Abstract
Patient: Female, 36
Final Diagnosis: Pregnancy – placenta increta
Symptoms: —
Medication: —
Clinical Procedure: Cesarean hysterectomy
Specialty: Obstetrics and Gynecology
Objective:
Unusual clinical course
Background:
The generally accepted treatment for placenta percreta is cesarean hysterectomy without attempts to detach the placenta. Preoperative internal iliac artery balloon occlusion (IIABO) has been widely performed to minimize blood loss during cesarean hysterectomy for an abnormal attachment of the placenta. Our case is the first reported case of common iliac artery balloon occlusion (CIABO) being more effective than IIABO for reducing blood loss during a cesarean hysterectomy in the same patient.
Case Report:
We performed cesarean hysterectomy with IIABO in a 36-year-old Japanese female who had placenta percreta. However, there was still a large amount of blood loss. We immediately changed the balloon from the internal iliac artery to the common iliac artery, which visibly reduced the amount of blood loss. We finally achieved cesarean hysterectomy.
Conclusions:
CIABO was found to be more effective than IIABO for reducing blood loss during cesarean hysterectomy. Failure of IIABO can be explained by the presence of extensive anastomoses in the pelvic vasculature.
Keywords: balloon occlusion, internal iliac artery, common iliac artery, placenta percreta, cesarean hysterectomy
Background
The options for treating abnormal attachment of the placenta include both conservative and extirpative approaches. The most severe form of abnormal attachment of the placenta is placenta percreta, which indicates that the placenta has penetrated the entire uterine wall. The generally accepted treatment for placenta percreta is cesarean hysterectomy without attempts to detach the placenta. Preoperative internal iliac artery balloon occlusion (IIABO) has been widely performed to reduce the blood loss during cesarean hysterectomy to treat an abnormal attachment of the placenta [1–4].
We experienced a case in which we were unable to reduce the blood loss during cesarean hysterectomy in any way using pre-operative IIABO. We immediately transferred the balloon from the internal iliac artery to the common iliac artery, which visibly reduced the amount of blood loss.
Case Report
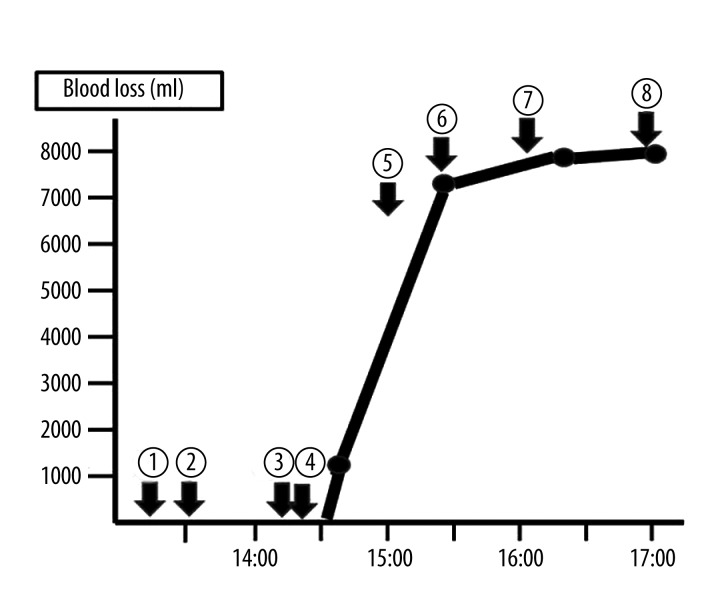
A 36-year-old, gravida 8, para 4, Japanese female, visited our hospital for amenorrhea and was found to be pregnant, at an estimated 16 weeks of gestation. The patient had undergone four previous cesarean sections. The first cesarean section was performed due to genital herpes, and the three subsequent surgeries were repeated cesarean sections. The patient had also undergone four artificial abortion. She had a history of smoking 10 cigarettes a day for 20 years. We diagnosed her current pregnancy as complete placenta previa at 23 weeks of gestation. Ultrasonography revealed the loss of the hypoechoic retroplacental zone, and the presence of multiple irregular placental lacunae (multiple dilated blood vessels) and increased vessels throughout the placenta. Cystoscopy revealed no infiltration of the placenta into the tunica mucosa vesicae urinariae. We diagnosed the pregnancy as placenta increta at 28 weeks of gestation. Elective cesarean hysterectomy with IIABO was planned to be performed at 35 weeks of gestation. We informed the patient and her family of all of the risks involved in the surgery. Prior to the surgery, bilateral ureteral stent-catheters were inserted by an urologist at our hospital. Preoperative occlusion balloons were placed in the bilateral internal iliac arteries by a radiologist at our hospital. Under general anesthesia, a transverse incision of the uterine fundus was made. A male baby was born with an