After peritonitis (1), ultrafiltration failure with volume overload is the next major cause of treatment failure in peritoneal dialysis (PD) (2). Multi-frequency bioimpedance spectroscopy (MF-BIS) can be used to estimate extracellular water (ECW) and intracellular water (ICW) (3,4) and has been validated against isotopic dilution methods in both healthy subjects and dialysis patients (5). Multi-frequency BIS can also be used to assess body composition (6,7). Although it is much more convenient for PD patients and staff to measure MF-BIS with dialysate dwelling, some manufacturers recommend measurements be made with an empty bladder, and therefore the abdomen is always drained before measurements are taken.
To assess the effects of indwelling peritoneal dialysate on MF-BIS, 40 PD outpatients [57.5% men; 17.5% with diabetes; median age: 62 years (range: 24 - 72.5 years); PD vintage: 28 months (range: 4 - 44 months)] attending for peritoneal transport assessment using a standard 2-L exchange with 22.7 g/L dextrose were studied before and after the peritoneal dialysate was drained. Measurements were taken using an 8-tactile-electrode system (InBody 720: BioSpace, Seoul, Korea) (8,9).
Median net PD ultrafiltration volume was 200 mL (range: 100 - 300 mL); serum C-reactive protein, 3 mg/dL (range: 1 - 5.5 mg/dL); and glucose, 5.6 mmol/L (range: 4.6-6.9 mmol/L). Mean albumin was 39.2 ± 3.4 g/dL.
To confirm reliability, measurements of ECW divided by total body water (TBW) were repeated in 22 patients, and a Bland-Altman analysis showed no significant differences (bias: 0.0003; t-statistic: 0.47; 95% confidence limits: -0.0016, 0.001). In 6 patients chosen for a wide range of TBW (24 L - 51 L), 4 MF-BIS measurements were made during a period of 2 hours with dialysate dwelling, and no differences in ECW (mean bias: -0.2 ± 0.21) or ICW (mean bias: 0.097 ± 0.041) were observed.
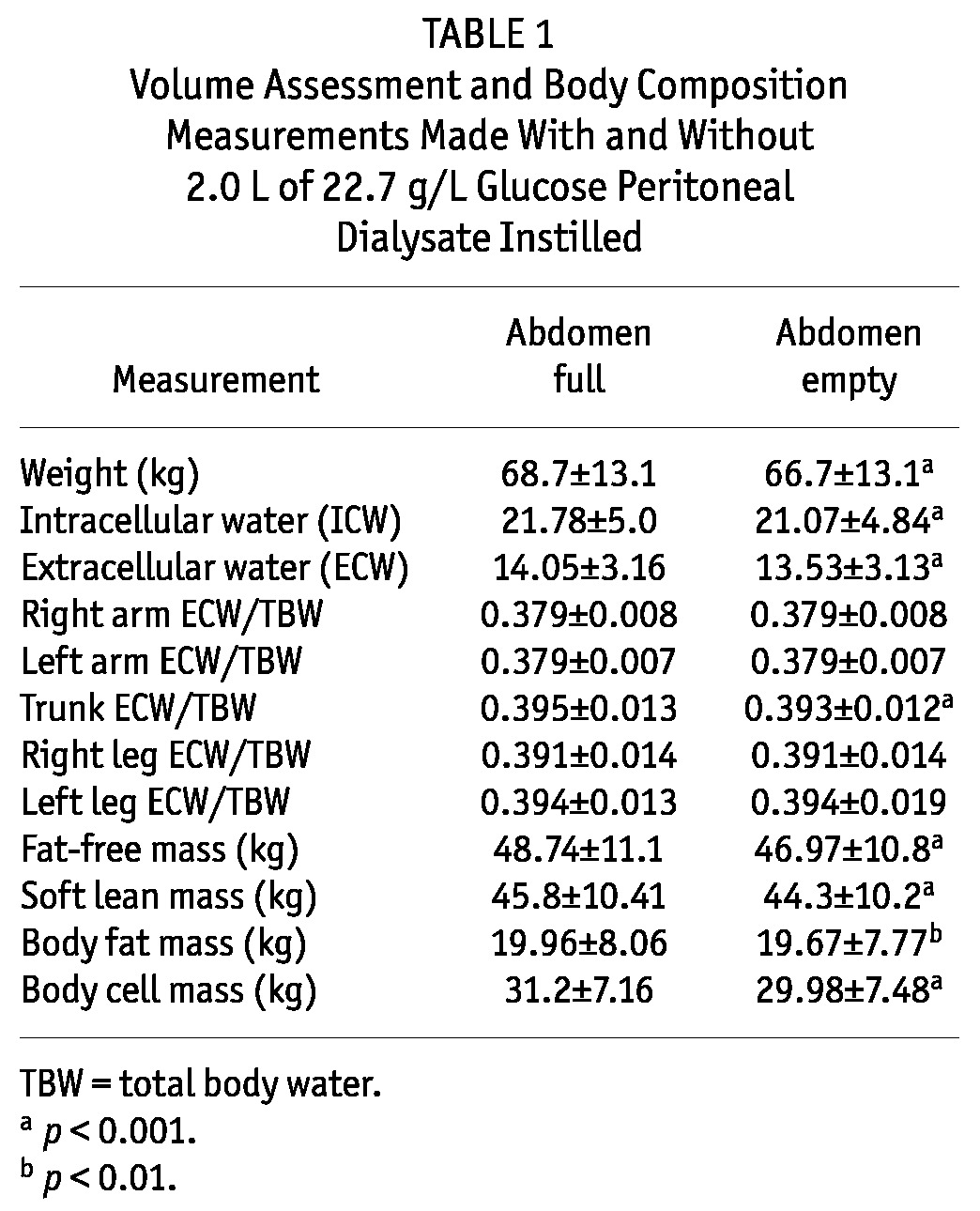
Using the InBody MF-BIS device, differences in TBW, ICW, and ECW were observed depending on whether dialysate was instilled or drained (Table 1). Not surprisingly, the greatest variation occurred in the truncal compartment; the ECW/TBW ratios did not vary for the limbs. Significant differences in body composition were noted depending on whether dialysate was instilled or drained (Table 1). Electrical resistance increased with fluid instilled, and the MF-BIS software algorithms overestimated muscle mass more than fat mass (10,11).
