Abstract
Background
The extent of clinicians’ commitment to nursing home care varies widely, from those who devote full time to those who care for only a few patients. We assessed potential avoidable hospitalizations of nursing home patients as a function of the percent clinical effort their primary care provider (PCP) devotes to nursing home practice.
Design
A retrospective cohort study
Setting
Nursing homes in Texas
Participants
12,249 patients newly admitted to long term nursing homes in 2006–2008 were identified by linking the Minimum Data Set to 100% Texas Medicare claims data.
Measurements
We measured the care patients received over successive 6 month periods as a time-dependent covariate. Potentially avoidable hospitalizations and Medicare costs were assessed over 6–48 months.
Results
The proportion of nursing home patients with an MD, advance practice nurse (APN) or physician assistant (PA) as their major PCP were 70%, 25%, and 5%, respectively. MD PCPs who derived <20% of their Medicare billings from nursing home patients cared for 36% of all nursing home patients. Most nursing home patients with APN or PA PCPs had providers with ≥85% of Medicare billings generated in nursing homes. Compared to patients whose PCPs devoted ≥85% clinical effort to nursing homes, patients with PCPs who provided <5% nursing home care were at 52% higher risk for potential avoidable hospitalization (1.52, 95% Confidence Interval: 1.25–1.83) and had $2,179 higher annual Medicare spending, controlling for PCP discipline.
Conclusion
The percent of clinical effort providers devote to nursing homes is associated with risk of avoidable hospitalization.
Keywords: Nursing home, primary care, Minimum Data Set, avoidable hospitalization
INTRODUCTION
Residents of nursing homes are at high risk for avoidable emergency room visits and hospitalization (1–5). One reason is availability of primary care providers (PCPs) (3, 6). For the 20% of primary care physicians who practice in nursing homes, nursing home care comprises <10% of their overall work time (7). Nursing home patients typically have multiple chronic conditions that can become acute, necessitating urgent or semi-urgent evaluation and treatment. Because of the limited on-site availability of their providers, this leads to trips to the emergency room and hospitalization.
Studies done in Europe found that full time nursing home physicians reduce hospitalizations (8–9). However, even though this model has grown in some areas of the U.S. (10), it is limited by physician interest in geriatrics and nursing home care (11–12). Studies in the U.S. using full time advance practice nurses (APNs) also found lower emergency room visits and hospitalizations (13–14). In the current study, we assess potential avoidable hospitalizations of nursing home patients as a function of the percent clinical effort their PCP devotes to nursing home practice. Our underlying hypothesis was that patients who had a PCP―whether physician, physician assistant (PA) or APN ― who spent most of his/her clinical effort at nursing homes would have fewer avoidable hospitalizations and lower Medicare costs, compared to patients cared for by PCPs who devote a smaller proportion of their effort to nursing home care.
METHODS
Source of Data
Data from merging the Minimum Data Set (MDS) to 100% Texas Medicare claims data in 2005–2009 were used to identify nursing home residents. We then identified their providers, type of medical care and outcomes through claims from hospital stays (Medicare Provider Analysis and Review, MEDPAR file), outpatient facilities (Outpatient Statistical Analysis files, OUTSAF) and physician services (Carrier files).
Establishment of the Study Cohort
Our overall approach was to identify Medicare enrollees age 66 and older admitted to nursing homes in 2006–2008, and who had not been in long term care in the previous year. We excluded patients without Medicare Parts A and B coverage, those who were enrolled in a health maintenance organization (HMO) for any time in the 12 months before nursing home enrollment, and those whose stay in the nursing home was less than 180 days. We used the method of Intrator et al. (15) to distinguish admissions to skilled nursing facilities (SNFs) or long term care nursing homes. In this report, we studied only admissions to long term care nursing homes. The final study cohort was 12,249 Texas Medicare patients in 1,094 Texas nursing homes.
Identification of Providers
Individual providers were identified by their Unique Provider Identification Number (UPIN) for years 2006–2007 and their National Provider Identifier (NPI) for years 2007–2008. We included only patients with an outpatient or nursing home Evaluation and Management (E&M) service provided by generalist physicians (general practitioner, family physician, general internist or geriatrician), APNs or PAs during the patient’s first 6 months of the nursing home stay.
We should note that all PAs and most APNs work in collaboration with MDs. Our intent was to identify the provider who provided the most care for a given patient, and rate that provider on the percent of their clinical effort devoted to nursing home care. We identified the major nursing home PCP for each patient as the provider who billed the most E&M services over the first 6 months, and then over succeeding 6 month period throughout the follow-up period (e.g., months 0–6, 1–7, 2–8, etc) as a time-dependent covariate. If two providers billed for the same number of E&M charges, the major PCP was designated as (in order) the MD, then APN. For each provider, we estimated his/her nursing home clinical effort based on the proportion of their total E&M bills from nursing home services (both long term care and SNF) in 2006–2008. We counted the number of PCPs who provided nursing home services to the patient and the total number of PCP visits as time-dependent covariates.
