Abstract
Colonic perforation occurs in a variety of clinical scenarios and colonoscopy-associated perforation is one of the important reasons for colonic perforation. Colonoscopy-associated perforation may be diagnosed during colonoscopy procedure by the visualization of evident colonic wall defect or, after the completion of colonoscopy, by the visualization of leaked air in the peritoneal or retroperitoneal space. Recently, the incidence of colonoscopy-associated perforation increased because of the introduction of colorectal endoscopic submucosal dissection. Traditionally, colonoscopy-associated perforation was managed surgically. However, medical management has been introduced widely and endoscopic clipping is the most important component for the medical management of colonoscopy-associated perforation. Timely administration of antibiotics is also important. Large perforations, diagnostic colonoscopy-associated perforations, large amount of pneumoperitoneum, and severe abdominal pain have been reported to be predictive of the necessity of surgery after endoscopic clipping. Surgery should be performed if patients show clinical deterioration even after the initiation of medical management.
Keywords: Perforation, Colonoscopy, Surgical instruments, Endoscopy, Colon
INTRODUCTION
Colonic perforation may occur either as a sequela of various colorectal diseases or as a complication of colonoscopy. Perforation associated with severe acute appendicitis, diverticulitis, or colorectal cancer is an example of disease-related perforation. Toxic megacolon accompanying such conditions as severe ulcerative colitis or clostridium colitis may also lead to colonic perforation. Diagnostic and therapeutic colonoscopy is another principal cause of colonic perforation. Although the incidence of perforation associated with colonoscopy is only 0.05% to 0.39%,1-4 it is of importance because surgical intervention may be necessary for the management of colonoscopy-associated perforation. In addition, recent advent of endoscopic submucosal dissection (ESD) resulted in high incidence of perforation although the indication for endoscopic therapy of colorectal neoplasm has been expanded. Understanding the clinical characteristics of colonic perforation and its management is becoming more important as colonoscopic procedures become more diverse and aggressive. In this paper, colonic perforation associated with colonoscopy will be reviewed, especially from the viewpoint of endoscopic management of perforation.
INCIDENCE OF PERFORATION
The incidence of colonoscopy-associated perforation is reported to be 0.05% to 0.39%.1-4 Rectosigmoid colon is the segment where perforation occurs most commonly. Old age, female, comorbidity, diverticulosis, and polypectomy were reported as risk factors of colonoscopy-associated perforations.5
Recently, ESD has been introduced for the resection of large colorectal neoplasm, which was complicated with high incidence of colonic perforation ranging from 1.4% to 10.0%.6-13 Large tumor size, presence of submucosal fibrosis, and laterally spreading tumor type were reported as risk factors of colorectal ESD-associated perforations.14,15 Furthermore, the cecum and ascending colon appear to be more susceptible to perforation during ESD compared to the rectum.13
MECHANISM OF PERFORATION
Several mechanisms may be involved in colonoscopy-associated colonic perforation, which include blunt trauma on the colonic wall, unintentional endoscopic resection, and excessive thermal injury. In general, blunt trauma is the main cause of diagnostic colonoscopy-associated perforation. Perforations from blunt trauma are usually large in size. They occur commonly in rectosigmoid area because they develop when colonoscope is pushed without resolution of looping at the rectosigmoid colon or when colonoscope is retroflexed immoderately.5
Unintentional endoscopic resection and excessive thermal injury are related to perforations during therapeutic colonoscopy such as endoscopic mucosal resection or ESD. Perforations resulted from unintentional endoscopic resection are generally small and more common in the right colon.5 Thermal injury-related perforations, in general, are also small.5 Thermal injury-related perforations may not be detected often during colonoscopic procedure because only excessive transmural burn is evident without overt perforation right after endoscopic mucosal resection. Therefore, thermal injury-related perforations are usually diagnosed after the completion of colonoscopic procedure.