Apgar score of 4/9 points, and weighed 2668g. The balloons in the bilateral internal iliac arteries were then inflated. We then sutured the uterine wound without detaching the placenta. When we started to perform the hysterectomy, a large amount of blood suddenly gushed in torrents from the vagina. We were unable control the bleeding with IIABO. A radiologist immediately deflated the two balloons in the internal iliac arteries. He transferred them to the bilateral common iliac arteries and inflated them. Following this, the bleeding decreased significantly. The transfer from IIABO to CIABO took 30 minutes, during which time, the amount of blood loss measured 5,910 ml (Figure 1). The hysterectomy was performed with a total blood loss of 7,720 ml. The bilateral common iliac arteries were occluded for a total of 62 minutes. The patient was transfused with a total of 1,200 ml of autologous blood, 10 units of packed red cell concentrate, and 10 units of packed fresh frozen plasma. The serum potassium level was 3.9 (3.5–4.8 mEq/l) after 120 min of CIABO. Severe acidosis was not observed. The placenta had completely penetrated the left side of the uterine wall and we diagnosed the pregnancy as placenta percreta (Figure 2). The patient’s postoperative course was uneventful. She was discharged from our hospital on the eighth postoperative day without any complications. Six months after the operation, both she and her infant remained healthy.
Figure 1.
Progress in the operation and blood losses. 1. The patient entered a operation room. 2. The preoperative occlusion balloons were placed in the bilateral internal iliac arteries by a radiologist. 3. We started the cesarean section. 4. 14:25 A male baby was born. The balloons in the bilateral internal iliac arteries were inflated, and we started the hysterectomy. 5. 15:00 A radiologist immediately transferred the balloon from the internal iliac artery to the common iliac artery. 6. 15:15 We restarted the hysterectomy. 7. We removed the uterus, and the balloons were deflated. 8. The operation finished.
Figure 2.
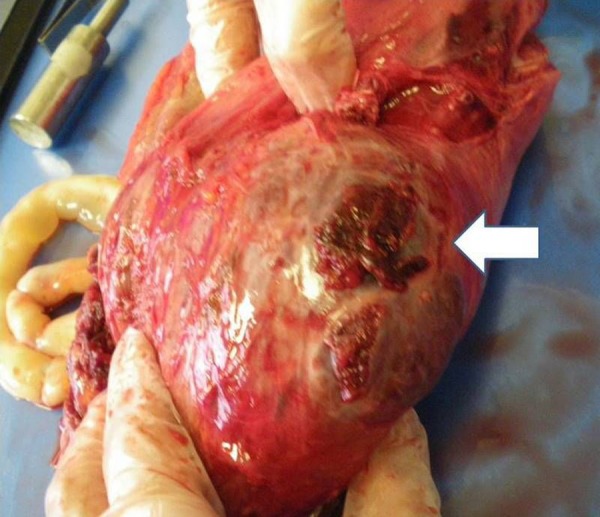
The placenta had completely penetrated the left side of the uterine wall.
Discussion
The options to treat abnormal attachment of the placenta (placenta accreta, placenta increta and placenta percreta) include both conservative and extirpative approaches. The extirpative approach usually requires an adjuvant hemostatic technique, such as bilateral internal iliac artery ligation or preoperative placement of balloon occlusion at the upper reaches of the artery. Carnevale et al. described 21 cases of IIABO used to treat patients with placenta accreta who underwent cesarean hysterectomy, and concluded that this technique is safe and effectively reduces blood loss.¹ Some reports have reached similar conclusions [2–4]. In our case, we attempted to perform IIABO; however, massive vaginal bleeding suddenly occurred due to detachment of the placenta as a result uterine contractions. A quick exchange from IIABO to CIABO was very effective for reducing the amount of blood loss. This indicates that the patient’s internal iliac artery likely had extensive anastomoses. Failure of IIABO can be explained by the presence of extensive anastomoses in the pelvic vasculature. Some reports have concluded that the use of IIABO in patients did not improve surgical outcomes compared with patients without the treatment [5,6]. Shih et al. have insisted that the obturator artery serves as an important anastomosis bridging the internal and external iliac arteries [7]. Angiographic studies of patients undergoing IIA ligation have also identified the branches of the lumbar, sacral, rectal, femoral, and even internal thoracic arteries as the origins of collateral circulation.
