Abstract
Individuals react in a variety of ways when experiencing environmental challenges exceeding their capacity to cope adaptively. Some researchers have suggested that Asian populations tend to react to excessive stress with somatic symptoms whereas Western populations tend to respond more with affective or depressive symptoms. Other researchers, however, have suggested that such differences may represent different approaches to help-seeking rather than actual variations in prevalence. In the present study we compared somatic versus affective symptoms in American and Thai children, from community and mental health clinic samples. In the clinic sample, Thai children were reported to have higher levels of somatic versus depressive symptoms relative to American children, whereas in the community sample both groups were reported to have slightly higher levels of depressive than somatic symptoms. Since a primary difference between clinic and community samples is that the former have been through the clinical referral process (i.e., were seeking help), these results suggest that differences in somatic vs. depressive symptom presentation may be related to help-seeking behavior, at least for the samples involved in this study.
Keywords: somatization, Asian populations, neurasthenia, psychologization
There is considerable diversity in how humans react when environmental demands exceed their capacity to adaptively cope. Reactions can range from maladaptive behaviors such as substance abuse and aggression to anxiety, depression, and somatization, and at least part of this variability in response likely is related to cultural factors (e.g., Wong & Wong, 2006). If psychology is to be a science of universal human behavior, describing this diversity and the factors that underlie it is essential; however, for the most part psychological research has been limited to Western countries and cultures (Arnett, 2008).
One possible cultural difference in symptom manifestation was first highlighted by Kleinman (1977), who found that 88% of Taiwanese psychiatric patients in his sample initially reported somatic complaints without affective complaints, whereas the comparable figure for European-Americans was 20%. Kleinman hypothesized that Asian populations may tend to respond to stressful life events in ways that emphasize somatic rather than depressive symptoms, because depressive symptoms may be experienced by Asian populations as more self-centered and hence more disruptive to group harmony than somatic symptoms. Support for this position is found in research on neurasthenia, which is a psychiatric diagnosis that emphasizes somatic symptoms (e.g., fatigue; diffuse aches and pains), and is the most widely used diagnosis by psychiatrists in China but is seldom used in the U.S. (Parker, Gladstone & Tsee-Chee, 2001).
However, an alternative perspective has been suggested, that Western and Asian differences in somatization and affective symptoms reflect differences in help-seeking behavior rather than actual prevalence differences, with somatic complaints seen as more likely than affective symptoms to gain access to treatment services in developing countries. To best evaluate the hypothesis, community and clinic-referred samples should be compared, to determine the extent that differential problem rates between depressive and somatization symptoms vary as a function of whether individuals are seeking help for mental health problems. Yen, Robins and Lin (2000), for example, compared mental health outpatient Chinese students with non-referred Chinese students, as well as Chinese, Chinese-American, and European-American college students on “Somatic” and “Affective” factors. They concluded that reporting of somatic symptoms was not any greater among Chinese populations but that this tendency may be influenced by help seeking in China. However, no European-American clinic-referred sample was assessed and hence no clinic-referred/community sample comparison was possible among the European-Americans, which would be necessary to fully evaluate the hypothesis. Further, the “Affective” and “Somatic” factors used in this study did not fit theoretical conceptions regarding depressive affect, and somatic complaints and neurasthenia very well (e.g., two items that clearly reflected depressive affect had strong loadings on the “Somatic” factor).
To test the hypothesis that higher rates of somatic symptoms among Asian populations represent help seeking behavior, the present study determined whether rates of somatic vs. depressive symptoms were higher among Thai vs. American children for clinic-referred but not community samples. We used design enhancements to address limitations of previous research, with these enhancements including (a) use of a comprehensive of measure of psychopathology, (b) a fully crossed design in regards ethnic group and type of sample (referred vs. non-referred), and (c) a large sample size. We focused on children and adolescents to assess how these social processes might unfold across early stages of development, hypothesizing that cross-cultural effects on depressive vs. somatic symptoms would be smaller among adolescents because adults may tend to be more tolerant of younger children violating cultural expectations (e.g., displaying affective symptoms). Our Asian sample was obtained from Thailand, allowing for a strong test of these hypotheses because Thailand and the U.S. differ substantially in religious and cultural practices and beliefs that might underlie differences in symptom manifestation (Klausner, 2000).
