Abstract
The advent of deep enteroscopy (DE) has dramatically changed diagnostic and therapeutic approaches to small bowel diseases. Unlike capsule endoscopy, which is unable to obtain biopsies or treat a disease, DE techniques have diagnostic and therapeutic capabilities. Double-balloon enteroscopy (DBE) was introduced in 2001, and single-balloon enteroscopy (SBE) and spiral enteroscopy (SE) were subsequently developed for small bowel investigation. In published reports comparing these different enteroscopy techniques, most comparative parameters (depth of insertion, complications, learning curve, diagnostic yield, and therapeutic yield) were comparable among DBE, SBE, and SE. However, the procedure duration appears to be shorter for SE than for DBE and SBE. The rate of complete enteroscopy is clearly superior for DBE, compared with SE and SBE. Because these results do not indicate an increase in diagnostic or therapeutic yield, the clinical impact of complete enteroscopy remains controversial. According to previous studies, the three DE methods seem to be equally effective and safe in the clinical setting. Although larger randomized controlled trials are needed to evaluate the procedural characteristics and clinical impact, the selection of an enteroscopic technique should be based on availability and the endoscopist's experience.
Keywords: Double-balloon enteroscopy, Single-balloon enteroscopy, Spiral enteroscopy
INTRODUCTION
A wide variety of diseases may be associated with small bowel lesions. However, the diagnosis of small bowel disorders has long been a challenge to gastroenterologists because of the length and anatomy of the small intestine and the lack of adequate diagnostic tools. Traditionally, the diagnosis andassessment of small bowel lesions have depended on radiologic tests such as small bowel follow-through and computed tomo-graphy. In recent years, the advent of capsule endoscopy (CE) and deep enteroscopy (DE) has dramatically changed diagnostic and therapeutic approaches to small bowel diseases. Although CE can be used to examine areas unreachable by enteroscopy, a main disadvantage of this technique is the inability to obtain biopsies or to treat the disease. In contrast, DE techniques have diagnostic and therapeutic capabilities. Three DE methods are currently available: double-balloon enteroscopy (DBE), single-balloon enteroscopy (SBE), and spiral enteroscopy (SE). In this review, we provide a detailed analysis of the current status of the different types of DE.
TYPES OF SMALL BOWEL ENTEROSCOPY
Device-assisted enteroscopy
Historically, a conventional colonoscope or a 200-cm long flexible enteroscope was used to intubate the small bowel with limited intubation depth. The development of device-assisted enteroscopy (DAE) allows deeper intubation of the small bowel. DAE, including balloon-assisted enteroscopy (BAE) and SE, can be divided into three techniques; DBE, SBE, and SE.
DBE
Dr. Hironi Yamamoto developed DBE in 2001,1 and this method was introduced in Korea in 2004. The use of a balloon enables gripping of the intestinal wall and prevents subsequent loop formation.1,2 The two most commonly used DBE systems (EN-450P5 and EN450T5; Fujinon Inc., Saitama, Japan) have diameters of 8.5 and 9.3 mm and operating channels of 2.2 and 2.8 mm, respectively. Corresponding overtubes (TS-12140 and TS-13140; Fujinon Inc.) are 12.2 and 13.3 mm wide, respectively, with a length of 140 cm.3 The maximum balloon pressure using a balloon pump controller is 45 mm Hg. An overtube-balloon system can be reused, but an enteroscope balloon can be used only once. A DBE system consists of a balloon at the distal end of an enteroscope and an overtube; its use entails a series of steps employing a push and pull technique.4 The enteroscope is advanced further, while an inflated balloon on the overtube is used to maintain a stable position. After deflation of the balloon on the overtube and inflation of the balloon on the enteroscope, the balloon overtube advances to meet the enteroscope balloon (push procedure). The pull procedure begins using both the enteroscope and the overtube pulled back with balloons inflated.5,6
SBE
The SBE system is represented by the SIF-Q160 endoscope (Olympus Optical Co., Ltd., Tokyo, Japan), which has a working length of 200 cm, a distal end diameter of 9.2 mm, and a working channel with a 2.8-mm diameter, and the ST-SB1 single-use splinting tube (overtube) with a length of 132 cm and an outer diameter of 13.2 mm.2,3 This system can use narrow band imaging with the EVIS EXERA II system. The balloon material is silicone, not latex, and the missing scope balloon is what distinguishes it from DBE. The SBE system is controlled by repeatedly inflating and deflating a single balloon attached to the distal end of a splinting tube.2 The SBE-technique uses the angulated tip of the endoscope, called hooked-tip, to fix the bowel to the scope compensating the second balloon at the tip of the endoscope. Because SBE was introduced in 2007, few published studies have directly compared this method with DBE or SE.
