ABSTRACT
BACKGROUND
A minority of hospitalized smokers actually receives assistance in quitting during hospitalization or cessation counseling following discharge. This study aims to determine the impact of a guideline-based intervention on 1) nurses’ delivery of the 5A’s (Ask-Advise-Assess-Assist-Arrange follow-up) in hospitalized smokers, and 2) nurses’ attitudes toward the intervention.
METHODS
We conducted a pre-post guideline implementation trial involving 205 hospitalized smokers on the inpatient medicine units at one US Department of Veterans Affairs (VA) medical center. The intervention included: 1) academic detailing of nurses on delivery of brief cessation counseling, 2) modification of the admission form to facilitate 5A’s documentation, and 3) referral of motivated inpatients to receive proactive telephone counseling. Based on subject interviews, we calculated a nursing 5A’s composite score for each patient (ranging from 0 to 9). We used linear regression with generalized estimating equations to compare the 5A’s composite score (and logistic regression to compare individual A’s) across periods. We compared 29 nurses’ ratings of their self-efficacy and decisional balance (“pros” and “cons”) with regard to cessation counseling before and after guideline implementation. Following implementation, we also interviewed a purposeful sample of nurses to assess their attitudes toward the intervention.
RESULTS
Of 193 smokers who completed the pre-discharge interview, the mean nursing 5A’s composite score was higher after guideline implementation (3.9 vs. 3.1, adjusted difference 1.0, 95 % CI 0.5–1.6). More patients were advised to quit (62 vs. 48 %, adjusted OR = 2.1, 95 % CI = 1.2–3.5) and were assisted in quitting (70 vs. 45 %, adjusted OR = 2.9, 95 % CI = 1.6–5.3) by a nurse during the post-implementation period. Nurses’ attitudes toward cessation counseling improved following guideline implementation (35.3 vs. 32.7 on “pros” subscale, p = 0.01), without significant change on the “cons” subscale.
CONCLUSIONS
A multifaceted intervention including academic detailing and adaptation of the nursing admission template is an effective strategy for improving nurses’ delivery of brief cessation counseling in medical inpatients.
KEY WORDS: smoking cessation, Veterans, counseling, guideline-based intervention
BACKGROUND
Those who are medically ill smoke at higher rates than the general population (37 vs. 21 %, respectively)1 and benefit substantially from smoking cessation, which reduces the risk of lung cancer, heart disease, stroke, and chronic lung disease.2 Hospitalization has been identified as a “teachable moment” for many smokers,3 as inpatients are not exposed to the usual external cues to smoke4 and the acute illness brings them into contact with health professionals who are well positioned to provide assistance in quitting. Although adherence to smoking cessation guidelines has been mandated in the US Department of Veterans Affairs (VA) since 1997, VA inpatient staff do not generally receive cessation resources, education, performance feedback, and adequate support from management in the area of cessation counseling,5 as recommended by the US Public Health Service (USPHS) Clinical Practice Guideline (2008 update).6 The ongoing trend toward shorter hospital length of stay,7 coupled with acute medical illness and the psychological stress of hospitalization, present challenges to providing cessation counseling to inpatients. Discontinuity between the hospital and outpatient setting also complicates the implementation of effective treatment.
One strategy to reduce gaps in inpatient cessation counseling is to engage inpatient nurses in brief cessation counseling and referral. The USPHS guideline, which has been adopted by the VA,8 recommends that nurses use the 5A’s framework (Ask, Advise, Assess, Assist, Arrange).6 Several controlled trials have shown that nurse-delivered counseling increases quit rates in hospitalized patients.9 Moreover, acute care nurses can efficiently refer patients to outpatient telephone counseling.10
Attitudes are a significant determinant of behavioral intentions, which in turn have been shown to predict practice behavior of health professionals.11 As part of a larger effectiveness trial of smoking cessation guidelines in hospitalized veterans, the objectives of this study are to determine the impact of guideline implementation on: 1) nurses’ attitudes toward and self-efficacy for providing smoking cessation counseling, and 2) nurses’ delivery of the 5A’s using quantitative survey methods. To better understand attitudes and particular change mechanisms at the study hospital, a secondary aim of this study is to explore barriers and facilitators to implementation of smoking cessation guidelines in the VA inpatient setting using qualitative methods. Unlike most prior studies, the current study relies on staff nurses (rather than research personnel) to initiate and deliver brief cessation counseling at the bedside.
