Abstract
Background:
Soft-tissue releases are commonly necessary to achieve symmetrical flexion and extension gaps in primary total knee arthroplasty performed with a measured resection technique. We reviewed the frequency of required releases according to preoperative alignment and the clinical and radiographic results; associations with failure, reoperations, and complications are presented.
Methods:
We reviewed 1216 knees that underwent primary total knee arthroplasty from 2004 to 2009; 774 (64%) were in female patients and 442 (36%), in male patients. In the coronal plane, 855 knees had preoperative varus deformity, 123 were neutral, and 238 had valgus deformity. The mean age at the time of the index procedure was 62.7 years (range, twenty-three to ninety-four years), and the mean body mass index was 32.7 kg/m2 (range, 17.4 to 87.9 kg/m2). Clinical outcomes included the Knee Society Score (KSS), implant failure, reoperation, and complications. Radiographs were analyzed for component alignment.
Results:
The only difference in the total KSS was found at the time of final follow-up between valgus knees with zero releases (total KSS = 178) and those with one or two releases (KSS = 160, p = 0.026). Overall, 407 knees (33.5%) required zero releases, 686 (56.4%) required oneor two releases, and 123 (10.1%) required three or more releases. Among varus knees, 37% required zero releases, 55% required one or two releases, and 7.5% required three or more releases. Among neutral knees, 39% required zero releases, 55% required one or two releases, and 5.7% required three or more releases. Only 17% of valgus knees required zero releases whereas 61% required one or two releases and 21.8% required three or more releases. Valgus knees required more releases than neutral or varus knees did (p < 0.001).
Conclusions:
Selective soft-tissue release for gap balancing in primary total knee arthroplasty is an effective technique that produced excellent clinical and radiographic results regardless of preoperative alignment. Consistent anatomic coronal-plane alignment and soft-tissue balance could be achieved without bone cut modification by using measured bone resection and selective soft-tissue release.
There is general agreement that a balanced soft-tissue envelope is a prerequisite for successful total knee arthroplasty (TKA). For several decades, Whiteside and others have emphasized the concept of selective rather than global release of tight soft-tissue structures to achieve a balanced total knee arthroplasty1-6. It is well known that techniques for performing total knee arthroplasty vary widely, but all have the desired end result of a pain-free, long-lasting, highly functional joint. The preferred method of achieving balanced flexion and extension gaps is controversial and includes full or partial release of soft tissue to facilitate attainment of a neutral mechanical axis, alteration of femoral and tibial bone cuts to accommodate the existing or pre-released soft tissues, or a combination thereof. Measured resection and gap balancing are the two most commonly employed techniques for performing the bone cuts in total knee arthroplasty7-10.
The principle of total knee arthroplasty performed with measured-resection bone cuts involves performing global or selective soft-tissue releases to produce equal or balanced flexion and extension gaps and a neutral mechanical axis. Femoral component external rotation should be parallel to the epicondylar axis, and the anteroposterior position, or size, of the femoral component can be determined with either anterior or posterior referencing7,11-13. Tibial component alignment is perpendicular to the long axis of the tibia in the coronal plane, 3° to 7° of posterior slope in the sagittal plane, and rotation equivalent to the center of the ankle. Selective or global release of tight medial and lateral soft-tissue structures is used to produce balanced flexion and extension gaps after bone preparation. Retention or substitution of the posterior cruciate ligament (PCL) are additional methods to provide posterior stability after total knee arthroplasty; for surgeons who prefer to retain the PCL, the decision to retain or substitute may be based on the ability to balance the PCL14,15. Methods for fixation of implants in total knee arthroplasty may include cemented, cementless, or hybrid fixation, and any of these may be utilized regardless of the chosen soft-tissue balancing techniques.
For over eight years, we have prospectively recorded the soft-tissue releases required at surgery to produce balanced flexion and extension gaps in primary total knee arthroplasty performed with a standard measured resection technique for bone preparation. The required releases and the clinical and radiographic results during this time period are presented.
The purpose of this study was to assess which soft-tissue structures were released, the quantity and frequency of releases, and the differences among releases performed in varus, valgus, and neutral knees. We also sought to determine whether there was a relationship between soft-tissue release and outcomes including alignment, the clinical outcome, complications, and revisions.
Materials and Methods
Patients
After receiving an exemption from the university’s institutional review board, we retrospectively reviewed a consecutive series of 1216 knees that underwent primary total knee arthroplasty. The arthroplasties were performed by a single senior surgeon (C.L.P.) at an academic medical center. Residents and fellows were involved in all cases, with the senior surgeon being responsible for the intraoperative balancing decisions. All primary total knee arthroplasties performed from 2004 to 2009 were included in the analysis (Fig. 1). Selective soft-tissue releases were performed intraoperatively to achieve soft-tissue balance as described below. The goal for coronal alignment was an anatomic axis of 5° of valgus on short radiographs and a mechanical axis (hip-knee-ankle angle) of 0° on long standing radiographs. Intraoperative selective soft-tissue releases were recorded prospectively in a surgical database by one of the authors.
Fig. 1.
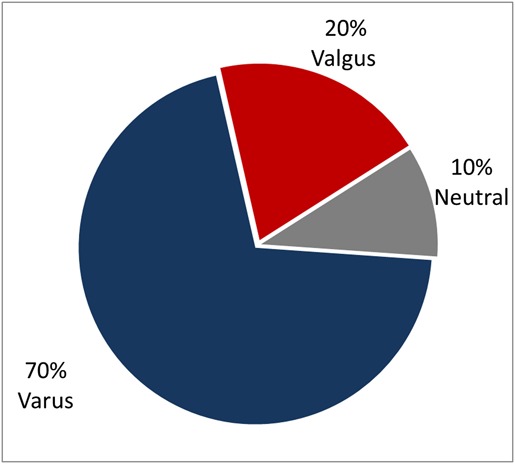
Pie chart showing the distribution of varus, valgus, and neutral preoperative alignment.