Measures
Medicare enrollment files provided data on patient age and gender, and MDS data provided data on race/ethnicity and education. We used the admission assessment data from MDS to obtain cognitive function (short term / long term memory problem, daily decision-making skills), activities of daily living (ADL) and comorbid diseases (16–17). To better aggregate multiple risk factors, we calculated the hospitalization risk score using the model developed for nursing home patients by the Centers for Medicare and Medicaid Services (CMS) (18). This model includes age, sex, Charlson comorbidity score, number of hospitalizations in the previous 90 days, and occurrences of pneumonia, urinary tract infections, pressure ulcers, oral feeding tubes, septicemia, parenteral/IV nutrition, indwelling catheters and antibiotic-resistant infections, with specific weighted coefficients for each covariate.
Study Outcomes
The outcomes were potential avoidable hospitalization and average Medicare costs. Medicare costs were estimated from the paid amounts in the MEDPAR, OUTSAF and carrier files, following the payment calculation worksheets provided by the Research Data Assistance Center. We presented the cost estimates in 2009 dollars using the gross domestic product deflator. Potential avoidable hospitalizations were taken from a list of ambulatory-care sensitive conditions (e.g., dehydration, diabetes, congestive heart failure, chronic obstructive pulmonary disease, urinary tract infection) developed by the Agency for Healthcare Quality and Research (19).
Statistical Analyses
We first used the proportion of each PCP’s E&M bills that were generated from nursing homes as a continuous variable to assess its effect on hospitalization. By the Cumulative Martingale Residuals plot, a nonlinear function form was found. Based on both the log-likelihood ratio test and Akaike’s information criterion, the best-fitting model was quadratic. To preserve the functional form and for ease of interpretation, we categorized the proportions of PCP bills in nursing homes into five levels: <5%, 5–19%, 20–49%, 50–84% and >85%.
A multilevel survival model (20) was built to study the time dependent effect of the PCP’s effort in nursing homes on avoidable hospitalization, adjusting for the clustering of patients within nursing home facilities, patient race/ethnicity, education, number of ADLs and hospitalization risk score. In addition, the pattern of primary care, including number of different primary care providers, number of primary care visits and PCP discipline, was adjusted in a time dependent manner in succeeding six month intervals (e.g., months 0–6, 1–7, 2–8, etc). In these analyses, nursing home was treated as a random effect and patients were censored at death, discharge from the nursing home, no identifiable PCP over a six month period, or the end of study (12/31/2009). We also assessed the percentage of variance in having potentially preventable hospitalizations attributed to patient characteristics, the pattern of primary care, and the nursing homes (21).
We used a two-part log gamma model to estimate differences in Medicare costs model. The model included a logit model in the first part (which estimated the percent of patients with any Medicare costs) and a log gamma model in the second part (which estimated the average costs for those patients with any costs) (22). In these analyses, the percent Medicare charges the PCP generated from nursing home care, number of PCPs, number of PCP visits and PCP discipline were measured in the initial 6 months and Medicare costs were measured over the 6–18 month period, with censoring as described above.
RESULTS
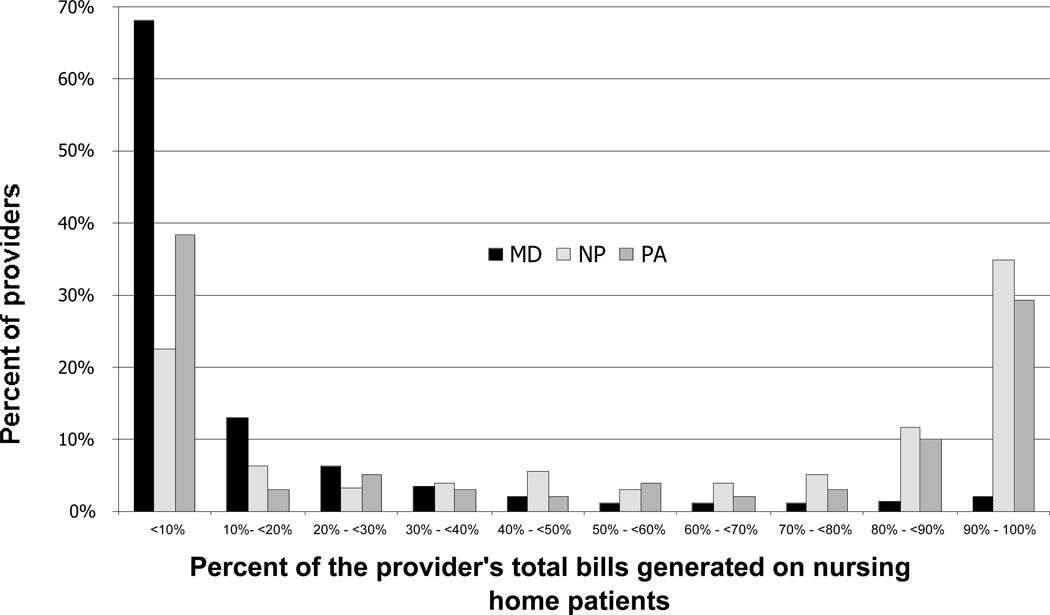
Our sample included 12,249 patients who were admitted to a long term care nursing home in 2006–2008 and who had not resided in a long term care facility in the prior 12 months. We identified 2,317 PCPs for these patients. Of those, 80% were MDs, 16% were ANPs and 4% were PAs. Figure 1 shows the distribution of these PCPs as a function of the percent of their Medicare E&M claims generated from nursing home patients. More than 80% of MD PCPs generated fewer than 20% of their Medicare charges from nursing home patients, while less than 4% of MD PCPs generated ≥80% their Medicare charges from nursing home patients. In contrast, 46% of APNs and 39% of PAs generated ≥80% of their Medicare charges from nursing home patients.