METHODS
Study Design
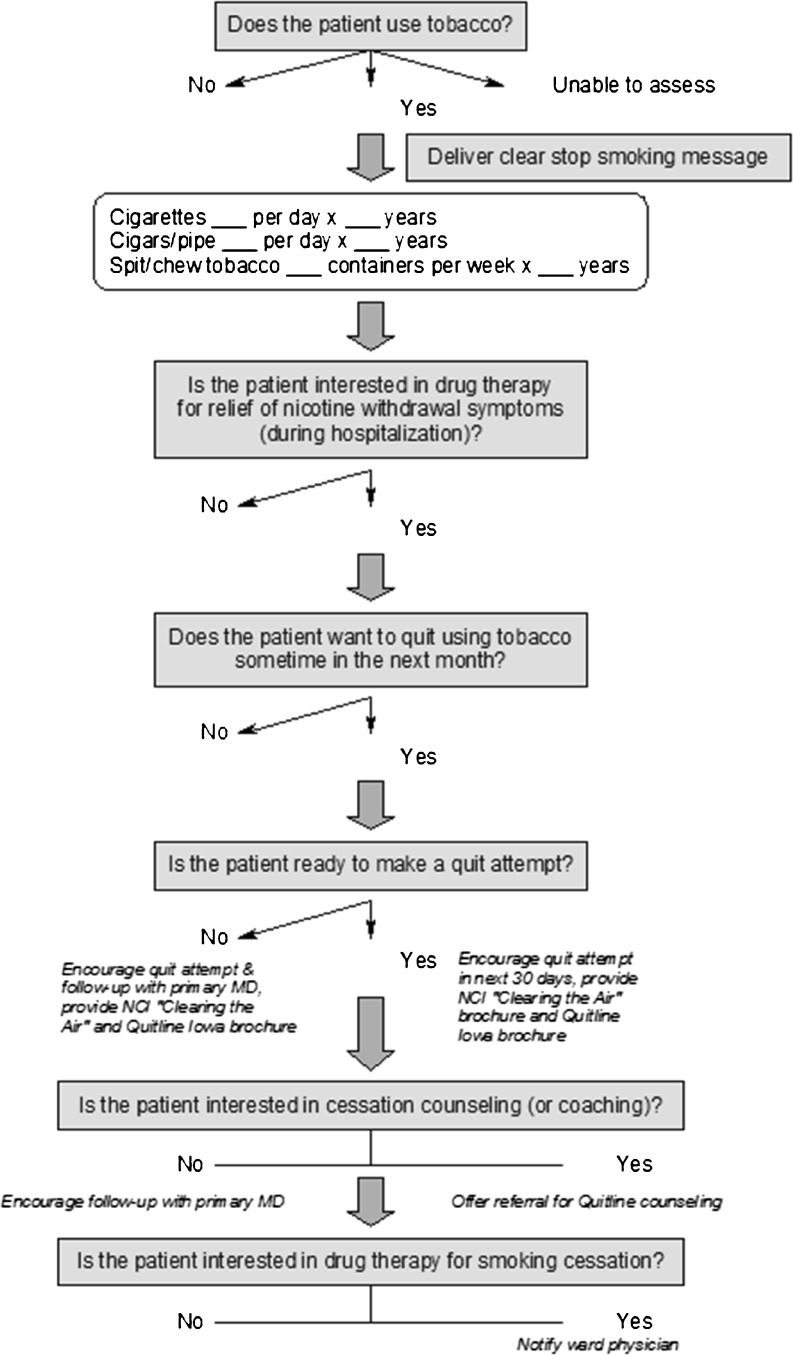
We conducted a quasi-experimental before-after trial in smokers who were hospitalized on two general medicine units of a single University-affiliated VA hospital, in preparation for broader guideline implementation in a multi-center trial. During the 7-month baseline period of patient enrollment, nursing staff were provided with general information on the rationale for the current study, but did not receive any specific training or additional resources for implementing the 5A’s algorithm on the inpatient medical units. Subsequently, the smoking cessation intervention was adapted for the study hospital, and inpatient staff were trained on use of the 5A’s algorithm during a 4.5 month implementation period (Fig. 1). A new cohort of study patients was enrolled over the subsequent 8-month post-intervention period (Fig. 2).
Figure 1.
VA-BEST smoking cessation algorithm (5A’s).
Figure 2.
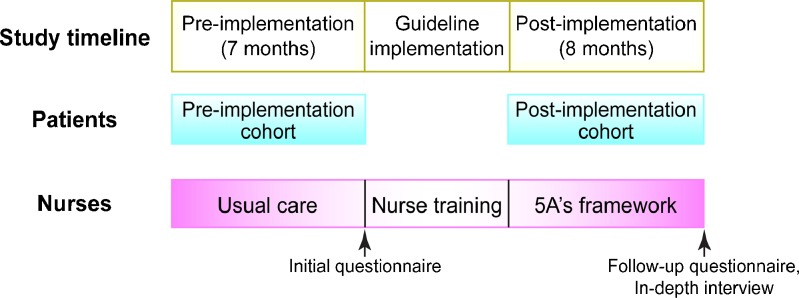
Schematic of study design.
Study Site
The Iowa City VA Health Care System provides tertiary care to patients from the entire state of Iowa and western Illinois; annual volume of admissions to the medicine units is approximately 3,000. At the time of this study, the medicine units at the Iowa City VA Hospital were staffed by 40 staff nurses. Internal medicine residents from the University of Iowa rotate through the medicine service in 3-week blocks. Ward nurses work closely with resident physicians by obtaining orders for smoking cessation medication (such as nicotine replacement therapy, NRT). A hospital pharmacist was responsible for dispensing smoking cessation medications and educating inpatients on their appropriate use at discharge. This project was approved by the Iowa City VA Health Care System’s Institutional Review Board.
Patients
Adult patients (age ≥ 18 years) who smoked at least one cigarette per day on average over the past 7 days (regardless of their willingness to quit smoking) and who were hospitalized on a medicine inpatient unit for at least 18 h were eligible; a complete list of exclusion criteria has been previously reported.12
Guideline Implementation
Based on the Chronic Care Model,13 the implementation plan included the following components that have been used successfully in prior translational research studies: academic detailing of staff nurses, adaptation of the clinical information system, patient self-management, and organizational support and feedback, as previously described.12 We describe how each component was implemented below:
Enhanced academic detailing with staff nurses. Academic detailing is a form of educational outreach that employs two-way interactions with clinical staff to encourage adoption of a desired practice pattern.14,15 In this trial, we used enhanced academic detailing (face-to-face training, performance feedback, and periodic check-ins with both nurse managers and peer leaders) to promote use of the 5A’s framework; this approach has been used successfully in primary care to support practice change in the delivery of cessation counseling.16 Specifically, we provided personalized, on-site instruction for one or two nurses at a time during their assigned shift. Because of multiple competing demands on their time, nurses were instructed to perform the 5A’s within 5 min at the time of hospital admission (or as soon as the patient’s acute medical condition had stabilized), and were shown how to use charting and referral tools for cessation counseling in the VA Computerized Patient Record System (CPRS). Each face-to-face training session lasted approximately 25–30 min, and was supplemented by a 30 min online tutorial and post-test. To increase awareness of the 5A’s intervention, posters were displayed in each nursing break room. In addition, members of the research team periodically circulated on the medicine units to answer questions, to provide support, and to distribute pens and note pads with the study logo to nursing staff. Group feedback on use of the 5A’s was presented during nurse training and periodically throughout the post-implementation period.