The procedure was unilateral in 1142 knees (94%) and simultaneous bilateral in seventy-four knees (6%) in thirty-seven patients. Of the 1216 knees, 774 (64%) were in female patients and 442 (36%) were in male patients. The reason for total knee arthroplasty and other demographic information are presented in Tables I and II.
TABLE I.
Diagnoses
| Preoperative Diagnosis | No.* (%) |
| Osteoarthritis | 1130 (93) |
| Posttraumatic arthritis | 40 (3) |
| Rheumatoid arthritis | 35 (3) |
| Osteonecrosis | 9 (1) |
| Other | 5 (0.4) |
The total is 1219 rather than 1216 because patients could have more than one diagnosis.
TABLE II.
Demographics
| Parameter | Mean | Range | Std. Dev. |
| Age (yr) | 62.7 | 23-94 | 10.96 |
| Height (cm) | 169 | 127-206 | 11 |
| Body mass index (kg/m2) | 32.7 | 17.4-87.9 | 7.98 |
| Tourniquet time (min) | 59.7 | 0-120 | 12.62 |
| Estimated blood loss (mL) | 122.9 | 40-800 | 65.8 |
| Soft-tissue releases per knee | 1.1 | 0-5 | 1.02 |
Soft-Tissue Balancing Technique
The surgeon’s preferred approach to primary total knee arthroplasty is a medially based midline incision with a medial parapatellar arthrotomy. The patella is prepared first and is left uneverted for the remainder of the operation. An initial medial release of the deep medial collateral ligament (MCL) to the midsagittal line of the tibia is performed as part of the initial exposure. After bone preparation with measured resection bone cuts (using posterior referencing), the symmetry of the flexion and extension gaps is evaluated with trial components in place. Further selective MCL, lateral collateral ligament (LCL), and PCL soft-tissue releases are performed to achieve balanced rectangular gaps. Patterns of required releases associated with preoperative limb alignment are described below.
Varus, Valgus, and Neutral Knees
The most common finding in a varus knee is residual medial tightness present in extension. In this instance, a selective release involving the posterior oblique MCL fibers and semimembranosus is performed with the trial components in place. Selective release of the anterior fibers of the deep MCL is performed for medial tightness in flexion as previously described by Whiteside et al.6. Residual lateral tightness in flexion occurs in 10% to 15% of varus knees, for which selective release of the popliteus with or without release of the PCL is indicated.
In a valgus knee, residual lateral tightness in flexion requires selective release of the popliteus tendon, and in some cases selective release of the PCL16,17. Residual lateral tightness in extension can be balanced by selective release of the iliotibial band (full or fractional release, depending on the amount of deformity). If required to relieve lateral tightness in flexion, release of the lateral posterior capsule off the posterior aspect of the femur can be performed. Rarely, further lateral tightness may be balanced with release of the LCL.
Balancing a neutral knee follows the same concepts as described in varus and valgus knees. Gap balancing is performed after measured resection bone cuts with the total knee arthroplasty trial implants in place.
The PCL
PCL retention was our preferred technique. When the knee is tested with trial components in place and flexion-extension gaps are balanced and symmetric, the desired femorotibial contact point in the sagittal plane is in the middle of the tibia with the knee in 90° of flexion. PCL sacrifice and substitution is appropriate if the flexion space is symmetric (rectangular) but tight (unbalanced) relative to the extension gap. Alternatively, partial release of the PCL off the femur or tibia is preferred by some surgeons and was performed in a small minority of cases in this series.
Clinical and Radiographic Evaluation
Clinical evaluation was based on the Knee Society Score (KSS), which was complete for 630 of the 1216 knees in this series. Failure was defined as revision surgery of the femoral and/or tibial components. Reoperations and other complications were also recorded. Reoperations included irrigation and debridement, polyethylene exchange, and patellar revision. Closed manipulation for postoperative arthrofibrosis was recorded. Major complications were defined for this study as irrigation and debridement (deep and superficial), irrigation and debridement with polyethylene exchange, periprosthetic fracture, deep venous thrombosis, pulmonary embolism, patellar fracture, and death. Minor complications were defined as hematoma, cellulitis, incisional infection or stitch abscess (nonoperatively treated), blisters, postoperative bracing for ligament instability for six weeks, wound dehiscence (nonoperatively treated), and peroneal nerve dysfunction.
The preoperative coronal alignment was measured as the anatomic axis on short standing knee radiographs. Preoperative long standing hip-knee-ankle radiographs were obtained in some of the patients because of deformity but were not included in this analysis. The anatomic axis was again measured postoperatively on short standing radiographs18. The postoperative mechanical axis angle (hip-knee-ankle angle) was measured on long standing hip-knee-ankle radiographs when the quality of the radiograph was deemed adequate (eliminating those with substantial rotation or leg length discrepancy that altered alignment).
Statistical Analysis
Six types of outcome metrics were analyzed: revisions, manipulations, reoperations, complications (major and minor), KSS (clinical, functional, and total scores), and coronal alignment (the absolute change in coronal alignment in relation to the number of releases). Each metric was analyzed in knees with preoperative varus (<5° of valgus), valgus (>7° of valgus), and neutral (5° to 7° of valgus) alignment that had undergone zero, one or two, or at least three soft-tissue releases.
All of the statistical comparisons used a mixed-effects modeling approach, with knees clustered within patients. For continuous outcome variables, multivariate mixed-effects linear regression was used. For dichotomous outcomes, multivariate mixed-effects logistic regression was used. Covariates controlled for included age, body mass index (BMI), and diagnosis. For knee score outcomes collected at postoperative patient visits, the follow-up time from the surgery to the postoperative visit was added as another covariate in the models. Statistical analyses were performed with use of Stata statistical software (version 12; StataCorp, College Station, Texas).
Source of Funding
There was no external funding for this study.