Shih et al. were the first to report a successful case of CIABO during cesarean hysterectomy to treat placenta percreta. CIABO occludes more central arteries than IIABO, and is considered to have stronger hemostatic properties. Additionally, CIABO is an easier method with regard to inserting the catheter than IIABO. However, prolonged occlusion of the common iliac arteries may be associated with reperfusion injury, thrombosis, and the formation of embolisms in the lower extremities. Surgery to treat abdominal aortic aneurysms requires at least one hour of aortic cross clamping, and patient can successfully undergo abdominal aortic aneurysm repair; therefore, the amount of time to safely perform CIABO is thought to be one hour or less. However, pregnancy is a relatively hypercoagulable state. Therefore, the occlusion time should be as short as possible. Only one case report has so far been published about thrombosis in CIABO [8].
There are also very few reports of the use of CIABO. Additionally, there have been no randomized controlled studies comparing the amount of intraoperative blood loss occurring with IIABO and CIABO. Our case is the first reported case of CIABO being more effective than IIABO for reducing blood loss during a cesarean hysterectomy in the same patient. Further evaluations of the efficacy and outcomes of CIABO are needed in order to select alternative techniques to use when performing cesarean hysterectomies.
Conclusions
CIABO was found to be more effective than IIABO for reducing blood loss during cesarean hysterectomy. Failure of IIABO can be explained by the presence of extensive anastomoses in the pelvic vasculature.
Footnotes
Declaration of competing interests
We declare that we have no competing interests.
References:
- 1.Carnevale FC, Kondo MM, de Oliveira Sousa W, Jr, et al. Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accreta. Cardiovasc Intervent Radiol. 2011;34:758–64. doi: 10.1007/s00270-011-0166-2. [DOI] [PubMed] [Google Scholar]
- 2.Tan CH, Tay KH, Sheah K, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. AJR. 2007;189:1158–63. doi: 10.2214/AJR.07.2417. [DOI] [PubMed] [Google Scholar]
- 3.Dubois J, Garel L, Grignon A, et al. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997;176:723–26. doi: 10.1016/s0002-9378(97)70582-9. [DOI] [PubMed] [Google Scholar]
- 4.Ojala K, Perälä J, Kariniemi J, et al. Arterial embolization and prophylactic catheterization for the treatment for severe obstetric hemorrhage. Acta Obstet Gynecol Scand. 2005:1075–80. doi: 10.1111/j.0001-6349.2005.00727.x. [DOI] [PubMed] [Google Scholar]
- 5.Levine AB, Kuhlman K, Bonn J. Placenta accreta: comparison of cases managed with and without pelvic artery balloon catheters. J Matern Fetal Med. 1999;8:173–76. doi: 10.1002/(SICI)1520-6661(199907/08)8:4<173::AID-MFM7>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 6.Bodner LJ, Nosher JL, Gribbin C, et al. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol. 2006;29:354–61. doi: 10.1007/s00270-005-0023-2. [DOI] [PubMed] [Google Scholar]
- 7.Shih JC, Liu KL, Shyu MK. Temporary balloon occlusion of the common iliac artery: new approach to bleeding control during cesarean hysterectomy for placenta percreta. Am J Obstet Gynecol. 2005;193:1756–58. doi: 10.1016/j.ajog.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Sewell MF, Rosenblum D, Ehrenberg H. Arterial embolus during common iliac balloon catheterization at cesarean hysterectomy. Obstet Gynecol. 2006;108:746–48. doi: 10.1097/01.AOG.0000201992.80130.2c. [DOI] [PubMed] [Google Scholar]