Adaptation of the computerized information system. A member of the research team worked with the Clinical Applications Coordinator at the study hospital to modify the nursing admission database to include pertinent questions about smoking. The modified database prompted nurses to assess patients’ willingness to quit, provided links to patient education materials, and reminded nurses to offer a Quitline referral to those who were ready to quit. To facilitate prescribing of VA-approved pharmacotherapy by ward physicians, computerized “quick orders” for these medications (with prefilled dose, duration, and patient instructions) were created. Resident physicians were trained to use these quick orders and to reinforce the nurse’s advice to quit.
Patient self-management support. The strategy for patient self-management included brief bedside counseling, pharmacotherapy, and proactive telephone counseling starting within 72 h after hospital discharge. Specifically, nurses were instructed to provide all smokers with self-help materials (‘Clearing the Air: Quit Smoking Today’17 and Quitline brochure), to offer to show patients a motivational smoking cessation video developed by the study team for veterans on closed-circuit TV, to offer medication for relief of nicotine withdrawal symptoms (and long-term abstinence), and to refer those who were ready to make a quit attempt to the state Quitline (operated by National Jewish Hospital, Denver, CO, at the time of this study). Quitline referral required completion of a separate form (which could be completed in CPRS). A member of the research team faxed completed referral forms to the Quitline prior to discharge and kept track of all fax referrals to the Quitline.
Organizational support and feedback. At the outset of this study, the principal investigator met with the study hospital’s Clinical Executive Board and nurse’s union representative to explain the purpose of the study and the components of the intervention. On each ward, the nurse manager designated a peer leader to serve as a liaison between the study team and nurses (e.g., helping to facilitate scheduling of training and feedback sessions), to provide point of care coaching on use of the 5A’s, to suggest improvements to the implementation strategy, and to help with troubleshooting. The peer leaders were well-respected VA nurses who had 3 years of nursing experience on average. They received additional training in brief cessation counseling during a 1-h workshop that included role play and feedback from a standardized patient.18
Data Collection
Patient Survey
Every adult inpatient on the medicine units was screened for eligibility by medical record review. After obtaining informed consent, the study research assistant (RA) administered a survey to current smokers to obtain more detailed information on smoking history, smoking-related medical comorbidities,19 health beliefs related to smoking, level of tobacco addiction,20 and nicotine withdrawal symptoms.21–23 We assessed the patient’s readiness to quit smoking using the Contemplation Ladder, an 11-point instrument designed to assess a smoker’s readiness to quit on a continuum ranging from having no thoughts about quitting to being actively engaged in quitting (range 0–10).24
To determine whether or not the hospital staff had performed the 5A’s during the hospital stay, the RA interviewed study patients just prior to hospital discharge (46 %); study patients who were discharged while the RA was off-duty were interviewed by telephone within 48 h after discharge (54 %). There was no significant difference in delivery of the 5A’s for those patients who were interviewed pre-discharge versus post-discharge. As it was not possible to blind the RA to the period of the study (pre-implementation versus post-implementation), the RA was trained to administer the 5A’s survey verbatim. Using a modified version of the index described by Berndt et al.,25 we calculated a 5A’s composite score for each patient (ranging from 0–9), based on the sum of nine recommended actions (each of which was scored as 0 or 1).
Nurse Survey
We administered a written pre-implementation and post-implementation survey to staff nurses who provided direct patient care on the internal medicine units (“float” nurses and nursing assistants were excluded). The questionnaire included a 20-item decisional balance scale, which includes ten items that reflect positive attitudes (Pros) and ten items that reflect negative attitudes (Cons) toward the delivery of smoking cessation assistance.26 The questionnaire also included two items that asked nurses to rate their self-efficacy and satisfaction in helping patients to stop smoking on a 4-point and 5-point Likert-type scale, respectively.27 Based on the transtheoretical model of change, decisional balance and self-efficacy are key constructs that predict transitions across the stages of change.26
Summative Evaluation
To better understand attitudes and particular change mechanisms at the study hospital, semi-structured one-on-one interviews were conducted with eight staff nurses at the end of the post-implementation period. We used purposeful sampling to target nurses with different attitudes regarding cessation counseling, based on their responses to the decisional balance questionnaire prior to implementation. Specifically, we interviewed a convenience sample of nurses from each of four possible decisional balance subgroups (i.e., high “pros” and low “cons”, high “pros” and high “cons”, low “pros” and low “cons”, and low “pros” and high “cons”). Interviews with staff nurses were conducted on-site in a private room and lasted an average of 20 min (range 10–38 min). The interviewer asked staff nurses to identify barriers and facilitators to changing smoking cessation practices and explored their thoughts about the usefulness of the intervention. All interviews were tape recorded, transcribed, reviewed by the interviewer for completeness and accuracy, and imported into MAXQDA 10 (Berlin-Marburg-Amoneburg, Germany), a qualitative data management and analysis software program.
Data Analysis
Statistical Analysis
Pre-implementation and post-implementation groups were compared with respect to potential confounding variables using the two-independent-sample t-test, Wilcoxon rank-sum, or chi-squared tests as appropriate. We compared nurses’ attitudes toward smoking cessation counseling pre-implementation and post-implementation using the paired t-test for the two decisional balance subscales and the signed rank test for the self-efficacy and role satisfaction items. We used logistic regression to compare performance of individual A’s across the two periods and adjusted for those covariates that differed significantly between the pre-intervention and post-intervention cohorts in bivariate analysis (p ≤ 0.05). Similarly, we used linear regression to compare the 5A’s composite score across the two periods. To check for secular trend, we used linear regression to analyze the 5A’s composite score as a function of month of enrollment during the pre-intervention period. Specification of the regression function and the assumption of homoscedasticity of errors were checked by examining plots of the residuals versus predicted values.28
We used PROC GENMOD in SAS for Windows, Version 9.3 (SAS Institute, Cary, NC) and R programming language for all analyses. All models were estimated using generalized estimating equations (GEE) to account for clustering of performance measures at the nurse level.29 All tests were two-sided and a p value of ≤ 0.05 was defined as statistically significant; we did not adjust for multiple comparisons.