Figure 1.
Distribution of primary care providers by the percentage of their Evaluation and Management claims to Medicare that were generated on nursing home patients, stratified by discipline of the primary care provider.
The proportions of nursing home patients with an MD, APN or PA as their PCP were 70%, 25%, and 5%, respectively. Half of all nursing home patients who had an MD as their PCP received care from a provider who derived <20% of their Medicare billings from nursing home care. This represents 36% of all nursing home patients. In contrast, >60% of nursing home patients with APN or PA PCPs had providers with ≥85% of Medicare billings generated in nursing homes (Table 1, bottom).
Table 1.
Characteristics of nursing home patients cared for by primary care providers (PCPs) with different levels of clinical effort in nursing homes and with different disciplines.
| % bills generated from Nursing Homes | Primary Care Provider Discipline | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <5% | 5 – 19% | 20 – 49% | 50 – 85% | >=85% | p-value | MD | NP | PA | p-value | |
| Number of patients | 2171 | 2580 | 2466 | 1963 | 3069 | 8841 | 2845 | 563 | ||
| Age (years) | ||||||||||
| 66 – 74 | 13.2% | 14.2% | 14.3% | 15.6% | 16.0% | 0.0483 | 14.2% | 16.0% | 16.0% | 0.0943 |
| 75 – 84 | 41.0% | 39.5% | 42.3% | 40.6% | 39.9% | 41.1% | 39.7% | 37.8% | ||
| 85 + | 45.8% | 46.3% | 43.4% | 43.8% | 44.1% | 42.7% | 44.3% | 46.2% | ||
| 83.3 ± 7.2 | 83.1 ± 7.5 | 82.8 ± 7.4 | 82.8 ± 7.6 | 82.8 ± 7.6 | 83.0 ± 7.5 | 82.7 ± 7.5 | 83.1 ± 7.6 | |||
| Female | 72.8% | 72.9% | 71.7% | 70.9% | 72.6% | 0.5185 | 72.1% | 72.6% | 73.2% | 0.7513 |
| Race | ||||||||||
| White | 75.3% | 79.9% | 78.4% | 77.0% | 78.2% | <0.0001 | 77.5% | 79.4% | 76.9% | <0.0001 |
| Hispanic | 18.3% | 11.7% | 13.0% | 11.5% | 10.0% | 13.6% | 9.9% | 11.7% | ||
| Black | 5.6% | 7.7% | 7.6% | 9.7% | 10.8% | 7.9% | 9.8% | 10.3% | ||
| Others | 0.8% | 0.7% | 1.0% | 1.8% | 0.9% | 1.0% | 0.9% | 1.1% | ||
| High School graduate or above | 63.0% | 60.5% | 64.0% | 67.6% | 68.8% | <0.0001 | 63.6% | 67.3% | 71.6% | <0.0001 |
| Risk of hospitalizationa | 0.58 ± 0.09 | 0.58 ± 0.09 | 0.57 ± 0.08 | 0.58 ± 0.09 | 0.58 ± 0.09 | 0.3950 | 0.58 ± 0.09 | 0.58 ± 0.09 | 0.57 ± 0.08 | 0.1274 |
| Short term memory problemb | 71.3% | 75.9% | 78.8% | 78.6% | 79.9% | <0.0001 | 76.5% | 79.2% | 76.9% | 0.0125 |
| Long term memory problemb | 47.7% | 52.7% | 55.9% | 56.0% | 57.7% | <0.0001 | 53.3% | 57.7% | 52.3% | 0.0002 |
| Decision makingb | ||||||||||
| Independent | 19.9% | 15.7% | 15.3% | 14.9% | 13.3% | <0.0001 | 16.2% | 14.0% | 15.3% | 0.0002 |
| Modified independent | 35.0% | 33.2% | 31.0% | 31.4% | 30.5% | 32.4% | 31.0% | 32.2% | ||
| Moderated impaired | 35.4% | 39.4% | 40.7% | 40.2% | 41.1% | 39.5% | 39.6% | 39.5% | ||
| Severely impaired | 9.6% | 11.7% | 13.0% | 13.5% | 15.2% | 11.9% | 15.4% | 13.0% | ||
| Physical function limitation (ADL)b | ||||||||||
| 0 | 8.6% | 10.9% | 10.9% | 8.7% | 7.1% | <0.0001 | 9.7% | 7.4% | 11.4% | 0.0094 |