TABLE 1.
Volume Assessment and Body Composition Measurements Made With and Without 2.0 L of 22.7 g/L Glucose Peritoneal Dialysate Instilled
Thus, although it is much more convenient to take MF-BIS measurements with peritoneal dialysate in situ, my group also advocates drainage of the dialysate, in keeping with the InBody manufacturer’s recommendation that measurements should be performed with an empty bladder. Further work is required to determine whether other MF-BIS devices are equally affected. The differences in measurements are probably not clinically significant provided they are made in a standardized and reproducible fashion (12) and are performed serially to document change rather than absolute values; however, single measurements of body composition may be prone to error with dialysate instilled.
Disclosures
The author has no financial conflicts of interest.
References
- 1. Davenport A. Peritonitis remains the major clinical complication of peritoneal dialysis: the London, UK, peritonitis audit 2002-2003. Perit Dial Int 2009; 29:297–302 [PubMed] [Google Scholar]
- 2. Habib AM, Preston E, Davenport A. Risk factors for developing encapsulating peritoneal sclerosis in the icodextrin era of peritoneal dialysis prescription. Nephrol Dial Transplant 2010; 25:1633–8 [DOI] [PubMed] [Google Scholar]
- 3. Konings CJ, Kooman JP, Schonck M, Cox-Reijven PL, van Kreel B, Gladziwa U, et al. Assessment of fluid status in peritoneal dialysis patients. Perit Dial Int 2002; 22:683–92 [PubMed] [Google Scholar]
- 4. Woodrow G, Oldroyd B, Wright A, Coward WA, Truscott JG. The effect of normalization of ECW volume as a marker of hydration in peritoneal dialysis patients and controls. Perit Dial Int 2005; 25(Suppl 3):S49–51 [PubMed] [Google Scholar]
- 5. Moissl UM, Wabel P, Chamney PW, Bosæus I, Levin NW, Bosy-Westphal A, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 2006; 27:921–33 [DOI] [PubMed] [Google Scholar]
- 6. Fürstenberg A, Davenport A. Comparison of multifrequency bioelectrical impedance analysis and dual-energy X-ray absorptiometry assessments in outpatient hemodialysis patients. Am J Kidney Dis 2011; 57:123–9 [DOI] [PubMed] [Google Scholar]
- 7. Fürstenberg A, Davenport A. Assessment of body composition in peritoneal dialysis patients using bioelectrical impedance and dual-energy X-ray absorptiometry. Am J Nephrol 2011; 33:150–6 [DOI] [PubMed] [Google Scholar]
- 8. Davenport A, Willicombe M. Comparison of fluid status in patients treated by different modalities of peritoneal dialysis using multi-frequency bioimpedance. Int J Artif Organs 2009; 32:779–86 [DOI] [PubMed] [Google Scholar]
- 9. Davenport A, Willicombe MK. Does diabetes mellitus predispose to increased fluid overload in peritoneal dialysis patients? Nephron Clin Pract 2010; 114:c60–6 [DOI] [PubMed] [Google Scholar]
- 10. Davenport A, Hussain Sayed R, Fan S. The effect of racial origin on total body water volume in peritoneal dialysis patients. Clin J Am Soc Nephrol 2011; 6:2492–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Woodrow G. Extracellular water expansion: part of the malnutrition-inflammation-atherosclerosis syndrome? Perit Dial Int 2006; 26:566–70 [PubMed] [Google Scholar]
- 12. Davenport A, Willicombe MK. Hydration status does not influence peritoneal equilibration test ultrafiltration volumes. Clin J Am Soc Nephrol 2009; 4:1207–12 [DOI] [PMC free article] [PubMed] [Google Scholar]