Methods
Participants
Data for U.S. participants were obtained from clinical and normative datasets for the parent-report Child Behavior Checklist (Achenbach, 1991). These included data for 1,834 clinic-referred and 1,834 non-referred U.S. children (6–11 years) and adolescents (12–17). U.S. clinic-referred participants were obtained from 52 clinics across the U.S., with a broad distribution of socio-economic and demographic characteristics (Achenbach, 1991). U.S. community participants were selected to be representative of the U.S. population with respect to ethnicity, SES, geographic region of the 48 contiguous states, and urban, suburban, or rural residence.
Data for Thai participants were obtained from clinic and community studies of the Thai Youth Checklist (Weisz et al., 1993). These data included 1,927 clinic-referred and 768 non-referred Thai children and adolescents, whose symptoms were reported upon by their parents. Thai clinic-referred participants were obtained from six mental health clinics and programs from urban and rural locations across Thailand. Thai community participants were obtained from urban, suburban, and semi-rural environments in the five major regions of Thailand. The Thai sample selection and data collection were structured to parallel U.S. CBCL data collection procedures (Weisz et al., 1993). For the U.S. participants, the mean age of the children was 11.30 (3.27) years, and 49% were male; for the Thai participants, the mean age was 11.45 (3.27) years, and 52% were male (see Table 1 for demographics for the samples).
Table 1.
Comparison of Thai and U.S. samples on demographic and clinical characteristics
| Factor | Sample | NationalityMean (S.D.) or % | Effect size (95% CI)1 | |
|---|---|---|---|---|
| Age | Clinic | Thai | 11.35 (3.19) | 0.02 (−.02 ~ .05) |
| U.S. | 11.30 (3.27) | |||
| Community | Thai | 11.69 (3.44) | 0.12 (.08 ~ .16)** | |
| U.S. | 11.30 (3.27) | |||
| CBCL total | Clinic | Thai | 52.63 (26.56) | −.03 (−.06 ~ .00) |
| U.S. | 53.46 (27.09) | |||
| Community | Thai | 21.56 (13.90) | −.15 (−.19 ~ −.11)*** | |
| U.S. | 23.95 (16.47) | |||
| SES2 | Clinic | Thai | 4.47 (2.70) | −.22 (−.25 ~ −.19)*** |
| U.S. | 5.04 (2.45) | |||
| Community | Thai | 4.43 (2.40) | −.51 (−.54 ~ −.47) *** | |
| U.S. | 5.57 (2.20) | |||
| Gender3 | Clinic | Thai | 52% | 0.04 (.01 ~ .07)* |
| U.S. | 49% | |||
| Community | Thai | 50% | 0.01 (−.03 ~ .05) | |
| U.S. | 49% | |||
| Ethnicity | Clinic | Thai | Thai | 98% 0.70 (.68 ~ .72) *** |
| Other Asian | 2% | |||
| U.S. | African-American | 13% | ||
| Asian | 2% | |||
| Euro-American | 80% | |||
| Hispanic | 0% | |||
| Community | Thai | Thai | 99% 0.71 (.69 ~ .73) *** | |
| Other Asian | 1% | |||
| U.S. | African-American | 16% | ||
| Asian | 2% | |||
| Euro-American | 73% | |||
| Hispanic | 6% | |||
Notes.