| 1 – 2 | 17.5% | 16.8% | 16.9% | 14.7% | 18.3% | 16.8% | 17.3% | 17.1% | ||
| 3 – 4 | 15.4% | 14.9% | 16.0% | 16.3% | 14.8% | 15.5% | 15.6% | 13.6% | ||
| >=5 | 58.6% | 57.4% | 56.1% | 60.4% | 59.7% | 58.0% | 59.7% | 57.9% | ||
| Health conditionb | ||||||||||
| Diabetes | 25.7% | 24.5% | 21.9% | 22.8% | 24.3% | 0.0290 | 23.7% | 24.8% | 22.5% | 0.3849 |
| Hypothyroidism | 20.4% | 22.3% | 20.8% | 20.4% | 20.5% | 0.5277 | 20.8% | 20.0% | 27.1% | 0.0023 |
| Anxiety Disorder | 16.6% | 17.3% | 16.2% | 16.1% | 18.5% | 0.1923 | 16.1% | 19.3% | 20.7% | 0.0001 |
| Depression | 33.0% | 33.3% | 35.7% | 37.6% | 41.1% | <0.0001 | 34.5% | 41.4% | 40.5% | <0.0001 |
| CHFd | 15.3% | 15.5% | 14.9% | 16.3% | 17.5% | 0.1230 | 15.6% | 16.9% | 16.6% | 0.2934 |
| Hypertension | 70.4% | 68.8% | 66.4% | 68.8% | 67.8% | 0.1116 | 68.2% | 67.9% | 71.8% | 0.2450 |
| PVDd | 6.4% | 6.0% | 5.7% | 7.1% | 6.4% | 0.4566 | 6.0% | 6.8% | 7.9% | 0.1381 |
| COPDd | 10.8% | 10.7% | 9.2% | 11.7% | 11.9% | 0.0450 | 10.6% | 11.7% | 10.6% | 0.3726 |
| Arthritis | 23.6% | 24.9% | 22.5% | 25.9% | 25.1% | 0.1114 | 24.0% | 24.7% | 29.7% | 0.0189 |
| Osteoporosis | 19.5% | 18.6% | 20.5% | 22.4% | 23.4% | 0.0005 | 20.2% | 22.0% | 27.4% | 0.0004 |
| Anemia | 13.9% | 13.5% | 14.4% | 16.3% | 19.3% | <0.0001 | 14.5% | 19.1% | 16.9% | <0.0001 |
| Cancer | 4.6% | 5.0% | 4.3% | 5.2% | 6.0% | 0.1087 | 4.9% | 5.2% | 6.8% | 0.1910 |
| Alzheimer’s Disease | 24.9% | 27.5% | 29.0% | 26.4% | 29.7% | 0.0041 | 27.3% | 29.4% | 25.9% | 0.1026 |
| Dementia | 32.3% | 37.4% | 39.2% | 42.7% | 42.2% | <0.0001 | 37.8% | 41.9% | 43.2% | 0.0003 |
| Stroke | 14.1% | 14.6% | 15.6% | 14.3% | 15.4% | 0.5073 | 14.7% | 15.4% | 15.0% | 0.6302 |
| UTId | 7.7% | 9.3% | 7.5% | 9.6% | 9.0% | 0.0354 | 8.2% | 9.5% | 10.8% | 0.0223 |
| Total number of providersc | 1.4 ± 0.8 | 1.4 ± 0.7 | 1.5 ± 0.7 | 1.7 ± 0.8 | 2.1 ± 0.9 | <0.0001 | 1.4 ± 0.6 | 2.1 ± 0.7 | 2.0 ± 0.7 | <0.0001 |
| Total number of provider visitsc | 3.5 ± 3.0 | 4.8 ± 2.9 | 6.0 ± 3.8 | 7.2 ± 4.8 | 8.4 ± 4.9 | <0.0001 | 5.5 ± 4.0 | 8.1 ± 4.9 | 7.5 ± 4.7 | <0.0001 |
| Discipline of PCP | ||||||||||
| MD | 92.8% | 92.9% | 85.9% | 69.6% | 30.8% | <0.0001 | ||||
| NP | 4.8% | 6.0% | 12.3% | 25.8% | 57.8% | |||||
| PA | 2.4% | 1.1% | 1.8% | 4.6% | 11.4% | |||||
| % bills generated from Nursing Homes | ||||||||||
| <5% | 22.8% | 3.7% | 9.2% | <0.0001 | ||||||
| 5 – 19% | 27.1% | 5.4% | 5.0% | |||||||
| 20 – 49% | 24.0% | 10.7% | 7.8% | |||||||
| 50 – 85% | 15.4% | 17.8% | 16.0% | |||||||
| >=85% | 10.7% | 62.4% | 62.0% | |||||||
Risk of hospitalization was based on the hospitalization risk adjustment model developed for nursing home patients by the Center for Medicare and Medicaid Service (18). This model includes age, sex, Charlson comorbidity score, number of hospitalizations in the previous 90 days, and occurrences of pneumonia, urinary tract infections, pressure ulcers, oral feeding tubes, septicemia, parenteral/IV nutrition, indwelling catheters and antibiotic resistant infections, with specific weighting coefficients for each covariate.