Results
Rate of Release According to Preoperative Deformity
There were 407 knees (33.5%) that required no releases, 686 (56.4%) that required one or two releases, and 123 (10.1%) that required three or more releases (Fig. 2, Table III). More releases were required in valgus knees than in neutral or varus knees (p < 0.001) (Fig. 3). Among the varus knees, 37% required zero releases, 55% required one or two releases, and 7.5% required three or more releases (Fig. 4). Among neutral knees, 39% required zero releases, 55% required one or two releases, and 5.7% required three or more releases (Fig. 5). However, among valgus knees, fewer (17%) required zero releases, whereas 61% required one or two releases and 21.8% required three or more releases (Fig. 6). As demonstrated in Figure 7, patients with greater preoperative deformity required a greater number of releases to achieve a balanced knee at the time of the primary total knee arthroplasty. Patients with valgus deformity had 22.2% more releases than those with neutral alignment and 20.4% more than those with varus deformity (p < 0.001).
Fig. 2.
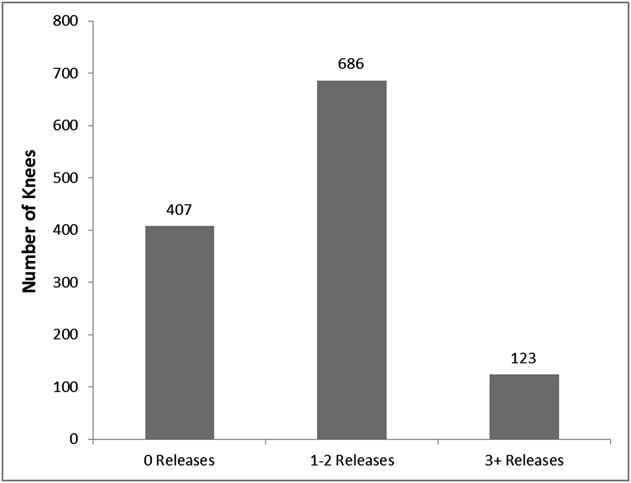
Bar graph showing the number of knees that required zero, one or two, and three or more releases.
TABLE III.
Number of Releases Required
| Preoperative Alignment |
||||
| Releases Required | Valgus* | Neutral† | Varus | All |
| 0 | 40 (17%) | 48 (39%) | 319 (37%) | 407 (33.5%) |
| 1-2 | 146 (61%) | 68 (55%) | 472 (55%) | 686 (56.4%) |
| ≥3 | 52 (21.8%) | 7 (5.7%) | 64 (7.5%) | 123 (10.1%) |
| All | 238 | 123 | 855 | 1216 |
P < 0.001 compared with varus and with neutral.
P = 0.74 compared with varus.
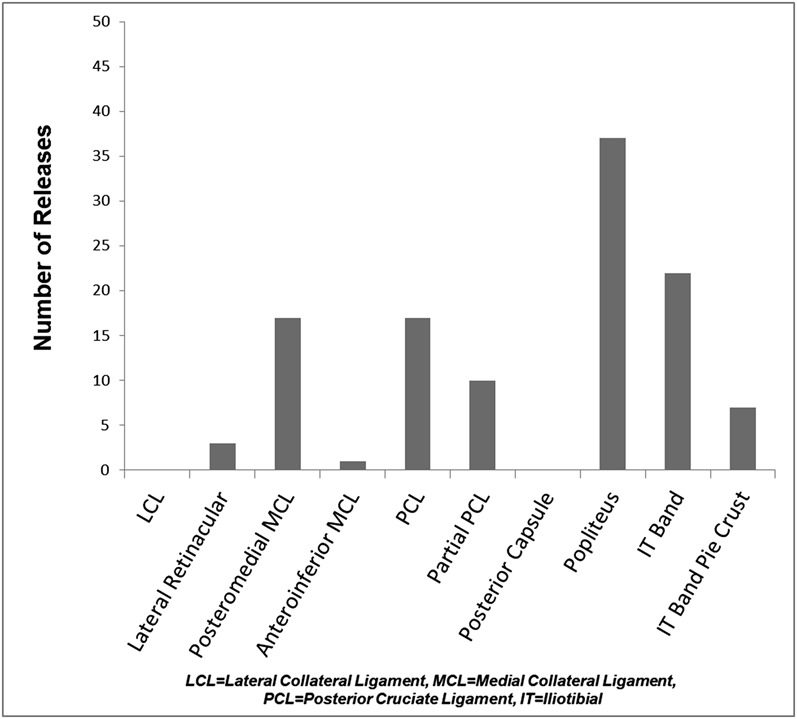
Fig. 3.
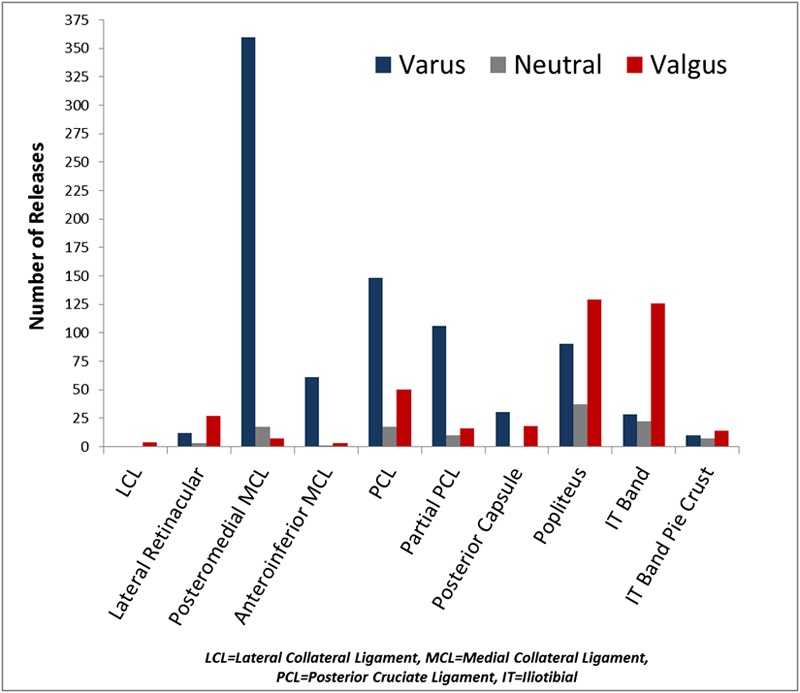
Bar graph showing the frequency of soft-tissue releases in all knees.