Qualitative Analysis
We used thematic content analysis to inductively characterize the issues raised by nurses and to construct a provisional coding structure that was then tested using a subset of transcripts.30 Each set of transcripts was coded by two independent coders and assessed for inter-rater agreement at two intervals. During the first interval, inter-rater agreement for all themes was less than 80 %;31 thus, all discrepancies in these interviews were discussed until a consensus between coders was reached. Subsequently, inter-rater agreement during the second interval was 100 %. Using a process known as constant comparison, codes were compared to identify areas of overlap in the coded segments.32 Related codes were initially grouped under the following overarching themes: impact of the intervention, application of 5A’s, and barriers to implementation. The coding structure was revised iteratively as new themes emerged. Descriptive statements about each domain (using the subjects’ words) were identified.
RESULTS
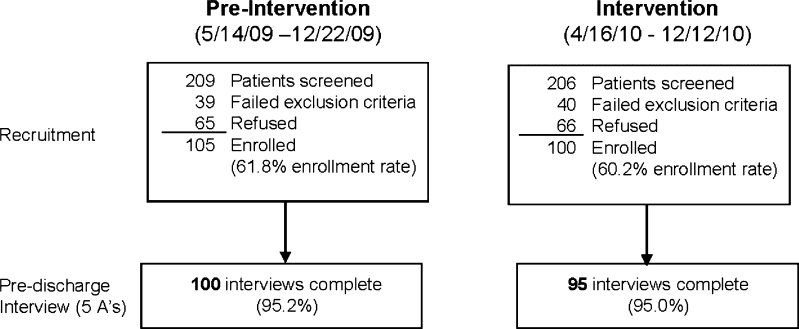
Patient Characteristics
During the pre-implementation and post-implementation periods, 62 % and 60 % of eligible patients agreed to participate, respectively (Fig. 3). Participants were younger than non-participants (59.0 and 62.1, respectively, p = 0.004); otherwise there were no significant differences between those who agreed to participate (N = 205) and those who did not (N = 131). Compared to the pre-implementation period, patients enrolled during the post-implementation period were more likely to rate their health as excellent or very good and had made fewer quit attempts, but all other variables were similar (Table 1).
Figure 3.
Patient enrollment and follow-up in the pre-implementation and post-implementation periods.
Table 1.
Characteristics of Study Patients
| Variable | Pre-intervention (n = 105) | Intervention (n = 100) |
|---|---|---|
| Age, mean (sd) | 58.9 (8.7) | 59.3 (10.3) |
| Gender, % male | 97 | 98 |
| Race, % nonwhite | 9 | 3 |
| Highest grade, median (IQR) | 12 (12–14) | 12 (12–14) |
| Marital status, % married or living with companion | 42 | 40 |
| Self-rated health, % excellent-very good | 13 | 29* |
| Alcohol use in past 3 months, % | 51 | 47 |
| Admission diagnoses, % | ||
| Cardiovascular system | 31 | 30 |
| Respiratory system | 13 | 15 |
| Digestive system | 8 | 12 |
| Endocrine and metabolic diseases | 6 | 5 |
| Neuropsychiatric disorders | 6 | 7 |
| Miscellaneous† | 36 | 31 |
| Smoking-related variables | ||
| Cigarettes per day, median (IQR) | 20 (10–20) | 20 (10–20) |
| Nicotine dependence (FTND), median (IQR) | 4 (3–6) | 5 (3–6) |
| Minnesota Nicotine Withdrawal Scale, median (IQR)‡ | 12 (6–16.5) | 10 (4–16) |
| Any smoking-related medical problem, %§ | 75 | 75 |
| Do you believe that you currently have a smoking-related medical problem? (% yes) | 46 | 46 |
| Do you believe that quitting smoking would improve your health? (% at least “somewhat”) | 72 | 78 |
| Prior quit attempts (≥ 1 full day), median (IQR)** | 5 (1–12) | 3 (1–7)* |
| Contemplation ladder (0–10), mean (sd) | 7 (5–10) | 8 (5–10) |
| Have you smoked any cigarettes while in hospital? (% yes) | 31 | 26 |
| Likelihood of staying off cigarettes after hospital discharge†† | 36 | 48 |
sd standard deviation, IQR interquartile range, FTND Fagerstrom Test of Nicotine Dependence
* p ≤ 0.05
†“Miscellaneous” includes abnormal clinical/laboratory findings and neoplastic, musculoskeletal, dermatologic, genitourinary, or infectious conditions,
‡Patients were asked to rate each of nine withdrawal symptoms over the past 24 h on a 5-point ordinal scale (range of total score 0–36).
§Based on the US Surgeon General’s 2004 Report, the following conditions are considered smoking-related: coronary heart disease, congestive heart failure, stroke or transient ischemic attack, chronic obstructive lung disease, peripheral vascular disease, tobacco-related cancer (e.g., lung, oral cavity).