Derived from MDS admission assessment
Providers were limited to generalist physicians (general internal medicine, family medicine, geriatrician, and general practitioner), advanced practices nurses (APNs), and physician assistants (PAs).
PVD, peripheral artery disease; COPD, chronic obstructive pulmonary disease; CHF: congestive heart failure; UTI: urinary tract infection.
Table 1 also presents the characteristics of patients, stratified by the proportion of Medicare charges their PCP generated from nursing homes. Patients differed little in age and overall risk of hospitalization by level of provider nursing home effort. Patients cared for by providers with ≥85% clinical effort in nursing homes were less likely to be Hispanic, more likely to have a high school education, more likely to have cognitive impairment, ADL limitation and a greater number of chronic conditions, and had more provider visits in the initial 6 month period. When patient characteristics were stratified by discipline of the PCP, patients cared for by APNs and PAs had similar characteristics to those with PCPs who provided ≥ 85% effort to nursing homes.
Table 2 presents the results of multilevel multivariable survival analyses for potential avoidable hospitalizations as a function of the percent Medicare charges the PCP generated from nursing home care. Risk of potentially-avoidable hospitalizations increased with decreasing levels of PCP nursing home effort (p<0.001 for linear trends). For example, compared to patients whose PCPs devoted >85% effort to nursing homes, patients whose PCPs had <5% nursing home effort were at 52% higher risk for potential avoidable hospitalization (1.52, 95% CI: 1.25–1.83). The risk of hospitalization did not differ between MDs, APNs and PAs. In this multilevel analysis we calculated the variation in risk of preventable hospitalization due to the measured patient characteristics, the model of primary care, and the nursing home. Measureable patient characteristics and the primary care model accounted for 7.5% and 6.8%of the variation, respectively, while very little (0.1%) of the variation was attributed to the individual nursing homes.
Table 2.
Potentially avoidable hospitalization and yearly Medicare cost for nursing home patients cared for by primary care providers (PCPs), by level of provider nursing home effort.
|
Potentially Avoidable Hospitalizationa |
Yearly Average Adjusted Medicare Costsb (95% CI) | ||||||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | Professional Services |
Outpatient Facilitiesd |
Hospital |
Skilled
Nursing Facilities |
Total | ||
| In the Nursing Home |
Out of the Nursing Home |
||||||
| % PCP effort in nursing homes | |||||||
| <5% | 1.52 | $594 | $2,104 | $2,177 | $4,367 | $5,881 | $15,178 |
| (1.25 – 1.83) | (548 – 644)e, f | (1920 – 2307)e, f | (1948 – 2432) | (4012 – 4753)e, f | (5370 – 6439)e | (13838 – 16646)e | |
| 5 – 19% | 1.44 | $756 | $1,923 | $2,009 | $3,950 | $5,280 | $13,940 |
| (1.21 – 1.72) | (705 – 812)e, f | (1760 – 2101) | (1794 – 2249) | (3615 – 4316) | (4817 – 5787) | (12694 – 15308) | |
| 20 – 49% | 1.17 | $841 | $1,839 | $1,998 | $3,686 | $4,907 | $13,103 |
| (098 – 1.40) | (788 – 897) | (1676 – 2018) | (1804 – 2213) | (3560 – 4063) | (4490 – 5362) | (11994 – 14316) | |
| 50 – 84% | 1.08 | $930 | $1,758 | $2,022 | $3,637 | $5,139 | $13,467 |
| (0.90 – 1.34) | (876 – 988) | (1590 – 1943) | (1780 – 2296) | (3346 – 3953) | (4683 – 5639) | (12328 – 14710) | |
| >85% | 1.00 | $942 | $1,830 | $1,923 | $3,629 | $4,780 | $12,999 |
| (892 −995) | (1689 – 1984) | (1752 – 2113) | (3384 – 3891) | (4457 – 5125) | (12020 – 14032) | ||
| Discipline of primary care provider | |||||||
| MD | 1.00 | ||||||
| NP | 1.08 | (0.92 – 1.26) | |||||
| PA | 1.04 | (0.76 – 1.42) | |||||
| Total number of providers seen | |||||||
| 1 | 1.00 | ||||||
| 2 | 1.06 | (0.93 – 1.21) | |||||
| >=3 | 1.07 | (0.88 – 1.30) | |||||
| Total number of provider visits | 1.05 | (1.04 – 1.06) | |||||
| Risk scorec | 1.02 | (0.96 – 1.08) | |||||
| every 10% increased | |||||||
| Race/Ethnicity | |||||||
| White | 1.00 | ||||||
| Black | 1.04 | (0.86 – 1.25) | |||||
| Hispanic/Others | 0.91 | (0.77 – 1.07) | |||||
| Education – High school or above | 0.82 | (0.74 – 0.92) | |||||
| Physical function limitation (ADL) | 1.04 | (1.02 – 1.07) | |||||