Fig. 4.
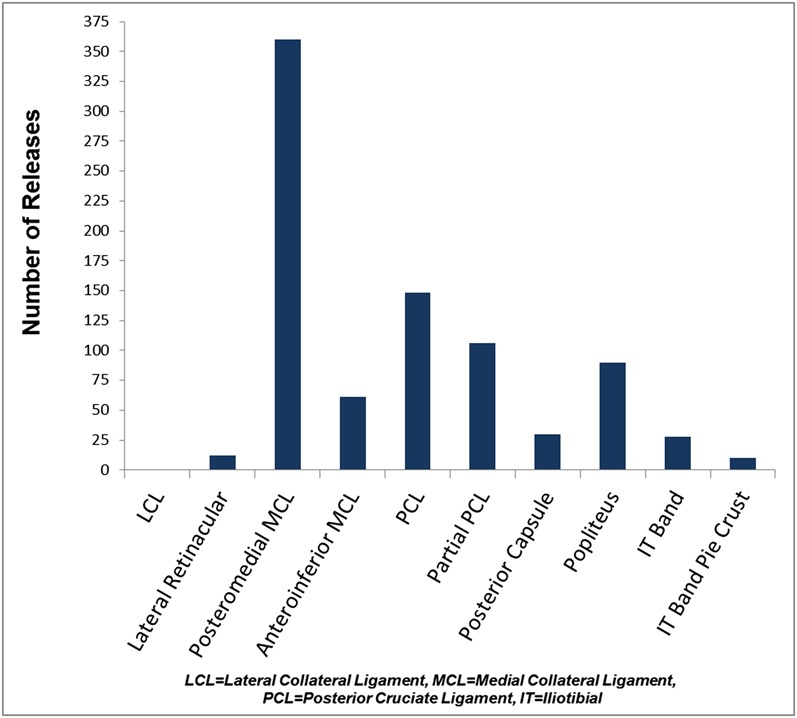
Bar graph showing the frequency of soft-tissue releases in varus knees.
Fig. 5.
Bar graph showing the frequency of soft-tissue releases in neutral knees.
Fig. 6.
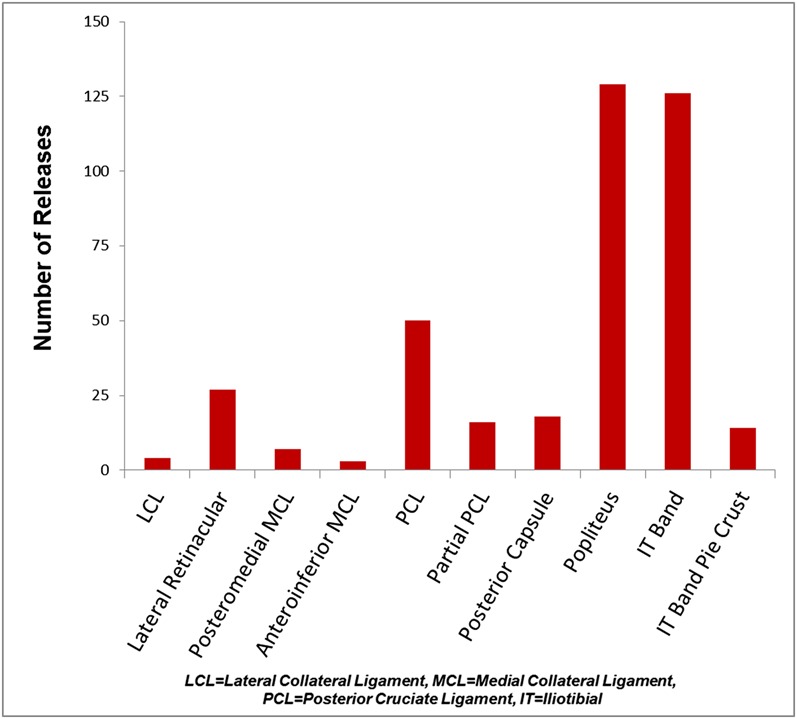
Bar graph showing the frequency of soft-tissue releases in valgus knees.
Fig. 7.
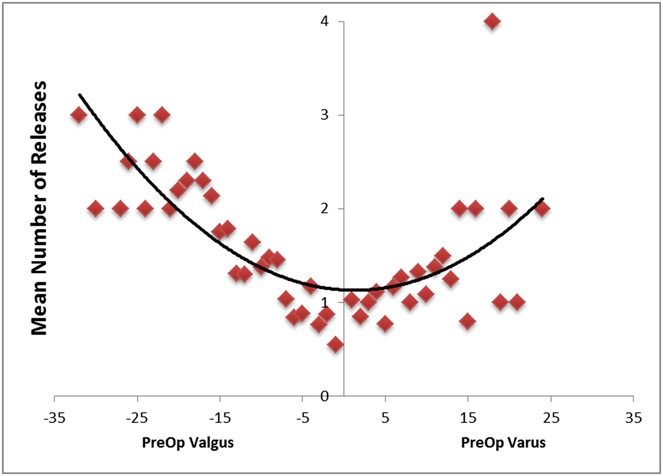
Scatterplot showing that the number of releases required increased with increased preoperative coronal malalignment (in degrees).
Clinical and Radiographic Results
All knees had a substantial improvement between the preoperative and the postoperative KSS. The only significant differences in functional outcome (as measured with the KSS) according to the preoperative alignment or the number of releases required were greater clinical and total postoperative KSS values in valgus knees with zero releases compared with valgus knees with one or two releases (Tables IV through IX).
TABLE IV.
KSS Clinical Subscore at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | KSS* | N | KSS* | N | KSS* | N |
| 0 | 94 ± 2 (74-100) | 20 | 88 ± 3 (42-100) | 20 | 90 ± 1 (43-100) | 167 |
| 1-2 | 84 ± 2 (12-100) | 77 | 90 ± 2 (42-100) | 36 | 92 ± 1 (16-100) | 239 |
| ≥3 | 90 ± 2 (62-100) | 34 | 94 ± 4 (80-100) | 6 | 92 ± 1 (70-100) | 34 |
The values are given as the mean and the standard error of the mean, with the range in parentheses.