**Patients who reported not having made any quit attempts were assigned a value of zero.
††Percent reporting at least “Somewhat likely” (based on 5-point Likert scale)
Performance of 5A’s
Overall, performance of the 5A’s was significantly greater during the post-implementation period (3.9 vs. 3.1 on the 5A’s composite score, adjusted difference 1.0, 95 % CI = 0.5, 1.6)(Table 2). Although the proportion of study patients who were asked about smoking was similar in both periods, patients were more likely to be advised to quit (adjusted OR = 2.1, 95 % CI = 1.2, 3.5) and to receive assistance in quitting (adjusted OR = 2.9, 95 % CI = 1.6, 5.3) during the post-implementation period. Assistance in quitting was largely comprised of providing self-help material; relatively few patients (11 %) had discussed a plan for quitting after hospital discharge and only 7 % of post-intervention patients accepted a Quitline referral. Although post-intervention patients were somewhat more likely to have been offered NRT to relieve withdrawal symptoms, the proportion of patients who actually received NRT was similar during the pre-intervention and post-intervention periods (31 vs. 29 %, p = 0.71).
Table 2.
Proportion of Interviewees Who Received Recommended Counseling Activities from an Inpatient Nurse (During the Pre-Implementation and Intervention Periods)
| Received inpatient nurse counseling, % (N)† | |||
|---|---|---|---|
| Pre-implementation | Post-implementation | Adjusted OR (95 % CI) | |
| Ask about smoking | 86 (93) | 91 (89) | 1.5 (0.6, 3.9) |
| Advise to quit | 48 (94) | 62 (87) | 2.1 (1.2, 3.5)* |
| Assess willingness to quit | 66 (94) | 75 (85) | 1.8 (0.9, 3.8) |
| Assist in quitting | 45 (93) | 70 (87) | 2.9 (1.6, 5.3)* |
| Given self-help literature or offered to show video | 17 (100) | 40 (93) | 3.5 (1.8, 6.6)* |
| Discuss a plan for quitting after hospital discharge | 15 (95) | 11 (88) | 0.8 (0.4, 1.5) |
| Offer nicotine patches to relieve withdrawal symptoms during hospitalization | 33 (93) | 45 (85) | 1.7 (0.95, 3.1) |
| Discuss pharmacotherapy to help you quit | 26 (99) | 35 (92) | 1.8 (0.9, 3.5) |
| Arrange follow-up | 20 (99) | 29 (91) | 1.7 (0.96, 3.0) |
| Arrange quitline referral or recommend PCP follow-up to discuss smoking cessation | 13 (100) | 18 (93) | 1.6 (0.7, 3.4) |
| Arrange for inpatient smoking cessation consult to provide intensive counseling | 3 (94) | 1 (90) | 0.3 (0.1, 1.6) |
| Adjusted difference (95 % CI) | |||
| 5A’s summary score, mean (sd)[N]‡ | 3.1 (2.1) [72] | 3.9 (2.0) [69] | 1.0 (0.5, 1.6)* |
* p < 0.05
†The number of patients who provided evaluable data for each survey item is shown in parentheses
‡Index score ranged from 0 to 9 for level of adherence with the 5A’s. The adjusted difference between periods is based on linear regression using generalized estimating equations
Staff nurse characteristics and survey results
Table 3 shows the characteristics of staff nurses in this study: approximately 21 % were current smokers. Thirty-eight nurses (95 %) completed face-to-face training and 53 % viewed the online tutorial and/or post-test during the intervention period. Following implementation of the intervention, nurses had higher scores on the “pros” subscale of the decisional balance questionnaire (35.3 vs. 32.7, p = .008); there was no significant change on the “cons” subscale. Staff nurses also tended to rate themselves as moderately or very effective in cessation counseling after guideline implementation (38 vs. 21 %), although this difference was not statistically significant (Table 4). Patients of smoking nurses were no less likely to receive cessation counseling than those of non-smoking nurses (5A’s composite score: 3.65 vs. 3.62, p = 0.95).
Table 3.
Descriptive Characteristics of the Inpatient Nurses
| Characteristic | Inpatient nurses (N = 40) |
|---|---|
| Age, mean (sd) | 43.6 (11.5) |
| Gender, % male | 30 |
| RN or advanced nurse training, %* | 84 |
| Experience as hospital nurse (years), median (IQR) | 5 (3–14) |
| Experience on current unit (years), median (IQR) | 2.5 (1.5–6) |
| Smoking status, % current smoker | 21 |
*Includes RN diploma, Bachelors (BSN), Masters (MSN), or Doctor of Nursing (PhD) degree
Table 4.
Inpatient Nurses’ Attitudes Toward Smoking Cessation Counseling Before and After Guideline Implementation*
| Clinician variable | Pre-implementation | Post-implementation | p value (N)† |
|---|---|---|---|
| Decisional balance – “pros” subscale, mean (sd) | 32.7 (7.2) | 35.3 (7.7) | 0.008 (26) |
| Decisional balance – “cons” subscale, mean (sd) | 28.0 (7.5) | 26.5 (8.3) | 0.24 (29) |
| Self-efficacy in counseling, % moderately-very effective§ | 21 | 38 | 0.23 (29) |
| Satisfaction with counseling role, % satisfied** | 34 | 52 | 0.39 (29) |
*The Pros and Cons scales have high internal consistency (Cronbach’s alpha = 0.83, 0.86, respectively); validity was supported by finding significantly higher Pros scores and lower Cons scores for those clinicians who offered assistance to all patients who smoked [Park, 2001]. Analyses were based on those nurses who completed both pre-implementation and post-implementation surveys. Data were missing for those clinicians who were no longer employed at the study sites at the time of the pre-intervention and post-intervention surveys, who were employed as “floating” (or locum tenens) staff and did not attend project meetings, or who refused to complete either survey
†Comparisons are based on the signed rank test for ordinal variables (self-efficacy in counseling, satisfaction with counseling role) and the paired t-test for continuous variables (decisional balance subscales)
§4-point scale: Very effective = 3, Moderately effectively = 2, Slightly effective = 1, Ineffective = 0
**5-point scale: Very satisfied = 2, Satisfied = 1, Neutral = 0, Somewhat dissatisfied = −1, Very dissatisfied = −2
Summative Evaluation
Nurses’ perceptions about Veterans’ willingness to quit may have attenuated the effect of guideline implementation, as illustrated by the following:
[The intervention] just confirmed my belief that you can’t make someone stop if they don’t want to unless they’re really, really ready to. I have guys come here that, I mean, they’re just about on death’s door. 'I’ve been smokin’ for 62 years, and I’m not quittin’ now. I’ll have a cigarette in my coffin’ and stuff like that, but … No one should smoke, but people do, and I don’t think me tellin’ ‘em what their options are [will help], especially when they first come in.