Effect sizes for Thai vs. U.S. comparisons, continuous variables are z-scores, categorical variables are contingency coefficients, CI= 95% Confidence Interval;
= p<.05;
= p<.01;
= p<.001;
: SES is based on the Hollingshead’s nine-step scale used by Achenbach (1991) to rate SES based on parent occupation. We make no assumption about the validity of the Hollingshead scale for non-U.S. cultures. Our purpose here was to assess differences in parent occupation across the two national samples, which required that we use the same rating system used previously for U.S. CBCL samples.
: Gender is percent male.
Measures
Child Behavior Checklist
Child psychopathology data were obtained using the parent-report Child Behavior Checklist (CBCL; Achenbach, 1991), a 118-item checklist covering a wide range of child emotional and behavioral problems. Parents report whether their child has each problem on a 3 point scale ranging from “Not True” to “Very True or Often True.” Reliability and validity of this measure are well established (Achenbach, 1991).
Thai Youth Checklist
Thai psychopathology data were obtained using the parent-report Thai Youth Checklist (TYC), a Thai-language version of the CBCL (when referring to the two measures collectively, in this report we refer to the ‘CBCL’). CBCL items were translated into Thai through three waves of translation and back-translation, aiming for linguistic parallels and simplicity of expression. All CBCL / TYC items refer to behaviors also seen in Thai children, and the translation is readily understood by Thai parents (Weisz et al., 1993).
Dependent variables
To evaluate our hypotheses, items from the CBCL and TYC were used to derive (a) a neurasthenia factor, and (b) a depression factor. An initial pool of symptoms was obtained from diagnostic criteria for Neurasthenia (ICD-10, F48.0) and for Major Depressive Disorder (DSM-IV-TR, 296.2). Symptoms overlapping across the two scales were dropped although overlapping items core to a syndrome as defined by the diagnostic criteria (fatigue for neurasthenia; sadness, irritability and anhedonia for depression) were retained for the syndrome for which they were core. CBCL items then were identified for these symptoms. For the neurasthenia scale, these were: fatigue (#54), dizziness (#51), aches and pains (#56a), headaches (#56b), gastrointestinal problems (#56c, #56f, #56g), and inability to relax (#45). For the depression scale, these were: depressed mood (#103), irritability (#86), anhedonia (no CBCL item covered this symptom), weight or appetite problems (#24, #53, #55), sleep problems (#76, #77, #100), psychomotor problems (#102), feelings of worthlessness or excessive guilt (#35 and #52, respectively), concentration problems (#8), and suicidal ideation or behavior (#91 and #18).
Factor analysis
We next conducted a factor analysis with the clinic-referred samples to determine the actual structure for these items. We did not want to weight analyses by the number of CBCL items representing a particular symptom (e.g., three CBCL items involve sleep problems whereas one CBCL item involves sadness), so for each symptom area (e.g., sleep problems; sadness) we computed and analyzed the mean of the underlying CBCL items, generating item “parcels” for these symptoms. Because we had selected items on a theoretical basis, we considered using a confirmatory factor analysis. However, because our item-level CBCL data were neither normally distributed nor interval level, we conducted an exploratory factor analysis with unweighted least squares estimation (which is less dependent on the data distribution) with a loading criterion of .40 on the factor structure, and a promax rotation of the two factors. This analysis produced a neurasthenia factor (see Table 2)1 with symptom parcels Dizzy, Fatigued, Aches and Pains, Headaches, and GI Problems as well as a depression syndrome with symptom parcels Affect, Low Self-esteem and Worthlessness, and Suicidal Ideation and Behavior. To assess the adequacy of the fit, we computed confirmatory factor analysis fit statistics, which were non-normed index=.93, normed fit index=0.95, and RMSEA=0.06, indicating good fit (Kline, 2004).
Table 2.