TABLE V.
Comparison of KSS Clinical Subscores at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | Difference* | P Value | Difference* | P Value | Difference* | P Value |
| 1-2 vs. 0 | −11 (−18, −3) | 0.008 | 4 (−5, 12) | 0.40 | 2 (−1, 4) | 0.19 |
| ≥3 vs. 0 | −4 (−9, 1) | 0.11 | 7 (−7, 20) | 0.32 | 2 (−2, 6) | 0.35 |
| ≥3 vs. 1-2 | 5 (−2, 11) | 0.14 | 4 (−7, 16) | 0.48 | 0 (−4, 4) | 0.99 |
The values are given as the adjusted mean difference, with the 95% confidence interval in parentheses.
TABLE VI.
KSS Functional Subscore at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | KSS* | N | KSS* | N | KSS* | N |
| 0 | 84 ± 5 (30-100) | 21 | 78 ± 6 (5-100) | 23 | 85 ± 2 (3-100) | 172 |
| 1-2 | 74 ± 3 (0-100) | 78 | 84 ± 5 (5-100) | 38 | 84 ± 1 (−10-100) | 265 |
| ≥3 | 82 ± 4 (20-100) | 35 | 81 ± 9 (47-100) | 6 | 81 ± 4 (−5-100) | 37 |
The values are given as the mean and the standard error of the mean, with the range in parentheses.
TABLE VII.
Comparison of KSS Functional Subscores at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | Difference* | P Value | Difference* | P Value | Difference* | P Value |
| 1-2 vs. 0 | −12 (−24, 0) | 0.052 | 4 (−10, 17) | 0.59 | −0.3 (−4, 4) | 0.89 |
| ≥3 vs. 0 | −1 (−14, 11) | 0.82 | 2 (−24, 29) | 0.86 | −3 (−10, 4) | 0.41 |
| ≥3 vs. 1-2 | 8 (−3, 18) | 0.17 | −4 (−23, 16) | 0.71 | −3 (−10, 5) | 0.45 |
The values are given as the adjusted mean difference, with the 95% confidence interval in parentheses.
TABLE VIII.
Total KSS at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | KSS* | N | KSS* | N | KSS* | N |
| 0 | 178 ± 6 (112-200) | 20 | 165 ± 9 (64-200) | 20 | 175 ± 2 (56-200) | 167 |
| 1-2 | 160 ± 5 (12-200) | 77 | 173 ± 6 (64-200) | 36 | 177 ± 2 (24-200) | 238 |
| ≥3 | 173 ± 5 (90-200) | 34 | 175 ± 11 (127-200) | 6 | 175 ± 4 (118-200) | 34 |
The values are given as the mean and the standard error of the mean, with the range in parentheses.
TABLE IX.
Comparison of Total KSS at Last Follow-up Visit
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | Difference* | P Value | Difference* | P Value | Difference* | P Value |
| 1-2 vs. 0 | −21 (−40, −3) | 0.026 | 8 (−14, 29) | 0.49 | 2 (−4, 8) | 0.43 |
| ≥3 vs. 0 | −3 (−19, 13) | 0.69 | 10 (−27, 47) | 0.59 | 1 (−10, 12) | 0.82 |
| ≥3 vs. 1-2 | 13 (−3, 29) | 0.11 | 1 (−28, 30) | 0.95 | −2 (−13, 9) | 0.72 |
The values are given as the adjusted mean difference, with the 95% confidence interval in parentheses.
On the basis of the numbers available, the rates of revision, manipulation, reoperation, and major or minor complications in each group did not differ significantly according to the preoperative alignment or the number of required releases. A greater number of releases in this series of primary total knee arthroplasties did not increase the rates of revision, manipulation, or complications (Tables X through XVII).
TABLE X.
Occurrence of Major Complications*
| Preoperative Alignment† |
|||
| Releases Required | Valgus | Neutral | Varus |
| 0 | 1/40 (3%) | 2/48 (4%) | 11/319 (3%) |
| 1-2 | 4/146 (3%) | 3/68 (4%) | 16/472 (3%) |
| ≥3 | 1/52 (2%) | 0/7 (0%) | 7/64 (11%) |
Major complications included polyethylene exchange, periprosthetic fracture, deep or superficial irrigation and debridement, deep venous thrombosis, pulmonary embolism, patellar fracture, and death.
The values are given as the number of patients with a major complication relative to the total number of patients in that category, with the percentage in parentheses.
TABLE XI.
Comparison of the Occurrence of Major Complications
| Preoperative Alignment (P
Value) |
|||
| Releases Required | Valgus | Neutral | Varus |
| 1-2 vs. 0 | 0.92 | 0.94 | 0.87 |
| ≥3 vs. 0 | 0.87 | >0.99 | 0.11 |
| ≥3 vs. 1-2 | 0.76 | >0.99 | 0.051 |
TABLE XII.
Occurrence of Minor Complications*
| Preoperative Alignment† |
|||
| Releases Required | Valgus | Neutral | Varus |
| 0 | 8/40 (20%) | 6/48 (12%) | 47/319 (15%) |
| 1-2 | 23/146 (16%) | 19/68 (28%) | 60/472 (13%) |
| ≥3 | 10/52 (19%) | 2/7 (29%) | 11/64 (17%) |
Minor complications included hematoma, cellulitis, incisional infection, stitch abscess, blisters, postoperative bracing for six weeks, dehiscence, peroneal nerve dysfunction, iliotibial band syndrome, bursitis, tendinitis, and other.
The values are given as the number of patients with a minor complication relative to the total number of patients in that category, with the percentage in parentheses.
TABLE XIII.