SE
SE, which was introduced in 2007, has the potential advantages of shorter examination time and ease of use compared with BAE.7 The Endo-Ease Discovery SB system (Spirus Medical, Stoughton, MA, USA) is made of polyvinyl chloride and has a length of 118 cm, with external and internal diameters of 16 mm and 9.8 mm, respectively. The distal end of the overtube has a raised hollow spiral, 5.5 mm in height and 21 cm in length, and a soft tapered tip. Enteroscopes made by Fujinon and Olympus (overtube- or balloon-free) can be used for SE. This method enables the enteroscope to be advanced and withdrawn through the small bowel using rotatory clockwise and counter clockwise movements.2,3
Indications for enteroscopy
The development of enteroscopy has expanded its indications. According to the published data, the most common indication for DE is the evaluation of obscure gastrointestinal bleeding (OGIB).8 Among other indications are the evaluation of inflammatory mucosal lesions (e.g., Crohn disease and nonsteroidal anti-inflammatory drug-induced enteropathy) and small bowel tumors, acquisition of biopsies, treatment of disease, and surveillance of polyposis syndrome. In special situations, such as surgically altered anatomy or failed colonoscopy, BAE has been used recently. Indications of DBE, SBE, and SE are similar. In a meta-analysis, Xin et al.8 showed that the distribution of positive findings appears to differ between Eastern and Western countries. In particular, inflammatory lesions (37.6%) were primarily found in the East, whereas vascular lesions (65.9%) were frequently diagnosed in the West.8,9
COMPARISON OF DBE, SBE, AND SE
To date, six randomized controlled trials (RCTs) have compared the use of DBE, SBE, and SE.7,10-14 The results of these studies have differed slightly. Table 1 summarizes reported comparative procedure-related data.
Table 1.
Procedure-Related Data
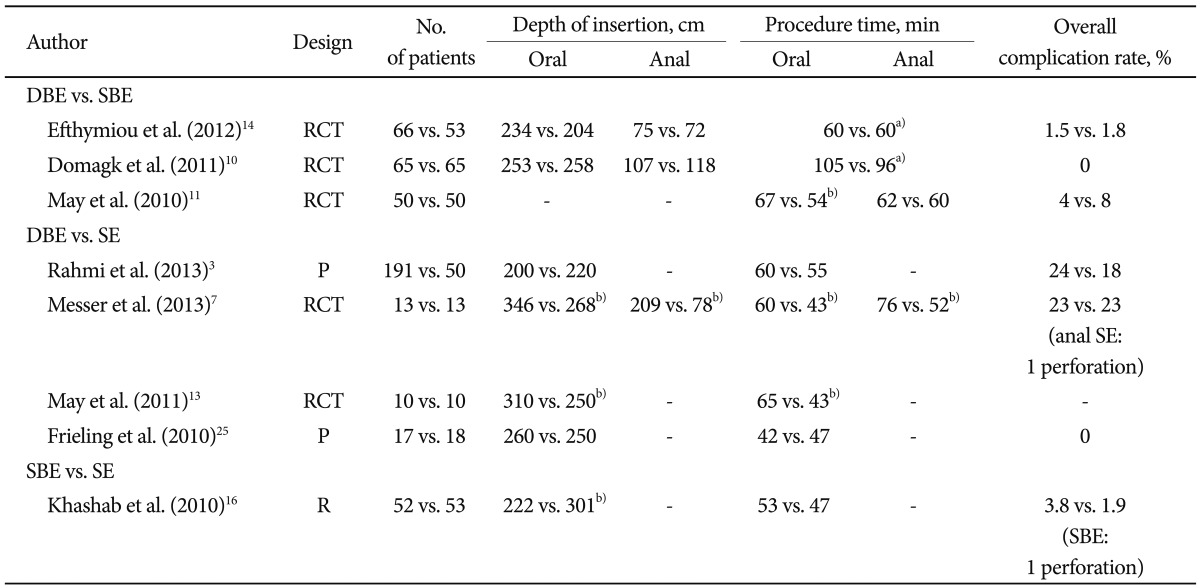
DBE, double-balloon enteroscopy; SBE, single-balloon enteroscopy; RCT, randomized controlled trial; SE, spiral enteroscopy; P, prospective study; R, retrospective study.
a)No mention of the direction; b)Significant difference.