Although several nurses expressed doubts about whether they could overcome patients’ resistance to quitting, they confirmed that the intervention provided them with tools to help those who were interested in smoking cessation. Specifically, nurses reported that the modified admission database, patient education brochures, and quick orders for smoking cessation pharmacotherapy provided them with an efficient mechanism for implementing the 5A’s. As one nurse explained, “I always give ‘em the brochures. I just think it’s something they can take home and at least look at if they need to.”
On the other hand, some nurses acknowledged difficulty in delivering the 5A’s on account of rapid patient turnover and competing demands on their time. For example, one nurse explained:
Um, someone could say they wanted to quit smoking within the next month, and you know they’d be gone the next day, or we get uh, busy, and you know it wasn’t done. The referral wasn’t put in or it just slipped through the cracks…
Nurses also reported difficulty in completing the Quitline referral despite efforts of the study team to simplify the referral process. One nurse recalled:
I wasn’t able to do [a Quitline referral] very often. The biggest part of that is that it was actually a patient who wanted to stop smoking, so, we actually wrote out the note, and the Quitline stuff, filled it out, and for a while they were filling it out wrong, I guess. We got a note from our boss showing us the right website to use and blah, blah, blah, and I would have to write a separate note in order to fill it out correctly.
In spite of these barriers, interview data confirmed the observed increases in performance of the 5A’s during the post-implementation period, as demonstrated by the quantitative data. We also observed statistically significant increases in nurses’ responses to the following DBQ items: “Nurses can be effective in helping their patients stop smoking” (perceived effectiveness), and “Patients expect me to counsel them about smoking” (perceived practice norms). Nurses responded that they would likely continue to use the 5A’s, “because it’s in our field [CPRS] now.” Another nurse explained:
[The intervention] added to my knowledge of what’s available. Other than making sure we follow through and do [the 5A’s], which, probably in the past we weren’t as forthcoming on, you know, if someone was a smoker, we didn’t go through the whole thing of trying this and that.
DISCUSSION
The recent Joint Commission on Accreditation of Healthcare Organizations (JCAHO) performance measure for smoking cessation requires hospitals to provide inpatient smokers with evidence-based cessation counseling, drug therapy, and post-discharge referral for further cessation counseling.33 Results of the current study demonstrate the effectiveness of a multimodality approach that includes enhanced academic detailing, adaptation of the electronic medical record, and peer leadership in improving the quality of smoking cessation services for medical inpatients (above and beyond ‘ask’ and ‘advise’ performance measures).33,34
Of the 5A’s, we observed the largest gains in advising patients to stop smoking and in providing assistance in quitting. Offering tailored advice to quit requires skill and self-confidence, and was an area of emphasis during nurse training. Our results suggest that ward nurses overcame their reluctance to advise patients to quit35 and expressed an increased comfort level with inpatient smoking cessation counseling when provided with stage-specific patient education materials, CPRS prompts, and education about the 5A’s. Overall, nurses showed a more positive attitude toward 5A’s counseling following guideline implementation. Similar results were found after a training intervention in home health nurses, who showed improved performance of the 5A’s and greater likelihood of providing cessation counseling to all smokers, regardless of motivation to quit.36
There was not, however, a statistically significant increase in referral of study patients to the Quitline, an evidence-based long-term cessation strategy.37 Possible explanations for this finding are: 1) nurses’ skepticism and lack of familiarity with the Quitline, despite training, to convincingly recommend its services to veterans; 2) inability to fully integrate the Quitline referral into the nurse’s workflow in CPRS; and 3) the reluctance of many patients (especially elderly veterans) to opt for telephone coaching during the process of quitting. In one recent online survey of smokers, only 11 % of respondents indicated any interest in Quitline counseling; older smokers tended to prefer nonsocial-informational methods, such as informational booklets.38 For many nurses, the perceived value and outcome expectancies of cessation counseling were low on account of the patient population. Many patients, especially the elderly, tend to have a fatalistic attitude toward smoking cessation and express doubts about the benefits of quitting,39,40 which may have contributed to the ambivalence of some VA nurses toward cessation counseling.
Our results are similar to those of Duffy et al., who demonstrated significant improvements in the provision of smoking cessation medication following a multimodality intervention (computerized template for nurse documentation, patient education materials, follow-up telephone counseling by VA volunteers, feedback, opinion leaders) on the general medicine units of two VA hospitals.41 In an quasi-experimental, non-equivalent control group trial, Freund et al. also demonstrated significant improvements in patient-reported provision of NRT and written resources following a hospital-wide multi-component intervention that included training of inpatient staff, local consensus and guideline adaptation, reminders, and monitoring and feedback.42 Neither of the above studies significantly increased the proportion of patients who received post-discharge support (e.g., telephone counseling) at intervention sites.