Hazard ratios for potentially avoidable hospitalization for patients cared for by providers with different degrees of nursing home involvement were estimated from the multilevel survival model adjusted for the covariates listed and the clustering patients within nursing home facilities. Avoidable hospitalizations include hospitalizations with a primary diagnosis of ambulatory sensitive conditions (19). This model included time-dependent covariates for provider’s clinical effort in nursing home, discipline of primary care provider, total number of providers seen and total number of provider visits measured over the first 6 months, and shifted monthly throughout the follow-up period.
Adjusted for race/ethnicity, education, ADL, risk of hospitalization, total number of providers seen in first 6 months, total number of provider visits in first 6 months, discipline of primary care provider, number of months in the 12 month follow-up period, and the cluster effect of nursing homes.
Risk of hospitalization was based on the hospitalization risk adjustment model developed for nursing home patients by the Center for Medicare and Medicaid Service (19).
Outpatient facilities represent facility charges (i.e. non-professional charges), such as hospital based clinic, laboratories, radiology etc.
Significantly different from those with PCPs with nursing home effort >85%
Significantly different from those with PCPs with nursing home effort 50 – 84%
Table 2 also shows the average adjusted Medicare costs as a function of the percent of provider Medicare charges generated from nursing home care. Costs were assessed for the period 6 to 18 months after nursing home admission. Annual Medicare spending was $2,179 higher for patients cared for by PCPs with <5% nursing home effort compared to patients cared for by PCPs with ≥85% nursing home effort (p<0.001). Professional charges for provider visits in the nursing home were higher in patients with full time nursing home providers, while costs were lower in all other cost categories. Results of analyses extended to 48 months of follow up were similar. Average monthly cost was $208 higher for patients cared for by PCPs with <5% nursing home effort compared to those whose PCPs had ≥85% nursing home effort (p<0.001).
In additional analyses, we examined overall survival of the patients and length of stay in the nursing home, as a function of provider discipline or by provider percent time in the nursing home. There were no significant differences in any comparisons (data not presented).
DISCUSSION
Our study is the first population-based study to examine the association between provider nursing home effort and medical outcomes. We found a one third reduction in avoidable hospitalizations for patients cared for by providers spending >85% of their effort in nursing homes compared to those who spent <5%. This is consistent with findings from European (8–9) and Canadian (23) studies. The magnitude of cost reduction found in our study is similar to that found by INTERACT, a CMS program to facilitate communication and manage acute changes in nursing home patients (24–25).
Skilled nursing facilities (SNF) were responsible for approximately 38% of the total Medicare costs in this cohort of long term care nursing home patients (Table 2). SNF care is funded by Medicare for post-hospitalization care of patients expected to return to the community. It is surprising that patients who had spent at least 6 months in long term care nursing homes would subsequently experience substantial SNF costs.
Several barriers limit the availability of full time providers in nursing homes. Patients entering a nursing facility may prefer to be cared for by their own community-based PCP with whom they have a relationship. Physicians may be reluctant to provide full-time nursing home care due to the perceived high rate of nursing-home-related malpractice and relatively low reimbursement rate for such care (26). Nursing homes may wish to avoid the cost of employing full time APNs or PAs (27). For APNs and PAs, the scope of their clinical activities may be limited by state laws (28).
In the multilevel null model, the variance in risk of preventable hospitalization attributed to nursing homes was 7.3%. After adjusting for the pattern of primary care and measurable patient characteristics (age, gender, individual factors in the hospitalization risk model) the nursing homes had almost no impact explaining 0.1% of the variance. This suggest that differences among nursing homes in hospitalization rates is mediated via different models of providing primary care, as well as differences in patient case mix. Our study cohort was new residents in long term nursing homes. The impact of the nursing home might be greater in longer term nursing home patients.
