship care. In: Conference Proceedings of the Annual Meeting of the American Society of Clinical Oncology. Chicago, IL; 2012 [Google Scholar]
- 36. Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103(2):117–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007;3(2):79–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zapka J, Taplin SH, Ganz P, et al. Multilevel factors affecting quality: examples from the cancer care continuum. J Natl Cancer Inst Monogr. 2012;2012(44):11–19 [DOI] [PMC free article] [PubMed] [Google Scholar]