Limitations of this study deserve comment. First, pre–post changes in outcome may be attributable to Hawthorne effects, ‘history’ (the influence of events during the study that affect the study outcomes), or ‘maturation’ (the change of staff performance during the study related to the evolution of clinical skills).43 Potential Hawthorne effects were minimized by employing a sufficiently long post-implementation period (8 months). There was no significant secular trend in the performance of smoking cessation counseling during the pre-implementation period (based on the 5A’s composite score); in addition, there were no new policies or concurrent quality improvement directives that might explain the observed improvements in performance of the 5A’s at the study hospital. Second, data on delivery of the 5A’s were based on patient self-report. Although direct observation of patient encounters is often considered the “gold standard,” patient recall has been shown to be reasonably accurate in clinical practice.44 Third, nursing staff were not required to demonstrate their knowledge of or skill in cessation counseling; although we asked patients to indicate whether they received the 5A’s, we did not directly rate the quality of the nurses’ counseling. Finally, it is not clear whether the intervention would have been as effective in a non-teaching hospital that had less interest in smoking cessation or less support from hospital leadership.
In conclusion, this study demonstrates the effectiveness of a multifaceted guideline implementation strategy that includes enhanced academic detailing, adaptation of the nursing admission form, performance feedback, and ready access to patient education materials in improving the delivery of smoking cessation treatment to unselected hospitalized smokers. Use of a nurse-initiated strategy is consistent with expert recommendations for nurses to play a larger role in delivering smoking cessation counseling in the inpatient setting.45 Lessons from this preliminary investigation have informed efforts to adapt the intervention at subsequent study sites, and highlight the importance of building inpatient nurses’ brief counseling skills, integrating the 5A’s into nursing work flow, and making it easier to refer patients to VA or community-based resources for smoking cessation (such as state quitlines). Using this approach will enable health care professionals to treat tobacco dependence with the same level of coordination and thoroughness as other chronic conditions, such as hypertension and diabetes. Finally, counseling efforts by inpatient staff and community partners should be transparent in the electronic medical record in order for the primary care team to treat tobacco dependence effectively over the care continuum.
Acknowledgements
The authors thank those who provided research assistance throughout the study: Margaret Graham, MS; Justin McDonald, MHA; George Bailey, MS, for assisting with database design, and Erin Greve for assisting with data entry. We are especially grateful for the assistance of the nurse facilitators and managers who served as liaisons to the study team: Michael Sellz, RN; Maureen Drexler, RN; Nathan Mehaffy, RN; Susan Linnell, RN; Julie Gerard, RN. We also thank Bonnie Bootsmiller, PhD for administrative support and Megan Watson for assistance with manuscript preparation.
Disclaimer
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Funding/Support
Veterans Affairs Health Services Research and Development (IIR 07–113)
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults-United States, 2006. MMWR Morb Mortal Wkly Rep. 2007;56(44):1157–1161. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. The health benefits of smoking cessation: A report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health. DHHS Publication No. (CDC) 90–8416;1990. DHHS Publication No. (CDC) 90–8416.
- 3.McBride C, Emmons K, Lipkus I. Understanding the potential of teachable moments: The case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 4.Orleans CT, Kristeller JL, Gritz ER. Helping hospitalized smokers quit: New directions for treatment and research. J Consult Clin Psychol. 1993;61(5):778–789. doi: 10.1037/0022-006X.61.5.778. [DOI] [PubMed] [Google Scholar]
- 5.Duffy SA, Reeves P, Hermann C, Karvonen C, Smith P. In-hospital smoking cessation programs: What do VA patients and staff want and need? Appl Nurs Res. 2008;21(4):199–206. doi: 10.1016/j.apnr.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Fiore M, Bailey W, Cohen S, et al. Treating tobacco use and dependence. Clinical Practice Guideline. Rockville: US Department of Health and Human Services, US Public Health Service; 2008. [Google Scholar]
- 7.Ashton CM, Souchek J, Petersen NJ, et al. Hospital use and survival among Veterans Affairs beneficiaries. N Engl J Med. 2003;349(17):1637–1646. doi: 10.1056/NEJMsa003299. [DOI] [PubMed] [Google Scholar]
- 8.VA/DoD Evidence Based Practice Working Group. Management of tobacco use (MTU). 2008; http://www.healthquality.va.gov/Management_of_Tobacco_Use_MTU.asp. Accessed 4/1/2013.
- 9.France EK, Glasgow RE, Marcus AC. Smoking cessation interventions among hospitalized patients: What have we learned? Prev Med. 2001;32:376–388. doi: 10.1006/pmed.2000.0824. [DOI] [PubMed] [Google Scholar]
- 10.Katz DA, Vander Weg M, Holman J, et al. The Emergency Department Action in Smoking Cessation (EDASC) trial: Impact on delivery of smoking cessation counseling. Acad Emerg Med. 2012;19(4):409–420. doi: 10.1111/j.1553-2712.2012.01331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals’ intentions and behaviours: A systematic review of studies based on social cognitive theories. Implement Sci. 2008;3:36. doi: 10.1186/1748-5908-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz DA, Vander Weg M, Fu S, et al. A before-after implementation trial of smoking cessation guidelines in hospitalized veterans ( NCT00816036): Study protocol. Implement Sci. 2009;4:58. doi: 10.1186/1748-5908-4-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. doi: 10.2307/3350391. [DOI] [PubMed] [Google Scholar]
- 14.Soumerai S, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263(4):549–556. doi: 10.1001/jama.1990.03440040088034. [DOI] [PubMed] [Google Scholar]
- 15.Lafata JE, Gunter MJ, Hsu J, et al. Academic detailing to improve laboratory testing among outpatient medication users. Med Care. 2007;45(10):966–972. doi: 10.1097/MLR.0b013e3180546856. [DOI] [PubMed] [Google Scholar]
- 16.Sheffer M, Baker T, Fraser D, Adsit R, McAfee T, Fiore M. Fax referrals, academic detailing, and tobacco quitline use: a randomized trial. Am J Prev Med. 2012;42(1):21–28. doi: 10.1016/j.amepre.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 17.National Cancer Institute. Clearing the Air: Quit Smoking Today. . 2008; http://www.smokefree.gov/pubs/Clearing-The-Air_acc.pdf. Accessed 4/1/2013.