This study has certain limitations. First, our method of identifying the patient’s major PCP is based on E&M charges. Our estimate of care from APNs or PAs is conservative. When both the physician and an APN/PA personally perform and document a substantive portion of a face-to-face encounter with the patient, the physicians rather than the APN/PA will normally submit the charge because of a 15% higher reimbursement rate (29). Second, we used UPIN/NPI to identify individual PCPs who provided care to the patients. We recognize that all PAs and most APNs are working in collaboration with MDs in nursing homes. Our intent was to identify the provider who provided the most care for a given patient. We were unable to identify teams consisting of an MD and APN or PA with our data. Future exploratory studies on using taxpayer identification number or through social network analyses to identify teams would be useful. Third, patients cared for by providers with different degrees of effort in the nursing home and providers from different disciplines are different (Table 1). We adjusted for these differences. MDS is superior to claims data in allowing for better adjustment of risk factors in analyses of the impact of different patterns of care on patient outcomes (18). Last, we studied nursing home residents in Texas. The study findings may be not generalizable to regions outside Texas.
In summary, the effort providers devote to the nursing home setting is associated with risk of potential avoidable hospitalization regardless of the discipline of the provider. This result could guide stakeholders in making more informed decisions about cost-effective care for long-term nursing home residents.
ACKNOWLEDGMENTS
We thank Sarah Toombs Smith, PhD, Science Editor and Assistant Professor in the Sealy Center on Aging, University of Texas Medical Branch at Galveston, for her editorial assistance.
Grant Support: This work was supported by grants R01-HS020642 from the Agency for Healthcare Research and Quality, R01-AG033134 and P30-AG024832 from the National Institute on Aging, K05-CA134923 from the National Cancer Institute, and UL1-RR029876 from the National Center for Research Resources, National Institutes of Health. The funders had no role in the design and conduct of study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Sponsor’s Role: Sponsors had no role in the design, methods, subject recruitment, data collection, analysis or preparation of the paper.
Footnotes
Conflict of Interest Disclosure: The authors have no financial, personal or potential conflicts of interest to disclose.
Author Contributions: Kuo: Study concept and design, analysis and interpretation of data, drafting the manuscript. Raji: Interpretation of data and critical review of the manuscript. Goodwin: Study concept and design, interpretation of data, drafting and critical review of the manuscript.
REFERENCES
- 1.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 2.Walker JD, Teare GF, Hogan DB, et al. Identifying potentially avoidable hospital admissions from Canadian long-term care facilities. Med Care. 2009;47:250–254. doi: 10.1097/MLR.0b013e3181847588. [DOI] [PubMed] [Google Scholar]
- 3.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalization of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc. 2010;58:627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- 4.Ouslander JG, Berenson RA. Reducing unnecessary hospitalizations of nursing home residents. N Engl J Med. 2011;365:1165–1167. doi: 10.1056/NEJMp1105449. [DOI] [PubMed] [Google Scholar]
- 5.Walsh EG, Wiener JM, Haber S, et al. Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc. 2012;60:821–829. doi: 10.1111/j.1532-5415.2012.03920.x. [DOI] [PubMed] [Google Scholar]
- 6.Shield RR, Wetle T, Teno J, et al. Physicians ‘‘missing in action’’: Family perspectives on physician and staffing problems in end-of-life care in the nursing home. J Am Geriatr Soc. 2005;53:1651–1657. doi: 10.1111/j.1532-5415.2005.53505.x. [DOI] [PubMed] [Google Scholar]
- 7.Katz PR, Karuza J, Kolassa J, et al. Medical practice with nursing home residents: Results from the National Physician Professional Activities Census. J Am Geriatr Soc. 1997;45:911–917. doi: 10.1111/j.1532-5415.1997.tb02958.x. [DOI] [PubMed] [Google Scholar]
- 8.Johnson M. Changing the culture of nursing homes: The physician’s role. Arch Intern Med. 2010;170:407–409. doi: 10.1001/archinternmed.2009.550. [DOI] [PubMed] [Google Scholar]