DIAGNOSIS OF PERFORATION
Colonoscopy-associated perforations may be classified into an endoscopically proven perforation and a radiologically proven perforation based on the diagnostic process.16 An endoscopically proven perforation refers to colonic mural defect detected during colonoscopy procedure (Fig. 1). It may be accompanied by observable intraabdominal organ or fat tissue through the mural defect if the perforation is large enough. A target sign, white center (muscularis propria and/or serosa) with surrounding blue area (indigo carmine stained submucosa), at the postresection colon ulcer site or at the resection side of resected specimen, may be helpful in determining the probability of small perforation.17
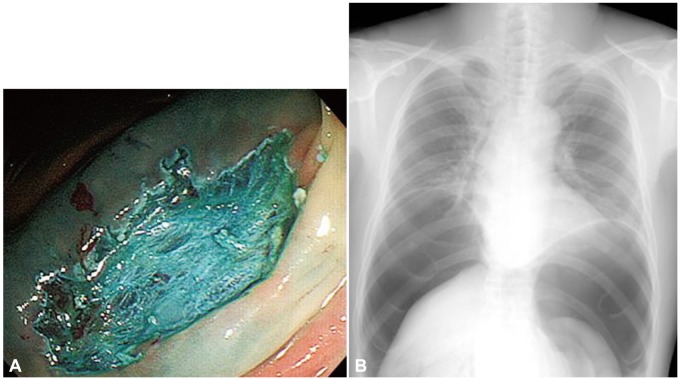
Fig. 1.
Endoscopically proven perforation. (A) Diagnostic colonoscopy-associated perforation. The perforation occurred during excessive pushing of the colonoscope. It is relatively large. (B) Therapeutic colonoscopy-associated perforation. The perforation developed during endoscopic submucosal dissection (ESD) of colonic adenoma. It is relatively small and the surrounding area shows ESD ulcer.
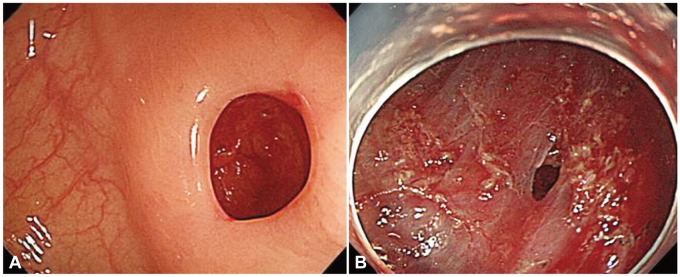
A radiologically proven perforation is defined as a pneumoperitoneum or a pneumoretroperitoneum shown on a simple abdominal X-ray or as extraluminal air density or abscess at the site of the therapeutic procedure (Fig. 2). Endoscopically proven perforations may be accompanied by radiological evidence of perforation. However, some radiologically proven perforations do not show endoscopic evidence of perforation. Therefore, they may be diagnosed only after the completion of colonoscopy procedure.
Fig. 2.
Radiologically proven perforation. (A) An endoscopic submucosal dissection (ESD) ulcer shows no definite evidence of endoscopically proven perforation. (B) Follow-up X-ray taken right after the completion of ESD shows a large amount of pneumoperitoneum, which means the presence of microperforation at the ESD ulcer bed.
MANAGEMENT OF PERFORATION
Surgical management
Surgery has been the mainstay of management of colonic perforation. Recently, endoscopic clipping has been introduced and conservative management has been feasible in many perforation cases. However, surgery is still indicated in cases of large perforations, generalized peritonitis, aggravating peritonitis, ongoing sepsis, and concomitant colorectal pathology such as large advanced neoplasm which is difficult to resect by endoscopic techniques.5 One study showed diagnostic colonoscopy-associated perforation or large perforation, leukocytosis over 10,000/mm3, fever ≥37℃, severe abdominal pain, and large amount of free air in peritoneal cavity ≥3 cm might be risk factors for surgery within 24 hours after colonoscopic clip closure trial.18 Therefore, patients with these factors should be observed closely after the initiation of medical management by clipping and emergency surgery should be considered when patients show clinical deterioration such as generalized peritonitis.