- 18.Papadakis MA, Croughan-Minihane M, Fromm LJ, Wilkie HA, Ernster VL. A comparison of two methods to teach smoking-cessation techniques to medical students. Acad Med. 1997;72(8):725–727. doi: 10.1097/00001888-199708000-00021. [DOI] [PubMed] [Google Scholar]
- 19.The health consequences of smoking: a report of the surgeon general. Rockville: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2004. [Google Scholar]
- 20.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 21.Hughes JR. Background on the Minnesota Withdrawal Scale-Revised (MNWS-R). 2012; http://www.uvm.edu/~hbpl/minnesota/minnesota/2012/Background_8_2012.pdf, Accessed 4/1/2013.
- 22.Sood A, Ebbert JO, Prasad K, Croghan IT, Bauer B, Schroeder DR. A randomized clinical trial of St. John’s wort for smoking cessation. J Altern Complement Med. 2010;16(7):761–767. doi: 10.1089/acm.2009.0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine Tob Res. 2007;9(3):315–327. doi: 10.1080/14622200701188919. [DOI] [PubMed] [Google Scholar]
- 24.Biener L, Abrams D. The contemplation ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10(5):360–365. doi: 10.1037/0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- 25.Berndt N, Bolman C, de Vries H, Segaar D, van Boven I, Lechner L. Smoking cessation treatment practices: recommendations for improved adoption on cardiology wards. J Cardiovasc Nurs. 2013;28(1):35–47. doi: 10.1097/JCN.0b013e318231f424. [DOI] [PubMed] [Google Scholar]
- 26.Park E, Eaton CA, Goldstein MG, et al. The development of a decisional balance measure of physician smoking cessation interventions. Prev Med. 2001;33:261–267. doi: 10.1006/pmed.2001.0879. [DOI] [PubMed] [Google Scholar]
- 27.Katz D, Muehlenbruch D, Brown R, Fiore M, Baker T. Effectiveness of implementing the Agency for Healthcare Research and Quality Smoking Cessation Clinical Practice Guideline: A randomized controlled trial. J Nat Cancer Inst. 2004;96:594–603. doi: 10.1093/jnci/djh103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neter J, Kutner M, Nachtsheim C, Wasserman W. Applied linear statistical models. 4. Homewood: Irwin; 1996. [Google Scholar]
- 29.Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- 30.Bernard H, Ryan G. Analyzing qualitative data: Systematic approaches. Thousand Oaks: Sage Publications; 2010. [Google Scholar]
- 31.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Newbury Park: Sage Publications; 1994. [Google Scholar]
- 32.Pope C, Ziebland S, Mays N. Qualitative research in health care: Analyzing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fiore MC, Goplerud E, Schroeder SA. The Joint Commission’s new tobacco-cessation measures–will hospitals do the right thing? N Engl J Med. 2012;366(13):1172–1174. doi: 10.1056/NEJMp1115176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dawood N, Vaccarino V, Reid KJ, et al. Predictors of smoking cessation after a myocardial infarction: The role of institutional smoking cessation programs in improving success. Arch Intern Med. 2008;168(18):1961–1967. doi: 10.1001/archinte.168.18.1961. [DOI] [PubMed] [Google Scholar]
- 35.McCarty M, Hennrikus D, Lando H, Vessey J. Nurses’ attitudes concerning the delivery of brief cessation advice to hospitalized smokers. Prev Med. 2001;33:674–681. doi: 10.1006/pmed.2001.0944. [DOI] [PubMed] [Google Scholar]
- 36.Borrelli B, Lee C, Novak S. Is provider training effective? Changes in attitude towards smoking cessation counseling behaviors of home health care nurses. Prev Med. 2008;46:358–363. doi: 10.1016/j.ypmed.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rigotti NA, Clair C, Munafo MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012;5:CD001837. doi: 10.1002/14651858.CD001837.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Westmaas JL, Abroms L, Bontemps-Jones J, Bauer JE, Bade J. Using the internet to understand smokers’ treatment preferences: informing strategies to increase demand. J Med Internet Res. 2011;13(3):e58. doi: 10.2196/jmir.1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rimer B, Orleans C, Fleisher L, et al. Does tailoring matter? The impact of a tailored guide on ratings and short-term smoking related outcomes for older smokers. Health Edu Res. 1994;9(1):69–84. doi: 10.1093/her/9.1.69. [DOI] [PubMed] [Google Scholar]
- 40.Donze J, Ruffieux C, Cornuz J. Determinants of smoking and cessation in older women. Age and Ageing. 2007;36:53–57. doi: 10.1093/ageing/afl120. [DOI] [PubMed] [Google Scholar]
- 41.Duffy SA, Karvonen-Gutierrez CA, Ewing LA, Smith PM. Veterans Integrated Services Network 11 Tobacco Tactics Team. Implementation of the Tobacco Tactics Program in the Department of Veterans Affairs. J Gen Intern Med. 2010;25(Suppl 1):3–10. doi: 10.1007/s11606-009-1075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freund M, Campbell E, Paul C, et al. Increasing hospital-wide delivery of smoking cessation care for nicotine-dependent in-patients: a multi-strategic intervention trial. Addiction. 2009;104(5):839–849. doi: 10.1111/j.1360-0443.2009.02520.x. [DOI] [PubMed] [Google Scholar]
- 43.Shadish W, Cook T, Campbell D. Experimental and quasi-experimental designs for generalized causal inference. Boston: Houghton Mifflin; 2002. [Google Scholar]
- 44.Ward J, Sanson-Fisher R. Accuracy of patient recall of opportunistic smoking cessation advice in general practice. Tob Control. 1996;5(2):110–113. doi: 10.1136/tc.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wewers M, Ahijevych K, Sarna L. Smoking cessation interventions in nursing practice. Nurs Clin North Am. 1998;33:61–74. [PubMed] [Google Scholar]