- 9.Schols J, Crebolder H, van Weel C. Nursing home and nursing home physician: The Dutch experience. Long-Term Care around the Globe. J Am Med Direct Assoc. 2004;5:207–212. doi: 10.1097/01.JAM.0000123031.43619.60. [DOI] [PubMed] [Google Scholar]
- 10.Levy C, Epstein A, Landry L, et al. Office of Disability, Aging and Long-Term Care Policy, Office of the Assistant Secretary for Planning and Evaluation. U.S. Department of Health and Human Services; Physician practice in nursing homes: Final report. Contract #HHS-100-03-0028. [Google Scholar]
- 11.Kane RS. Factors affecting physician participation in nursing home care. J Am Geriatr Soc. 1993;41:1000–1003. doi: 10.1111/j.1532-5415.1993.tb06768.x. [DOI] [PubMed] [Google Scholar]
- 12.Thomas DC, Leipzig RM, Smith LG, et al. Improving geriatrics training in internal medicine residency programs: Best practices and sustainable solutions. Ann Intern Med. 2003;139:628–634. doi: 10.7326/0003-4819-139-7-200310070-00037. [DOI] [PubMed] [Google Scholar]
- 13.Kane RL, Keckhafer G, Flood S, et al. The effect of Evercare on hospital use. J Am Geriatr Soc. 2003;51:1427–1434. doi: 10.1046/j.1532-5415.2003.51461.x. [DOI] [PubMed] [Google Scholar]
- 14.Burl JB, Bonner A, Rao M, et al. Geriatric nurse practitioners in long-term care: Demonstration of effectiveness in managed care. J Am Geriatr Soc. 1998;46:506–510. doi: 10.1111/j.1532-5415.1998.tb02475.x. [DOI] [PubMed] [Google Scholar]
- 15.Intrator O, Hiris J, Berg K, et al. The residential history file: Studying nursing home residents’ long term care histories. Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mor VA. comprehensive clinical assessment tool to inform policy and practice: Applications of the Minimum Data Set. Med Care. 2004;42:50–59. doi: 10.1097/01.mlr.0000120104.01232.5e. [DOI] [PubMed] [Google Scholar]
- 17.Crystal S, Gaboda D, Lucas J, et al. Assessing medication exposure and outcomes in the frail elderly: Assessing research challenge in nursing home pharmacotherapy. Med Care. 2010;48:S23–S31. doi: 10.1097/MLR.0b013e3181de9d10. [DOI] [PubMed] [Google Scholar]
- 18.Risk adjustment for hospitalization measures nursing home value based purchasing (NHVBP) demonstration. [Accessed May 20 2011];Centers for Medicare and Medicaid Services. https://www.cms.gov/DemoProjectsEvalRpts/downloads/NHP4P_Hospitalization_Risk_Adjustment.pdf.
- 19.White A, Hurd D, Moore T, et al. Quality Monitoring for Medicare Global Payment Demonstrations: Nursing Home Quality-Based Purchasing Demonstration. Abt Associates, Inc. for the Centers for Medicare and Medicaid Services. Contract # 500-00-0032. [Google Scholar]
- 20.Klein JP, Moeschberger ML. Survival Analysis: Techniques for Censored and Truncated Data. 2nd ed. New York, NY: Springer Publication Co. Inc; 2003. [Google Scholar]
- 21.Lam KF, Ip D. REML and ML estimation for clutered grouped survival data. Stat Med. 2003;22:2025–2034. doi: 10.1002/sim.1323. [DOI] [PubMed] [Google Scholar]
- 22.Mullahy J. Much ado about two: Reconsidering retransformation and the two-part model in helath econometrics. J Health Econ. 1998;17:247–281. doi: 10.1016/s0167-6296(98)00030-7. [DOI] [PubMed] [Google Scholar]
- 23.McAiney CA, Haughton D, Jennings J, et al. A unique practice model for nurse practitioners in long-term care homes. J Adv Nurs. 2008;62:562–571. doi: 10.1111/j.1365-2648.2008.04628.x. [DOI] [PubMed] [Google Scholar]
- 24.Ouslander JG, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011;59:745–753. doi: 10.1111/j.1532-5415.2011.03333.x. [DOI] [PubMed] [Google Scholar]
- 25.Tena-Nelson R, Santos K, Weingast E, et al. Reducing potentially preventable hospital transfers: Results from a thirty nursing home collaborative. J Am Med Dir Assoc. 2012;13:651–656. doi: 10.1016/j.jamda.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 26.Katz PR, Karuza J, Intrator O, et al. Nursing home physician specialists: A response to the workforce crisis in long-term care. Ann Intern Med. 2009;150:411–413. doi: 10.7326/0003-4819-150-6-200903170-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stefanacci RG. Will nurse practitioners replace physicians as attendings in long-term care? J Am Med Dir Assoc. 2001;2:222–224. [PubMed] [Google Scholar]
- 28.Lugo NR, O’Grady ET, Hodnicki DR, et al. Ranking state NP regulation: practice environment and consumer healthcare choice. Am J Nurse Pract. 2007;11:8–24. [Google Scholar]
- 29.Kleinpell RM, Frech KD, Diamond EJ. Billing for NP provider services: updates on coding regulations. Nurse Pract. 2007;32:16–17. doi: 10.1097/01.NPR.0000275347.71945.62. [DOI] [PubMed] [Google Scholar]