Factor loadings, and parcel items
| Symptom | Parcel items | Factor 1 loadings (Neurasthenia) |
Factor 2 loadings (Depression) |
|---|---|---|---|
| Dizzy | 51 | 0.63 | 0.18 |
| Fatigue | 54 | 0.45 | 0.36 |
| Pains | 56a | 0.62 | 0.24 |
| Headaches | 56b | 0.75 | 0.19 |
| GI problems | 56c, 56f, 56g | 0.65 | 0.25 |
| Concentration problems | 8 | 0.05 | 0.33 |
| Psychomotor problems | 10, 102 | 0.32 | 0.31 |
| Suicide | 18, 91 | 0.18 | 0.40 |
| Appetite / weight | 24, 53, 55 | 0.31 | 0.33 |
| Worthless, guilty | 35, 52 | 0.24 | 0.61 |
| Affect | 86, 103 | 0.27 | 0.72 |
Note: The two factors were correlated .35.
Results
Tests of background characteristics
We compared community and clinic Thai and U.S. samples on age, gender, SES, total CBCL score, and ethnicity. The Thai and U.S. community samples differed significantly on age and total CBCL score (see Table 1); in the clinic samples the two groups differed on sex. As expected, the Thai and U.S. differed significantly in both samples on ethnicity and SES. Consequently our main analyses were conducted twice, once with no covariates, and once with SES and total CBCL score as covariates (age and sex were already included in our models). Total CBCL was nested within sample (community vs. clinic) since differences in total problem level represented a fundamental difference between the community and clinic samples. Inclusion of SES and total CBCL score resulted in minimal differences, therefore for simplicity’s sake we report results without these variables in the models.
Main analyses
We first conducted a repeated measures profile analysis with Ethnicity (Thai vs. U.S.), Source (community vs. clinic-referred), Age Group (child vs. adolescent) and Gender as independent variables, and the contrast between Depressive Symptoms and Neurasthenia Symptoms as the dependent variable, representing the within-subjects effect of Domain of Psychopathology.2 Based on the “cultural help-seeking behavior” hypothesis we predicted that the Domain of Psychopathology × Ethnicity × Source interaction would be significant, reflecting a greater difference in the Domain contrast (depressive minus neurasthenia symptoms) for the Thai vs. U.S. comparison in the clinic-referred vs. community sample. That is, we predicted that differences between the Thai and U.S. participants in regards to the depressive minus neurasthenia symptoms contrast would be greater in the clinic sample than in the community sample, with the Thai sample showing relatively higher levels of neurasthenia symptoms in the clinic sample. This 3-way interaction was significant, F(1,6347)=244.85, p<.0001. In addition, the Domain of Psychopathology × Ethnicity × Source × Age interaction also was significant F(1,6347)=4.53, p<.05. This latter interaction reflected differences in the Domain of Psychopathology × Source × Ethnicity interaction across adolescents (F[1,3137]=86.16, p<.0001) vs. children (F[1,3218]=161.42, p<.0001), with the hypothesis thus confirmed for both adolescents and children but more strongly so for children.
Interaction breakdown
We broke down the Domain of Psychopathology × Source × Ethnicity interactions by assessing the Ethnicity × Domain of Psychopathology interactions in the clinic and community samples, separately for the children and for the adolescents. For the clinic sample children, the effect of Domain of Psychopathology × Ethnic Group was significant (see Table 3), with the Depressive vs. Neurasthenia symptom contrast positive for the U.S. children and negative for the Thai children (see Table 4); i.e., in the clinic sample U.S. parents reported higher levels of depressive symptoms whereas Thai parents reported higher levels of neurasthenia symptoms. A similar significant effect, although a little smaller, was found for the clinic sample adolescents (see Tables 3 and 4). For the community sample, in contrast, the Domain × Ethnic Group interaction was not significant for either children or adolescents, indicating that the Thai and U.S. parents were reporting similar relative levels of neurasthenia vs. depressive symptoms. Z-score effect size estimates (and 95% confidence intervals) for the Domain of Psychopathology × Source × Ethnicity interactions (the effect testing our hypothesis) for children and adolescents were, respectively, z=.85 (.82 – .88) and z=.63 (.60 – .66).
Table 3.
Effects underlying significant Source × Domain × Ethnic interactions in children and adolescents
| Clinic sample | |||
| Age Group | Source | DF | F |
| Adolescents | Domain | 1, 1846 | 49.18**** |
| Domain*Ethnic | 1, 1846 | 155.69**** | |
| Children | Domain | 1, 1911 | 59.36**** |
| Domain*Ethnic | 1, 1911 | 318.23**** | |
| Community sample | |||
| Age Group | Source | DF | F |
| Adolescents | Domain | 1, 1291 | 2.77 |
| Domain*Ethnic | 1, 1291 | 0.09 | |
| Children | Domain | 1, 1307 | 30.62**** |
| Domain*Ethnic | 1, 1307 | 0.11 | |
Note:
= p < .0001
Table 4.
Means and standard deviations, by source, age group and ethnicity
| Adolescents | |||||
| Source | Nationality | Domain | Mean (s.d.) | Contrast (s.d.)1 | Effect size (CI)2 |
| Clinic | Thai | Depressive | .52 (.40) | −.06 (.51) | 0.63 (.58 ~ .68) |
| Neurasthenia | .58 (.48) | ||||
| U.S. | Depressive | .59 (.39) | .22 (.43) | ||
| Neurasthenia | .37 (.40) | ||||
| Community | Thai | Depressive | .16 (.18) | .01 (.24) | 0.00 (−.05 ~ .05) |
| Neurasthenia | .15 (.20) | ||||
| U.S. | Depressive | .19 (.22) | .01 (.26) | ||
| Neurasthenia | .18 (.25) | ||||
| Children | |||||
| Source | Nationality | Domain | Mean (s.d.) | Contrast (s.d.) | Effect size (CI) |
| Clinic | Thai | Depressive | .42 (.33) | −.10 (.47) | 0.85 (.81 ~ .89) |
| Neurasthenia | .52 (.47) | ||||
| U.S. | Depressive | .53 (.38) | .26 (.41) | ||
| Neurasthenia | .27 (.34) | ||||
| Community | Thai | Depressive | .19 (.18) | .04 (.24) | 0.00 (−.05 ~ .05) |
| Neurasthenia | .14 (.21) | ||||
| U.S. | Depressive | .17 (.19) | .04 (.24) | ||
| Neurasthenia | .13 (.21) | ||||
Notes.
: "Contrast" refers to the Depressive symptoms minus Neurasthenia symptoms contrast within ethnic group.
: Effect size is the standardized effect size for the Domain of Psychopathology × Ethnic Group interaction, within Source and Age group; CI = 95% confidence interval.
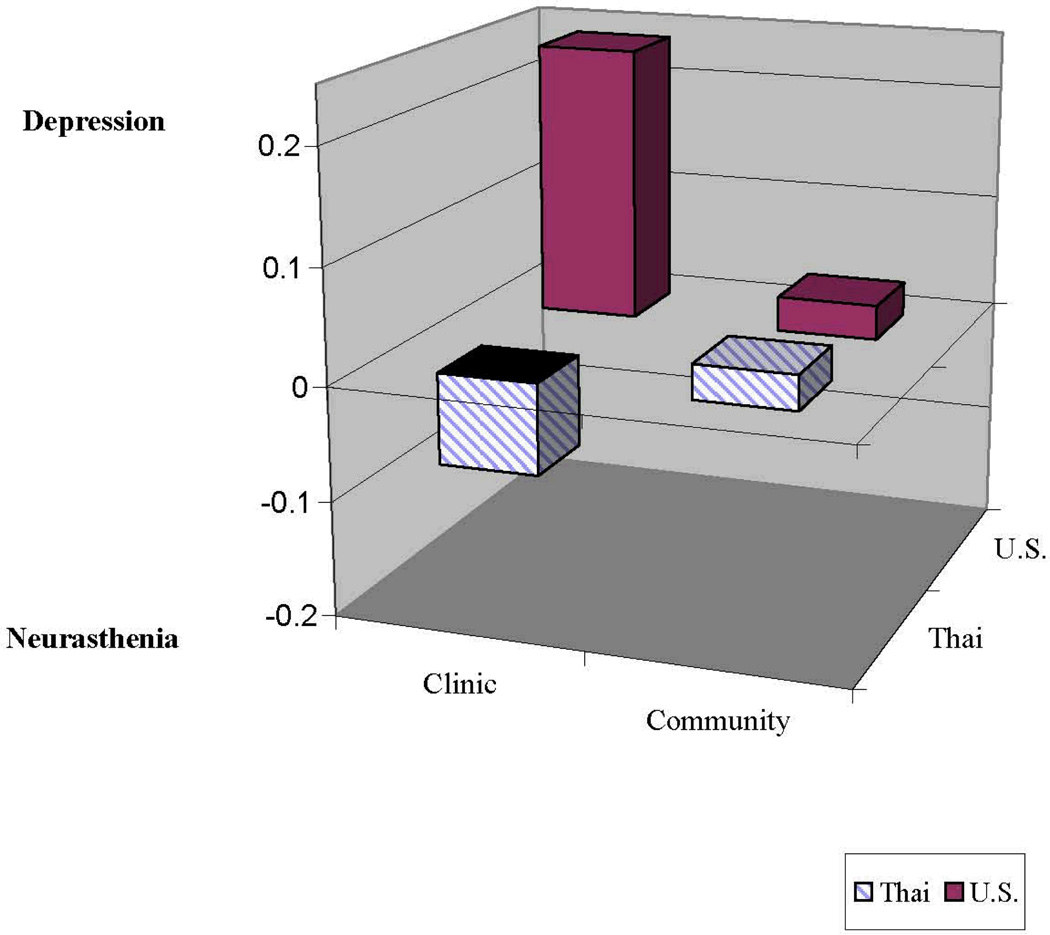
Figure 1 summarizes these results, collapsed across children and adolescents. In this figure, the z-axis represents the Depression – Neurasthenia contrast, with groups with their block above the 0 point having a positive mean contrast (i.e., reporting more depressive than neurasthenia symptoms), and groups with their block below the 0 point having a negative mean contrast (i.e., reporting more neurasthenia than depressive symptoms). The figure illustrates that in the clinic sample, Thai parents reported higher levels of neurasthenia symptoms whereas U.S. parents reported higher levels of depressive symptoms, but in the community sample both Thai and U.S. parents reported similar relative levels of depressive vs. neurasthenia symptoms.
Figure 1.
Contrast for depressive minus neurasthenia symptoms
Controlling for overall level of psychopathology
The Ethnicity × Domain of Psychopathology × Source (clinic vs. community samples) interaction reflects the fact that relations between ethnicity, and domain and level of psychopathology differ across the community and clinical samples. One possible difference between the community and clinical samples underlying this effect may be overall level of child psychopathology, which was much higher in the clinic than community sample. To evaluate whether these effects of Source might be due to differences in psychopathology levels, we reran our primary analysis including the main effect of total CBCL score as well as its interaction with ethnicity and domain of psychopathology. The value of the F test for the Domain of Psychopathology × Ethnicity × Source interaction decreased from 244.85 to 160.94 but remained significant (F[1,6345]=160.94, p<.0001. The fact that the F decreased approximately 33% but remained significant suggests that effects of Source vis-à-vis differential reporting were partially but not primarily due differences in overall levels of psychopathology. We also tested whether the Source (clinic vs. community samples) effect was due to differences in overall psychopathology level by testing the Domain of Psychopathology × Ethnicity interaction among community sample participants whose total CBCL score was above the 35th percentile for the clinic sample, which equated the community sample’s mean for total CBCL score with the clinic sample’s mean. This produced a community sample with 342 participants. In this sub-sample, we tested the Domain of Psychopathology × Ethnicity interaction, which was non-significant. The fact that we did find a significant Domain of Psychopathology × Ethnicity interaction in the clinic sample but not in the community sample when it was restricted to children and adolescents with psychopathology levels comparable to those in the clinic sample suggests that effects of Source are due to factors other than differences in overall psychopathology levels.
Discussion
Before discussing our findings we should note that although we selected Thailand for theoretical reasons, it still represents a single country from a diverse continent, and other cultures might produce different results. Our results are consistent with the hypothesis that when seeking clinical services Asian populations report higher levels of somatic problems relative to Western populations but that when not seeking services the two populations report similar levels of depressive vs. somatic symptoms; however, any conclusion about Asian and Western populations in general would certainly require data from Asian countries other than Thailand and Western countries other than the U.S.
However, differential rates between clinic and community samples may reflect not only differences in help-seeking behavior but also how worrisome, how treatable, etc. the various problems are seen to be (Weisz & Weiss, 1991). Thus, there are several possible explanations for our findings: Thai parents may be (a) more concerned about somatic symptoms relative to depressive affect symptoms and hence more likely to seek treatment for the somatic symptoms, (b) more likely to seek treatment for somatic symptoms because they view them as more likely to be successfully treated than affective symptoms, perhaps because the somatic symptoms are more congruent with their cultural conceptualizations of child problems, (c) view somatic symptoms as more socially acceptable reasons to seek treatment, or (d) view somatic symptoms as more likely to provide access to services. All of these possibilities potentially could lead to the observed higher rates of somatic symptoms reported for Thai clinical samples.
In considering these alternatives, it is important to note that the clinic-referred samples were obtained from mental health clinics, where one might expect a level of acceptance regarding depressive symptoms. It thus will be important to understand how stigma and social desirability operate (Sue & Chu, 2003) when reporting child symptoms to a stranger such as a research assistant vs. a mental health professional with whom one may have a helping relationship for a relatively extended period. Thus, another alternative explanation for our findings is that Thai parents were more open about affective symptoms with strangers with whom they knew that they would not have an ongoing relationship (i.e., when assessed as part of the community sample) in contrast to someone with whom they knew they likely would have an ongoing relationship.
The finding that the Thai and U.S. community samples did not differ significantly on depression vs. neurasthenia might seem contradictory to previous comparisons of U.S. and Thai children (e.g., Weisz et al., 1993) that have found some internalizing problems are more prevalent among Thai children. However, neurasthenia and depression are both internalizing problems and the higher overall levels of internalizing problems among Thai children apparently was not differential across sub-types (neurasthenia, depression) of internalizing problems.
In regards to clinical implications, these results highlight the importance of clinicians not taking presenting problems at face value, and this may be particularly true for families in or from lesser-developed countries. Results also emphasize the importance of understanding how parents view various mental health problems, as their beliefs and perceptions about the appropriateness, treatability, etc. of the problems may influence their reactions to the problems, and hence the treatment. Theoretically, our results suggest that an important part of understanding service access and mental health disparities will involve not only objective conditions but also personal beliefs, with cultural factors likely at least in part underlying these beliefs (Sue, 1991).
Our results are clear that the Thai and American clinical samples differed substantially in regards to depressive vs. neurasthenia symptoms whereas the community samples did not. Nonetheless, clinical implications and study limitations suggest areas where future research may be fruitful. For instance, we did not directly assess stigma or other attitudes towards mental health problems (cf., Ryder et al., 2008) such as treatability, and assessment of these factors and including them as covariates to determine whether such factors may underlie the differential symptom reports would be useful. Another limitation of the study was that our neurasthenia and depression factors were derived from the parent-report CBCL, and it is possible that we might obtain different results if these factors had included all of the precise symptoms defining them, and different results might have been obtained if other informants had been used. Finally, our sample sizes were large with sufficient power to detect small effects. Therefore, as effect size estimates we computed standardized scores for the difference between the Depressive / Neurasthenia symptoms contrast for the U.S. and Thai children; for the children z=.85, and for the adolescents, z=.63. Based on Cohen’s (1988) widely used definitions of small (.2), medium (.5), and large (.8) effect sizes, these effects appear substantial in size.
Acknowledgments
This research was supported in part of NIH grant D43 TW007769.
Footnotes
Although this process produced factors that were internally consistent, these factors were derived for specific theoretical purposes, to test the relations among specific sub-sets of CBCL items that were initially selected based on theoretical considerations. Thus, we are not suggesting that the CBCL be modified to fit the factors derived from these analyses.
We also conducted these analyses with the uncollapsed items (i.e., where each CBCL item was analyzed, rather than the symptom parcel). Although parameter estimates changed slightly, substantively results were unchanged.
Contributor Information
Bahr Weiss, Vanderbilt University.
Jane M. Tram, Pacific University
John R. Weisz, Harvard University and Judge Baker Children’s Center
Leslie Rescorla, Bryn Mawr College.
Thomas M. Achenbach, University of Vermont
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Arnett JJ. The Neglected 95%: Why American psychology needs to become less American. American Psychologist. 2008;63:602–614. doi: 10.1037/0003-066X.63.7.602. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum Associates; 1988. [Google Scholar]
- Klausner WJ. Reflections on Thai Culture. Bangkok: Siam Society; 2000. [Google Scholar]
- Kleinman A. Depression, somatization, and the"new cross-cultural psychiatry". Social Sciences and Medicine. 1977;11:3–10. doi: 10.1016/0037-7856(77)90138-x. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. NYC: Guildford Press; 2004. [Google Scholar]
- Parker G, Gladstone G, Tsee-Chee K. Depression in the planet's largest ethnic group: The Chinese. American Journal of Psychiatry. 2001;158:857–864. doi: 10.1176/appi.ajp.158.6.857. [DOI] [PubMed] [Google Scholar]
- Ryder AG, Yang J, Zhu X, Yao S, Yi J, Heine SJ, Bagby RM. The cultural shaping of depression: Somatic symptoms in China, psychological symptoms in North America? Journal of Abnormal Psychology. 2008;117:300–313. doi: 10.1037/0021-843X.117.2.300. [DOI] [PubMed] [Google Scholar]
- Sue S. Ethnicity and culture in psychological research and practice. In: Goodchilds JD, editor. Psychological perspectives on human diversity in America. Washington, DC: American Psychological Association; 1991. pp. 47–85. [Google Scholar]
- Sue S, Chu JY. The mental health of ethnic minority groups: Challenges posed by the supplement to the Surgeon General's report on mental health. Culture, Medicine and Psychiatry. 2003;27:447–465. doi: 10.1023/b:medi.0000005483.80655.15. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Suwanlert S, Chaiyasit W, Weiss B, Achenbach TM. Epidemiology of behavioral and emotional problems among Thai and American children: Parent reports for ages 12–16. Journal of Abnormal Psychology. 1993;102:395–403. doi: 10.1037//0021-843x.102.3.395. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Weiss B. Studying the "Referability" of child clinical problems. Journal of Consulting and Clinical Psychology. 1991;59:266–273. doi: 10.1037//0022-006x.59.2.266. [DOI] [PubMed] [Google Scholar]
- Wong PTP, Wong LCJ. Handbook of multicultural perspectives on stress and coping. Dallas: Spring Publications; 2006. [Google Scholar]
- Yen S, Robins CJ, Lin N. A cross-cultural comparison of depressive symptom manifestation: China and the United States. Journal of Consulting and Clinical Psychology. 2000;68:993–999. doi: 10.1037//0022-006x.68.6.993. [DOI] [PubMed] [Google Scholar]