Comparison of the Occurrence of Minor Complications
| Preoperative Alignment (P
Value) |
|||
| Releases Required | Valgus | Neutral | Varus |
| 1-2 vs. 0 | 0.38 | 0.18 | 0.16 |
| ≥3 vs. 0 | 0.94 | 0.43 | 0.25 |
| ≥3 vs. 1-2 | 0.56 | 0.94 | 0.31 |
TABLE XIV.
Closed Manipulations
| Preoperative Alignment* |
|||
| Releases Required | Valgus | Neutral | Varus |
| 0 | 1/40 (2%) | 0/48 (0%) | 10/319 (3%) |
| 1-2 | 1/146 (1%) | 5/68 (7%) | 19/472 (4%) |
| ≥3 | 1/52 (2%) | 1/7 (14%) | 3/64 (5%) |
The values are given as the number of patients with a manipulation relative to the total number of patients in that category, with the percentage in parentheses.
TABLE XV.
Comparison of Closed Manipulations
| Preoperative Alignment (P
Value) |
|||
| Releases Required | Valgus | Neutral | Varus |
| 1-2 vs. 0 | 0.36 | 0.13 | 0.47 |
| ≥3 vs. 0 | 0.87 | 0.25 | 0.50 |
| ≥3 vs. 1-2 | 0.46 | 0.91 | 0.81 |
TABLE XVI.
Femoral or Tibial Component Revisions
| Preoperative Alignment* |
|||
| Releases Required | Valgus | Neutral | Varus |
| 0 | 0/40 (0%) | 1/48 (2%) | 3/319 (1%) |
| 1-2 | 2/146 (1%) | 2/68 (3%) | 10/472 (2%) |
| ≥3 | 0/52 (0%) | 0/7 (0%) | 1/64 (2%) |
The values are given as the number of patients with a revision relative to the total number of patients in that category, with the percentage in parentheses.
TABLE XVII.
Comparison of Femoral or Tibial Component Revisions
| Preoperative Alignment (P
Value) |
|||
| Releases Required | Valgus | Neutral | Varus |
| 1-2 vs. 0 | >0.99 | >0.99 | 0.21 |
| ≥3 vs. 0 | >0.99 | >0.99 | 0.70 |
| ≥3 vs. 1-2 | >0.99 | >0.99 | 0.77 |
Postoperative short standing anteroposterior radiographs were available for review for 1171 (96.3%) of the knees, and these were measured to assess the anatomic axis; 73% (855) attained the goal of 2° to 8° of anatomic valgus (Fig. 8, Tables XVIII and XIX). Adequate postoperative long standing radiographs were available for review for 972 (80%) of the knees, and these were measured to assess the hip-knee-ankle angle (mechanical axis). The goal was 0°, and the mean postoperative mechanical axis (and standard deviation) was 0.7° ± 3.7° (Fig. 9, Table XX).
Fig. 8.
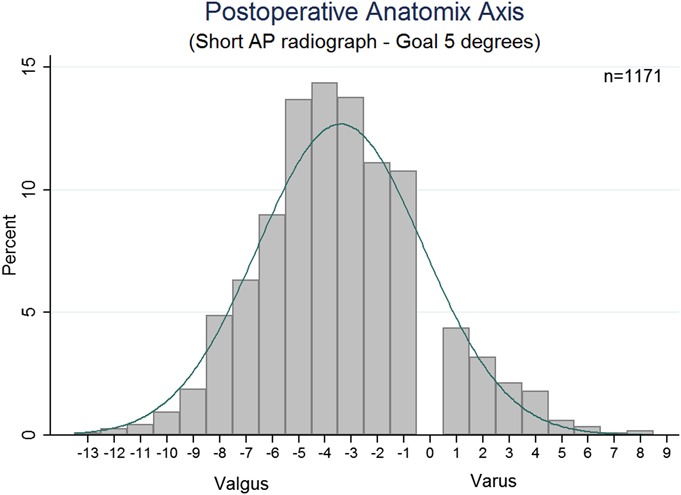
Histogram showing the postoperative alignment (in degrees) of 1171 knees according to the anatomic axis on a short anteroposterior (AP) radiograph.
TABLE XVIII.
Change in Coronal Alignment of the Anatomic Axis on Short Standing Radiographs
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | Change* (deg) | N | Change* (deg) | N | Change* (deg) | N |
| 0 | 6.6 ± 0.6 (1-17) | 39 | 2.9 ± 0.4 (0-11) | 47 | 5.5 ± 0.2 (0-20) | 308 |
| 1-2 | 8.4 ± 0.4 (0-29) | 139 | 3.0 ± 0.3 (0-10) | 66 | 7.1 ± 0.2 (0-27) | 457 |
| ≥3 | 12.3 ± 0.7 (2-27) | 47 | 4.3 ± 0.7 (1-6) | 7 | 7.7 ± 0.6 (0-26) | 61 |
The values are given as the mean and the standard error of the mean, with the range in parentheses.
TABLE XIX.
Comparison of the Change in Coronal Alignment of the Anatomic Axis on Short Standing Radiographs
| Preoperative Alignment |
||||||
| Valgus |
Neutral |
Varus |
||||
| Releases Required | Difference* (deg) | P Value | Difference* (deg) | P Value | Difference* (deg) | P Value |
| 1-2 vs. 0 | 2.2 (0.5, 3.8) | 0.01 | 0.1 (−0.8, 1.0) | 0.78 | 1.5 (0.9, 2.1) | <0.001 |
| ≥3 vs. 0 | 5.6 (3.8, 7.5) | <0.001 | 1.4 (−0.7, 3.4) | 0.19 | 2.1 (1.1, 3.2) | <0.001 |
| ≥3 vs. 1-2 | 3.8 (2.1, 5.4) | <0.001 | 1.4 (−0.5, 3.2) | 0.15 | 0.2 (−1.0, 1.5) | 0.69 |
The values are given as the adjusted mean difference, with the 95% confidence interval in parentheses.
Fig. 9.