The depth of insertion
To compare the different enteroscopy techniques, reasonable comparative parameters are essential. Of the various parameters, the depth of insertion (DI) is an important parameter that can be used to evaluate the performance of different endoscopy systems.6 Assessment of DI is performed as follows: the efficacy of each push-and-pull maneuver is estimated and the advancement length is recorded on a standardized sheet, and the enteroscope DI is estimated by calculating the overtube insertion length. Based on preliminary surgical observations, every 5 cm of overtube advancement is equivalent to 40 cm of small bowel visualization.15
Efthymiou et al.14 compared 66 DBEs and 53 SBEs in an RCT. The mean DI for DBE and SBE were 75.5 and 72.1 cm, respectively (p=0.835), with the anal approach, and 234.1 and 203.8 cm, respectively (p=0.176), with the oral approach. Another multicenter RCT also evaluated these two enteroscopy techniques (65 DBEs vs. 65 SBEs). The mean oral and anal DI showed noninferiority of DBE versus SBE (mean oral DI, 253 cm vs. 258 cm; mean anal DI, 107 cm vs. 118 cm, respectively).10 In two RCTs comparing the double- and single-balloon techniques, the oral DI was more than 200 cm, while the anal DI was 70 to 120 cm; no significant difference was found in the DI. The results of previous studies have been inconsistent in the comparison of DBE and SE. A prospective crossover study was carried out to compare 10 SEs and 10 DBEs. The median oral DI was greater in the DBE group than in the SE group (310 cm vs. 250 cm, p=0.004).13 Another RCT enrolled 26 patients (13 DBE vs. 13 SEs) and evaluated these two enteroscopy techniques. A greater DI was found in the DBE group in both oral (346 cm vs. 268 cm, p=0.006) and anal (209 cm vs. 78 cm, p<0.001) examinations.7 In two RCTs, the oral DI of SE was significantly lower than that of DBE. In a larger prospective comparative study, 191 DBEs and 50 SEs were compared and the mean oral DI were 200 and 220 cm (p=0.13), respectively.3 Therefore, according to these studies, the oral DI of the two techniques seems to be comparable. Only one study evaluated SBE and SE endoscopy systems competitively in a retrospective design (52 SBEs vs. 53 SEs), determining that the oral DI of SBE was significantly lower than that of SE (222 cm vs. 301 cm, p<0.001).16 However, published data have indicated that the oral DI seem to be comparable among DBE (239±24.3 cm), SBE (233±31 cm), and SE (236±23 cm).6
Complete enteroscopy
Another comparative parameter is complete enteroscopy. Given the difficulty of estimating insertion depths, the rate of total enteroscopy has been considered to be the gold standard. The mean of complete small bowel visualization has been used differently (successful panenteroscopy vs. complete visualization in attempted examinations) in several studies.17,18 The rate and clinical impact of complete small bowel visualization is controversial.6,19,20 If complete enteroscopy were assumed to be panenteroscopy, low overall rates would be achieved. Therefore, we should consider whether a complete enteroscopy was attempted. Although the rate of complete enteroscopy is clearly superior for DBE compared with SE and SBE,6 these rates have not been translated into increased diagnostic or therapeutic yields.11,21 In a study by Takano et al.,12 the complete enteroscopy rate was 0% in the SBE group and 57% in the DBE (p<0.0001). However, this study reported no distinct differences in the diagnostic and therapeutic yield between the groups. This remarkable finding explained that the rate of complete enteroscopy did not guarantee increased diagnostic and therapeutic yields. Therefore, complete small bowel visualization should be attempted based on clinical judgment because a diagnosis can be made without complete enteroscopy in the majority of patients.
The procedure and preparation times
The duration of the procedures is another parameter to consider. Factors related to short procedure time include the technical expertise of the endoscopist, previous operation history, bowel adhesion, and obesity. A shorter procedure is related to less patient discomfort, which relieves the endoscopist's anxiety and alleviates technical difficulties. In a retrospective study, Khashab et al.16 reported no significant difference in the mean procedure times between SBE and SE (53 minutes vs. 47 minutes, p=0.2). According to previous published data, the mean oral procedure times of DBE, SBE, and SE were 70, 60, and 40 minutes, respectively; the anal procedure time was similar (85 minutes vs. 69 minutes vs. 46 minutes).6 This suggests that the procedure duration was the shortest in the SE group. However, judging the availability of procedures based on procedure time alone is inappropriate. Two studies assessed preparation time, which was slightly shorter for SBE than for DBE.11,17
Safety
There are safety parameters to consider. Both major and minor complications can occur with enteroscopic procedures. Reported complications most commonly include perforation, bleeding, pancreatitis, and enteritis, which occur primarily after the procedure. Minor complications are usually self-limiting. In most published studies, the reported complications were minor.3,11,14
In the most recent study, a total of 27 patients were randomized: 13 to DBE and 13 to SE.7 The overall complication rate was the same (23% vs. 23%), but one perforation was reported during an anal SE examination. In another retrospective study comparing 52 SBEs with 53 SEs, the overall complication rate was 3.8% for SBE and 1.9% for SE (p=0.6).16 However, perforation occurred in one SBE procedure. Taken together, the rate of major complications was very low in all enteroscopy techniques, and DBE, SBE, and SE appear to be safe methods.6
The learning curve
Although no study has conducted a direct comparison, improvement in the overall procedural time or extent of small bowel visualized after the initial 10 to 15 procedures was reported in DBE and SBE studies.22,23 It appears that the learning curve is shortest with SE, as reports indicate that the device is easy to use and can be effectively operated after performance of as few as five training cases.24
Clinical outcomes
Table 2 summarizes reported comparative clinical outcomes. The parameters of clinical outcome include diagnostic and therapeutic yields. Diagnostic yield is defined as diagnosis confirmed by endoscopic means and the important parameter in the assessment of a method's clinical relevance. Therapeutic yield is also important to judge the clinical impact of the different enteroscopy techniques. Several clinical outcome comparisons of DBE and SBE in patients with small bowel disease have been published. In four RCTs,10-12,14 the diagnostic yield of both groups was 40% to 60%. Therapeutic yield is commonly reported to be 30%,12,14 although one study that estimated therapeutic yield as the number of therapeutic procedures reported therapeutic yield of less than 10% than that of other studies,10 with no significant difference in the procedure performed. Another study reported that therapeutic yield was significantly higher in the DBE group at 72%, compared with 48% in the SBE group (p=0.025).11 When comparing DBE and SE, there was no difference in the diagnosis and therapeutic yield.7,25 According to one study, SBE and SE systems showed similar diagnostic and therapeutic yields.16 Ultimately, the published diagnostic yields for all of these procedures are comparable.21 The methods have shown no significant difference in the rate of therapeutic yield.6,21
Table 2.
Comparative Clinical Outcomes
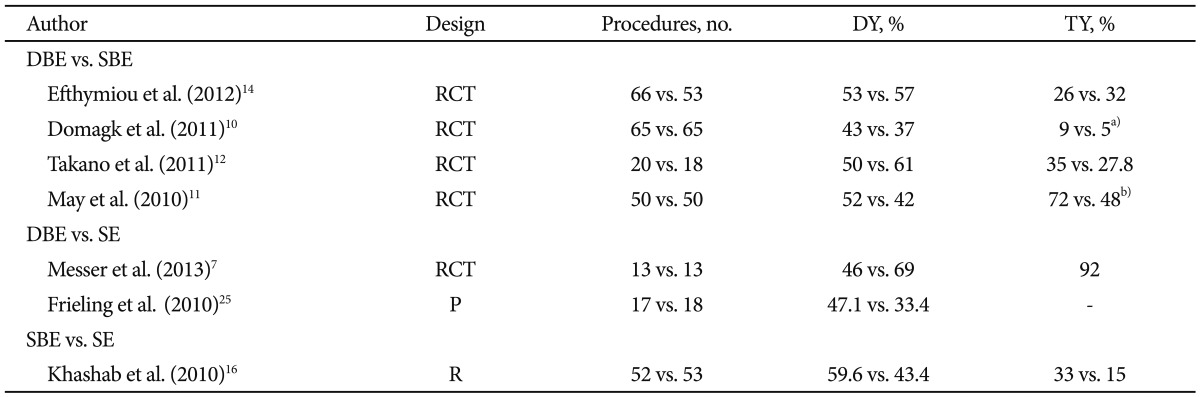
DY, diagnostic yield; TY, therapeutic yield; DBE, double-balloon enteroscopy; SBE, single-balloon enteroscopy; RCT, randomized controlled trials; SE, spiral enteroscopy; P, prospective study; R, retrospective study.
a)The number of therapeutic procedures; b)Significant difference (p=0.025).