Endoscopic management
Endoscopic management of colonic perforation has progressed significantly since the first report of clip application by Yoshikane et al.19 Through the scope clips have been used in clinical practice for decades of years with satisfactory success rate for the management of colonoscopy-associated perforation (Fig. 3).16 They are especially useful in the closure of small perforations such as those developing after endoscopic mucosal resection or ESD of colorectal tumors. Large perforations may not be closed by through the scope clips only. Because diagnostic colonoscopy-associated perforation is usually larger than the therapeutic colonoscopy-associated perforation, overall clip success rate in the management of colon perforation appears to be higher in the therapeutic colonoscopy-associated perforation (Tables 1, 2).18,20,21 In case of closure failure with clipping, combination of clips with detachable snare (endoloop) can be useful for endoscopic closure.22 Recently, over the scope clips were reported to be useful for the management of large gastrointestinal perforations.23 A case series which investigated the usefulness of over-the-scope clip in the management of nine colon perforation cases showed successful deployment and closure in all of the nine perforations up to 30 mm in size. Out of those nine cases, six cases improved conservatively. The other three cases required laparoscopy for the inspection of possible peritonitis, but none of the three cases showed leakage or peritonitis. Therefore, the authors concluded that the over the scope clip may be useful for the endoscopic management of colon perforation up to 30 mm in size.24
Fig. 3.
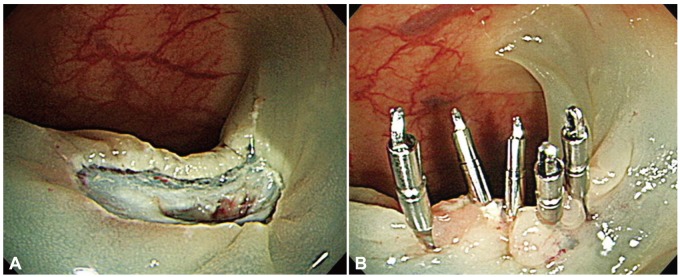
Endoscopic clipping. (A) A mural defect developed after endoscopic mucosal resection of colon polyp. (B) Five clips were applied and the perforation was closed completely.
Table 1.
Performance of Endoscopic Clipping in the Management of Diagnostic Colonoscopy-Associated Perforation
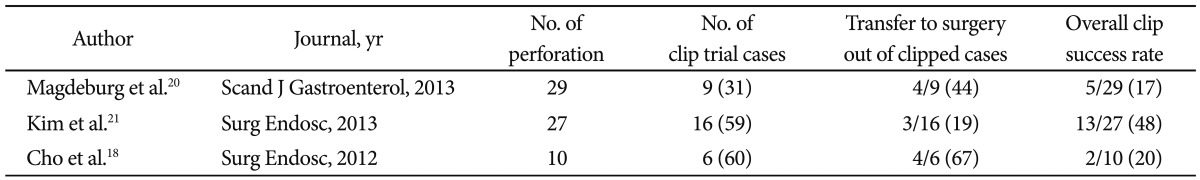
Values are presented as number (%).
Table 2.
Performance of Endoscopic Clipping in the Management of Therapeutic Colonoscopy-Associated Perforation
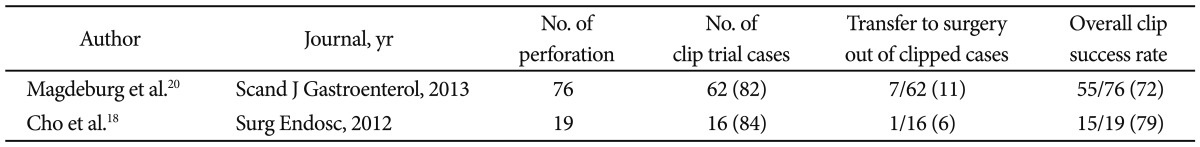
Values are presented as number (%).
For the successful endoscopic management of colonic perforations, adequate supportive measures should be provided with timely endoscopic clipping. They include nil per os, immediate intravenous antibiotics, and needle decompression of tension pneumoperitoneum. Tension pneumoperitoneum may lead to respiratory and circulatory compromise and air embolism through the portal venous system. Therefore, urgent decompression through the abdominal wall puncture by a large bore needle is important.5 In addition, to avoid serious peritonitis by the leakage of fecal material through the perforation site, endoscopists should remove all the residual feces, if possible, before attempting endoscopic resection of colorectal tumors.
In case of a radiologically proven perforation with no evidence of endoscopic perforation during colonoscopy, there is a debate on the necessity of the second look endoscopy with clipping trial. If the patient complains of little symptoms, conservative management only with nil per os and antibiotics may be sufficient. If the patient shows moderate abdominal pain, the second look endoscopy with clipping trial may be helpful. However, this approach does not have sufficient scientific evidence and requires further studies.
Despite recent progress in endoscopic management of colonoscopy-associated perforations, some perforations still need surgical interventions. In a colonoscopy-associated perforation study, of the 38 patients with perforations, 29 (76%) improved without surgery.16 However, surgical intervention was necessary in six of six (100%) endoscopically evident perforations in which endoscopic closure by clipping was not successful. Radiologically proven perforations, that is, delayed perforations whose perforation site was not detected during colonoscopy procedures, required surgical interventions in two of 10 patients (20%).16 In another colorectal ESD study, microperforations which were detected radiologically after the completion of ESD required longer hospital stay although they could be managed conservatively.25 Based on these studies, immediate endoscopic clipping appears to be important to avoid surgical management of colonoscopy-related perforations although it is not absolutely imperative.
CONCLUSIONS
Colonoscopy-associated perforations can be managed endoscopically if they can be closed by endoscopic clipping during colonoscopy. Some radiologically proven colonoscopy-associated perforations may be managed conservatively without endoscopic clipping. Therefore, cautious management by intense medical therapy may be warranted in colonoscopy-related perforations if they are not clinically deteriorated. Emergency surgery should be performed if patients show clinical deterioration.
Footnotes
The author has no financial conflicts of interest.
References
- 1.Vincent M, Smith LE. Management of perforation due to colonoscopy. Dis Colon Rectum. 1983;26:61–63. doi: 10.1007/BF02554687. [DOI] [PubMed] [Google Scholar]
- 2.Lo AY, Beaton HL. Selective management of colonoscopic perforations. J Am Coll Surg. 1994;179:333–337. [PubMed] [Google Scholar]
- 3.Jentschura D, Raute M, Winter J, Henkel T, Kraus M, Manegold BC. Complications in endoscopy of the lower gastrointestinal tract. Therapy and prognosis. Surg Endosc. 1994;8:672–676. doi: 10.1007/BF00678564. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal CW, Chun YS, Farley DR. Colonoscopic perforations: a retrospective review. J Gastrointest Surg. 2005;9:1229–1235. doi: 10.1016/j.gassur.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Raju GS, Saito Y, Matsuda T, Kaltenbach T, Soetikno R. Endoscopic management of colonoscopic perforations (with videos) Gastrointest Endosc. 2011;74:1380–1388. doi: 10.1016/j.gie.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Fujishiro M, Yahagi N, Nakamura M, et al. Endoscopic submucosal dissection for rectal epithelial neoplasia. Endoscopy. 2006;38:493–497. doi: 10.1055/s-2006-925398. [DOI] [PubMed] [Google Scholar]
- 7.Onozato Y, Kakizaki S, Ishihara H, et al. Endoscopic submucosal dissection for rectal tumors. Endoscopy. 2007;39:423–427. doi: 10.1055/s-2007-966237. [DOI] [PubMed] [Google Scholar]
- 8.Tamegai Y, Saito Y, Masaki N, et al. Endoscopic submucosal dissection: a safe technique for colorectal tumors. Endoscopy. 2007;39:418–422. doi: 10.1055/s-2007-966427. [DOI] [PubMed] [Google Scholar]
- 9.Saito Y, Uraoka T, Matsuda T, et al. Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video) Gastrointest Endosc. 2007;66:966–973. doi: 10.1016/j.gie.2007.02.053. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka S, Oka S, Kaneko I, et al. Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc. 2007;66:100–107. doi: 10.1016/j.gie.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 11.Byeon JS, Yang DH, Kim KJ, et al. Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc. 2011;74:1075–1083. doi: 10.1016/j.gie.2011.03.1248. [DOI] [PubMed] [Google Scholar]
- 12.Zhou PH, Yao LQ, Qin XY. Endoscopic submucosal dissection for colorectal epithelial neoplasm. Surg Endosc. 2009;23:1546–1551. doi: 10.1007/s00464-009-0395-5. [DOI] [PubMed] [Google Scholar]
- 13.Nishiyama H, Isomoto H, Yamaguchi N, et al. Endoscopic submucosal dissection for colorectal epithelial neoplasms. Dis Colon Rectum. 2010;53:161–168. doi: 10.1007/DCR.0b013e3181b78cb6. [DOI] [PubMed] [Google Scholar]
- 14.Kim ES, Cho KB, Park KS, et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011;43:573–578. doi: 10.1055/s-0030-1256339. [DOI] [PubMed] [Google Scholar]
- 15.Lee EJ, Lee JB, Choi YS, et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc. 2012;26:1587–1594. doi: 10.1007/s00464-011-2075-5. [DOI] [PubMed] [Google Scholar]
- 16.Yang DH, Byeon JS, Lee KH, et al. Is endoscopic closure with clips effective for both diagnostic and therapeutic colonoscopy-associated bowel perforation? Surg Endosc. 2010;24:1177–1185. doi: 10.1007/s00464-009-0746-2. [DOI] [PubMed] [Google Scholar]
- 17.Swan MP, Bourke MJ, Moss A, Williams SJ, Hopper A, Metz A. The target sign: an endoscopic marker for the resection of the muscularis propria and potential perforation during colonic endoscopic mucosal resection. Gastrointest Endosc. 2011;73:79–85. doi: 10.1016/j.gie.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 18.Cho SB, Lee WS, Joo YE, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc. 2012;26:473–479. doi: 10.1007/s00464-011-1903-y. [DOI] [PubMed] [Google Scholar]
- 19.Yoshikane H, Hidano H, Sakakibara A, et al. Endoscopic repair by clipping of iatrogenic colonic perforation. Gastrointest Endosc. 1997;46:464–466. doi: 10.1016/s0016-5107(97)70045-2. [DOI] [PubMed] [Google Scholar]
- 20.Magdeburg R, Sold M, Post S, Kaehler G. Differences in the endoscopic closure of colonic perforation due to diagnostic or therapeutic colonoscopy. Scand J Gastroenterol. 2013;48:862–867. doi: 10.3109/00365521.2013.793737. [DOI] [PubMed] [Google Scholar]
- 21.Kim JS, Kim BW, Kim JI, et al. Endoscopic clip closure versus surgery for the treatment of iatrogenic colon perforations developed during diagnostic colonoscopy: a review of 115,285 patients. Surg Endosc. 2013;27:501–504. doi: 10.1007/s00464-012-2465-3. [DOI] [PubMed] [Google Scholar]
- 22.Mocciaro F, Curcio G, Tarantino I, et al. Tulip bundle technique and fibrin glue injection: unusual treatment of colonic perforation. World J Gastroenterol. 2011;17:1088–1090. doi: 10.3748/wjg.v17.i8.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos) Gastrointest Endosc. 2010;72:881–886. doi: 10.1016/j.gie.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Gubler C, Bauerfeind P. Endoscopic closure of iatrogenic gastrointestinal tract perforations with the over-the-scope clip. Digestion. 2012;85:302–307. doi: 10.1159/000336509. [DOI] [PubMed] [Google Scholar]
- 25.Yoon JY, Kim JH, Lee JY, et al. Clinical outcomes for patients with perforations during endoscopic submucosal dissection of laterally spreading tumors of the colorectum. Surg Endosc. 2013;27:487–493. doi: 10.1007/s00464-012-2462-6. [DOI] [PubMed] [Google Scholar]