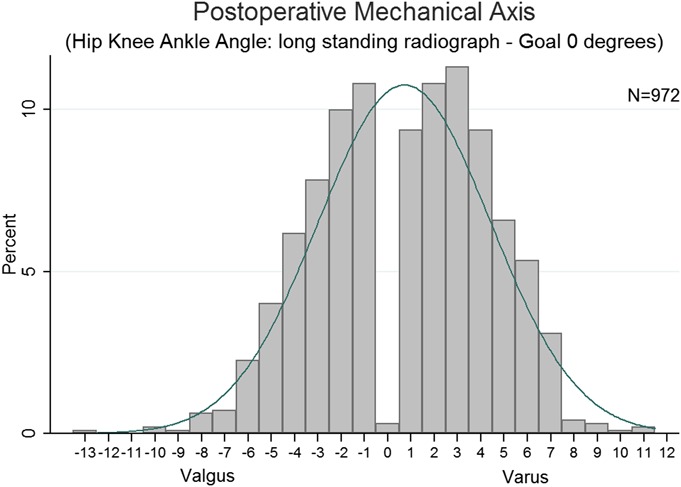
Histogram showing the postoperative alignment of 972 knees according to the mechanical axis (hip-knee-ankle angle) on a long standing radiograph.
TABLE XX.
Radiographic Analysis of Anatomic and Mechanical Axes
| Parameter | Mean | Range | Std. Dev. |
| Anatomic axis | |||
| Preop. | 1° valgus | 32° valgus to 24° varus | 7.38° |
| Change in alignment | 2.14° | 27° valgus to 29° varus | 7.85° |
| Postop., n = 1171 | 3.4° valgus | 13° valgus to 8° varus | 3.15° |
| Varus knees | 3.35° valgus | 12° valgus to 8° varus | 3.16° |
| Neutral knees | 3.68° valgus | 13° valgus to 5° varus | 3.29° |
| Valgus knees | 3.47° valgus | 12° valgus to 8° varus | 3.18° |
| Mechanical axis | |||
| Postop., n = 972 | 0.7° valgus | 13° valgus to 11° varus | 3.70° |
| Varus knees | 1.3° varus | 10° valgus to 11° varus | 3.63° |
| Neutral knees | 0.5° valgus | 8° valgus to 7° varus | 3.29° |
| Valgus knees | 0.7° valgus | 13° valgus to 10° varus | 3.68° |
Discussion
Soft-tissue releases play an important role in balancing a total knee replacement1,3-6,16,17,19-21. The objective of our study was to describe the soft-tissue releases necessary to achieve balanced flexion and extension gaps in primary total knee arthroplasty performed with a consistent surgical technique involving measured resection and posterior femoral component referencing. Additionally, we sought to assess the frequency of releases according to preoperative alignment, clinical and radiographic results, associations with failure, and perioperative complications. Given the predicted rise in the number of future total knee replacements22, this information may facilitate both refinement of the surgical technique and understanding of potential failure mechanisms in primary total knee arthroplasty.
Consistent with other reports2,5,6,19,21, selection of the structures to be released during the primary total knee arthroplasty was dependent on the preoperative deformity. Of the 1216 knees, 855 (70.3%) had preoperative varus deformity, and release of the posterior oblique or the anterior portion of the MCL was required in 49% (419) of these knees. In the 238 knees (19.6%) that had preoperative valgus deformity, 53% (126) required release of the iliotibial band and 54% (129) required release of the popliteus tendon. In total, 809 (67%) of the 1216 knees required one or more releases to achieve a balanced total knee replacement. Thirty percent (37) of the 123 knees with neutral preoperative alignment required release of the popliteus tendon. As described previously, this may be the consequence of appropriate external rotation of the femoral component and the resultant decrease (and subsequent tightness) in the lateral flexion gap3.
Seventy-three percent of the knees treated with the described selective soft-tissue release technique were corrected to the goal of 2° to 8° of anatomic valgus, as measured on a postoperative short standing anteroposterior knee radiograph. Clinical outcomes, as measured with the KSS, were improved for varus, valgus, and neutral knees. Aside from a difference in the postoperative KSS between knees with zero releases (mean KSS = 178) and those with one or two releases (KSS = 160), the improvements in the KSS were independent of the number of releases performed. There were no differences in the rates of complications, revisions, or manipulations among varus, valgus, and neutral knees according to the number of soft-tissue releases required. This would suggest that the technique of selective soft-tissue release is not associated with increased morbidity or failure.
The concept of selective soft-tissue release and the resultant independent effect on the flexion and extension spaces has been described by Whiteside, Krackow, and colleagues2,5,6,19. In 2000, Whiteside et al. described the concept in a cadaver model and a subsequent clinical study, which demonstrated that a high percentage of varus knees required release of the posterior oblique and anterior portions of the MCL due to tightness of the extension and the flexion space, respectively6. This technique was in contrast to previous techniques in which a more global release of soft-tissue structures prior to bone cuts was advocated23. Selective release for valgus deformity has also been described by several authors3,4,19,24,25, although clinical results were not commonly reported; the exception was the study by Aglietti et al., who reported good clinical and radiographic results with low complication rates24.
Regardless of the magnitude or direction of preoperative deformity, the selective soft-tissue releases in the present series restored overall limb alignment to within 3° of the anatomic axis goal (5° of valgus) in the majority of the knees. Furthermore, knees with varus or valgus deformity required more releases to restore postoperative alignment to the normal range compared with neutrally aligned knees. These findings are in agreement with cadaver-based studies of valgus knees showing that successive release of tight soft-tissue structures has a cumulative effect that would be applicable to knees with greater degrees of deformity3,25.