ENTEROSCOPY IN SPECIAL SITUATION
There have been recent reports of diagnostic and therapeutic endoscopic retrograde cholangiopancreatography (ERCP) using DAE for pancreaticobiliary lesions in patients with a history of surgical reconstruction.2 The surgical treatment such as complex liver, biliopancreatic, and obesity surgery will further increase the number of patients with R-en Y anastomosis with its associated risk of biliary complications.26 DAE-ERCP appears to be a true step towards addressing these biliary complications. Therefore, further DAE-ERCP procedure improvement is desirable. In a retrospective multicenter study, the success of ERCP was evaluated in patients who underwent long-limb surgical bypass using DBE, SBE, and SE. The overall success rate of ERCP was 63% (81/129), while that of enteroscopy was 71% (92/129); 88% (81/92) of patients who under-went enteroscopy achieved ERCP success.27 The success rates of ERCP were similar among SBE, DBE, and SE. In surgical bypass patients who require ERCP, ERCP using DAE may be considered before proceeding to a more invasive percutaneous or surgical alternative.
NEW ENTEROSCOPY
A new balloon-guided enteroscopy (BGE) system (NaviAid BGE; Smart Medical Systems Ltd., Ra'anana, Israel) enables enteroscopy with technology similar to that of DBE. The BGE device became fully commercial by the end of 2009. This system can be used with standard endoscopic equipment. The BGE device is comprised of a two-balloon add-on disposable element and an air supply unit to control the inflation and deflation of the balloons. The BGE disposable element is easily mounted on the endoscope, with a stabilizing balloon at the distal end of the endoscope and an advancing balloon sheltered within the stabilizing balloon. The advancing balloon is advanced or retracted manually ahead of the scope by a flexible advancing tube that passes through a dedicated external channel, leaving the endoscope instrument channel free for accessory use.28,29
This system has not been introduced in Korea yet. In a study that enrolled 35 patients, the mean procedure time was 52 minutes and the oral DI was 190 cm.28 The mean oral DI was 145 cm in another study, which is deeper than that in published results of push enteroscopy.29 According to these studies, BGE appears to be a safe and effective method. However, further larger studies are needed.
SUMMARY
Procedure duration appears to be shorter for SE than for DBE and SBE. Although the rate of complete enteroscopy is clearly superior for DBE, compared with SE and SBE, this result does not indicate an increase of diagnostic or therapeutic yield. Altogether, these methods are not significantly different with respect to the other factors. However, in patients with OGIB, BAE seems to be better than SE, which can cause a bit more trauma, allowing vascular lesions by one of the most common causes of OGIB. Table 3 shows the main characteristics of these three enteroscopic techniques.
Table 3.
Comparison between the Three Enteroscopic Techniques
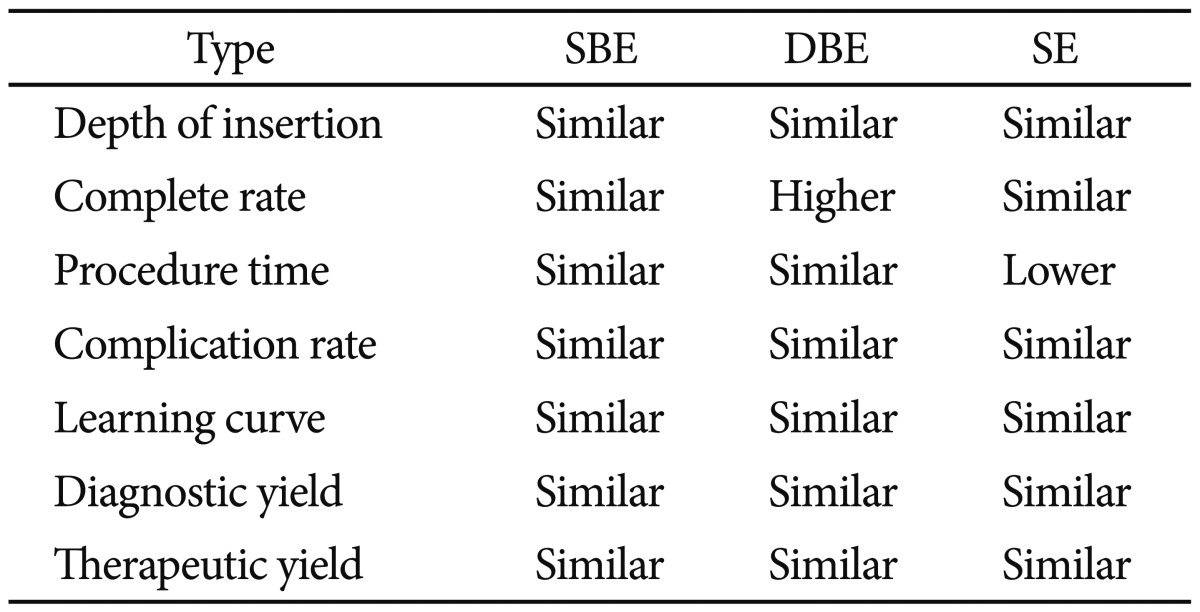
SBE, single-balloon enteroscopy; DBE, double-balloon enteroscopy; SE, spiral enteroscopy.
CONCLUSIONS
Although the clinical impact of total enteroscopy rates remains controversial, the results of previous studies suggest that DBE, SBE, and SE have comparable diagnostic and therapeutic yields. Therefore, the selection of an enteroscopic technique should be based on availability and the endoscopist's experience.
Acknowledgments
This work was supported in part by the Soonchunhyang University Research Fund.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 2.Elena RM, Riccardo U, Rossella C, Bizzotto A, Domenico G, Guido C. Current status of device-assisted enteroscopy: technical matters, indication, limits and complications. World J Gastrointest Endosc. 2012;4:453–461. doi: 10.4253/wjge.v4.i10.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rahmi G, Samaha E, Vahedi K, et al. Multicenter comparison of double-balloon enteroscopy and spiral enteroscopy. J Gastroenterol Hepatol. 2013;28:992–998. doi: 10.1111/jgh.12188. [DOI] [PubMed] [Google Scholar]
- 4.Monkemüller K, Fry LC, Bellutti M, Malfertheiner P. Balloon-assisted enteroscopy: unifying double-balloon and single-balloon enteroscopy. Endoscopy. 2008;40:537. doi: 10.1055/s-2007-995712. [DOI] [PubMed] [Google Scholar]
- 5.May A, Ell C. Push-and-pull enteroscopy using the double-balloon technique/double-balloon enteroscopy. Dig Liver Dis. 2006;38:932–938. doi: 10.1016/j.dld.2006.07.101. [DOI] [PubMed] [Google Scholar]
- 6.Lenz P, Domagk D. Double- vs. single-balloon vs. spiral enteroscopy. Best Pract Res Clin Gastroenterol. 2012;26:303–313. doi: 10.1016/j.bpg.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Messer I, May A, Manner H, Ell C. Prospective, randomized, single-center trial comparing double-balloon enteroscopy and spiral enteroscopy in patients with suspected small-bowel disorders. Gastrointest Endosc. 2013;77:241–249. doi: 10.1016/j.gie.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Xin L, Liao Z, Jiang YP, Li ZS. Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc. 2011;74:563–570. doi: 10.1016/j.gie.2011.03.1239. [DOI] [PubMed] [Google Scholar]
- 9.Jeon SR, Kim JO, Kim HG, et al. Changes over time in indications, diagnostic yield, and clinical effects of double-balloon enteroscopy. Clin Gastroenterol Hepatol. 2012;10:1152–1156. doi: 10.1016/j.cgh.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 10.Domagk D, Mensink P, Aktas H, et al. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy. 2011;43:472–476. doi: 10.1055/s-0030-1256247. [DOI] [PubMed] [Google Scholar]
- 11.May A, Farber M, Aschmoneit I, et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575–581. doi: 10.1038/ajg.2009.712. [DOI] [PubMed] [Google Scholar]
- 12.Takano N, Yamada A, Watabe H, et al. Single-balloon versus double-balloon endoscopy for achieving total enteroscopy: a randomized, controlled trial. Gastrointest Endosc. 2011;73:734–739. doi: 10.1016/j.gie.2010.10.047. [DOI] [PubMed] [Google Scholar]
- 13.May A, Manner H, Aschmoneit I, Ell C. Prospective, cross-over, single-center trial comparing oral double-balloon enteroscopy and oral spiral enteroscopy in patients with suspected small-bowel vascular malformations. Endoscopy. 2011;43:477–483. doi: 10.1055/s-0030-1256340. [DOI] [PubMed] [Google Scholar]
- 14.Efthymiou M, Desmond PV, Brown G, et al. SINGLE-01: a randomized, controlled trial comparing the efficacy and depth of insertion of single- and double-balloon enteroscopy by using a novel method to determine insertion depth. Gastrointest Endosc. 2012;76:972–980. doi: 10.1016/j.gie.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 15.May A, Nachbar L, Schneider M, Neumann M, Ell C. Push-and-pull enteroscopy using the double-balloon technique: method of assessing depth of insertion and training of the enteroscopy technique using the Erlangen Endo-Trainer. Endoscopy. 2005;37:66–70. doi: 10.1055/s-2004-826177. [DOI] [PubMed] [Google Scholar]
- 16.Khashab MA, Lennon AM, Dunbar KB, et al. A comparative evaluation of single-balloon enteroscopy and spiral enteroscopy for patients with mid-gut disorders. Gastrointest Endosc. 2010;72:766–772. doi: 10.1016/j.gie.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 17.May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc. 2005;62:62–70. doi: 10.1016/s0016-5107(05)01586-5. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto H, Kita H, Sunada K, et al. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010–1016. doi: 10.1016/s1542-3565(04)00453-7. [DOI] [PubMed] [Google Scholar]
- 19.May A. How much importance do we have to place on complete enteroscopy? Gastrointest Endosc. 2011;73:740–742. doi: 10.1016/j.gie.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 20.Xin L, Gao Y, Liao Z, Li ZS. The reasonable calculation of complete enteroscopy rate for balloon-assisted enteroscopy. Endoscopy. 2011;43:832. doi: 10.1055/s-0030-1256569. [DOI] [PubMed] [Google Scholar]
- 21.Gerson LB. Small-bowel enteroscopy. Endoscopy. 2013;45:292–295. doi: 10.1055/s-0032-1326286. [DOI] [PubMed] [Google Scholar]
- 22.Mehdizadeh S, Ross A, Gerson L, et al. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740–750. doi: 10.1016/j.gie.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Dutta AK, Sajith KG, Joseph AJ, Simon EG, Chacko A. Learning curve, diagnostic yield and safety of single balloon enteroscopy. Trop Gastroenterol. 2012;33:179–184. doi: 10.7869/tg.2012.45. [DOI] [PubMed] [Google Scholar]
- 24.Buscaglia JM, Dunbar KB, Okolo PI, 3rd, et al. The spiral enteroscopy training initiative: results of a prospective study evaluating the Discovery SB overtube device during small bowel enteroscopy (with video) Endoscopy. 2009;41:194–199. doi: 10.1055/s-0028-1119602. [DOI] [PubMed] [Google Scholar]
- 25.Frieling T, Heise J, Sassenrath W, Hulsdonk A, Kreysel C. Prospective comparison between double-balloon enteroscopy and spiral enteroscopy. Endoscopy. 2010;42:885–888. doi: 10.1055/s-0030-1255714. [DOI] [PubMed] [Google Scholar]
- 26.Moreels TG. Device-assisted enteroscopy: how deep is deep enteroscopy? Gastrointest Endosc. 2012;76:981–982. doi: 10.1016/j.gie.2012.08.030. [DOI] [PubMed] [Google Scholar]
- 27.Shah RJ, Smolkin M, Yen R, et al. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video) Gastrointest Endosc. 2013;77:593–600. doi: 10.1016/j.gie.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 28.Kiesslich R KS, Hoffman A, Goetz M, Galle PR, Neurath MF. Small bowel enteroscopy: feasibility and safety of the new balloon guided endoscopy system using different high definition, confocal and standard endoscopes. Gastrointest Endosc. 2009;69:AB364. [Google Scholar]
- 29.Adler SN, Bjarnason I, Metzger YC. New balloon-guided technique for deep small-intestine endoscopy using standard endoscopes. Endoscopy. 2008;40:502–505. doi: 10.1055/s-2007-995677. [DOI] [PubMed] [Google Scholar]