The current study has several limitations. First, although the type and number of soft-tissue releases for each knee were recorded prospectively according to a defined protocol, the clinical and radiographic follow-up data were obtained retrospectively and may be prone to biases inherent in a retrospective study. Second, complete KSS data were available for only 52% of the patients. Nevertheless, because of the large sample size, the study was adequately powered to detect differences in clinical outcome if they were present. Additionally, the perioperative complication data and radiographic data were substantially more complete, with 96% of the knees having adequate radiographic information. Third, the radiographic measurements were performed by only one member of the research team, and intraobserver reliability was not calculated. Nevertheless, only simple anatomic and mechanical axis measurements were included in this study, and the radiographic measurement methodology was consistent throughout. Fourth, there may have been limitations associated with using short radiographs for the measurement of coronal knee alignment. However, Colebatch et al.18 reported that anteroposterior standing radiographs of the knee are just as reliable as full-limb radiographs when measuring knee alignment. Thus, we do not believe that use of the short radiographs resulted in a notable limitation of this study. Additionally, the large number of radiographs reviewed in this study helps control for the potential variances in the measurements. Finally, and perhaps most importantly, assessment of the tightness requiring the selected soft-tissue releases was based on intraoperative observation and the perception of the senior surgeon and was not quantified. Direct measurement of the existing flexion and extension gap sizes and tensions present intraoperatively prior to soft-tissue release would have provided more concrete information on which to base the proposed releases.
In conclusion, selective soft-tissue release for gap balancing in primary total knee arthroplasty was a safe and effective technique and was associated with excellent clinical and radiographic results. Consistent anatomic coronal-plane alignment and soft-tissue balance could be achieved without bone cut modification. The technique is applicable to varus, valgus, and neutral knees and accommodates PCL retention or substitution. Valgus knees were more likely than both varus and neutral knees to require one or more releases to achieve a balanced total knee replacement. Compared with the more global release of tight concave structures advocated in the early total knee arthroplasty experience, selective soft-tissue release may avoid subsequent flexion instability and the need for increased levels of prosthetic constraint.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Acknowledgments
Note: The authors thank Gregory Stoddard for his contribution to the statistical analysis. This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the Public Health Services research grants UL1-RR025764 and C06-RR11234.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Griffin FM, Insall JN, Scuderi GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000 Dec;15(8):970-3 [DOI] [PubMed] [Google Scholar]
- 2.Mihalko WM, Whiteside LA, Krackow KA. Comparison of ligament-balancing techniques during total knee arthroplasty. J Bone Joint Surg Am. 2003;85(Suppl 4):132-5 [DOI] [PubMed] [Google Scholar]
- 3.Peters CL, Mohr RA, Bachus KN. Primary total knee arthroplasty in the valgus knee: creating a balanced soft tissue envelope. J Arthroplasty. 2001 Sep;16(6):721-9 [DOI] [PubMed] [Google Scholar]
- 4.Ranawat CS, Rose HA, Rich DS. Total condylar knee arthroplasty for valgus and combined valgus-flexion deformity of the knee. Instr Course Lect. 1984;33:412-6 [PubMed] [Google Scholar]
- 5.Whiteside LA. Soft tissue balancing: the knee. J Arthroplasty. 2002 Jun;17(4)(Suppl 1):23-7 [DOI] [PubMed] [Google Scholar]
- 6.Whiteside LA, Saeki K, Mihalko WM. Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000 Nov;380:45-57 [DOI] [PubMed] [Google Scholar]
- 7.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993 Jan;286:40-7 [PubMed] [Google Scholar]
- 8.Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA. Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty. 2001 Apr;16(3):301-5 [DOI] [PubMed] [Google Scholar]
- 9.Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000 Nov;380:72-9 [DOI] [PubMed] [Google Scholar]
- 10.Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):102-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty. 2000 Apr;15(3):354-9 [DOI] [PubMed] [Google Scholar]
- 12.Nagamine R, Miura H, Inoue Y, Urabe K, Matsuda S, Okamoto Y, Nishizawa M, Iwamoto Y. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci. 1998;3(4):194-8 [DOI] [PubMed] [Google Scholar]
- 13.Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995 Dec;321:168-72 [PubMed] [Google Scholar]
- 14.Sierra RJ, Berry DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty. 2008 Oct;23(7)(Suppl):20-3 Epub 2008 Aug 12 [DOI] [PubMed] [Google Scholar]
- 15.Jacobs WC, Clement DJ, Wymenga AB. Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. 2005;(4):CD004803 Epub 2005 Oct 19 [DOI] [PubMed] [Google Scholar]
- 16.Peters CL. Soft-tissue balancing in primary total knee arthroplasty. Instr Course Lect. 2006;55:413-7 [PubMed] [Google Scholar]
- 17.Peters CL, Severson E, Crofoot C, Allen B, Erickson J. Popliteus tendon release in the varus or neutral knee: prevalence and potential etiology. J Bone Joint Surg Am. 2008 Nov;90(Suppl 4):40-6 [DOI] [PubMed] [Google Scholar]
- 18.Colebatch AN, Hart DJ, Zhai G, Williams FM, Spector TD, Arden NK. Effective measurement of knee alignment using AP knee radiographs. Knee. 2009 Jan;16(1):42-5 Epub 2008 Sep 14 [DOI] [PubMed] [Google Scholar]
- 19.Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002 Jan-Feb;10(1):16-24 [DOI] [PubMed] [Google Scholar]
- 20.Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB. Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc. 2010 Mar;18(3):381-7 [DOI] [PubMed] [Google Scholar]
- 21.Stern SH, Moeckel BH, Insall JN. Total knee arthroplasty in valgus knees. Clin Orthop Relat Res. 1991 Dec;273:5-8 [PubMed] [Google Scholar]
- 22.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780-5 [DOI] [PubMed] [Google Scholar]
- 23.Insall J, Ranawat CS, Scott WN, Walker P. Total condylar knee replacment: preliminary report. Clin Orthop Relat Res. 1976 Oct;120:149-54 [PubMed] [Google Scholar]
- 24.Aglietti P, Lup D, Cuomo P, Baldini A, De Luca L. Total knee arthroplasty using a pie-crusting technique for valgus deformity. Clin Orthop Relat Res. 2007 Nov;464:73-7 [DOI] [PubMed] [Google Scholar]
- 25.Kanamiya T, Whiteside LA, Nakamura T, Mihalko WM, Steiger J, Naito M. Ranawat Award paper. Effect of selective lateral ligament release on stability in knee arthroplasty. Clin Orthop Relat Res. 2002 Nov;404:24-31 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest


